Abstract
The ovarian follicle represents the basic functional unit of the ovary and consists of an oocyte, which is surrounded by granulosa cells (GCs). GCs play an important role in the growth and development of the follicle. They are subject to increased attention since it has recently been shown that the subpopulation of GCs within the growing follicle possesses exceptionally plasticity showing stem cell characteristics. In assisted reproduction programs, oocytes are retrieved from patients together with GCs, which are currently discarded daily, but could be an interesting subject to be researched and potentially used in regenerative medicine in the future. Isolated GCs expressed stem cell markers such as OCT-4, NANOG and SOX-2, showed high telomerase activity, and were in vitro differentiated into other cell types, otherwise not present within ovarian follicles. Recently another phenomenon demonstrated in GCs is transdifferentiation, which could explain many ovarian pathological conditions. Possible applications in regenerative medicine are also given.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Granulosa cells (GCs) play an important role in the growth and development of the follicle in the process known as folliculogenesis. With development of gap junctions they connect to each other and to the oocyte [51]. Complex bidirectional communication with the oocyte includes providing essential nutrients for oocyte development and accumulation of oocyte secreted metabolites [71]. Moreover, the natural role of GCs includes hormonal activity with production of estradiol during follicular growth and secretion of progesterone after ovulation [85].
From a granulosa cell perspective folliculogenesis translates to the dynamic process starting with changing the shape from flattened to cuboidal followed by mitosis and expression of follicle-stimulating hormone receptor (FSHR). Moreover, in a pre-ovulatory follicle, the spatial distribution creates four different granulosa cell layers: the outermost layer is the membrana granulosa, the inner most layer is the periantral, the intermediate layer is the cumulus oophorus, and the layer juxtaposed to the oocyte is the corona radiata [17]. All four layers are also functionally heterogeneous, secrete different molecules and express various hormone receptors [55]. The GCs are subject to increased attention since it has recently been shown that the subpopulation of GCs within the growing follicle is not terminally differentiated but showing stem cell characteristics [39, 41, 47, 77].
In the assisted reproduction programme GCs are in general ignored and constitute an uninteresting part of the in vitro fertilization procedure where follicular fluid together with GCs is unavoidably removed from the antrum during transvaginal ultrasound-guided aspiration of oocytes from mature follicles. Follicular fluid fills the antrum and surrounds the oocyte and its composition reflects changes in the secretory processes of granulosa and theca layers [16]. Besides oocytes, the aspirated follicular fluid contains granulosa, thecal, ovarian surface and vaginal epithelial cells, since an ultrasound-guided needle penetrates all these tissues. Following the removal of oocytes, the remaining cell-rich follicular aspirate is usually discarded in daily practice. However, it could be used for further immunoassays [37] or as a potential source of stem cells [25]. Among follicular cells GCs show the biggest stem cell potential, as recently demonstrated by several studies. In this mini-review the current knowledge on stem cell characteristics and transdifferentiation potential of GCs is presented and discussed. We also try to evaluate the follicular fluid retrieved in the in vitro fertilization program as a potential source of stem cells to be used in regenerative medicine in the future.
Expression of stem cell markers in granulosa cells from follicular aspirates
The presence of somatic stem cells in the ovary has not been speculated for a long time, however it is now clear that ovaries, like many other adult tissues and organs, contain somatic stem cells. Putative stem cells were found in the adult ovarian surface epithelium of different mammals, including humans [61, 78–80], in mouse ovarian stroma [21] and in the theca layer [29], which surrounds the developing follicle.
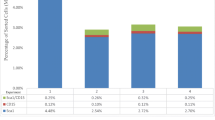
Stem cell potential of GCs was first indicated by Kossowska-Tomaszczuk et al. [41]. They demonstrated that luteinizing GCs isolated from the ovarian follicles of infertile patients included in the assisted reproduction program can be differentiated into other cell types, otherwise not present within ovarian follicles, such as neurons, chondrocytes and osteoblasts. The GCs were isolated from follicular aspirates—follicular fluid—obtained from patients after treatment with human menopausal gonadotropins, recombinant FSH, and 10,000 IU of human chorionic gonadotropin for controlled ovarian hyperstimulation and oocyte retrieval. Firstly, they showed that the prerequisite for successful long-term culturing of GCs is leukemia-inhibiting factor (LIF) added to the culture medium. In their cultures GCs exhibited two distinct morphologies: epithelial and fibroblastic-like. The ephitelial-like cells disappeared after approximately 3-weeks of culturing, whereas the remaining cells retained their fibroblastic morphology. After 1 week of culturing GCs progressively lost their ability to express FSHR and after 8 weeks they also lost the aromatase activity; however 1–3 % of GCs expressing FSHR also expressed OCT-4 marker of pluripotency. The OCT-4 marker was expressed in the freshly collected luteinizing GCs and remained expressed in the luteinizing GCs throughout the culturing, as revealed by reverse transcriptase-PCR and immunocytostaining. Additionally, GCs were positive for various markers of mesenchymal stem cells: CD29, CD44, CD90, CD105, CD117, and CD166, but not for CD73 [41]. Another study by Varras et al. [77] showed that OCT-4 gene was expressed in GCs of women included in the assisted reproduction program, namely in 48 % of the studied women; however, the expression of this gene was demonstrated only by real time-PCR methodology. They carefully analyzed if OCT-4 expression was related to female clinical parameters (i.e., age, BMI, duration and causes of infertility, previous assisted reproduction attempts, basal serum FSH and LH levels, serum levels of PRL, serum estradiol levels on the fifth day of rFSH administration and on the day of hCG administration, the total dose of rFSH, the duration of treatment, the type of assisted reproduction, the number of aspirated follicles etc.), but they did not find any correlation. Unlike Kossowska-Tomaszczuk et al. [41] study in which GCs were pooled from various infertile women, Varras et al. [77] analyzed the gene expression of GCs in each single patient with tubal factor of infertility or with infertile partner. Although the OCT-4 transcription factor is a solid marker of cell stemness, we need to be careful when selecting the appropriate primers. The OCT-4 can encode three spliced variants designated as OCT-4A, OCT-4B and OCT-4B1, latest being also detected in various non-stem cell types [2]. Moreover, OCT-4 may play role in follicular development and oogenesis hence expression in ovarian compartments could be higher independent of the possible role in maintaining stem cell population [49, 87].
In contrast, Mattioli et al. [47] did not detect any sign of Oct-4 expression in isolated pig GCs. However, they demonstrated expression of other three typical pluripotent stem cell markers Nanog, Sox-2 and TERT in both growing and luteinized GCs. Although drastically reduced, all three markers were detected in GCs even after 3 weeks of in vitro osteogenic differentiation. It should be highlighted that they decided not to carry out any purification step based on the presence of FSHR or some other factor, but considered the isolated GCs as a homogeneous cell population in terms of their stemness. This is an interesting approach since all ovarian somatic cells coexist in the common ovarian niche [8], which can play an important role in maintaining of their stemness.
Comparing results of all three above described studies is difficult since all three studies used different methodologies when obtaining and processing GCs. Kossowska-Tomaszczuk et al. [41] isolated GCs from aspirated follicular fluid of infertile patients based on FSHR; Varras et al. [77] collected GCs from cumulus-oocyte complex during oocyte retrieval from fertile patients; and Mattioli et al. [47] scraped GCs from internal face of the follicle wall obtained from prepubertal pigs. First variable which can affect differences in stem cell markers is fertility since it was found that the cause of female infertility can drastically affect the GCs viability [34]; therefore this factor should always be taken into account when discussing the stem cell characteristics of GCs. Secondly, expression of genes varies between species and projection (e.g. from pig) on human is not always reliable. Thirdly, and most importantly, we see the main methodological difference in the location of isolated GCs. Kossowska-Tomaszczuk et al. [41] did experiments with aspirated GCs, which were probably mixture of all four granulosa layers, while Varras et al. [77] worked just with GCs from cumulus layer. On the other side Mattioli et al. [47] worked with GCs from periantral layer. The location of GCs seems to be an important factor, which has been overlooked when researching their plasticity. It is known that dynamics of GCs during expansion in growing follicle differs within the cellular mass [64]. Erickson [17] postulated that precursor cells could be located in the periantral layer of GCs. It was demonstrated that GCs in the membrane domain stop proliferating earlier than those in the central domain, which continue to divide through the healthy follicle development [26]. Overall, we think that the cause for discrepancy in expressing stem cells markers in GCs is using cells from different locations within granulosa layers. For the future research it is necessary to qualify subpopulations of GCs within preovulatory follicle. Kossowska-Tomaszczuk and De Geyter [39] proposed the hypothesis about several subpopulations based on the presence of FSHR and luteinizing hormone receptor (LHR) markers. We speculate that this hypothesis can be upgraded with the factor of location in the granulosa layers. Moreover, the question whether granulosa stem cells originate from the first line of flattened GCs in the primordial follicle or from the granulosa nests in ovarian surface epithelium [7] still remains opened.
Some additional evidence for stem cell characteristics of GCs came from cloning experiments by somatic cell nuclear transfer (SCNT) in animals since it has been demonstrated that cloning is more successful if the donor nucleus is provided from less differentiated cells [73]. Successful nuclear transfers using adult GCs nuclei have already been reported [15, 59, 82]. Moreover Pandey et al. [59] demonstrated that using GCs from cumulus layer is more successful at cloning by SCNT then using GCs from non-cumulus layer which is in favor of our hypothesis that location of GCs matters when studying their plasticity.
Telomerase activity and stemness in granulosa cells
The telomerase activity is another evidence for the stemness of normal, non-cancer cells in the ovaries [43, 53]. Telomerase is represented by a complex of reverse transcriptase proteins encoded by the TERT (telomerase reverse transcriptase) gene. In addition to maintaining the integrity of chromosomes ends (telomeres), telomerase plays an important role in the process of cell proliferation. All chromosomes are losing telomeric DNA during each cell division. However, adult stem cells are characterized by a relatively slower rate of telomere shortening in comparison with adult non-stem cells [27] and thus having high telomerase activity and the longest telomeres within a given tissue [19].
High telomerase activity was demonstrated in bovine growing follicles, where telomerase RNA was localized in the periantral layer. Telomerase activity was the highest in the smallest examined follicles and was decreasing significantly as the follicles enlarged [42]. Interestingly, it was shown that there is no significant difference between pig small antral and large antral follicles in telomerase activity of granulosa cells [74]. Additionally, a significantly decreased telomerase activity was observed in large and atretic follicles in comparison to small and healthy follicles in rat [83]. In human the low level of telomerase activity in the ovary was found to be related to the age-related primordial follicle depletion and it was speculated that telomerase activity could be used as a marker of the ovarian functional age [35]. Moreover, it was showed that the relative telomere length was longer in GCs from mature oocytes compared with GCs from immature oocytes in human [12]. In addition, the abnormal telomere lengths in GCs were confirmed to be related to the female infertility and diminished ovarian reserve [10]. It was shown that luteinized human GCs have a certain potential for proliferation and that telomerase activity of luteinized GCs may predict the clinical outcomes of in vitro fertilization [11]. In primary and preantral pig follicles, TERT was confirmed to be localized in granulosa cells and in germ cells, with a typical nuclear location. During antral differentiation only GCs close to the antrum and cumulus cells maintained the TERT expression [66]. Telomerase activity seems to be highly related to the estrogen metabolism since estrogen showed mitogenic effects on GCs proliferation by up-regulation of TERT gene [4], suggesting that infertile patients with estrogen deficiency are not suitable for research of their GCs stemness. Recently, more on the impact of steroid hormones, antiestrogens and aromatase inhibitors on telomerase activity was reviewed by Chronowska [13].
It was proven that telomerase activity in stem cells is regulated by Wnt signaling pathway [28]. The Wnt signaling pathway is a network of proteins that passes signals from receptors on the cell surface through the cytoplasm and ultimately to the nucleus where the signaling cascade leads to the expression of target genes. It controls the cell-cell communication, cell proliferation and differentiation during development and in adult tissues. In postnatal ovary Wnt signaling is required for normal folliculogenesis and is highly expressed in GCs as reviewed by Boyer et al. [6]. Currently, three different pathways are believed to be activated upon Wnt receptor activation, however Wnt/β-catenin is best understood [14]. Wnt/β-catenin signaling maintains stemness in stem cells from different tissues and prevents them from differentiating [36, 70]. For mouse GCs it was demonstrated that WNT2 protein regulates their proliferation through β-catenin pathway [18, 81] which when misregulated can lead to ovarian granulosa cell tumor (GCT) [5].
Altogether it is clear that GCs possess greater telomerase activity in comparison with non-stem adult cells. This could be a consequence of a progenitor GCs subpopulation which is characterized by high proliferation rate regulated by Wnt/β-catenin signaling pathway. According to localization of telomerase RNA and TERT highly proliferative subpopulation of GCs originate from periantral layer.
Granulosa cells and ability for transdifferentiation
Transdifferentiation is the switch of cell from one differentiated type into another as defined by Okada [56]. The natural transdifferentiation occurs in two steps: firstly, the cell dedifferentiates; and secondly, the natural developmental program is activated, allowing the cell to differentiate into the new lineage [3, 32, 72]. It is particularly common in organisms such as amphibians that exhibit regeneration of missing parts. For example, when the lens is removed in the eye, pigmented epithelial cells from the dorsal iris first dedifferentiate, proliferate to create new lens vesicle, and then differentiate into the mature cells of the lens [75]. In mammals, natural transdifferentiation is very rare and is exemplified by the formation of coronary arteries from venous cells [63]. However, there are various methods to induce transdifferentiation, which were successfully demonstrated also in mammalian cells [62]. Firstly, using defined culture medium with high concentration of glucose after removing LIF successfully transdifferentiated liver cells to pancreatic-like cells [84]. Secondly, using co-cultures, cardiomyocytes induced skeletal muscle-derived cells to transdifferentiate into cardiomyocytes [30]. Thirdly, with ectopic expression of transcription factors C/EBP alpha, PPAR gamma and SREBP-1 transdifferentiation of fibroblasts into adipocyte-like cells was achieved [45]. Lastly, human fibroblasts have been successfully transdifferentiated to human T cells using cellular extract of human T cells [23].
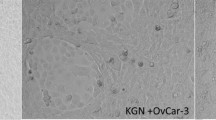
Bukovsky et al. [9] observed that when porcine ovarian granulosa cells were cultured in vitro, they changed their morphology into fibroepithelial phenotype. Moreover, after exposure of cells to the mixture of testosterone and progesterone after pretreatment with estradiol, a majority of granulosa cells transdifferentiated into neuron-like cells. These cells manifested an interconnectivity resembling primitive neuronal pathways in culture. They expressed SSEA-1, SSEA-4, NCAM and Thy-1 and showed characteristic neuronal morphology.
The main study in the field of GCs transdifferentiation was recently done by Oki et al. [57]. As many researchers mentioned above, they first observed that pig GCs began to proliferate and dedifferentiate into fibroblast-like cells after 48 h of culturing. In contrast to Kossowska-Tomaszczuk’s and Varros’s experiments they found that stem cell-related genes, such as Oct-4, were not expressed in freshly collected GCs. Interestingly, microarray assays revealed that GCs gradually started to express osteogenic genes during the culture, whereas the expression of GCs-specific genes decreased in the absence of any special factors. After osteogenic induction, dedifferentiated GCs underwent terminal osteoblast differentiation and matrix mineralization in vitro. Furthermore, when dedifferentiated GCs were transplanted into SCID mice, these cells formed ectopic osteoid tissue. Moreover, GCs that expressed osteogenic genes were completely differentiated into mature osteoblasts in vitro and in vivo. Taken together, they postulated that GCs can transdifferentiate into osteoblasts not as stem cells, but as functional differentiating cells both in vitro and in vivo [57]. This observation can be supported by some previous reports on the pathological condition of ovary in which the osteoid tissue was found [48, 52, 54, 65]. In one patient the ovarian tumor with predominating Sertoli cells and the calcified/ossified areas at the center of Sertoli cell nodule was reported [50]. We may speculate that the bone morphogenetic proteins (BMPs) could be involved in such cases since it is clear that BMP-2, BMP-6, BMP-7, BMP-9 can regulate differentiation of mesenchymal stem cells into osteogenic tissue in vitro and in vivo [46]. Moreover, it is known that BMPs affect granulosa cell physiology, among other things also GCs proliferation [20, 58]. It is an important question why GCs are so favorable for osteogenic differentiation and it was postulated that this may be related to RUNX2 transcriptional factor, fundamental for osteogenic differentiation [38, 86] and up-regulated in the process of GCs luteinization [60].
Uhlenhaut et al. [76] demonstrated the ability of GCs to transdifferentiate through conditional loss of a single transcriptional regulator FOXL2 into comparable male cell type—Sertoli-like cells. Sertoli cells are elongated cells supporting the germ cells of the seminiferous tubules in the testis; sharing a common precursor with GCs during prenatal development, they also inherit many characteristics with them [1]. In their study Uhlenhaut et al. [76] created homozygous Foxl2 mice line and 3 weeks after tamoxifen-induced Foxl2 deletion the appearance of testicular seminiferous tubules and the cells with morphological characteristics of Sertoli cells instead of GCs were found in the ovaries by histological examination. Moreover, they showed that the process of GCs reprogramming was autonomous, stable and independent of oocyte function.
The transcriptional regulator FOXL2 is required for optimal formation of primary follicles in the ovaries; in Foxl2-null mouse ovaries, granulosa cells fail to complete the squamous to cuboidal transition, thus resulting in the arrest of folliculogenesis at the primordial follicle stage [67]. Moreover, adult granulosa cell tumor (GCT) has recently been characterized by a single somatic missense mutation in the FOXL2 gene in human [31]. Since it is known that GCT can occurs also in the testes of juvenile and adult males [24, 68], transdifferentiation in relation with FOXL2 action could take a place [44].
Altogether, spontaneous transdifferentiation was observed from GCs to osteoblasts in vitro and in vivo. Induced transdifferentiation was demonstrated from GCs to neuron-like cells in vitro and Sertoli-like cells in vivo. Process seems to be physiologically relevant since cells which were transdifferentiated from GCs appear in different ovarian pathological conditions.
Conclusion
The expression of different stem cell markers, high telomerase activity and ability to differentiate into cell types otherwise not present within ovary are main arguments for stem cell characteristics of GCs with not exactly defined level of stemness yet. The discovery that GCs poses exceptional plasticity among somatic ovarian cells definitely requires attention. All these data show that the follicular fluid is rich in GCs and daily discarded in the in vitro fertilization program, but might be an interesting subject to be researched and to be used in the regenerative medicine in the future. In reproductive medicine we are especially interested in regeneration of ovarian function which represents the most important and complex part of reproductive tract. Loss of ovarian function caused by premature ovarian failure, chemotherapy or menopause not only affects the reproductive ability but also leads to termination of sex hormones production, which is one of the natural role of GCs. Cell therapy could be an ideal long-term solution for regeneration of ovarian endocrine function. The idea is to isolate stem cell population from GCs, enrich this population and transplant it to the patient. Kossowska-Tomaszczuk et al. [40] developed a three-dimensional (3D) culture system which allowed the long-term survival, growth and enrichment of luteinizing GCs subpopulation isolated from mature ovarian follicles. The 3D system supported them to proliferate into spherical structures exhibiting steroidogenic capacity. After transplantation into the ovaries of immunodeficient mice, these cells became localized preferentially within antral follicles. Moreover, they demonstrated expression of FSHR in transplantated GCs and thus their functionality. However, use of luteinized GCs as therapeutic cells is questioned since high rate of aneuploidy in GCs was reported in women who underwent in vitro fertilization [22, 33]. This limitation could be overcome with isolating and transplanting less differentiated subpopulation of GCs which has not yet undergone luteinization. On the other side, Sittadjody et al. [69] constructed multilayered microcapsule with encapsulated theca cells and GCs from rats to recapitulate the follicular structure. They assessed microcapsules in vitro and demonstrated high viability of encapsulated cells which secreted sex steroids and peptide hormones. Ambitiously, in the future we could transplant engineered follicle as allografts or xenografts.
To that end, the further research of GCs at the molecular, cellular and tissue level will definitely help to better understand the GCT manifestation and recurrence, female infertility, and the outcome of assisted reproduction treatments. Better understanding of GCs proliferation could also play a crucial role in the developing of cell therapies and engineering of ovarian tissue secreting sex steroids for regenerating ovarian endocrine function. However, we would like to expose GCs as a potential model for transdifferentiation in mammals, which is still poorly understood and makes GCs even more special and interesting for both the human and veterinary medicine.
References
Albrecht KH, Eicher EM. Evidence that Sry is expressed in pre-Sertoli cells and Sertoli and granulosa cells have a common precursor. Dev Biol. 2001;240:92–107.
Atlasi Y, Mowla SJ, Ziaee SA, et al. OCT4 spliced variants are differentially expressed in human pluripotent and nonpluripotent cells. Stem Cells. 2008;26:3068–74.
Barrero MJ, Belmonte JCI. Regenerating the epigenome. EMBO Rep. 2011;12:208–15.
Bayne S, Li H, Jones ME, et al. Estrogen deficiency reversibly induces telomere shortening in mouse granulosa cells and ovarian aging in vivo. Protein Cell. 2011;2:333–46.
Boerboom D, Paguet M, Hsieh M, et al. Misregulated Wnt/beta-catenin signaling leads to ovarian granulosa cell tumor development. Cancer Res. 2005;65:9206–15.
Boyer A, Goff AK, Boerboom D. WNT signaling in ovarian follicle biology and tumorigenesis. Trends Endocrinol Metab. 2010;21:25–32.
Bukovsky A, Caudle MR. Immunoregulation of follicular renewal, selection, POF, and menopause in vivo, vs. neo-oogenesis in vitro, POF and ovarian infertility treatment, and a clinical trial. Reprod Biol Endocrinol. 2012. doi:10.1186/1477-7827-10-97.
Bukovsky A. Ovarian stem cell niche and follicular renewal in mammals. Anat Rec (Hoboken). 2011;294:1284–306.
Bukovsky A, Caudle MR, Svetlikova M. Steroid-mediated differentiation of neural/neuronal cells from epithelial ovarian precursors in vitro. Cell Cycle. 2008;7:3577–83.
Butts S, Riethman H, Ratcliffe S, et al. Correlation of telomere length and telomerase activity with occult ovarian insufficiency. J Clin Endocrinol Metab. 2009;94:4835–43.
Chen H, Wang W, Mo Y, et al. Women with high telomerase activity in luteinised granulosa cells have a higher pregnancy rate during in vitro fertilization treatment. J Assist Reprod Genet. 2011;28:797–807.
Cheng EH, Chen SU, Lee TH, et al. Evaluation of telomere length in cumulus cells as a potential biomarker of oocyte and embryo quality. Hum Reprod. 2013. doi:10.1093/humrep/det004.
Chronowska E. Regulation of telomerase activity in ovarian granulosa cells. Indian J Exp Biol. 2012;50:595–601.
Clevers H, Nusse R. Wnt/β-Catenin signaling and disease. Cell. 2012;149:1192–205.
Daniels R, Hall V, Trounson AO. Analysis of gene transcription in bovine nuclear transfer embryos reconstructed with granulosa cell nuclei. Biol Reprod. 2000;63:1034–40.
Edwards RG. Follicular fluid. J Reprod Fertil. 1974;37:189–219.
Erickson G. The graafian follicle: a functional definition. In: Adashi EY, editor. Ovulation: evolving scientific and clinical concepts. New York: Springer; 2000. p. 31–48.
Fan HY, O’Connor A, Shitanaka M, et al. β-Catenin (CTNNB1) promotes preovulatory follicular development but represses LH-mediated ovulation and luteinization. Mol Endocrinol. 2010;24:1529–42.
Flores I, Canela A, Vera E, et al. The longest telomeres: a general signature of adult stem cell compartments. Genes Dev. 2008;22:654–67.
Glister C, Kemp CF, Knight PG. Bone morphogenetic protein (BMP) ligands and receptors in bovine ovarian follicle cells: actions of BMP-4, -6 and -7 on granulosa cells and differential modulation of Smad-1 phosphorylation by follistatin. Reproduction. 2002;127:239–54.
Gong SP, Lee ST, Lee EJ, et al. Embryonic stem cell-like cells established by culture of adult ovarian cells in mice. Fertil Steril. 2010;93:2594–601.
Grunwald K, Feldmann K, Melsheimer P, et al. Aneuploidy in human granulosa lutein cells obtained from gonadotrophin-stimulated follicles and its relation to intrafollicular hormone concentrations. Hum Reprod. 1998;10:2679–87.
Håkelien AM, Landsverk HB, Robl JM, et al. Reprogramming fibroblasts to express T-cell functions using cell extracts. Nature. 2002;20:460–6.
Hanson JA, Ambaye AB. Adult testicular granulosa cell tumor: a review of the literature for clinopathologic predictors of malignancy. Arch Pathol Lab Med. 2011;135:143–6.
Heng BC, Cao T, Bested SM, et al. “Waste” follicular aspirate from fertility treatment – a potential source of human germline stem cells? Stem Cells Dev. 2005;14:11–4.
Hirshfield AN. Patterns of [3H] thymidine incorporation differ in immature rats and mature, cycling rats. Biol Reprod. 1986;34:229–35.
Hiyama E, Hiyama K. Telomere and telomerase in stem cells. Brit J Cancer. 2007;96:1020–4.
Hoffmeyer K, Raggioli A, Rudloff S, et al. Wnt/β-Catenin signaling regulates telomerase in stem cells and cancer cells. Science. 2012;336:1549–54.
Honda A, Hirose M, Hara K, et al. Isolation, characterization, and in vitro and in vivo differentiation of putative thecal stem cells. Proc Natl Acad Sci USA. 2007;104:12389–94.
Iijima Y, Nagai T, Mizukami M, et al. Beating is necessary for transdifferentiation of skeletal muscle-derived cells into cardiomyocytes. FASEB J. 2003;17:1361–3.
Jamieson S, Fuller PJ. Molecular pathogenesis of granulosa cell tumors of the ovary. Endocr Rev. 2012;33:109–44.
Jopling C, Boue S, Izpisua Belmonte JC. Dedifferentiation, transdifferentiation and reprogramming: three routes to regeneration. Nat Rev Mol Cell Biol. 2011;12:79–89.
Kaleli S, Yanikkaya-Demirel G, Erel CT, et al. High rate of aneuploidy in luteinized granulosa cells obtained from follicular fluid in women who underwent controlled ovarian hyperstimulation. Fertil Steril. 2005;84:802–4.
Karuputhula NB, Chattopadhyay R, Chakravarty B, et al. Oxidative status in granulosa cells of infertile women undergoing IVF. Syst Biol Reprod Med. 2013;59:91–8.
Kinugawa C, Murakami T, Okamura K, et al. Telomerase activity in normal ovaries and premature ovarian failure. Tohoku J Exp Med. 2000;190:231–8.
Kléber M, Sommer L. Wnt signaling and the regulation of stem cell function. Curr Opin Cell Biol. 2004;16:681–7.
Knight PG, Muttukrishna S, Groome NP. Development and application of a two-site enzyme immunoassay for the determination of “total” activin-A concentrations in serum and follicular fluid. J Endocrinol. 1996;148:267–79.
Komori T. Regulation of osteoblast differentiation by Runx2. Adv Exp Med Biol. 2010;658:43–9.
Kossowska-Tomaszczuk K, De Geyter C. Cells with stem cell characteristics in somatic compartments of the ovary. Biomed Res Int. 2013. doi:10.1155/2013/310859.
Kossowska-Tomaszczuk K, Pelezar P, Güven S, et al. A novel three-dimensional culture system allows prolonged culture of functional human granulosa cells and mimics the ovarian environment. Tissue Eng A. 2010;16:2063–73.
Kossowska-Tomaszczuk K, De Geyter C, De Geyter M, et al. The multipotency of luteinizing granulosa cells collected from mature ovarian follicles. Stem Cells. 2009;27:210–9.
Lavranos TC, Mathis JM, Latham SE, et al. Evidence for ovarian granulosa stem cells: telomerase activity and localization of the telomerase ribonucleic acid component in bovine ovarian follicles. Biol Reprod. 1999;61:358–66.
Lee HW, Blasco MA, Gottlieb GJ, et al. Essential role of mouse telomerase in highly proliferative organs. Nature. 1998;392:569–74.
Lima JF, Jin L, de Araujo AR, et al. FOXL2 mutations in granulosa cell tumors occurring in males. Arch Pathol Lab Med. 2012;136:825–8.
Liu S, Wang Y, Wang L, et al. Transdifferentiation of fibroblasts into adipocyte-like cells by chicken adipogenic transcription factors. Comp Biochem Physiol A Mol Integr Physiol. 2010;156:502–8.
Luu HH, Song W, Luo X, et al. Distinct role of bone morphogenetic proteins in osteogenic differentiation of mesenchymal stem cells. J Orthop Res. 2007;25:665–77.
Mattioli M, Gloria A, Turriani M, et al. Osteo-regenerative potential of ovarian granulosa cells: an in vitro and in vivo study. Theriogenology. 2012;77:1425–37.
Misselevich I, Boss JH. Metaplastic bone in a mucinous cystadenoma of the ovary. Pathol Res Pract. 2000;196:847–8.
Monti M, Redi C. Oogenesis specific genes (Nobox, Oct4, Bmp15, Gdf9, Oogenesin1 and Oogenesin2) are differentially expressed during natural and gonadotropin-induced mouse follicular development. Mol Reprod Dev. 2009;76:994–1003.
Mooney EE, Vaidya KP, Tavassoli FA. Ossifying well-differentiated Sertoli-Leydig cell tumor of the ovary. Ann Diagn Pathol. 2000;4:34–8.
Mora JM, Fenwick MA, Castle L, et al. Characterization and significance of adhesion and junction-related proteins in mouse ovarian follicles. Biol Reprod. 2012;86:1–14.
Morizane M, Ohara N, Mori T, et al. Ossifying luteinized thecoma of the ovary. Arch Gynecol Obstet. 2003;267:167–9.
Morrison SJ, Prowse KR, Ho P, et al. Telomerase activity in hematopoietic cells is associated with self-renewal potential. Immunity. 1996;5:207–16.
Mukonoweshuro P, Oriowolo A. Stromal osseous metaplasia in a low-grade ovarian adenocarcinoma. Gynecol Oncol. 2005;99:222–4.
Nguyen T, Lee S, Hatzirodos N, et al. Spatial differences within the membrana granulosa in the expression of focimatrix and steroidogenic capacity. Mol Cell Endocrinol. 2012;363:62–73.
Okada TS. Transdifferentiation: flexibility in cell differentiation. Oxford: Oxford University Press; 1991.
Oki Y, Ono H, Motohashi T, et al. Dedifferentiated follicular granulosa cells derived from pig ovary can transdifferentiate into osteoblasts. Biochem J. 2012;447:239–48.
Otsuka F, Shimasaki S. A negative feedback system between oocyte bone morphogenetic protein 15 and granulosa cell kit ligand: Its role in regulating granulosa cell mitosis. Proc Natl Acad Sci USA. 2002;99:8060–5.
Pandey A, Gupta SC, Gupta N, et al. Comparative potential of cultured skin fibroblast, cumulus, and granulosa cell to produce somatic cell nuclear transfer (SCNT) preimplantation embryos in buffaloes (Bubalus bubalis) in relation to gene expressions. Cell Reprogram. 2010;12:357–68.
Park ES, Park J, Franceschi RT, Jo M. The role for runt related transcription factor 2 (RUNX2) as a transcriptional repressor in luteinizing granulosa cells. Mol Cell Endocrinol. 2012;362:165–75.
Parte S, Bhartiya D, Telang J, et al. Detection, characterization, and spontaneous differentiation in vitro of very small embryonic-like putative stem cells in adult mammalian ovary. Stem Cells Dev. 2011;20:1451–64.
Perán M, Marchal JA, Rodríguez-Serrano F, et al. Transdifferentiation: why and how? Cell Biol Int. 2011;35:373–9.
Red-Horse K, Ueno H, Weissman I, et al. Coronary arteries form by developmental reprogramming of venous cells. Nature. 2010;464:549–53.
Rodgers RJ, Irving-Rodgers HF, van Wezel IL, et al. Dynamics of the membrana granulosa during expansion of the ovarian follicular antrum. Mol Cell Endocrinol. 2001;171:41–8.
Silva JC R e, Andrade D, Becker AP, et al. Isolated osseous ovarian metaplasia: case report. Eur J Gynaecol Oncol. 2010;31:469–70.
Russo V, Berardinelli P, Martelli A, et al. Expression of telomerase reverse transcriptase subunit (TERT) and telomere sizing in pig ovarian follicles. J Histochem Cytochem. 2006;54:443–55.
Schmidt D, Ovitt CE, Anlag K, et al. The murine winged-helix transcription factor Foxl2 is required for granulosa cell differentiation and ovary maintenance. Development. 2004;131:933–42.
Shukla AR, Huff DS, Canning DA, et al. Juvenile granulosa cell tumor of the testis: contemporary clinical management and pathological diagnosis. J Urol. 2004;171:1900–2.
Sittadjody S, Saul JM, Joo S, et al. Engineered multilayer ovarian tissue that secretes sex steroids and peptide hormones in response to gonadotropins. Biomaterials. 2012;34:2412–20.
Stand M, Micchelli CA. Quiescent gastric stem cells maintain the adult Drosophila stomach. Proc Natl Acad Sci USA. 2011;108:17696–701.
Su YQ, Sugiura K, Eppig JJ. Mouse oocyte control of granulosa cell development and function: paracrine regulation of cumulus cell metabolism. Semin Reprod Med. 2009;27:32–42.
Sugimoto K, Gordon SP, Meyerowitz EM. Regeneration in plants and animals: dedifferentiation, transdifferentiation, or just differentiation? Trends Cell Biol. 2011;21:212–8.
Tian XC, Kubota C, Enright B, et al. Cloning animals by somatic cell nuclear transfer – biological factors. Reprod Biol Endocrinol. 2003. doi:10.1186/1477-7827-1-98.
Tománek M, Chronowska E, Kott T, et al. Telomerase activity in pig granulosa cells proliferating and differentiating in vitro. Anim Reprod Sci. 2008;104:284–98.
Tsonis PA, Madhavan M, Tancous EE, et al. A newt’s eye view of lens regeneration. Int J Dev Biol. 2004;48:975–80.
Uhlenhaut NH, Jakob S, Anlag K, et al. Somatic sex reprogramming of adult ovaries to testes by FOXL2 ablation. Cell. 2009;139:1130–42.
Varras M, Griva T, Kalles V, et al. Markers of stem cells in human ovarian granulosa cells: is there a clinical significance in ART? J Ovarian Res. 2012. doi:10.1186/1757-2215-5-36.
Virant-Klun I, Zech N, Rozman P, et al. Putative stem cells with an embryonic character isolated from the ovarian surface epithelium of women with no naturally present follicles and oocytes. Differentiation. 2008;76:843–56.
Virant-Klun I, Rozman P, Cvjeticanin B, et al. Parthenogenetic embryo-like structures in the human ovarian surface epithelium cell culture in postmenopausal women with no naturally present follicles and oocytes. Stem Cells Dev. 2009;18:137–49.
Virant-Klun I, Skutella T, Stimpfel M, et al. Ovarian surface epithelium in patients with severe ovarian infertility: a potential source of cells expressing markers of pluripotent/multipotent stem cells. J Biomed Biotechnol. 2011. doi:10.1155/2011/381928.
Wang HX, Li TY, Kidder GM. WNT2 regulates DNA synthesis in mouse granulosa cells through beta-catenin. Biol Reprod. 2010;82:865–75.
Wells DN, Misica PM, Tervit HR. Production of cloned calves following nuclear transfer with cultured adult mural granulosa cells. Biol Reprod. 1999;60:996–1005.
Yamagata Y, Nakamura Y, Umayahara K, et al. Changes in telomerase activity in experimentally induced atretic follicles of immature rats. Endocr J. 2002;49:589–95.
Yang L, Li S, Hatch H, et al. In vitro trans-differentiation of adult hepatic stem cells into pancreatic endocrine hormone-producing cells. Proc Natl Acad Sci USA. 2002;99:8078–83.
Yong EL, Baird DT, Yates R, et al. Hormonal regulation of the growth and steroidogenic function of human granulosa cells. J Clin Endocrinol Metab. 1992;74:842–9.
Zhang X, Yang M, Lin L, et al. Runx2 overexpression enhances osteoblastic differentiation and mineralization in adipose-derived stem cells in vitro and in vivo. Calcif Tissue Int. 2006;79:169–78.
Zuccotti M, Merico V, Belli M, et al. OCT4 and the acquisition of oocyte developmental competence during folliculogenesis. Int J Dev Biol. 2012;56:853–8.
Conflict of interest
The authors indicate no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dzafic, E., Stimpfel, M. & Virant-Klun, I. Plasticity of granulosa cells: on the crossroad of stemness and transdifferentiation potential. J Assist Reprod Genet 30, 1255–1261 (2013). https://doi.org/10.1007/s10815-013-0068-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-013-0068-0