Abstract
Purpose
To compare two different embryo culture methods and to determine whether grouping embryos based on quality following Day 3 improved outcomes.
Methods
Two group embryo culture methods were compared in this study. All zygotes were individually cultured from Day 1 to Day 3. On Day 3, embryos were then cultured in group of 2–5 embryos per droplet until Day 5 or 6. The two group culture methods are: A, embryos were randomly grouped regardless of embryo quality; B, good and poor quality embryos were separately grouped. Blastocyst development rate, blastocyst utilization rate, implantation rate and pregnancy rate were detected.
Results
The group culture of Day 3 embryos, in which good or poor quality embryos were separately grouped, significantly promoted blastocyst development (61.2 %, 289/472) and blastocyst utilization rate (55.9 %, 264/472) in comparison with those embryos that were randomly grouped for culture regardless of embryo quality (44 %, 177/402 and 41.5 %, 167/402). There was no significant difference in the implantation rate and pregnancy rate between two group culture methods.
Conclusions
Grouping of embryos after Day 3 based on embryo quality may benefit blastocyst formation. This may be due to secretion of beneficial factors by good embryos, or removal of detrimental factors from poor embryos. No impacts on pregnancy or implantation outcomes were observed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blastocyst culture and transfer have emerged as important components in human IVF. While the culture of embryos to blastocyst stage for subsequent transfer yields high pregnancy rates and minimizes the risk of multiple gestations, the availability of blastocysts is limited in many IVF clinics because of the high rates of attrition in in-vitro embryo culture [1–3]. Sub-optimal culture conditions can compromise many aspects of embryo development [4]. Therefore, the challenge for many scientists has been to optimize culture conditions so that more human embryos can develop into viable blastocysts.
In recent years, blastocyst development has been improved by a number of ways, such as co-culture of embryos with autologous or heterologous adult somatic cells, or established cell lines [5, 6], use of defined, serum-free, sequential culture media [7–10], use of reduced volumes of culture medium [11, 12], and culture of embryos in group [13–16].
It is hypothesized that one reason for benefit of group embryo culture is embryo modification of their microenvironment due to secretion and/or depletion of various factors in the media [17–21]. However, some other factors derived from poor quality embryos may have negative influences on the development of surrounding embryo. Different quality of companion embryos may differentially secrete or utilize substances into/from the culture medium. Therefore, there may be a benefit of grouping embryos separately for culture according to their quality. It has been reported that in vitro development of solitary cat embryos is improved by culture with excellent-quality heterospecific companions [22, 23].
Recently, Rebollar-Lazaro and Matson (2010) reported that culturing embryos in groups from Day 1 to Day 3 had no impact on pregnancy and implantation rates compared to those embryos cultured individually [24]. This is similar to a previous report that indicated no benefit of group culture of human embryos prior to Day 2 or Day 3 transfer [25]. In addition, in some cases, the group culture of embryos to blastocyst stage is not always practical because not all patients are blastocyst culture candidates. Therefore, the ability to individually track embryos in these non-blastocyst transfer cases is useful for selection purposes.
The objective of this study was to compare two different embryo culture methods and to determine whether grouping embryos based on quality following Day 3 improved outcomes.
Materials and methods
Patients and stimulation
The study was approved by the local Ethics Review Committee. Data were obtained from 78 patients undergoing IVF (37 cases) and ICSI (41 cases) at the Conceptia Clinic at Moncton, New Brunswick, Canada. They were referred to our clinic with a history of more than 1 year infertility. Patients had the following primary etiologies for their infertility: Male factor, tubal factor, unexplained, endometriosis, anovulation and the polycystic ovary syndrome. Ovarian stimulation was performed with a GnRH analog (Suprefact, Sanofi-Aventis) down regulation utilizing our long or micro-flare protocols with recombinant FSH (Gonal F, EMD Serono or Puregon, Merck) and LH (Luveris, EMD Serono) or human menopausal gonadotrophin (Menopur or Bravelle, Ferring), dose adjusted according to body mass index. During the ovarian stimulation regimen, the patients underwent transvaginal ultrasonographic evaluation of endometrial thickness and measurement of follicular number and size. Ovulation was induced with recombinant HCG (Ovidrel, EMD Serono) when 3 or more follicles were at least 18 mm in their greatest diameter.
Oocyte retrieval and in vitro fertilization
All oocyte retrievals were done by transvaginal aspiration under ultrasound guidance 36–37 h after hCG administration. The medium used for flushing the follicles is G-MOPS (Vitrolife). After retrieval, oocytes were rapidly isolated from follicular fluid, rinsed, and placed in G-IVF medium (Vitrolife). Oocytes were inseminated 3–5 h later either by classical IVF with a mean concentration of 200 000 motile spermatozoa per ml or by ICSI. Spermatozoa for IVF and ICSI were prepared with the swim-up technique and density gradient centrifugation method according to our standard protocols, respectively. For ICSI cases, cumulus cells were first removed by hyaluronidase (Vitrolife) and mechanical treatments. ICSI was performed as described by Palermo et al. [26]. Single motile spermatozoan of the best available morphologic appearance was injected into each mature oocyte. Care was taken to inject as little extra media volume (2 to 3 pL) as possible.
Day 3 embryo classification
The occurrence of fertilization was determined 16–19 h after insemination. Oocytes with two pronuclei were individually placed in 20 μl droplets of G1-V5 medium (Vitrolife) under Ovoil for culture. Incubation was performed at 37 °C, in a humidified atmosphere containing 6 % CO2, 5 % O2 and 89 % N2 for 48 h. On day 2, embryos were examined for cell stage, fragmentation and multinucleation. Embryos were classified on Day 3 into four categories as follows: grade (G) 1: embryos (≥ 8-cells) have even, regular, spherical blastomeres with no or < 5 % fragmentation. G 2: embryos (≥ 6-cells) have regular, spherical blastomeres, with < 15 % fragmentation. G 3: embryos (≥ 4-cells) have uneven shaped blastomeres, with < 40 % fragmentation. G 4: embryos (< 4-cells) have unequal, dark blastomeres, with > 15 % fragmentation or the number of blastomeres is more than 4-cells, with unequal, dark blastomeres and > 40 % fragmentation. Grade1 and Grade 2 were considered as good quality, Grade 3 and 4 were considered as poor quality.
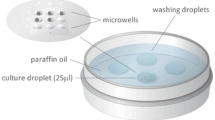
Embryo group culture strategies
On Day 3, patients who had 4 or more good quality of cleavage embryos were invited to have the embryos cultured to blastocyst stage for transfer. Embryos were then cultured in group of 2–5 embryos per droplet (50 μl G2-V5) until Day 5 or 6. The group culture strategy is: A, embryos were randomly grouped regardless of embryo quality; B, good and poor quality embryos were separately grouped. All embryos with multiple nuclei or from abnormal fertilization were cultured separately or discarded. Patient cycles with less than 4 good quality embryos or with no poor quality embryos on Day 3 were eliminated in this study.
Blastocyst classification and transfer
On the morning of Day 5, blastocyst formation was determined and each blastocyst was graded by using the system of Gardner and Schoolcraft [27]. Briefly, blastocysts were given an alphanumeric score from 1 to 6, based on their degree of expansion, hatching status, as follows: 1, early blastocyst, the blastocoel being less than half the volume of the embryo; 2, blastocyst, the blastocoel being half or greater than half of the volume of the embryo; 3, full blastocyst, the blastocoel completely fill the embryos; 4, expanded blastocyst, the blastocoel volume is larger than that of the early embryo and the zona is thinner than before; 5, hatching blastocyst, the trophectoderm has started to herniate through the zona; 6, hatched Blastocyst, the blastocyst has completely escaped from the zona.
The development of the inner cell mass (ICM) was graded as follows: A, tightly packed, many cells; B, loosely grouped, several cells; or C, very few cells. The trophectoderm was assessed as follows: A, many cells forming a cohesive epithelium; B, few cells forming a loose epithelium; or C, very few large cells.
By using this scoring system, maximum of two blastocysts were transferred to patient on Day 5. Those that did not reached the blastocyst stage on Day 5 were cultured one more day till Day 6. The criterion for cryopreservation of blastocysts was that blastocysts with a score of ≥ 3BB at Days 5 or 6 according to Gardner et al. [28]. Blastocysts displaying ICM and/or trophectoderm with very few cells (score as C) were considered as unusable embryos and discarded.
Transfer was performed by using G2-V5 medium, Wallace catheter and ultrasonographic guidance. The chemical pregnancies were defined as a positive pregnancy test result on luteal day 12 with a rising titer confirmed by a second hCG measurement. The clinical pregnancies were diagnosed by ultrasonographic evidence of embryonic heart activity. Statistical analysis was done by using chi-square test.
Results
General observations
A total of 1243 oocytes were collected from 78 patients. 874 of them were fertilized by IVF or ICSI. The fertilization rate was 70.3 %. The percentages of good and poor quality cleavage embryos on Day 3 were, respectively, 76.7 % (670/874) and 23.3 % (204/874). Eighteen cases were eliminated because they had no poor quality embryos on Day 3. There were poor quality embryos on Day 3 in every case. The high percentage of good quality cleavage embryos on Day 3 might be due to a quality culture system in this study.
Comparison of blastocyst development and pregnancy between two methods
Outcome of blastocyst development and pregnancy in two groups were summarized in Table 1. The blastocyst rate in group B (61.2 %) (Good and poor quality embryos were separately grouped) were significantly higher than that in group A (44 %) (Embryos were randomly grouped regardless of embryo quality). There was no statistical difference between two groups in the implantation rate and clinical pregnancy rate.
Effect of group culture methods on blastocyst utilization rates
Blastocyst utilization rates from two different group culture strategies were compared in Table 2. The blastocyst utilization rate was calculated as the number of blastocysts suitable for freezing and transfer/total number of 2 PN embryos cultured to Day 5 and 6. The rates of blastocyst utilization and cryopreservation in group B (55.9 % and 39.2 %, respectively) were significantly higher than those in group A (41.5 % and 25.1 %, respectively). The average number of blastocysts cryopreserved per patient in group B (4.5) was also significantly greater compared with that in group A (2.7).
Quality of blastocysts transferred on Day 5 in both group culture methods
Patients were assigned to one of three situations according to the quality of their blastocysts transferred on Day 5 in both group culture methods. Maximum of two blastocysts were transferred per patient. Patients in situation 1 had two top-scoring blastocysts for transfer (≥ 3AA). Patients in situation 2 had one top-scoring blastocyst (≥ 3AA) with or without one blastocyst (< 3AA) for transfer. Patients in situation 3 did not have a top-scoring blastocyst for transfer. There were no significant differences in the top-scoring blastocyst (transferred) rate and the distribution of top-scoring blastocysts in three transfer situations between two group culture methods (Table 3). Six patients in situation 2 (3 from method A, 3 from method B) were selected for doing single embryo transfer.
Discussion
All the procedures taking place in an embryology laboratory are the elements of great importance influencing the efficacy of human assisted reproductive technology. Proper embryo culture strategy is one of the major factors of a successful IVF program. Recently group culture of embryos to blastocyst stage has been beneficially applied in mice [29, 30], sheep [31], cow [32–34] and human [35, 36].
It has been reported that group culture may promote embryo development vie secretion of embryotrophic factors [14, 37, 38], and embryos cultured in group developed better than those cultured individually [39–41]. However, opponents of the approach argue that embryos in group may either deplete the media of substrates or negatively affect nearby embryos via the transmission of other secreted factors. The blastocyst development rate in mouse embryos is promoted by an increase of embryo density in culture drops [20, 39], which suggests that specific factors are secreted from the embryos to influence embryo growth in an autocrine or paracrine manner. However, some other factors derived from poor quality embryos may have negative influences on the surrounding embryo development. It has been reported that the accumulation of toxic substances such as ammonia and oxygen-derived free radicals in the culture medium [42–44] may lead to the late developmental anomalies.
Assessing pronuclear morphology at Day 1 [45, 46] and detecting the presence of multinucleated blastomeres at Day 2 [47, 48] have proven to be useful for the prediction of embryo development potential. In addition, the group culture of embryos to blastocyst stage in humans is not always possible due to the small number of available oocytes at retrieval or the poor quality of embryos on Day 3. Therefore, individual culture and tracking of embryos from Day 1 to Day 3 is preferable because it is able to correlate the embryo morphologic features or cleavage speed evaluated at Day 1 or 2 with the evaluation at Day 3, and with the benefits for selection of embryos to be transferred at Day 3 when there are not enough good quality of Day 3 embryos available for blastocyst culture.
The theoretical reasons and practical evidences of the benefit of group culture to blastocyst stage in the literature as mentioned earlier had prompted the present study to investigate the combination of single culture to Day 3 and group culture to Day 5 or 6 in an attempt to obtain the best of both culture strategies.
It is without question that embryos can modify their surrounding environment by creating localized zones of secreted and depleted factors. Whether these modifications of the local environment are beneficial or detrimental is not clear. The hypothesis generated in this study is that in addition to the positive effects, human embryo development in group culture may also be harmfully affected by negative factors that derived from poor quality of embryos. In this study, the culture of Day 3 embryos, in which good and poor quality embryos were separately grouped, significantly promoted both blastocyst development and blastocyst utilization rate in comparison with those embryos that were randomly grouped regardless of embryo quality. Even though there was no significant difference in the implantation rate and the pregnancy rate between two group culture methods, with the strategy that good and poor quality embryos be separately grouped for culture, the IVF program and patient may be benefited by improving the overall embryo quality, by increasing the number of good blastocysts cryopreserved and by increasing cumulative pregnancy rates with frozen-thawed blastocyst transfer. The reason why there were no significant differences in the implantation and pregnancy rates might be that both group culture methods had similar distribution of top-scoring blastocyst rates in all their three transfer situations.
Our results also raise the question of whether quality of the entire cohort is intrinsic due to the shared origins of the embryos, or if it is merely a result of group culture in vitro. The further study is needed to find out the differences in embryo phenotypes or embryo derived factors between good and poor quality embryos [49], and their effects on embryo development. If the benefit of group culture is the paracrine effect of embryonic factors which are secreted from good quality embryos, identification and addition of these factors to culture media may permit individual embryo culture to perform similarly to the group embryo culture.
Various factors that affect blastocyst formation and quality could not be controlled in one study. This study focused on the group embryo culture methods. However, in efforts to sweep generalizations, many other factors need to be evaluated that potentially impact outcomes. These include fertilization procedures (IVF or ICSI), stimulation protocols, number of oocytes, causes of infertility, embryo density, embryo spacing and type of culture media.
In conclusion, our findings indicate that grouping of embryos after Day 3 based on embryo quality may benefit blastocyst formation. This may be due to secretion of beneficial factors by good embryos, or removal of detrimental factors from poor embryos. The strategy of the combination of individual culture to Day 3 and good and poor quality of embryos be separately grouped for culture to Day 5 or 6 is recommended for clinical use.
References
Gardner DK, Lane M, Schoolcraft WB. Culture and transfer of viable blastocysts: a feasible proposition for human IVF. Hum Reprod. 2000;15:9–23.
Milki AA, Hinckley MD, Fisch JD, Dasig D, Behr B. Comparison of blastocyst transfer with day 3 embryo transfer in similar patient populations. Fertil Steril. 2000;73:126–9.
Dobson AT, Raja R, Abeyta MJ, Taylor T, Shen S, et al. Unique transcription through day 3 of human preimplantation development. Hum Mol Genet. 2004;13:1461–70.
Lane M, Gardner DK. Amino acids and vitamins prevent culture-induced metabolic perturbations and associated loss of viability of mouse blastocysts. Hum Reprod. 1998;13:991–7.
Menezo Y, Hazout A, Dumont M, Herbaut N, Nicollet B. Coculture of embryos on Vero cells and transfer of blastocysts in humans. Hum Reprod. 1992;1:101–6.
Quinn P, Margalit R. Beneficial effects of coculture with cumulus cells on blastocyst formation in a prospective trial with supernumerary human embryos. J Assist Reprod Genet. 1996;13:9–14.
Martin KL, Leese HJ. Role of glucose in mouse preimplantation embryo development. Mol Reprod Dev. 1995;40:436–43.
Gardner DK. Changes in requirements and utilization of nutrients during mammalian preimplantation embryo development and their significance in embryo culture. Theriogenology. 1998;49:83–102.
Gardner DK, Lane M, Calderon I, Leeton J. Environment of the preimplantation human embryo in vivo: metabolite analysis of oviduct and uterine fluids and metabolism of cumulus cells. Fertil Steril. 1996;65:349–53.
Wiemer WE, Anderson AR, Kyslinger ML, Weikert ML. Embryonic development and pregnancies following sequential culture in human tubal fluid and a modified simplex optimised medium containing amino acids. Reprod Biomed Online. 2002;5:323–7.
Canseco RS, Sparks AE, Person RE, Gwaszdauskas FC. Embryo density and medium volume effects on early murine embryo development. J Assist Reprod Genet. 1992;9:454–7.
Hoelker M, Rings F, Lund Q, Ghanem N, Phatsara C, Griese J, et al. Effect of the microenvironment and embryo density on developmental characteristics and gene expression profile of bovine preimplantative embryos cultured in vitro. Reproduction. 2009;137:415–25.
Rijnders PM, Jansen CAM. Influence of group culture and culture volume on the formation of human blastocysts: a prospective randomized study. Hum Reprod. 1999;14:2333–7.
Fujita T, Umeki H, Shimura H, Kugumiya K, Shiga K. Effect of group culture and embryo-culture conditioned medium on development of bovine embryos. J Reprod Dev. 2006;52:137–42.
Almagor M, Bejar C, Kafka I, Yaffe H. Pregnancy rates after communal growth of preimplantation human embryos in vitro. Fertil Steril. 1996;66(3):394–7.
Moessner J, Dodson WC. The quality of human embryo growth is improved when embryos are cultured in groups rather than separately. Fertil Steril. 1995;64(5):1034–5.
Hardy K, Spanos S. Growth factor expression and function in the human and mouse preimplantation embryo. J Endocrionol. 2002;172:221–36.
O’Neil C. Evidence for the requirement of autocrine growth factors for development of mouse preimplantation embryos in vitro. Biol Reprod. 1997;56:229–37.
Richter KS. The importance of growth factors preimplantation embryo development and in vitro culture. Curr Opin Obstet Gynecol. 2008;20:292–304.
Paria BC, Dey SK. Preimplantation embryo development in vitro: cooperative interactions among embryos and role of growth factors. Proc Natl Acad Sci USA. 1990;87:4756–60.
Reed ML, Woodward BJ, Swain JE. Single or group culture of mammalian embryos: the verdict of the literature. J Reprod Stem Cell Biotechnol. 2011;2:77–87.
Spindler RE, Crichton EG, Agca Y, Loskutoff N, Critser J, Gardner DK, et al. Improved felid embryo development by group culture is maintained with heterospecific companions. Theriogenology. 2006;66(1):82–92.
Spindler RE, Wildt DE. Quality and age of companion felid embryos modulate enhanced development by group culture. Biol Reprod. 2002;66(1):167–73.
Rebollar-Lazaro I, Matson P. The culture of human cleavage stage embryos alone or in groups: effect upon blastocyst utilization rates and implantation. Reprod Biol. 2010;10(3):227–34.
Spyropoulou I, Karamalego C, Bolton VN. A prospective randomized study comparing the outcome of in-vitro fertilization and embryo transfer following culture of human embryos individually or in groups before embryo transfer on day 2. Hum Reprod. 1999;14(1):76–9.
Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermtozoon into an oocyte. Lancet. 1992;340:17–8.
Gardner DK, Schoolcraft WB. In vitro culture of human blastocyst. In: Jansen R, Mortimer D, editors. Towards reproductive certainty: infertility and genetics beyond 1999. Carnforth: Parthenon Press; 1999. p. 378–88.
Gardner DK, Lane M. Embryo culture system. In: Trounson AO, Gardner DK, editors. Handbook of in vitro fertilization. 2nd ed. Boca Raton: CRC Press; 2000. p. 205–64.
Lana M, Gardnar DK. Effect of incubation volume and embryo density on the development and viability of mouse embryos in vitro. Hum Reprod. 1992;7:558–62.
Stoddart NR, Wild AE, Fleming TP. Stimulation of development in vitro by platelet-activating factor receptor ligands released by mouse preimplantation embryos. J Reprod Fertil. 1996;108:47–53.
Gardnar DK, Lana M, Spitzer A, Batt PA. Enhanced rates of cleavaged and development for sheep zygotes cultured to the blastocyst stage in the absence serum and somatic cells: amino acids, vitamins, and culturing embryos in groups stimulate development. Biol Reprod. 1994;50:390–400.
Palma GA, Clement-Stegewald A, Berg U, Brem G. Role of the embryo number in the development of in vitro produced bovine embryos. Theriogenology. 1992;37:271.
Ferry L, Mermillod P, Massip A, Dessy F. Bovine embryo culture in serum-poor oviduct conditioned medium need cooperation to reach the blastocyst stage. Theriogenology. 1994;42:445–53.
O’Doherty EM, Wade MG, Hill JL, Boland MP. Effects of culturing bovine oocytes either sigly or in groups on development to blastocysts. Theriogenology. 1997;48:161–9.
Ebner T, Shebl O, Moser M, Mayer RB, Arzt W, Tews G. Group culture of human zygotes is superior to individual culture in terms of blastulation, implantation and life birth. Reprod Biomed Online. 2010;21:762–8.
Gardner D, Lana M. Culture systems for the human embryo. In: Textbook of assisted reproductive technologies: laboratory and clinical perspectives, 2008;219–240. Eds Gardner D, Weissman A, Howles C, Shoham Z, Third edition. Informa Healthcare, London.
Kane MT, Morgan PM, Coonan C. Peptide growth factors and preimplantation development. Hum Reprod Update. 1997;3:137–57.
Summers MC, Biggers JD. Chemically defined media and the culture of mammalian preimplantation embryos: historical perspective and current issues. Hum Reprod Update. 2003;9:557–82.
Salahuddin S, Ookutsu S, Goto K, Nakanishi Y, Nagata Y. Effects of embryo density and co-culture of unfertilized oocytes on embryonic development of in-vitro fertilized mouse embryo. Hum Reprod. 1995;10:2382–5.
Lane M, Gardner DK. Differential regulation of mouse embryo development and viability by amino acids. J Reprod Fertil. 1997;109:153–64.
Kato Y, Tsunoda Y. Effects of the culture density of mouse zygotes on the development in vitro and in vivo. Theriogenology. 1994;41:1315–22.
Gardner DK, Lana M. Amino acids and ammonium regulate mouse embryo development in culture. Biol Reprod. 1993;48:377–85.
Johnson MH, Nasr-Esfahani MH. Radical solutions and culture problem: could free oxygen radicals be responsible for the impaired development of preimplantation mammalian embryos in vitro ? BioAssays. 1994;16:31–8.
Sinclair KD, Dunne LD, Maxfield EK, Maltin CA, Young LE, Wilmut I, et al. Fetal growth and development following temporary exposure of day 3 ovine embryos to an advanced uterine environment. Reprod Fertil Dev. 1998;10:263–9.
Montag M, Van der Venl H. Evaluation of pronuclear morphology as the only selection criterion for further embryo culture and transfer: results of a prospective multicentre study. Hum Reprod. 2001;16:2384–9.
Tesarik J, Greco E. The probability of abnormal preimplantation development can be predicted by a single static observation on pronuclear stage morphology. Hum Reprod. 1999;14:1318–23.
Balakier H, Cadesky K. The frequency and developmental capability of human embryos containing multinucleated blastomeres. Hum Reprod. 1997;12:800–4.
Kligman I, Benadiva C, Alikani M, Munne S. The presence of multinucleated blastomeres in human embryos is correlated with chromosomal abnormalities. Hum Reprod. 1996;11:1492–8.
Jun SH, Choi B, Shahine L, Westphal LM, Behr B, et al. Defining human embryo phenotypes by cohort-specific prognostic factors. PLoS One. 2008;3:1–7.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Our study demonstrates that Day 3 embryos with good and poor quality may be separately grouped for culture to blastocyst stage. Some unknown factors derived from poor quality embryos (such as arrested embryos) may inhibit the surrounding embryo development. The strategy of the combination of individual culture to Day 3 and good and poor quality of embryos be separately grouped for culture to Day 5 or 6 is recommended for clinical use.
Rights and permissions
About this article
Cite this article
Tao, T., Robichaud, A., Mercier, J. et al. Influence of group embryo culture strategies on the blastocyst development and pregnancy outcome. J Assist Reprod Genet 30, 63–68 (2013). https://doi.org/10.1007/s10815-012-9892-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-012-9892-x