Abstract
Premature luteinization (PL) refers to a rise in serum progesterone (P) levels on the day of hCG administration. Most studies used an absolute P level on the day of hCG administration as an indicator of PL, and the cutoff level differed from 0.8 to 2 ng/mL. Some authors defined PL as a P/E2 ratio of >1. There is a marked variation in the incidence (13% to 71%), of PL due to discrepancies in definition, population characteristics and/or treatment protocols. The pathogenesis of PL in COH is still poorly understood. Several hypotheses may be considered to explain this phenomenon: elevation of follicular LH levels, serum accumulation of HCG from HMG, increased LH receptor sensitivity of the granulosa cells to FSH, or poor ovarian response with increased LH sensitivity. The consequences of this premature elevation of serum P on IVF outcome remain controversial. Attempts to prevent COH include: use of Low-dose hCG alone in the late COH stages, flexible antagonist protocol, use of mifepristone, aspiration of a single leading follicle, hCG administration when the levels of serum P exceeded 1.0 ng/mL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of gonadotrophin-releasing hormone (GnRH) analogues for pituitary suppression in in vitro fertilization (IVF) significantly decreased the incidence of premature luteinizing hormone (LH) surge [1]. Despite pituitary downregulation, however, several researchers have described a phenomenon reported as PL [2–5]. This refers to a rise in serum progesterone levels on the day of human chorionic gonadotrophin (hCG) administration [6]. This phenomenon has aroused interest because some authors [7–9] have reported decreased implantation and pregnancy rates with this phenomenon. Its pathogenesis is still poorly understood. Its impact on pregnancy outcome is still controversial. One of the major reasons for the controversy has been the diverse definitions of PL in previous literature.
Definition
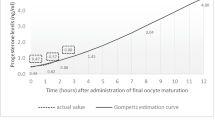
Many researchers in the past have adopted the term ‘PL’ for patients with progesterone elevation on the day of hCG administration for final oocyte maturation [3–5, 10]. This suggests that the excessive amount of progesterone is produced by granulosa cells that have started the process of luteinization. Recently, Venetis et al. [6] affirmed that, at least for the studies using GnRH agonists to inhibit LH surge, the use of the term ‘PL’ in the presence of normal LH levels might not be appropriate.
The definition of PL differed and was believed to be responsible for the variable pregnancy rates in previously published literature. Most studies used an absolute P level on the day of hCG administration as an indicator of PL, and the cutoff level differed from 0.8 to 2 ng/mL [2, 4, 7, 11–13]. (Table 1)
Recently, it has been asserted that ovarian response [14] or reserve may be of critical importance when considering PL. More follicles produce more serum P. It would, therefore, be better to take into account the ovarian response, rather than the serum P level only, when considering the reasons for PL. Therefore, Younis et al. [15] defined PL as a P/E2 ratio of >1. This criterion could differentiate between the P level secretion from dysmature follicles and physiologic secretion from multiple healthy mature follicles.
Vaginal ultrasound scanning seems to be helpful in the evaluation of minor changes in the follicular structure, correlating frequently with hormonal findings [16]. Ultrasonic features of PL of follicles are thickening of the follicular wall and the appearance of irregular echogenic structures in the follicle.
Incidence
There is a marked variation in the incidence of PL due to discrepancies in definition, population characteristics and/or treatment protocols among the studies (Table 1). It should be noted that the proportion of patients with progesterone elevation varied widely even among studies [7, 17] in which the same serum progesterone threshold (0.9 ng/mL) and the same type of GnRH analogue (agonist) were used (12.4% versus 52.3%, respectively). Previous literature reported incidence varying from 13% to 71%, using P only to define PL [2, 4, 7, 8, 11–13]. The incidence of PL using the definition of P/E2 ratio >1 was 41% in the report of Younis et al. [15].
Subtle serum progesterone rise during the late follicular phase, when gonadotrophin releasing hormone agonists (GnRHa) are combined with menotrophins for ovarian stimulation, has been reported to occur in 5–35% of IVF cycles [4, 7–9, 11, 13, 18]. The incidence of PL was 20% (P > or =1.1 ng/mL) [4] and 38.3% (P > or =1.2 ng/mL) [5] during GnRH antagonist IVF-ET cycles. The incidence of a subtle progesterone rise (P < 1.2 ng/ml or P >/= 1.2 ng/ml) was 54.7% in women undergoing COH with CC, hMG and a single 2.5 mg dose of the GnRH antagonist, cetrorelix [19]. With a flare-up protocol of GnRHa combined with high dose FSH, 85% of the cycles exhibited a rise of serum progesterone to a peak concentration of >1.0 ng/ml [20].
Pathogenesis
The pathogenesis of PL in COH is still poorly understood. Several hypotheses may be considered to explain this phenomenon.
-
I.
Elevation of follicular LH levels: Some investigators believed that PL is associated with elevation of follicular LH levels [15]. In some patients the pituitary desensitization induced by GnRHa is incomplete [2]. For this reason, increased LH secretion during the late follicular phase could be sufficient to stimulate granulosa cells to produce progesterone, but inadequate to trigger ovulation [18]. Since the introduction of long GnRHa protocol, pituitary desensitization has usually been profound and endogenous LH levels have usually been low. Although the long GnRHa protocol can prevent premature LH elevation in 95–98% of patients [21, 22], we cannot invariably blame increased preovulatory LH levels as the sole pathogenic factor in premature luteinization.
-
II.
Serum accumulation of HCG from HMG: Other investigators have suggested that the serum accumulation of hCG from hMG is responsible for PL [23]. Therefore, the use of rFSH instead of hMG has been regarded as an excellent model for elucidating this phenomenon. In comparing women with and without PL during GnRHa and hMG IVF cycles, Copperman et al. [23] found higher hCG serum levels in women who experienced a serum P rise, suggesting that PL, despite pituitary suppression with GnRHa, may be due to the hCG content of hMG [24]. According to this hypothesis, the use of human rFSH or human urinary FSH in which LH activity is negligible [25] or practically absent [26] should not provoke PL. If this was the unique etiology of PL, the use of rFSH with negligible intrinsic LH bioactivity should then help avoid premature P rise [27]. However, using urinary FSH practically devoid of LH activity (FSH 75 IU and LH <0.7 IU) [26], or recombinant FSH, with a negligible intrinsic LH bioactivity less than one-tenth that of urinary FSH [25] in combination with GnRHa for ovarian stimulation, subtle serum progesterone rise at a similar ratio (23/171 cycles, 13.4%) was observed as reported in previous studies with the use of HMG [4]. These results suggest that the HCG content of HMG is not the only cause of subtle serum progesterone rise.
-
III.
Increased LH receptor sensitivity of the granulose cells to FSH. Ubaldi et al. [4] analyzed the IVF and clinical outcomes of women who underwent COH by using GnRHa in combination with rFSH or urinary FSH. They found that greater FSH exposure correlated with P exposure and suggested that the cause of the subtle rise in P may be related to an increased LH sensitivity of the granulosa cells of FSH-treated cycles. However, they defined PL by serum P level only. The highest sensitivity of the granulose cells to FSH is due to the increased oestradiol levels as well as due to the increased number of follicles with 17 mm or more [5, 27, 28]. These data suggest that the increased LH receptor sensitivity in the granulosa cells is due to higher cumulative exposure to oestradiol which, in conjunction with FSH, could be one of the mechanisms to account for the premature increases in serum progesterone concentration. Furthermore, Adonakis et al. [29] suggested that an increase in P in the late follicular phase is unrelated to any luteinizing process attributable to effects of follicular cells to LH.
-
IV.
Poor ovarian response with increased LH sensitivity. Premature luteinization as defined by the P/E2 ratio was more prevalent in poor ovarian responders. It was related to poor ovarian response with increased LH sensitivity, similar to the report by Younis et al. [30]. Based on LH measurements and the use of rFSH, Younis et al. concluded that neither the LH nor the hCG content of the recombinant preparations is responsible for this elevation of P/E2 ratio level. Younis et al. [30] suggested that Pl is not necessarily an LH dependent event and may be primarily related to an adversely affected cumulus–oocyte complex.
-
V.
Recently emerging evidence points to the existence of an oocyte granulosa cell regulatory loop by which complementary signaling and metabolic pathways drive the development and function of both the oocytes and follicular somatic compartments. Growth differentiation factor 9 (GDF9) and bone morphogenetic protein 15 (BMP15) are two well-characterized oocyte-derived growth factors that play crucial roles in follicle growth and ovulation in all mammalian species including humans [31, 32]. Genetic targeting or spontaneous mutations of either Gdf9 or Bmp15 in mammals affect fertility in females [33]. Disrupting signaling in the ovarian granulosa cells leads to premature luteinization of granulosa cells [34].
Impact
The consequences of this premature elevation of serum progesterone, defined as PL, on IVF outcome remain controversial [35, 36]. Several authors did not find any negative effect of this on IVF outcome [11–13, 17, 18, 37–51], Hoffman et al. [2, 10] observed no significant difference in pregnancy rate in patients undergoing IVF/embryo transfer with high or low progesterone concentrations on the day of HCG administration and in patients who received oocytes donated from women with high or low progesterone concentrations.
Other authors reported that pregnancy rate has been inversely related to serum progesterone levels on the day of HCG administration [5, 8, 11–13, 16, 41, 52–56]. Although a significant inverse relationship between serum progesterone on the day of HCG and the success of IVF is established in many programmes, the involved endocrinologic mechanism is unclear.
It has been described that it may affect it as an ovarian event, with adverse effects on oocyte maturation, fertilization or early cleavage [5, 8, 9, 31, 36, 41, 52, 57]. The mean number of retrieved oocytes, recovered mature oocytes, embryos and top quality embryos were significantly higher in the non-prematurely luteinized group than in the prematurely luteinized group. Although fertilization rates and implantation rates were similar between the two groups, the clinical pregnancy rate was higher in the non-prematurely luteinized group than in the prematurely luteinized group [14].
On the other hand, poorer embryo quality was not found in a number of studies [2, 3, 7, 12, 43, 58, 59]. These findings suggest that PL may influence the endometrium, adversely affecting implantation and subsequent embryo development due to PL. This hypotheses was sustained by others groups [41, 58, 60–63]. Forman et al. [61], Sharma et al. [58] and Silverberg et al. [7] suggested that the mechanism of deleterious effect of elevated progesterone was abnormally accelerated endometrial maturation leading to impaired endometrial receptivity. Melo et al. analysed retrospectively 240 oocyte-donation cycles in which 120 women donated twice, with PL in the first donation cycle and no PL in the following one, acting as its own control [64]. Recipients (n = 240) were divided in two groups according to the presence of PL (n = 120) or not (n = 120). There was no difference in PR between the groups (55.7 Vs 54.4%, respectively). The number of total oocytes (18.2 Vs 20.8) and the number of mature oocytes retrieved (16.9 Vs 19.4) were different among donors with progesterone <1.2 ng/ml and PL, respectively. There were no differences between the oocyte recipients in fertilization, cleavage, embryo division on day 3, blastocyst development or fragmentation rates. The number of embryos transferred, number of embryos cryopreserved, and implantation and miscarriage rates were similar between the groups. Melo et al. concluded that, PL does not appear to have a negative impact on ongoing PR in oocyte donation programme.
However, several clinical trials have been performed in which progesterone supplementation for luteal phase support was started on the day of HCG administration, without any negative impact on PR due to a deleterious effect on the endometrium, suggesting that there is no negative impact of the PL on IVF outcome [37–40].
Recent Systematic review and meta-analysis was conducted to evaluate whether progesterone elevation on the day of hCG administration is associated with the probability of pregnancy [6]. Eligible studies were considered those in which patients did not participate more than once. A literature search identified 12 eligible studies, 10 of which were retrospective. The majority (n = 10) of these studies did not detect a statistically significant association between progesterone elevation and the probability of pregnancy. Meta-analysis was performed only for the studies (n = 5) that provided data on clinical pregnancy per patient reaching hCG administration for final oocyte maturation. Clinical pregnancy rate was lower, but not significantly so, in the group with progesterone elevation. No statistically significant association between progesterone elevation and the probability of clinical pregnancy was detected (Odds ratio: 0.75, 95% confidence interval 0.53–1.06; P 5 0.10). In addition, subgroup analyses were conducted on the basis of type of GnRH analogue used and on the value of serum threshold used to classify patients in those with or without progesterone elevation. These analyses, however, did not materially change the results obtained.
The E2 levels (pg/mL) on the day of hCG administration were significantly higher in the group of patients that exhibited progesterone elevation on the day of hCG compared with those who did not cumulus-oocyte complexes (COCs) retrieved. No statistically significant difference in the number of COCs retrieved was detected between the patients with and those without progesterone elevation on the day of hCG administration. This systematic review reveals the lack of well-designed prospective studies that could answer the research question asked. The best available evidence does not support an association between progesterone elevation on the day of hCG administration and the probability of clinical pregnancy in women undergoing ovarian stimulation with GnRH analogues and gonadotrophins for IVF. The validity of this conclusion has been further debated, due to the fact that most of the studies that failed to show a deleterious effect when PL is present, used a low cut-off level for defining premature luteinization (0.9 ng/ml) [65].
Prevention
It should be noted that if a negative association between progesterone elevation on the day of hCG administration and the probability of pregnancy exists, it might be worth examining the possibility of cryopreserving the resulting embryos and their transfer in a subsequent frozen-thawed cycle [3, 7, 41] or alternatively, administering hCG at an earlier time in the follicular phase, prior to progesterone elevation [9]. On the contrary, absence of an association indicates that assessment of serum progesterone on the day of hCG administration might be redundant [6]. A literature search identified several regimens for prevention of PL.:
-
1.
Low-dose hCG alone in the late COH stages: Patients received ovarian priming with recombinant FSH/hMG followed by low-dose hCG (200 IU/day) alone [66]. This regimen did not cause PL and was associated with reduced recombinant FSH/hMG consumption, reduced number of small preovulatory follicles, more estrogenic intrafollicular environment and higher fertilization rate.
-
2.
Flexible antagonist protocol [67]. In IVF-ICSI patients undergoing COS with the antagonist protocol, the antagonist administration was initiated according to at least one of the following patient-specific criteria: (i) at least one follicle measuring >14 mm; (ii) estradiol levels >600 pg/ml; and (iii) LH levels >10 IU/l. Rapid response, causing earlier antagonist administration initiation, according to the proposed criteria for the prevention of premature LH surges, and the absence of PL, as evidenced by normal progesterone levels on HCG day, were found to be independent positive predictive factors for favourable IVF outcome. The employment of an algorithm of criteria, aimed at the prevention of premature LH surges in a flexible antagonist protocol, resulted in antagonist initiation earlier than on stimulation day 6 in a significant proportion of patients. In those patients, a higher pregnancy rate was observed.
-
3.
Mifepristone [68]. The effectiveness of a daily dose of 40 mg mifepristone in preventing premature LH surges in women undergoing COH for IVF was investigated. In all patients receiving mifepristone, 50 mg progesterone were administered IM at the time of hCG administration to counteract residual antiprogestogenic activity of mifepristone. No LH surges were observed in any subject treated with mifepristone. Serum P levels on the day of hCG/P were below the cut-off level (1.2 ng/ml) in all subjects of the mifepristone group (range, <0.5 to 1.05 ng/ml). The results of this exploratory study provide evidence that mifepristone is effective for the prevention of premature LH surges and/or PL in women undergoing COH for in vitro fertilization.
-
4.
HCG injection when serum P>1.0 ng/ml (rescued subtle P rise) [69]. Altering the timing of hCG injection according to serum progesterone concentrations improves embryo quality in cycles with subtle P rise. Serum was obtained daily or every 12 h from day 7 until the administration of hCG. hCG injection was given when the levels of serum P exceeded 1.0 ng/mL (“rescued” subtle P rise). The mean day of hCG administration in the rescued cycles was 1 day earlier than those of the subtle P rise and no P rise cycles. The rate of embryonic development beyond four-cell stage was increased significantly in the rescued cycles and no P rise cycles versus the subtle P rise cycles. Embryos obtained in the no P rise and rescued cycles were of better morphological quality than those obtained in the P rise cycles. The implantation rate was significantly higher in the rescued cycles than in the P rise cycles. The data suggest that, if hCG is administered when a subtle P rise is detected, embryo quality and subsequent implantation rate can be improved.
-
5.
Aspiration of a single leading follicle [70]. In 12 patients stimulated for IVF-ET, a single leading follicle developed, whereas the other follicles were 6 mm smaller. In 7 patients chosen at random (group A), the leading follicle was aspirated, whereas in the other 5 the leading follicle was allowed to continue growing (group B). Premature LH surge was avoided only in group A, and only in this group a second follicle aspiration for IVF-ET was done, and two pregnancies were achieved. In group B, aspiration for IVF-ET was canceled because of premature LH surge. It is suggested that aspiration of a single leading follicle during ovulation induction may be an efficient method to avoid premature LH surge enabling other follicles to develop up to the preovulatory stage.
References
Smitz J, Ron-El R, Tarlatzis BC. The use of gonadotrophin releasing hormone agonists for in vitro fertilization and other assisted procreation techniques: experience from three centres. Hum Reprod. 1992;7:49–66.
Hofmann GE, Bentzien F, Bergh PA, et al. Premature luteinization in controlled ovarian hyperstimulation has no adverse effect on oocyte and embryo quality. Fertil Steril. 1993;60:675–9.
Legro RS, Ary BA, Paulson RJ, et al. Premature luteinization as detected by elevated serum progesterone is associated with a higher pregnancy rate in donor oocyte in-vitro fertilization. Hum Reprod. 1993;8:1506–11.
Ubaldi F, Albano C, Peukert M, et al. Subtle progesterone rise after the administration of the gonadotrophin-releasing hormone antagonist cetrorelix in intracytoplasmic sperm injection cycles. Hum Reprod. 1996;11:1405–7.
Bosch E, Valencia I, Escudero E, et al. Premature luteinization during gonadotropin-releasing hormone antagonist cycles and its relationship with in vitro fertilization outcome. Fertil Steril. 2003;80:1444–9.
Venetis C, Kolibianakis E, Papanikolaou E, Bontis J, Devroey P, Tarlatzis B. Is progesterone elevation on the day of human chorionic gonadotrophin administration associated with the probability of pregnancy in in vitro fertilization? A systematic review and meta-analysis. Hum Reprod Update. 2007;13:343–55.
Silverberg KM, Martin M, Olive DL, et al. Elevated serum progesterone levels on the day of human chorionic gonadotropin administration in in vitro fertilization cycles do not adversely affect embryo quality. Fertil Steril. 1994;61:508–13.
Fanchin R, de Ziegler D, Taieb J, et al. Premature elevation of plasma progesterone alters pregnancy rates of in vitro fertilization and embryo transfer. Fertil Steril. 1993;59:1090–4.
Harada T, Yoshida S, Katagiri C, et al. Reduced implantation rate associated with a subtle rise in serum progesterone concentration during the follicular phase of cycles stimulated with a combination of a gonadotrophin-releasing hormone agonist and gonadotrophin. Hum Reprod. 1995;10:1060–4.
Hofmann GE, Khoury J, Johnson CA, et al. Premature luteinization during controlled ovarian hyperstimulation for in vitro fertilization embryo transfer has no impact on pregnancy outcome. Fertil Steril. 1996;66:980–6.
Edelstein MC, Seltman HJ, Cox BJ, et al. Progesterone levels on the day of human chorionic gonadotropin administration in cycles with gonadotropin-releasing hormone agonist suppression are not predictive of pregnancy outcome. Fertil Steril. 1990;54:853–7.
Check JH, Chase JS, Nowroozi K, Dietterich CJ. Premature luteinization: treatment and incidence in natural cycles. Hum Reprod. 1991;6:190–3.
Givens CR, Schriock ED, Dandekar PV, et al. Elevated serum progesterone levels on the day of human chorionic gonadotropin administration do not predict outcome in assisted reproduction cycles. Fertil Steril. 1994;62:1011–7.
Ou YC, Lan KC, Chang SY, Kung FT, Huang FJ. Increased progesterone/estradiol ratio on the Day of hcg administration adversely affects Success of in vitro fertilization–embryo Transfer in patients stimulated with Gonadotropin-releasing hormone agonist and Recombinant follicle-stimulating hormone Taiwan. J Obstet Gynecol. 2008;47:168–74.
Younis JS, Simon A, Laufer N. Endometrial preparation: lessons from oocyte donation. Fertil Steril. 1996;66:873–84.
Hamori M, Stuckensen JA, Rumpf D, Kniewald T, Kniewald A, Kurtz CS. Premature luteinization of follicles during ovarian stimulation of in vitro fertilisation. Hum Reprod. 1987;2:639–43.
Martinez F, Coroleu B, Clua E, et al. Serum progesterone concentrations on the day of HCG administration cannot predict pregnancy in assisted reproduction cycles. Reprod Biomed Online. 2004;8:183–90.
Ubaldi F, Smitz J, Wisanto A, et al. Oocyte and embryo quality as well as pregnancy rate in intracytoplasmic sperm injection are not affected by high follicular phase serum progesterone. Hum Reprod. 1995;10:3091–6.
Seow KM, Lin YH, Huang LW, Hsieh BC, Huang SC, Chen CY, et al. Subtle progesterone rise in the single-dose gonadotropin-releasing hormone antagonist (cetrorelix) stimulation protocol in patients undergoing in vitro fertilization or intracytoplasmic sperm injection cycles. Gynecol Endocrinol. 2007;23:338–42.
Sims A, Seltman HJ, Muasher SJ. Early follicular rise of serum progesterone concentration in response to a flare-up effect of gonadotrophin-releasing hormone agonist impairs follicular recruitment for in-vitro fertilization. Hum Reprod. 1994;9:235–40.
Ron-El R. Improved pregnancy rate in IVF/ET by combined long-acting GnRH analogue and gonadotropins. In: Vickery BH, Lunenfeld B, editors. GnRH analogues in reproduction and gynecology, vol. II. Dordrecht: Kluwer Academic; 1990. p. 167–71.
Penzias AS, Shamma FN, Gutmann JN, Jones EE, DeCherney AH, Lavy G. Nafarelin versus leuprolide in ovulation induction for in vitro fertilization: a randomized clinical trial. Obstet Gynecol. 1992;79:739–42.
Copperman AB, Horowitz GM, Kaplan P, Scott RT, Navot D, Hofmann GE. Relationship between circulating human chorionic gonadotropin levels and premature luteinization in cycles of controlled ovarian hyperstimulation. Fertil Steril. 1995;63:1267–71.
Stokman PGW, de Leeuw R, van den Wijngaard HAGW, Kloosterboer HJ, Vemer HM, Sanders ALM. Human chorionic gonadotropin in commercial human menopausal gonadotropin preparations. Fertil Steril. 1993;60:175–8.
Mannaerts B, de Leeuw R, Geelen J, Van Ravestein A, Van Wezenbeek P, Schuurs A, et al. Comparative in vitro and in vivo studies on the biological characteristics of recombinant human follicle-stimulating hormone. Endocrinology. 1991;129:2623–30.
Shaw RW, Ndukwe G, Imoedemhe DA, Bernard AG, Burford G. Twin pregnancy after pituitary desensitization with LHRH agonist and pure FSH. Lancet. 1985;326:506–7.
Peluso JJ. Role of the amplitude of the gonadotropin surge in the rat. Fertil Steril. 1990;53:150–4.
Filicori M, Cognigni GE, Pocognoli P, Tabarelli C, Spettoli D, Taraborrelli S, et al. Modulation of folliculogenesis and steroidogenesis in women by graded menotrophin administration. Hum Reprod. 2002;17:2009–15.
Adonakis G, Deshpande N, Yates RWS, Fleming R. Luteinizing hormone increases estradiol secretion but has no effect on progesterone concentrations in the late follicular phase of in vitro fertilization cycles in women treated with gonadotropin-releasing hormone agonist and follicle stimulating hormone. Fertil Steril. 1998;69:450–3.
Younis JS, Matilsky M, Radin O, Ben-Ami M. Increased progesterone/estradiol ratio in the late follicular phase could be related to low ovarian reserve in in vitro fertilization-embryo transfer cycles with a long gonadotropin releasing hormone agonist. Fertil Steril. 2001;76:294–9.
Chand L, Ponnampalam P, Harris E, Winship M, Shelling N. Mutational analysis of BMP15 and GDF9 as candidate genes for premature ovarian failure. Fertil Steril. 2006;86:1009–12.
Di Pasquale E, Rossetti R, Marozzi A, Bodega B, Borgato S, Cavallo L, et al. Identification of new variants of human BMP15 gene in a large cohort of women with premature ovarian failure. J Clin Endocrinol Metab. 2006;91:1976–9.
Juengel L, McNatty P. The role of proteins of the transforming growth factor-beta superfamily in the intraovarian regulation of follicular development. Hum Reprod Update. 2005;11:143–60.
Pangas S, Li X, Robertson E, Matzuk M. Premature luteinization and cumulus cell defects in ovarian-specific Smad4 knockout mice. Mol Endocrinol. 2006;20:1406–22.
Fanchin R, Hourvitz A, et al. Premature progesterone elevation spares blastulation but not pregnancy rates in in vitro fertilization with coculture. Fertil Steril. 1997;68:648–52.
Shulman A, Ghetler Y, Beyth Y, et al. The significance of an early (premature) rise of plasma progesterone in in vitro fertilization cycles induced by a “long protocol” of gonadotropin releasing hormone analogue and human menopausal gonadotropins. J Assist Reprod Genet. 1996;13:207–11.
Howles CM, Macnamee MC, Edwards RG. Progesterone supplementation in the late follicular phase of an in vitro fertilisation cycle: a natural way to time oocyte recovery? Hum Reprod. 1988;3:409–12.
Mahadevan MM, Fleetham J, Taylor PJ. Effects of progesterone on luteinizing hormone release and estradiol/progesterone ratio in the luteal phase of women superovulated for in vitro fertilisation and embryo transfer. Fertil Steril. 1988;50:935–7.
Ben-Nun I, Ghetler Y, Jaffe R, Siegal A, Kaneti H, Fejgin M. The effect of preovulatory progesterone administration on the endometrial maturation and implantation rate after in vitro fertilisation and embryo transfer. Fertil Steril. 1990;53:276–81.
Hassiakos D, Toner JP, Muasher SJ, Jones HW. Implantation and progesterone profiles in cycles with and without the use of gonadotropin releasing hormone agonist suppression. Hum Reprod. 1990;5:1004–8.
Silverberg KM, Burns WN, Olive DL, et al. Serum progesterone levels predict success of in vitro fertilization/embryo transfer in patients stimulated with leuprolide acetate and human menopausal gonadotropins. J Clin Endocrinol Metab. 1991;73:797–803.
Antoine JM, Firmin C, Salat-Baroux J, et al. Prognostic value of preovulatory elevations of plasma progesterone during in vitro fertilization using LHRH agonists in a long protocol. J Gynecol Obstet Biol Reprod. 1992;21:629–34.
Bustillo M, Stern JJ, Coulam CB. Serum progesterone at the time of human chorionic gonadotrophin does not predict pregnancy in in-vitro fertilization and embryo transfer. Hum Reprod. 1995;10:2862–7.
Levy MJ, Smotrich DB, Widra EA, et al. The predictive value of serum progesterone and 17-OH progesterone levels on in vitro fertilization outcome. J Assist Reprod Genet. 1995;12:161–6.
Abuzeid MI, Sasy MA. Elevated progesterone levels in the late follicular phase do not predict success of in vitro fertilization-embryo transfer. Fertil Steril. 1996;65:981–5.
Huang JC, Jackson KV, Hornstein MD, et al. The effect of elevated serum progesterone during ovulation induction in in vitro fertilization-embryo transfer. J Assist Reprod Genet. 1996;13:617–24.
Miller KF, Behnke EJ, Arciaga RL, et al. The significance of elevated progesterone at the time of administration of human chorionic gonadotropin may be related to luteal support. J Assist Reprod Genet. 1996;13:698–701.
Moffitt DV, Queenan Jr JT, Shaw R. Progesterone levels on the day of human chorionic gonadotropin do not predict pregnancy outcome from the transfer of fresh or cryopreserved embryos from the same cohort. Fertil Steril. 1997;67:296–301.
Doldi N, Marsiglio E, Destefani A, et al. Elevated serum progesterone on the day of HCG administration in IVF is associated with a higher pregnancy rate in polycystic ovary syndrome. Hum Reprod. 1999;14:601–5.
Lindheim SR, Cohen MA, Chang PL, et al. Serum progesterone before and after human chorionic gonadotropin injection depends on the estradiol response to ovarian hyperstimulation during in vitro fertilization—embryo transfer cycles. J Assist Reprod Genet. 1999;16:242–6.
Urman B, Alatas C, Aksoy S, et al. Elevated serum progesterone level on the day of human chorionic gonadotropin administration does not adversely affect implantation rates after intracytoplasmic sperm injection and embryo transfer. Fertil Steril. 1999;72:975–9.
Schoolcraft W, Sinton E, Schlenker T, et al. Lower pregnancy rate with premature luteinization during pituitary suppression with leuprolide acetate. Fertil Steril. 1991;55:563–6.
Kagawa T, Yamano S, Nishida S, et al. Relationship among serum levels of luteinizing hormone, estradiol, and progesterone during follicle stimulation and results of in vitro fertilization and embryo transfer (IVF–ET). J Assist Reprod Genet. 1992;9:106–12.
Mio Y, Sekijima A, Iwabe T, et al. Subtle rise in serum progesterone during the follicular phase as a predictor of the outcome of in vitro fertilization. Fertil Steril. 1992;58:159–66.
Mio Y, Terakawa N. Reduced implantation rate associated with a subtle rise in serum progesterone concentration during the follicular phase of cycles stimulated with a combination of gonadotrophin-releasing hormone agonist and gonadotrophin. Hum Reprod. 1995;10:1060–4.
Ozcakir HT, Levi R, Tavmergen E, Goker EN. Premature luteinization defined as progesterone estradiol ratio >1 on hCG administration day seems to adversely affect clinical outcome in long gonadotropin-releasing hormone agonist cycles. J Obstet Gynaecol Res. 2004;30:100–4.
Fanchimont P, Hazee-Hagelstein MT, Hazout A, Frydman R, Scatz B, Demerle F. Correlation between follicular fluid content and the results of in vitro fertilisation and embryo transfer. Fertil Steril. 1989;52:1006–11.
Yovel I, Yaron Y, Amit A, et al. High progesterone levels adversely affect embryo quality and pregnancy rates in in vitro fertilization and oocyte donation programs. Fertil Steril. 1995;64:128–31.
Fanchin R, Righini C, Olivennes F, et al. Premature progesterone elevation does not alter oocyte quality in in vitro fertilization. Fertil Steril. 1996;65:1178–83.
Garcia JE, Acosta AA, Hsiu JG, Jones HW. Advanced endometrial maturation after ovulation induction with human menopausal gonadotrophin/ human chorionic gonadotrophin for in vitro fertilisation. Fertil Steril. 1984;41:31–5.
Forman RG, Eychenne B, Nessmann C, Frydman R, Robel P. Assessing the early luteal phase in vitro fertilisation cycles: relationships between plasma steroids, endometrial receptors, and endometrial histology. Fertil Steril. 1989;51:310–6.
Sharma V, Whitehead M, Mason B, Pryse-Davies J, Ryder T, Dowsett M, et al. Influence of superovulation on endometrial and embryonic development. Fertil Steril. 1990;53:822–9.
Burns WN, Witz CA, Klein NA, Silverberg KM, Schnken RS. Serum progesterone concentrations on the day after human chorionic gonadotropin administration and progesterone/oocyte ratios predict in vitro fertilisation/ embryo transfer outcome. J Assist Reprod Genet. 1994;11:17–23.
Melo M, Meseguer M, Garrido N, Bosch E, Pellicer A, Remohí J. The significance of premature luteinization in an oocyte-donation programme. Hum Reprod. 2006;21:1503–7.
Bosch E. Comment on: is progesterone elevation on the day of human chorionic gonadotrophin administration associated with the probability of pregnancy in in vitro fertilization? A systematic review and meta-analysis. By Venetis et al (2007). Hum Reprod Update. 2008;14:194–5.
Filicori M, Cognigni GE, Gamberini E, Parmegiani L, Troilo E, Roset B. Efficacy of low-dose human chorionic gonadotropin alone to complete controlled ovarian stimulation. Fertil Steril. 2005;84:394–401.
Lainas T, Zorzovilis J, Petsas G, Stavropoulou G, Cazlaris H, Daskalaki V, et al. In a flexible antagonist protocol, earlier, criteria-based initiation of GnRH antagonist is associated with increased pregnancy rates in IVF. Hum Reprod. 2005;20:2426–33.
Escudero EL, Boerrigter PJ, Bennink HJ, Epifanio R, Horcajadas JA, Olivennes F, et al. Mifepristone is an effective oral alternative for the prevention of premature luteinizing hormone surges and/or premature luteinization in women undergoing controlled ovarian hyperstimulation for in vitro fertilization. J Clin Endocrinol Metab. 2005;90:2081–8.
Harada T, Katagiri C, Takao N, Toda T, Mio Y, Terakawa N. Altering the timing of human chorionic gonadotropin injection according to serum progesterone concentrations improves embryo quality in cycles with subtle P rise. Fertil Steril. 1996;65:594–7.
Barash A, Shoham Z, Lunenfeld B, Segal I, Insler V, Borenstein R. Can premature luteinization in superovulation protocols be prevented by aspiration of an ill-timed leading follicle? Fertil Steril. 1990;53:865–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
Pathogenesis of premature luteinization is poorly understood and its impact on ICSI is controversial.
Rights and permissions
About this article
Cite this article
Elnashar, A.M. Progesterone rise on the day of HCG administration (premature luteinization) in IVF: An overdue update. J Assist Reprod Genet 27, 149–155 (2010). https://doi.org/10.1007/s10815-010-9393-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-010-9393-8