Abstract
Purpose
Implantation failure is known to be associated with an increased risk of aneuploidy in embryos, a situation leading to a pre-implantation genetic screening, not allowed in different countries like France. Our aim was to evaluate the gamete aneuploidy incidence in this context, using first polar body and spermatozoa aneuploidy screening.
Methods
Three groups were considered: 11 couples with pregnancy obtained after IVF for female infertility (group 1); 20 couples with pregnancy obtained after IVF for male infertility (group 2); and 35 couples with implantation failure (group 3). In group 3, 28 couples treated by ICSI volunteered for first polar body analysis (PB1).
Results
Spermatozoa aneuploidy rate was increased in groups 2 (1.6%) and 3 (2.1%) in comparison to group 1 (0.6%). PB1 aneuploidy rate was 35.4% in group 3. Finally, eight couples (32%) had no particular chromosomal risk in gametes, 15/25 (60%) presented an increased spermatic (>2%) or oocyte (>1/3) aneuploidy rate, and 2/25 (8%) had both.
Conclusion
Those results confirm that implantation failure has a heterogeneous origin, that gamete chromosome abnormality rate is one of the major contributing factors, and that 1st Polar body and spermatozoa aneuploidy screening or pre-implantation genetics screening may be indicated for these couples.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the general population, 60% of human embryos are estimated to be aneuploid [1], and most of them do not implant. Aneuploidy arises in the oocyte in more than 70% of cases, and most abnormalities occur during the first meiotic division [2, 3]. Maternal aging is the only etiologic factor unequivocally linked to aneuploidy risk at birth, and aneuploidy incidence in oocytes increases with maternal age [4–6].
Recurrent implantation failure has been associated with increased oocyte aneuploidy rate. Pre-implantation genetic screening of embryos has confirmed the increase in embryo aneuploidy rate in cases of recurrent implantation failure [7–9], but aneuploidy mechanism seems to differ compare to women with advanced maternal age [10, 11].
Recently, it has been shown for women with recurrent implantation failure that availability of euploid embryos is associated with high ongoing pregnancy and implantation rates, especially on two consecutive PGD cycles. At the opposite, absence of euploid embryos for transfer predicts poor reproductive outcome [12].
However, in 40% of cases chromosomal factors in oocytes are not involved [4], and implantation failure may result from abnormalities of uterine receptivity or uterine cavity, or poor gametic quality [13].
In cases of increased genetic risk in embryos with no genetic disease identified in the parents, ie advanced maternal age [4, 14] or recurrent implantation failure [4], pre-implantation genetic screening is not allowed in France, but preconception screening can be offered before ICSI as a research protocol, since this concerns gametes and not embryos.
Oocyte abnormalities are the main cause of fetal aneuploidy [15], but 5–15% of trisomy cases are of paternal origin [16]. In case of fetuses conceived after ICSI, increased aneuploidy rate has been reported [17], which particularly concerned gonosomes [18], probably due to increased sperm aneuploidy rate in infertile patients [19–21]. Spermatozoa morphological abnormalities, including macrocephalia [22, 23], asthenospermia [24] and globozoospermia [25, 26] are known to be associated with increased aneuploidy rate. These abnormalities are regarded as a justification for pre-implantation genetic screening in some countries [8, 9]. Furthermore, spermatozoa aneuploidy rates were shown to be increased in recurrent implantation failure compared with controls or with patients with pregnancy obtained within three ICSI treatment attempts [19].
As embryo screening is not permitted in many countries like France, we evaluated gametic chromosomal abnormalities for a couple with recurrent implantation failure, using preconception screening of the first polar body and FISH of spermatozoa, and their utility in this context. Spermatozoa results were compared with those from control patients and patients with a pregnancy obtained at the first ICSI attempt.
Materials and methods
Patients
Three groups of patients were considered: group 1 (n = 11)—control couples with pregnancy obtained after conventional IVF with normal sperm for tubal pathology or oocyte donation, group 2 (n = 20)—couples with pregnancy and delivery (before ten embryos transferred) obtained after IVF (with or without ICSI) for male infertility, and group 3 (n = 35)—couples with implantation failure with more than ten embryos transferred without pregnancy.
Male mean age was similar in the three groups (35 + 3; 34 + 8 and 36 + 6 years old for groups 1, 2 and 3, respectively). Sperm characteristics (Table 1) were significantly different in group 1 compared with groups 2 and 3 (p < 0.05). The absence of differences between groups 2 and 3 confirmed the poor predictive value of sperm parameters on ICSI outcome.
Characteristics of the women included in the study are summarized in Table 2. Women in group 2 were significantly (p < 0.02) younger than those of groups 1 and 3. Women in group 1 had statistically (p < 0.0005) more previous pregnancies. Women in group 3 had statistically (p < 0.0001) more previous IVF attempts and embryos transferred.
FISH spermatozoa analysis
Spermatozoa were fixed in a 3:1 methanol/acetic acid solution after two water washes, spread on a slide, air-dried and fixed with methanol for 5 min at room temperature. Spermatozoa decondensation was performed in 1 N NaOH (2 min). After dehydration, FISH was carried out using X, Y and 18 centromeric probes: CEPX (green), CEPY (red) and CEP18 (aqua) (Vysis–Abbott). FISH was performed at 73°C, 4 min and 37°C overnight hybridization program.
Slides were washed and counterstained with DAPI solution and spermatozoa were analyzed under an Olympus microscope using the PathVysion kit. Observation and interpretation criteria were based on the number of spots per probe on the sperm nuclei. Only spermatozoa with one spot for 18 and one spot for either X or Y were regarded as normal. X/Y/18 results were compared between the three patients groups. For each patient, about 1,000 spermatozoa were analyzed.
Polar body analysis
Polar body biopsy was offered to women with recurrent implantation failure. Out of 35 patients, 28 agreed to polar body screening, which was carried out using the Zilos TK laser (Hamilton Thorne Biosciences). No control group was possible for preconception screening, taking into account the restrictions of French bioethics law. Immediately after oocyte retrieval and decoronization, three or four laser impacts (180 mW, 0.5 ms pulse) penetrated the zona pellucida (ZP). The polar body was then extracted with a biopsy micropipette (Humagen) and placed in 0.5 µl of water on a siliconized slide. This water drop was air-dried and two drops of Carnoy solution were added.
The slide was transferred into a series of solutions: 5 min in methyl alcohol at room temperature, 10 min in 2×SSC at 37°C, 10 min in a 1% paraformaldehyde solution at room temperature, 5 min in PBS at room temperature, 10 min in 0.1 N HCl with 30 μl/40 ml of 10% active pepsin solution, 5 min in PBS at room temperature, 2 min in 70%, 85% and 100% ethyl alcohol for dehydration.
A 3 μl drop of probe solution was placed on each polar body. Codenaturation and hybridization were automatically performed in the Hybrite (Vysis) (73°C for 4 min and 37°C for 4 h).
The slide was then washed in two solutions: 1 min 45 s in a 0.7×SSC/0.3% NP40 solution, and 15 s in a 2×SSC/0.1% NP40 solution, then counterstained with an antifade solution, and analyzed with a five-filter fluorescence microscope (Olympus BX60) and the PathVysion imaging system.
Polar bodies were analyzed by the MultiVysionTM Polar Body Kit probe panel hybridization mixture marketed by Abbott including LSI® 13 (13q14) labeled with SpectrumRedTM, CEP® 16 (satellite II D16Z3) labeled with SpectrumAquaTM, CEP® 18 (alpha satellite D18Z1) labeled with SpectrumBlueTM, LSI® 21 (21q22.13–21q2.2) labeled with SpectrumGreenTM, and LSI® 22 (22q11.2) labeled with SpectrumGoldTM.
Each polar body chromosome normally consists of two chromatids. Locus-specific probes always give a doublet signal corresponding to each chromatid and each chromosome was represented by a doublet of distinct color, sometimes very close, or by two separate signals. Centromeric probes usually give large signals for one chromosome or a doublet with very close signals. Signal absence or four signals were interpreted as nondisjunction and one or three spots as unbalanced premature separation of sister chromatids. Two separate signals were not considered as an abnormality, but as a balanced separation of sister chromatids.
ICSI procedure
Oocytes with normal FISH results or without FISH analysis because of technical failure or immaturity (the biopsy was not possible in the morning although the polar body was expelled at the time of ICSI in the afternoon) were then microinjected. The opening in the zona pellucida was kept at 12 or 6 o’clock in order to keep the spindle away from the microinjection site. Oocytes were then microinjected with a 7 µm outer diameter ICSI micropipette (Humagen, Charlottesville, VA, USA).
Statistical analysis
Statistical analysis (χ2 test, Fisher test and Mann Whitney test) were performed using the Statview program. Differences were considered significant when p < 0.05.
Results
Sperm aneuploidy rate
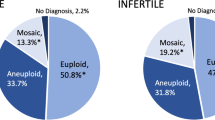
A total of 11248 spermatozoa were analyzed for group 1 (control) patients (1,023 per patient), 19,682 for group 2 (fertile after IVF) patients (984 per patient) and 29,540 (844 per patient) for group 3 (recurrent implantation failure) patients. When all patients were considered, overall spermatozoa aneuploidy rate was 1.61%, with 1.22% for gonosomes i.e. three times the chromosome 18 aneuploidy rate (0.36%). We observed an overall increased aneuploidy rate in groups 2 (1.64%; p < 0.0005) and 3 (1.97%; p < 0.001) compared with group 1 (0.59%), and this increase concerned both chromosome 18 (p < 0.05) and gonosomes (p < 0.05) (Fig. 1, Table 3).
We chose 2% (3.5 times the mean group1 rate) and 5% (8.5 times the mean group1 rate), respectively as cut-off points for moderate and high aneuploidy rate. Eight out of 32 patients in group 3, six out of 20 in group 2, but none in group 1 had a moderate sperm aneuploidy rate (between 2% and 5%, see Table 4). Two patients in group 3 had a high aneuploidy rate in spermatozoa (6.5% and 25%) but none in groups 1 or 2. The first patient had cryptozoospermia (40,000 spermatozoa/ml, only 215 spermatozoa could be analyzed by FISH); the second had a partial macrocephalia syndrome with 8% typical forms and 20% macrocephalic spermatozoa.
Polar body aneuploidy rate
Polar body aneuploidy rate was 34.5% (60 out of 174) and spanned from 0% to 85.7%. Twenty-five patients with more than three first polar bodies tested were divided into three groups according to the abnormality rate. Fifty-two percent (13/25) had one third or less abnormal first polar bodies (subgroup 1), 36% (9/25) had between 1/3 and 2/3 abnormal first polar bodies (subgroup 2) and 12% (3/25) had 2/3 or more abnormal first polar bodies (subgroup 3). Altogether, 12 patients had more than 1/3 abnormal PB1.
Seventy eight abnormalities were retrieved, aneuploidy mechanism frequencies were similar with 35 (44.9%) meiotic non disjunction (MND) and 43 (55.1%) premature sepapration of sister chromatids (PSSC).
Incidence of chromosome alteration in recurrent implantation failure
All together, taking into account the 25 couples who had both spermatozoa and polar body analysis, 32% of couples (8/25) had no particular chromosomal risk in gametes, 60% (15/25) presented an increased sperm (>2%) or oocyte (>1/3) aneuploidy rate, and 8% (2/25) had both.
Assisted reproduction
A total of 229 oocytes showing the first polar body were retrieved (median 6), and 198 (89.4%) could be biopsied. Of these 198 first polar bodies, 174 (92.1%) were analyzed by FISH. Four (1.7%) oocytes were lysed. Spermatozoa were injected into 165 oocytes, 113 with normal first polar body FISH, and 52 without or with inconclusive first polar body FISH. Ninety-nine (60.0%) were fertilized, and among them 92 (92.9%) cleaved. 90 embryos were transferred (2.20 per transfer), five pregnancies (17.6% per couple, n = 28) occurred: three pregnancies in subgroup 2, and 2 in subgroup 1. Two miscarriages occurred in subgroup 2.
Discussion
Previous studies separately reported spermatozoa [19, 20], polar body [4] or embryo aneuploidy rate evaluations [9, 27, 28]. This study is the first to deal with both spermatozoa and oocyte aneuploidy rates in couples with recurrent implantation failure. Although spermatozoa aneuploidy rate is easy to explore, first polar body screening has to be restricted to women with high oocyte aneuploidy risk undergoing ICSI.
The spermatozoa aneuploidy rate of the control group was similar to rates previously observed (for review [29]). As previously reported [20, 21] spermatozoa aneuploidy rates were increased for patients with altered spermogram (respectively 2.1% and 1.6% for men with or without implantation failure) compared with control group (0.6%). This increase was observed both on gonosomes (p < 0.05) and chromosome 18 (p < 0.05) aneuploidy rates: 0.49% versus 1.25% and 1.47% for gonosomes and 0.10% versus 0.38% and 0.45% for chromosome 18. No difference was found between men with or without implantation failure (groups 2 and 3). This result differed from a previous study [19] reporting an increased spermatozoa aneuploidy rate for recurrent implantation failure patients compared with patients who received successful IVF for male indication. It should be noted that in the previous study, only ten patients were studied for each group and sperm characteristics differed, with a two fold decrease of sperm count and mobility. Considering only chromosome X, Y and 18, aneuploidy rate were quite similar for patients with successful IVF (1.39% vs 1.64%). For patients with recurrent implantation failure, aneuploidy rate was at 2.52% vs 1.97% in our study. Chromosome 18 abnormalities were as frequent as gonosomes abnormalities. These data are in contradiction with previous series where gonosomes abnormalities were more frequent than autosomes abnormalities [29].
Two patients had an aneuploidy rate above 5%; the first one was cryptozoospermic and the second one had a partial macrocephalia. Cryptozoospermia [30] and macrocephalia [31] have previously been associated with a high risk of spermatozoa aneuploidy. Since France does not allow pre-implantation genetic screening of embryos for this indication, it is only possible to offer prenatal diagnosis to assess fetal aneuploidy. High-magnification ICSI developed by Bartoov [32], could provide an alternative as it seems to give good results [33] in cases of paternal defect and recurrent implantation failure, but the technique is still under development.
For preconception screening cycles, the fertilization rate (60.0%) and cleavage rate (92.9%) were in agreement with the French FIVNAT registry data [34]. This confirms that the first polar biopsy had no deleterious effect on IVF results [4, 14]. Pregnancy rate per transfer was only 15.6%, but similar to ESHRE pre-implantation genetic diagnosis consortium data (14.6% pregnancy rate) for this indication [9]. First polar body screening is the only pre-implantation and, more precisely, preconception screening technique allowed by French legislation for recurrent implantation failure, though analysis of the complete cohort, fertilized and unfertilized oocytes, is possible. However, due to time limitations only 76% of first polar bodies could be assessed by FISH, a proportion similar to published values (81.6% [35], 85.5% [4]), but much higher than successful oocyte karyotyping rates (less than 50% of unfertilized oocytes [36]).
The PB1 aneuploidy rate was 34.5% in the recurrent implantation failure group (group 3), below values reported in pre-implantation genetic diagnosis studies [7, 28, 37]. This study confirms that oocyte chromosomal abnormalities play a key role in certain implantation failures, but also confirms the etiologic diversity of recurrent implantation failure. A low aneuploidy rate in oocytes (≤1/3, 52% of cases) suggests that in this subgroup chromosomal factors are not the main cause of implantation failure and that other investigations such as endometrial examination are required. Molecular abnormalities at the endometrial level and abnormal embryo-endometrium interchange may also be responsible for some cases of recurrent implantation failure, and over- or under-expressed genes may be related to successful implantation. We have previously suggested [4] that chromosomal malsegregation seems to be involved in 48% of cases of recurrent implantation failure, following investigation of five chromosomes among the 23 pairs that can malsegregate. The three (12%) patients diagnosed with more than 2/3 oocytes showing abnormal FISH results may produce only aneuploid oocytes, and oocyte donation, adoption or a spontaneous cycle should be discussed.
In order to study the gamete aneuploidy incidence, two cut-off rates have been defined: 2% for spermatozoa; 1/3 for the polar bodies, comparable to published categories [29, 38]. No control patient had a sperm aneuploidy rate above 2%, and 1/3 for polar bodies accords with Pellestor [36] who found 22.1% aneuploid oocytes in the general IVF population. Of 25 couples in our study, one third had no obvious gametic aneuploidy rate modification and other investigations of the recurrent implantation failure are required [13, 39]. For example, endometrial receptivity evaluation by three-dimensional power Doppler ultrasound vascularity testing coupled with cytokines mRNA expression assay could be performed [40]. Blastocyst transfer or assisted hatching, or co-cultures have been performed but these have not yet been shown to be of benefit to patients.
Approximately two thirds of the patients had an increased gametic aneuploidy rate, which involved spermatozoa only (20%), oocyte only (40%), or both (8%). In group of women with an oocyte aneuploidy rate between 1/3 and 2/3, two miscarriages occurred for three pregnancies obtained, possibly linked to an embryo aneuploidy involving a chromosome that was not tested in our protocol. Studies using a CGH approach [41], argue for a preferential participation of chromosome X and the smaller autosomes in aneuploidy, not all of them having been screened here.
For five couples (20%), the abnormality rate was very high, up to 5% in spermatozoa (two men) or above 2/3 in polar bodies (three women). In those situations a major meiotic defect is very likely and this condition alone probably explains the recurrent implantation failure.
Concerning aneuploidy mechanism, frequencies were similar, for meiotic non disjunction and premature separation of sister chromatids, as previously observed in this indication [11].
Conclusion
This study confirmed the previously reported multifactor origin of recurrent implantation failure [13, 39], but also the key importance of aneuploidy (68% of cases), although 32% of couples had normal aneuploidy rates. Gametic aneuploidy screening in recurrent implantation failure seems to be necessary, using preconception screening and FISH on spermatozoa in countries like in France, Germany or Italy where pre-implantation genetic screening is not allowed. Gametic aneuploidy screening results will probably influence medical recommendations for patients with recurrent implantation failure in thoses countries.
References
Griffin DK. The incidence, origin, and etiology of aneuploidy. Int Rev Cytol. 1996;167:263–96. doi:10.1016/S0074-7696(08)61349-2.
Pellestor F. Frequency and distribution of aneuploidy in human female gametes. Hum Genet. 1991;86(3):283–8. doi:10.1007/BF00202410.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2(4):280–91. doi:10.1038/35066065.
Vialard F, Petit C, Bergere M, Gomes DM, Martel-Petit V, Lombroso R, et al. Evidence of a high proportion of premature unbalanced separation of sister chromatids in the first polar bodies of women of advanced age. Hum Reprod. 2006;21(5):1172–8. doi:10.1093/humrep/dei484.
Kuliev A, Cieslak J, Ilkevitch Y, Verlinsky Y. Chromosomal abnormalities in a series of 6,733 human oocytes in preimplantation diagnosis for age-related aneuploidies. Reprod Biomed Online. 2003;6(1):54–9.
Pellestor F, Andreo B, Arnal F, Humeau C, Demaille J. Maternal aging and chromosomal abnormalities: new data drawn from in vitro unfertilized human oocytes. Hum Genet 2003;112(2):195–203.
Gianaroli L, Magli MC, Ferraretti AP, Munne S. Preimplantation diagnosis for aneuploidies in patients undergoing in vitro fertilization with a poor prognosis: identification of the categories for which it should be proposed. Fertil Steril. 1999;72(5):837–44. doi:10.1016/S0015-0282(99)00377-5.
Kahraman S, Benkhalifa M, Donmez E, Biricik A, Sertyel S, Findikli N, et al. The results of aneuploidy screening in 276 couples undergoing assisted reproductive techniques. Prenat Diagn. 2004;24(4):307–11. doi:10.1002/pd.842.
Sermon KD, Michiels A, Harton G, Moutou C, Repping S, Scriven PN, et al. ESHRE PGD consortium data collection VI: cycles from January to December 2003 with pregnancy follow-up to October 2004. Hum Reprod. 2007;22(2):323–36. doi:10.1093/humrep/del402.
Mantzouratou A, Mania A, Fragouli E, Xanthopoulou L, Tashkandi S, Fordham K, et al. Variable aneuploidy mechanisms in embryos from couples with poor reproductive histories undergoing preimplantation genetic screening. Hum Reprod. 2007;22(7):1844–53. doi:10.1093/humrep/dem102.
Vialard F, Lombroso R, Bergere M, Gomes DM, Hammoud I, Bailly M, et al. Oocyte aneuploidy mechanisms are different in two situations of increased chromosomal risk: older patients and patients with recurrent implantation failure after in vitro fertilization. Fertil Steril. 2007;87(6):1333–9. doi:10.1016/j.fertnstert.2006.11.042.
Pagidas K, Ying Y, Keefe D. Predictive value of preimplantation genetic diagnosis for aneuploidy screening in repeated IVF-ET cycles among women with recurrent implantation failure. J Assist Reprod Genet. 2008;25(2–3):103–6. doi:10.1007/s10815-008-9200-y.
Urman B, Yakin K, Balaban B. Recurrent implantation failure in assisted reproduction: how to counsel and manage. B. Treatment options that have not been proven to benefit the couple. Reprod Biomed Online. 2005;11(3):382–91.
Montag M, van der Ven K, Dorn C, van der Ven H. Outcome of laser-assisted polar body biopsy and aneuploidy testing. Reprod Biomed Online. 2004;9(4):425–9.
Hassold T, Abruzzo M, Adkins K, Griffin D, Merrill M, Millie E, et al. Human aneuploidy: incidence, origin, and etiology. Environ Mol Mutagen. 1996;28(3):167–75. doi:10.1002/(SICI)1098-2280(1996)28:3<167::AID-EM2>3.0.CO;2-B.
Nicolaidis P, Petersen MB. Origin and mechanisms of non-disjunction in human autosomal trisomies. Hum Reprod. 1998;13(2):313–9. doi:10.1093/humrep/13.2.313.
Van Steirteghem A, Bonduelle M, Devroey P, Liebaers I. Follow-up of children born after ICSI. Hum Reprod Update. 2002;8(2):111–6. doi:10.1093/humupd/8.2.111.
Liebaers I, Bonduelle M, Van Assche E, Devroey P, Van Steirteghem A. Sex chromosome abnormalities after intracytoplasmic sperm injection. Lancet. 1995;346(8982):1095. doi:10.1016/S0140-6736(95)91768-3.
Petit FM, Frydman N, Benkhalifa M, Le Du A, Aboura A, Fanchin R, et al. Could sperm aneuploidy rate determination be used as a predictive test before intracytoplasmic sperm injection? J Androl. 2005;26(2):235–41.
Rubio C, Gil-Salom M, Simon C, Vidal F, Rodrigo L, Minguez Y, et al. Incidence of sperm chromosomal abnormalities in a risk population: relationship with sperm quality and ICSI outcome. Hum Reprod. 2001;16(10):2084–92. doi:10.1093/humrep/16.10.2084.
Calogero AE, Burrello N, De Palma A, Barone N, D’Agata R, Vicari E. Sperm aneuploidy in infertile men. Reprod Biomed Online. 2003;6(3):310–7.
Guthauser B, Vialard F, Dakouane M, Izard V, Albert M, Selva J. Chromosomal analysis of spermatozoa with normal-sized heads in two infertile patients with macrocephalic sperm head syndrome. Fertil Steril. 2006;85(3):750 e5–750 e7.
Devillard F, Metzler-Guillemain C, Pelletier R, DeRobertis C, Bergues U, Hennebicq S, et al. Polyploidy in large-headed sperm: FISH study of three cases. Hum Reprod. 2002;17(5):1292–8. doi:10.1093/humrep/17.5.1292.
Rives N, Mousset-Simeon N, Mazurier S, Mace B. Primary flagellar abnormality is associated with an increased rate of spermatozoa aneuploidy. J Androl. 2005;26(1):61–9.
Dam AH, Feenstra I, Westphal JR, Ramos L, van Golde RJ, Kremer JA. Globozoospermia revisited. Hum Reprod Update, 2006.
Ditzel N, El-Danasouri I, Just W, Sterzik K. Higher aneuploidy rates of chromosomes 13, 16, and 21 in a patient with globozoospermia. Fertil Steril. 2005;84(1):217–8. doi:10.1016/j.fertnstert.2005.01.109.
Gianaroli L, Magli MC, Ferraretti AP, Tabanelli C, Trengia V, Farfalli V, et al. The beneficial effects of preimplantation genetic diagnosis for aneuploidy support extensive clinical application. Reprod Biomed Online. 2005;10(5):633–40.
Findikli N, Kahraman S, Saglam Y, Beyazyurek C, Sertyel S, Karlikaya G, et al. Embryo aneuploidy screening for repeated implantation failure and unexplained recurrent miscarriage. Reprod Biomed Online. 2006;13(1):38–46.
Shi Q, Martin RH. Aneuploidy in human spermatozoa: FISH analysis in men with constitutional chromosomal abnormalities, and in infertile men. Reproduction. 2001;121(5):655–66. doi:10.1530/rep.0.1210655.
Gianaroli L, Magli MC, Cavallini G, Crippa A, Nadalini M, Bernardini L, et al. Frequency of aneuploidy in sperm from patients with extremely severe male factor infertility. Hum Reprod, 2005.
Machev N, Gosset P, Viville S. Chromosome abnormalities in sperm from infertile men with normal somatic karyotypes: teratozoospermia. Cytogenet Genome Res. 2005;111(3–4):352–7. doi:10.1159/000086910.
Bartoov B, Berkovitz A, Eltes F, Kogosovsky A, Yagoda A, Lederman H, et al. Pregnancy rates are higher with intracytoplasmic morphologically selected sperm injection than with conventional intracytoplasmic injection. Fertil Steril. 2003;80(6):1413–9. doi:10.1016/j.fertnstert.2003.05.016.
Hazout A, Dumont-Hassan M, Junca AM, Cohen Bacrie P, Tesarik J. High-magnification ICSI overcomes paternal effect resistant to conventional ICSI. Reprod Biomed Online. 2006;12(1):19–25.
Verlinsky Y, Cieslak J, Ivakhnenko V, Evsikov S, Wolf G, White M, et al. Prevention of age-related aneuploidies by polar body testing of oocytes. J Assist Reprod Genet. 1999;16(4):165–9. doi:10.1023/A:1020304621338.
Pellestor F, Andreo B, Arnal F, Humeau C, Demaille J. Mechanisms of non-disjunction in human female meiosis: the co-existence of two modes of malsegregation evidenced by the karyotyping of 1397 in-vitro unfertilized oocytes. Hum Reprod. 2002;17(8):2134–45. doi:10.1093/humrep/17.8.2134.
Caglar GS, Asimakopoulos B, Nikolettos N, Diedrich K, Al-Hasani S. Preimplantation genetic diagnosis for aneuploidy screening in repeated implantation failure. Reprod Biomed Online. 2005;10(3):381–8.
Pang MG, Hoegerman SF, Cuticchia AJ, Moon SY, Doncel GF, Acosta AA, et al. Detection of aneuploidy for chromosomes 4, 6, 7, 8, 9, 10, 11, 12, 13, 17, 18, 21, X and Y by fluorescence in-situ hybridization in spermatozoa from nine patients with oligoasthenoteratozoospermia undergoing intracytoplasmic sperm injection. Hum Reprod. 1999;14(5):1266–73. doi:10.1093/humrep/14.5.1266.
Margalioth EJ, Ben-Chetrit A, Gal M, Eldar-Geva T. Investigation and treatment of repeated implantation failure following IVF-ET. Hum Reprod. 2006;21(12):3036–43. doi:10.1093/humrep/del305.
Ledee N, Chaouat G, Serazin V, Lombroso R, Dubanchet S, Oger P, et al. Endometrial vascularity by three-dimensional power Doppler ultrasound and cytokines: a complementary approach to assess uterine receptivity. J Reprod Immunol. 2008;77(1):57–62. doi:10.1016/j.jri.2007.07.006.
Fragouli E, Wells D, Thornhill A, Serhal P, Faed MJ, Harper JC, et al. Comparative genomic hybridization analysis of human oocytes and polar bodies. Hum Reprod. 2006;21(9):2319–28. doi:10.1093/humrep/del157.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vialard, F., Hammoud, I., Molina-Gomes, D. et al. Gamete cytogenetic study in couples with implantation failure: aneuploidy rate is increased in both couple members. J Assist Reprod Genet 25, 539–545 (2008). https://doi.org/10.1007/s10815-008-9258-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-008-9258-6