Abstract
Purpose
Culturing embryos in groups is a common practice in mammalian embryology. Since the introduction of different microwell dishes, it is possible to identify oocytes or embryos individually. As embryo density (embryo-to-volume ratio) may affect the development and viability of the embryos, the purpose of this study was to assess the effect of different embryo densities on embryo quality.
Methods
Data of 1337 embryos from 228 in vitro fertilization treatment cycles were retrospectively analyzed. Embryos were cultured in a 25 μl microdrop in a microwell group culture dish containing 9 microwells. Three density groups were defined: Group 1 with 2–4 (6.3–12.5 μl/embryo), Group 2 with 5–6 (4.2–5.0 μl/embryo), and Group 3 with 7–9 (2.8–3.6 μl/embryo) embryos.
Results
Proportion of good quality embryos was higher in Group 2 on both days (D2: 18.9 vs. 31.5 vs. 24.7%; p < 0.001; D3: 19.7 vs. 27.1 vs. 21.2%; p = 0.029; Group 1. vs. Group 2. vs. Group 3). Cell number on Day 3 differed between Groups 1 and 2 (6.8 ± 2.2; 7.3 ± 2.1; p = 0.004) and Groups 2 and 3 (7.3 ± 2.1 vs. 7.0 ± 2.0; p = 0.014).
Conclusions
Culturing 5–6 embryos together in a culture volume of 25 μl may benefit embryo quality. As low egg number, position, and distance of the embryos may influence embryo quality, results should be interpreted with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Providing optimal culture conditions for the embryos in an in vitro fertilization (IVF) treatment is crucial, due to its high impact on embryo development and thus on the outcome of the treatment.
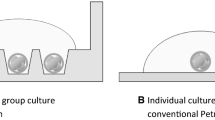
One of the variables considered by each laboratory is to culture embryos individually or in groups. The unique identification of each oocyte/embryo is possible in case of individual culture; therefore, their development can be followed individually. Embryos modify their environment via autocrine signaling; however, paracrine communication cannot take place due to the hermetic separation of the embryos from each other [1, 2]. In case of group culture embryos share the same droplet of culture medium, and are within close proximity to each other. This proximity allows embryo-to-embryo communication via paracrine signaling. Culturing embryos in a group is a prerequisite for achieving acceptable embryo quality in several mammalian species, and has also been reported to provide superior results in human, compared to individual culture [3, 4]. On the other hand, group culture may enable substances from the metabolism of the embryos to accumulate to a concentration that may have negative effects on embryo development. However, with the control of ammonium in novel culture media, this still remains hypothetical [5]. The individual identification and the possibility of autocrine and paracrine signaling between the developing embryos were first made possible with the so-called well-of-the-well (WOW) dish [6]. This type of culture dish (a manually modified four-well dish) used narrow, deep microwells to designate the place of each embryo within close distance from each other, to facilitate autocrine signaling and enable paracrine communication between sibling embryos, thus combining the beneficial effects of individual and group culture.
Another important attribute of embryo culture is the volume of media applied to support the development of the embryos with nutrients and buffer the shifts caused by the embryos’ metabolic processes. The amount of media is usually determined per embryo: embryo-to-volume ratio (or embryo density) is calculated as the volume of culture media divided by the number of embryos. The same embryo density can be achieved either by changing the number of embryos in a given volume of culture media, or by manipulating the culture volume. Choosing an appropriate density may benefit embryo development and thus can be an easy yet effective tool to improve culture conditions and maintain better embryo quality [7].
Although a large number of animal studies dealing with embryo density have been published so far [8,9,10,11,12,13], only a few papers are available on the density of human embryos cultured together in groups [7, 14, 15]. Therefore, the optimal density still remains inconclusive [16, 17], although Gardner and Lane [18] recommend using a density of 12.5 μl (a maximum of four embryos cultured together in 50 μl of media).
We hypothesized that embryo density does affect in vitro embryo quality. Accordingly, we analyzed the effect of three different embryo-to-volume ratios on embryo quality in fixed volume, using a commercially available microwell group culture dish (Primo Vision Dish, Vitrolife, Sweden; formerly discussed by Pribenszky et al. [19, 20]).
Materials and methods
This study presents a retrospective analysis of embryological data obtained from 228 in vitro fertilization (IVF) cycles, where group culture was performed at the Division of Assisted Reproduction, First Department of Obstetrics and Gynaecology, Semmelweis University, Budapest, Hungary, between September 2012 and April 2015. Every cycle was included in the study, if at least a minimum of two embryos in one dish have cleaved until Day 2. Data of an additional 180 cycles, where embryos were cultured individually, were also analyzed. These cycles were performed independently at the same time period in the same department.
Ovarian stimulation
Gonadotropin-releasing hormone (GnRH)-agonist “long protocol” or multiple-dose flexible GnRH-antagonist regimens were used for ovarian stimulation. Using the long protocol, pituitary down-regulation was achieved with the GnRH-agonist triptorelin (Gonapeptyl; Ferring, Kiel, Germany) at a dose of 0.1 mg/day from the midluteal phase of the cycle preceding the treatment cycle. In the multiple-dose flexible GnRH-antagonist protocol [21], 0.25 mg/day Cetrorelix (Cetrotide; Serono, Rome, Italy) was administered when the diameter of the leading follicle was ≥14 mm. Human menopausal gonadotropin (HMG) (Menopur, Ferring, Saint-Prex, Switzerland) or Follicle Stimulating Hormone (FSH) (Fostimon HP; IBSA, Lugano, Switzerland) was used for ovarian stimulation, which was monitored by 1–2 daily estradiol (E2) measurements and transvaginal ultrasound folliculometry. Ovulation was induced with 5000–10,000 IU of human Chorionic Gonadotropin (hCG) (Choragon; Ferring) when at least one follicle with a diameter of 18 or three or more follicles with a diameter of 16 mm were seen on ultrasound, and serum estradiol levels reached 200–300 pg/mL per ≥16 mm follicle. Transvaginal ultrasound-guided aspiration of follicles was performed 36 h after hCG administration.
In vitro fertilization and embryo culture
Following egg retrieval and collection, oocytes were incubated for 4–6 h before fertilization. Semen samples from the male partners were collected on the same day, and were analyzed 30–60 min following sampling according to the current WHO recommendation [22] and prepared with one of the following methods according to their quality. Density gradient centrifugation using SpermGrad (Vitrolife, Göteborg, Sweden) in two different concentrations (90 and 45%) were performed in most of the cases. Washing with Earl’s Balanced Salt Solution with HEPES (EBSS-H, Lonza, Verviers, Belgium) supplemented with 1% human serum albumin (HSA, Vitrolife) was performed in case of poor semen quality (cryptozoospermia).
Decision on conventional in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) was made based on the quality of the processed sperm sample, IVF history and egg count. In case of conventional IVF, swim-up method was used in order to obtain adequate sperm motility. Conventional IVF was performed in G-IVF Plus (Vitrolife) media, in 4-well petri dish (Nunc, Thermo Fisher Scientific, Waltham, MA, USA). Oocytes and zygotes were transferred into the microwell culture dishes for continued in vitro culture after fertilization check, performed at 18-h post-insemination.
In case of ICSI, cumulus cells were removed by gentle pipetting following a short enzymatic digestion using Hyaluronidase (FertiPro, Beernem, Belgium). Oocytes were injected in G-Mops Plus media (Vitrolife) and then transferred to microwell culture dishes right away, approximately 5-min post-insemination.
Embryo culture was performed in a Forma Scientific 3141 incubator (Forma Scientific; Waltham, MA, USA). Embryos were cultured in groups using a 9-microwell Primo Vision microwell group culture dish (Vitrolife) (Fig. 1). The size of a single microwell is 350 μm in diameter. The distance between the microwells is 100 μm in case of the adjacent wells, and 130 μm in case of the diagonally opposite wells. Oocytes and/or zygotes were placed together into the microwells, under a small droplet of preincubated G-1 Plus (Vitrolife) culture media with a fixed volume of 25 μl, covered by mineral oil (Ovoil, Vitrolife). If the egg count exceeded nine, oocytes were divided into two to three dishes.
Fertilized oocytes were scored for pronuclei on Day 1 at 16–18 h and for early pronuclear breakdown at 24–26-h post-insemination. Degenerated oocytes were removed after fertilization check. Number of blastomeres, fragmentation, and morphology scores on Day 2 (43–45-h post-insemination) as well as on Day 3 (67–69-h post-insemination) were recorded. Quality assessment was made according to the recommendation of international embryology societies [23]; however, our scoring system differed from that. Morphology score from 0 to 4 (higher score means better quality) was given based on stage-appropriate cell size, position and shape (Table 1). For example, a two-cell-stage embryo was considered stage appropriate if it had two equally sized blastomeres with oval shape, but a three-cell-stage embryo should have had one bigger and two smaller equally sized blastomeres as a result of cell cleaving. Degree of fragmentation was also taken into account. An embryo was defined as a GQE on Day 2 when having ≥4 blastomeres and <25% fragmentation, with no multinucleation and stage-appropriate cell sizes. On Day 3, an embryo with ≥7 blastomeres of stage-appropriate size, <25% fragmentation and no multinucleation was considered GQE. In case the patient had more normally fertilized oocytes on Day 1 than that could be transferred, embryo transfer (ET) was performed on Day 3; otherwise on Day 2. When choosing embryos for transfer with otherwise equal quality on Day 3, early cleavage and the presence of nuclei in the cells were also taken into account.
Study design
Data of 1337 (group culture) and 791 (individual culture) normally fertilized oocytes (showing two pronuclei on Day 1) were analyzed. Only cycles with at least two cleaving embryos were included in the study.
Embryo density was defined as follows: culture volume (25 μl) divided by the number of cultured embryos that have been cleaved until Day 2, regardless of whether they are normally or abnormally fertilized. Three different groups were made based on the number of embryos cultured together:
-
1.
Group 1: 2–4 embryos in one culture drop (6.3–12.5 μl/embryo),
-
2.
Group 2: 5–6 embryos in one culture drop (4.2–5 μl/embryo),
-
3.
Group 3: 7–9 embryos in one culture drop (2.8–3.6 μl/embryo).
Cell number, morphology, fragmentation, number of GQEs embryos on Days 2 and 3 were compared between groups.
For the correct interpretation of the results, we considered to perform additional investigations. As there was a difference in group culture time between the two fertilization methods, and the proportion of ICSI cycles varied between the groups, we compared morphology data between the different techniques of fertilization.
Furthermore, data of 791 embryos from 180 IVF cycles with individual culture performed during the same time period were also analyzed. Only cycles with 2–9 cleaving embryos were included, and divided into three different groups according to the following: I-Group 1: 2–4 embryos, I-Group 2: 5–6 embryos, I-Group 3: 7–9 embryos. All embryos were cultured in an individual droplet with a volume of 25 μl. Ovarian stimulation, handling of the gametes and fertilization were performed in the same way as described earlier. Embryo culture was performed in Falcon 3004 Petri dishes (Becton–Dickinson, Erembodegem, Belgium) using the above-mentioned incubator and culture media.
Statistical analysis
Statistical analyses were performed with Statistica 7 (StatSoft, USA) software. p < 0.05 was considered statistically significant. Embryological and clinical data of the different density groups was tested with analysis of variance (ANOVA). Tukey’s honest significant difference (HSD) test was performed as a post hoc test in order to distinguish between the groups. For the comparison of categorical variables, such as stimulation or fertilization method, rate of good quality embryos, Chi-squared test was used.
Results
Embryo qualities of 1337 cleavage stage embryos on Day 2 (Group 1: n = 370, Group 2: n = 486, Group 3: n = 481) and 1229 on Day 3 (Group 1: n = 269, Group 2: n = 479, Group 3: n = 481) were analyzed. The lower number of embryos on Day 3 is a result of Day 2 embryo transfers. Attributes of the different groups are presented in Table 2. Basic clinical characteristics are shown in Table 3. Statistically significant differences between the three groups occurred in the stimulation length and method, as well as in the type of the fertilization.
Morphology outcomes using different fertilization techniques are shown in Table 4. No statistically significant difference was found in Group 1. Even though the patient age was lower in case of ICSI in Group 2, blastomere number on Day 3 was higher (7.9 ± 2.2 vs. 7.1 ± 2; p < 0.001), fragmentation rate was lower on Day 2 (12.6 ± 8.4 vs. 14.8 ± 9.1; p = 0.011) and on Day 3 (12 ± 8.6 vs. 15.7 ± 10.8; p < 0.001) following conventional IVF. In Group 3, morphology score on Day 2 (2.3 ± 0.7 vs. 2.2 ± 0.7; p = 0.027) and Day 3 (2.3 ± 0.7 vs. 2.1 ± 0.6; p = 0.003), and also GQE rate on Day 3 (25.4 vs. 17.5%; p = 0.034) differed statistically significantly in favor of IVF.
Table 5 shows the proportion of zygotes with early pronuclear breakdown, while Table 6 shows embryo quality and the rate of GQEs in the different density groups on Day 2. No differences were found between the number of blastomeres; however, morphology score was lower (2.2 ± 0.7 vs. 2.3 ± 0.7; p = 0.003), and fragmentation rate was higher (16.1 ± 10.9 vs. 14.2 ± 8.9%; p = 0.009) in Group 1 than in Group 2. Rate of GQEs was higher in Group 2 than in any other groups (Groups 1 and 2: 18.9 vs. 31.5%; p < 0.001 and Groups 2 and 3: 31.5 vs. 24.7% p = 0.02), but there was also a slight difference between Groups 1 and 3 (18.9 vs. 24.7%; p = 0.043).
Day 3 embryo quality is shown in Table 7. Cell number was significantly higher in Group 2 (7.3 ± 2.1) than in Group 1 (6.8 ± 2.2; p = 0.004) and Group 3 (7.0 ± 2.0; p = 0.014). Superior average morphology score was also assessed in Group 2 (2.3 ± 0.7) compared to Group 1 (2.1 ± 0.7; p = 0.021), but did not differ from that in Group 3 (2.2 ± 0.6; p = 0.474). Slightly higher fragmentation rate was assessed in Group 2 compared to Group 3 (14.7 ± 10.4 vs. 14.2 ± 9.4%; p = 0.768), but it was significantly lower in both groups compared to Group 1 (Groups 1–2: 16.7 ± 11.5 vs. 14.7 ± 10.4; p = 0.029; Groups 1–3: 16.7 ± 11.5 vs. 14.2 ± 9.4 p = 0.005). GQE rate shows the same pattern as blastomere number. The highest rate was assessed in Group 2 (27.1%), followed by Group 3 (21.2%; p = 0.032) and Group 1 (19.7% p = 0.023).
Table 8 shows the clinical outcomes of individual culture, while the comparison of embryology data gave the following results. Number of examined embryos was 210 in I-Group 1, 254 in I-Group 2, and 327 in I-Group 3. Blastomere number on Day 2 differed significantly (p = 0.005), and was the highest in I-Group 2 (3.7 ± 1.4 vs. 4.1 ± 1.4 vs. 3.9 ± 1.4). On Day 3, there were no differences between the groups (6.3 ± 2.4 vs. 6.6 ± 2.4 vs. 6.5 ± 2.3; p = 0.566). Degree of fragmentation did not show any statistically significant difference on Day 2 (16 ± 11.7 vs. 16 ± 10.5 vs. 14.4 ± 10.5%; p = 0.129), but did on Day 3, with the lowest rate in I-Group 3 (17.9 ± 12.5 vs. 16.3 ± 11.7 vs. 14.5 ± 10.6% p = 0.023). Morphology score on Day 2 was significantly higher in I-Group 3 compared to I-Group 2 (2.1 ± 0.8 vs. 2.2 ± 0.9; p = 0.037), and was significantly lower in I-Group 1 than in I-Group 3 (2.0 ± 0.9 vs. 2.2 ± 0.8; p = 0.037) on Day 3. GQE rate was also similar on Day 2 (21.4 vs. 23.6 vs. 29.7%; p = 0.071) and on Day 3 (20.2 vs. 19.8 vs. 22.8%; p = 0.660). Figure 2 presents visualization of the study group outcomes in relation to the individual culture groups. The differences between the group and single-culture outcomes are the result of the efficiency of the different culture methods.
Discussion
Proper culture conditions can result in superior embryo viability. Embryo density during group culture can also affect embryo quality. In this study, we found that culturing 5–6 embryos in a volume of 25 μl (4.1–5.0 μl/embryo) resulted in an increased average blastomere number, and the highest GQE rate. Other quality parameters such as the amount of fragmentation or the morphology score also varied between the distinct groups. These differences were statistically significant between the less (6.3–12.5 μl/embryo) and the moderately dense group (Groups 1 and 2) in many instances.
As the group culture time is longer in cycles with ICSI, compared to the ones with conventional IVF, the unequal rate of ICSI between the groups has to be taken into consideration. Improved embryo quality has been found in the moderate- and high-density groups following conventional IVF; consequently, lower rate of ICSI in the higher density groups may indicate better embryo quality. However, this was not the case. According to our findings, a moderate density (5–6 embryos/25 μl) seems to have a beneficial effect on embryo quality, but the following limitations have to be taken into consideration. Degenerated oocytes were removed as soon as detected, but embryos with a low blastomere number might also have an adverse effect on better quality embryos [24, 25], although Larson and Kubish [26] have confuted this. However, some authors suppose that better quality embryos may promote the development of other embryos in the vicinity [25]. Unfertilized oocytes were not removed, even though Salahuddin et al. [9] have found a negative impact on embryo development of these oocytes in the mouse; however, they compared single-cultured zygotes and zygotes co-cultured with unfertilized ova. We could not consider the relative position of each embryo and the distance between them either, albeit these can also influence the development of the embryos [4, 7, 27,28,29]. Due to the study design, the effect of low egg count could not be eliminated. We were unable to compare pregnancy rates or clinical outcomes due to the study design. However, data of the literature [30,31,32] suggest that the impaired embryo quality in the low-density group (Group 1) is a result of the low number of oocytes collected, rather than a consequence of embryo density.
The association between oocyte number and embryo quality, which is known already, could also influence treatment outcomes. Ji et al. [32] found that the live birth rate (LBR) after fresh transfer in case of young patients was maximal in groups with 6–15 oocytes, and reduced in the groups with 1–5 or over 15 eggs. The cumulative LBR per initiated cycle increased with oocyte number. Accordingly, Timeva [30] found improved pregnancy rates when 6–15 oocytes were collected, while aspiration of 1–5 or >15 eggs led to lower pregnancy rates. The study of McAvey et al. [31] reports fairly similar results. Obtaining 6–9 metaphase II (MII) oocytes had an advantage compared to 1–5 MII oocytes in terms of live births, but obtaining 10 or more eggs was not beneficial. They also concluded that the optimal number of retrieved oocytes was dependent on the stimulation protocol. In contrast, Letterie et al. [33] did not find any difference in fertilization rates or clinical pregnancy rates regardless of the number of oocytes collected (in case of over three eggs) in oocyte donor cycles.
However, the inferior embryo quality in the high-density group (Group 3) seems to be influenced more by the embryo density, rather than oocyte count for two main reasons. First, according to the literature [30,31,32,33], it is not obviously clear that the higher number of eggs compromises embryo quality. We can also conclude that the higher number of embryos up to nine, when culturing individually, indicates an improvement of some quality parameters. Secondly, in this study, if the number of oocytes exceeded nine, embryos were cultured in two or more dishes, and therefore could be classified into any of the groups depending on the number of embryos. It is also important to emphasize that in our study, we compared the density of cleaving embryos instead of oocytes, which is almost always lower.
It seems that lower embryo quality in the low-density group is not necessarily a result of embryo density. Higher rate of ICSI as the method of fertilization cannot be neglected. Lower egg quality and higher proportion of degenerated oocytes may also negatively affect embryo quality. The result of individual culture seems to confirm this, as similar trends have been found, when culturing embryos in single droplets. This may imply that low embryo density can be as effective as the moderate one.
The explanation for the phenomenon that an optimal density may exist, is that higher embryo density results in the facilitation of the effective zone around the embryos, promotion of the autocrine and paracrine factors, and the limitation of the positive factors around the embryos [7], but over a definite threshold, the effect of the negative factors may prevail over. These paracrine factors can be embryonic growth factors [29, 34, 35] that are secreted by the embryos and can influence the development of other embryos. Increased distance between the embryos may also diminish the positive effects as found in animal studies [28, 29]. The latter indicates that the type and structure of the culture dish have an impact on the embryo quality too. Shape and size of the microwells, as well as the distance between them play an important role in the transport of autocrine/paracrine factors. Physical contact also seems to be a remarkable characteristic [4].
In conclusion, we confirm the earlier findings [14,15,16,17] that embryo density can affect embryo development. When culturing embryos in a Primo Vision Dish, a commercially available microwell group culture dish, 4.1–5.0 μl/embryo (5–6 embryos/25 μl) density seems to be beneficial. However, we cannot exclude that low embryo density (1–4 embryos/25 μl) can be as beneficial as the moderate one. To find the proper answer for this, and for many other questions, deeper understanding of this topic is necessary. The need of prospective randomized studies, which are lacking so far, is obvious, but since the proper density depends on many factors, including culture media, culture dish type, and others, every laboratory should define the appropriate value that fits to their own culture setting and thus contribute to a better treatment outcome indeed.
References
Reed M (2006) Communication skills of embryos maintained in group culture—the autocrine paracrine debate. Clin Embryol 9:5–19
Wydooghe E, Vandaele L, Heras S, De Sutter P, Deforce D, Peelman L, De Schauwer C, Van Soom A (2015) Autocrine embryotropins revisited: how do embryos communicate with each other in vitro when cultured in groups? Biol Rev 92:505–520
Moessner J, Dodson WC (1995) The quality of human embryo growth is improved when embryos are cultured in groups rather than separately. Fertil Steril 64:1034–1035
Ebner T, Shebl O, Moser M, Mayer RB, Arzt W, Tews G (2010) Group culture of human zygotes is superior to individual culture in terms of blastulation, implantation and life birth. Reprod Biomed Online 21:762–768
Hardarson T, Bungum M, Conaghan J, Meintjes M, Chantilis SJ, Molnar L, Gunnarsson K, Wikland M (2015) Noninferiority, randomized, controlled trial comparing embryo development using media developed for sequential or undisturbed culture in a time-lapse setup. Fertil Steril 104:1452–1459
Vajta G, Peura TT, Holm P, Paldi A, Greve T, Trounson AO, Callesen H (2000) New method for culture of zona-included or zona-free embryos: the Well of the Well (WOW) system. Mol Reprod Dev 55:256–264
Reed ML (2012) Culture systems: embryo density. In: Smith GD, Swain JE, Pool TB (eds) Embryo culture. Humana Press, New York City, pp 273–312
Lane M, Gardner DK (1992) Effect of incubation volume and embryo density on the development and viability of mouse embryos in vitro. Hum Reprod 7:558–562
Salahuddin S, Ookutsu S, Goto K, Nakanishi Y, Nagata Y (1995) Fertilization and early embryology: effects of embryo density and co-culture of unfertilized oocytes on embryonic development of in vitro fertilized mouse embryos. Hum Reprod 10:2382–2385
Fujita T, Umeki H, Shimura H, Kugumiya K, Shiga K (2006) Effect of group culture and embryo-culture conditioned medium on development of bovine embryos. J Reprod Develop 52:137–142
Hoelker M, Rings F, Lund Q, Ghanem N, Phatsara C, Griese J, Schellander K, Tesfaye D (2009) Effect of the microenvironment and embryo density on developmental characteristics and gene expression profile of bovine preimplantative embryos cultured in vitro. Reproduction 137:415–425
Sananmuang T, Tharasanit T, Nguyen C, Phutikanit N, Techakumphu M (2011) Culture medium and embryo density influence on developmental competence and gene expression of cat embryos. Theriogenology 75:1708–1719
Vutyavanich T, Saeng-anan U, Sirisukkasem S, Piromlertamorn W (2011) Effect of embryo density and microdrop volume on the blastocyst development of mouse two-cell embryos. Fertil Steril 95:1435–1439
Rijnders PM, Jansen CAM (1999) Influence of group culture and culture volume on the formation of human blastocysts: a prospective randomized study. Hum Reprod 14:2333–2337
Lehner A, Pribenszky C, Murber A, Rigo J Jr, Urbancsek J, Fancsovits P (2013) Embryo density in group culture of human embryos may influence embryo quality. Hum Reprod 28(Suppl. 1):180–181
De Munck N, Santos-Ribeiro S, Mateizel I, Verheyen G (2015) Reduced blastocyst formation in reduced culture volume. J Assist Reprod Gen 32:1365–1370
Minasi MG, Fabozzi G, Casciani V, Lobascio AM, Colasante A, Scarselli F, Greco E (2015) Improved blastocyst formation with reduced culture volume: comparison of three different culture conditions on 1128 sibling human zygotes. J Assist Reprod Gen 32:215–220
Gardner DK, Lane M (2004) Culture of the mammalian preimplantation embryo. In: Gardner DK, Lane M, Watson JA (eds) A laboratory guide to the mammalian embryo. Oxford University Press, Oxford, UK, pp 41–61
Pribenszky C, Losonczi E, Molnár M, Lang Z, Mátyás S, Rajczy K, Molnár K, Kovács P, Nagy P, Conceicao J, Vatja G (2010) Prediction of in vitro developmental competence of early cleavage-stage mouse embryos with compact time-lapse equipment. Reprod Biomed Online 20:371–379
Pribenszky C, Mátyás S, Kovács P, Losonczi E, Zádori J, Vajta G (2010) Pregnancy achieved by transfer of a single blastocyst selected by time-lapse monitoring. Reprod Biomed Online 21:533–536
Diedrich K, Diedrich C, Santos E, Zoll C, Al-Hasani S, Reissmann T, Krebs D, Klingmüller D (1994) Suppression of the endogenous luteinizing hormone surge by the gonadotrophin-releasing hormone antagonist Cetrorelix during ovarian stimulation. Hum Reprod 9:788–791
World Health Organization (2010) WHO laboratory manual for the examination and processing of human semen, 5th edn. WHO Press, Geneva
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology (2011) The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod 26:1270–1283
Jones GM, Trounson AO, Gardner DK, Kausche A, Lolatgis N, Wood C (1998) Evolution of a culture protocol for successful blastocyst development and pregnancy. Hum Reprod 13:169–177
Reed ML, Woodward BJ, Swain JE (2011) Single or group culture of mammalian embryos: the verdict of the literature. J Reprod Biotech Fertil 2:77–87
Larson MA, Kubisch HM (1999) The effects of group size on development and interferon-τ secretion by in vitro fertilized and cultured bovine blastocysts. Hum Reprod 14:2075–2079
Ali J (2004) Continuous ultra micro-drop culture yields higher pregnancy and implantation rates than either large-drop culture or fresh–medium replacement. Clin Embryol 7:1–23
Stokes PJ, Abeydeera LR, Leese HJ (2005) Development of porcine embryos in vivo and in vitro; evidence for embryo ‘cross talk’ in vitro. Dev Biol 284:62–71
Gopichandran N, Leese HJ (2006) The effect of paracrine/autocrine interactions on the in vitro culture of bovine preimplantation embryos. Reproduction 131:269–277
Timeva T, Milachich T, Antonova I, Arabaji T, Shterev A, Omar HA (2006) Correlation between number of retrieved oocytes and pregnancy rate after in vitro fertilization/intracytoplasmic sperm infection. Sci World J 6:686–690
McAvey B, Zapantis A, Jindal SK, Lieman HJ, Polotsky AJ (2011) How many eggs are needed to produce an assisted reproductive technology baby: is more always better? Fertil Steril 96:332–335
Ji J, Liu Y, Tong XH, Luo L, Ma J, Chen Z (2013) The optimum number of oocytes in IVF treatment: an analysis of 2455 cycles in China. Hum Reprod 28:2728–2734
Letterie G, Marshall L, Angle M (2005) The relationship of clinical response, oocyte number, and success in oocyte donor cycles. J Assist Reprod Gen 22:115–117
Paria BC, Dey SK (1990) Preimplantation embryo development in vitro: cooperative interactions among embryos and role of growth factors. Proc Natl Acad Sci USA 87:4756–4760
Kawamura K, Chen Y, Shu Y, Cheng Y, Qiao J, Behr B, Per RAR, Hsueh AJ (2012) Promotion of human early embryonic development and blastocyst outgrowth in vitro using autocrine/paracrine growth factors. PLoS One 7:e49328
Author contributions
AL: Conceptualization data collection data curation manuscript drafting. ZK: Data collection data curation manuscript drafting. AM: Data curation manuscript drafting. JR Jr: Conceptualization manuscript drafting (reviewing). JU: Conceptualization manuscript drafting (reviewing). PF: Conceptualization data collection data curation manuscript drafting.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
According to the Hungarian law (1997. évi XLVII törvény. 21. §), scientific data, collected during healthcare treatment, can be published in case patient identification is impossible. Every patient was informed in detail about the treatment procedures and risks, and has signed the patient consent paper before initiating an IVF cycle. This also means that they were aware that scientific data of their treatments can be used according to the law without further agreement.
Primo Vision microwell group culture dishes are individually CE and CFDA certified and cleared for sale in Hungary; thus it can be used in every day practice. As this study represents retrospective analysis of data collected during routine clinical work, neither additional agreement from the patients nor ethical approval was necessary.
Conflict of interest
We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lehner, A., Kaszas, Z., Murber, A. et al. Embryo density may affect embryo quality during in vitro culture in a microwell group culture dish. Arch Gynecol Obstet 296, 345–353 (2017). https://doi.org/10.1007/s00404-017-4403-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4403-z