Abstract
Purpose
To evaluate pre-implantation genetic testing for aneuploidy (PGT-A) outcomes in patients without infertility compared to infertile patients.
Methods
We performed a retrospective cohort study of all patients without an infertility diagnosis (“fertile” patients) who utilized PGT-A at a large university-affiliated fertility center between 2016 and 2021. Fertile patients were 1-to-3 matched to infertile controls by age and number of oocytes retrieved. The primary outcome was blastocyst aneuploidy rate. Secondary outcomes included ovarian reserve markers, laboratory outcomes, and other PGT-A outcomes [rates of euploidy, mosaicism, and potentially transferrable (euploid + mosaic) embryos].
Results
283 fertile and 849 infertile patients were included. Median age, anti-Mullerian hormone, and day 2 estradiol levels were equivalent among groups; day 2 follicle-stimulating hormone levels were higher in fertile patients (6.9 vs. 6.5 IU/mL, p < 0.01). The aneuploidy rate was similar among fertile and infertile patients (33.7% vs. 31.8%, p = 0.11); the euploidy rate was higher (50.8% vs. 47.0%, p < 0.01), and the mosaicism rate was lower in fertile patients (13.3% vs. 19.2%, p < 0.01). The rate of transferrable embryos was similar among groups (64.0% vs. 66.3%, p = 0.07), as was the percentage of patients yielding ≥ 1 euploid embryo (90.1% vs. 87.3%, p = 0.25). When controlling for significant covariates, multiple linear regression showed that aneuploidy rate was equivalent in both cohorts.
Conclusion
Aneuploidy rate was similar in fertile and infertile patients. Fertile patients had slightly higher euploidy and lower mosaicism than infertile patients. Still, compared to fertile patients, infertile patients had equivalent rates of transferrable embryos and were just as likely to yield ≥ 1 euploid embryo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chromosomal abnormalities are the leading cause of early pregnancy loss and a significant contributor to assisted reproductive technology (ART) failure [1,2,3,4]. It is well established that embryonic aneuploidy increases with advanced maternal age (AMA) due to increased meiotic errors in oocyte development [2, 3, 5, 6]. In some studies, utilization of pre-implantation genetic testing for aneuploidy (PGT-A) to select for euploid embryos has been shown to reduce miscarriage rates [7, 8] and increase live birth rates (LBR) per transfer in patients at increased risk of embryonic aneuploidy [5, 7, 9]; however, the benefits of routine PGT-A utilization in all ART patients are contested [10]. While PGT-A was initially suggested for select groups believed to have increased aneuploidy rates, including those with AMA, recurrent pregnancy loss (RPL), or previous aneuploid conception, the use of PGT-A has steadily risen, with PGT-A now increasingly offered to patients seeking reproductive assistance regardless of age or diagnosis [9]. Increasingly, this includes fertile patients or patients without infertility diagnoses, who may pursue PGT-A while undergoing elective or medically indicated fertility preservation, pre-implantation genetic testing for monogenic disorders (PGT-M), or sex selection, or as a way to minimize time to live birth or reduce rates of miscarriage.
Given the established association between AMA and aneuploidy, maternal age is the primary prognostic factor used to counsel PGT-A patients regarding the expected yield and percentage of euploid embryos [6]. However, as the majority of patients who undergo ART with PGT-A have infertility diagnoses, the incidence of aneuploidy reported in the literature and by specific institutions is largely extrapolated from infertile patients and thus may not reflect the general population [11, 12]. Analyses of euploidy in embryos derived from donor oocytes offer insight into the non-infertile population, but often lack data from patients aged ≥ 35 years [13, 14]. Few studies have addressed whether the estimated incidence of aneuploidy at each age is applicable to patients without infertility and current data conflicts. One study assessed aneuploidy rate in a small group of infertile compared to presumed fertile patients, stratified by age < 35 years or ≥ 35 years; these investigators found no difference in the proportion of aneuploid blastocysts among groups [11]. In contrast, a larger subsequent study that matched fertile and infertile patients by age found a significantly higher aneuploidy rate among infertile patients with RPL, previous ART failure, and prior aneuploid pregnancies, but not among infertile patients with male factor or unexplained infertility, compared to their counterpart fertile controls [12]. Given the paucity of data, it is unclear whether aneuploidy rates in infertile patients are comparable to aneuploidy rates in presumed fertile patients of the same age or whether the diagnosis of infertility confers an increased risk of aneuploidy. Additionally, no studies identified in the literature address the rate of mosaicism among these populations, which is increasingly important as mosaic embryos are increasingly considered transferrable, and mosaic embryo transfers are becoming more common [15, 16]. Therefore, the objective of this study was to compare ploidy rates in presumed fertile and infertile ART patients who opted for PGT-A.
Materials and methods
Design
With New York University Institutional Review Board approval (s13-00389), we conducted a retrospective cohort study of patients who underwent ART with PGT-A at the New York University Langone Fertility Center between January 1, 2016, and November 30, 2021. The study period was chosen given changes in PGT-A methodology at our institution, with a shift from array comparative genomic hybridization to next-generation sequencing (NGS) in 2016.
Subjects
First, we reviewed “fertile” patients who underwent ART with PGT-A during the study period. Fertile patients were defined as those who met all of the following criteria: (1) did not hold a diagnosis of infertility or RPL, (2) were not referred to our center for an infertility work-up, and (3) did not receive previous fertility treatment. These patients included those undergoing ART for planned embryo banking and/or PGT-M. Fertile patients pursuing ART solely for sex selection were not included, given the rarity of these patients at our institution. Embryos derived from donor oocytes were not included in the fertile cohort. Only the first ART cycle from each fertile patient was included for analysis. Fertile patients were excluded if their first ART cycle at our institution did not utilize PGT-A or was not performed within the study period.
These fertile patients were one-to-three matched to patients with infertility diagnoses (“infertile patients”). Only the first ART cycle from each infertile patient was included for analysis, and infertile patients had the same exclusion criteria as fertile patients. Matching parameters were (1) patient age at ART cycle start and (2) number of total oocytes retrieved, grouped by interquartile ranges as defined by the fertile cohort’s total oocyte yield. Interquartile ranges of total oocytes retrieved in the fertile cohort were 0 to 11, 12 to 17, 18 to 24, and more than 25 oocytes.
Data collection and outcomes
All demographics and variables were collected from the electronic medical record in January 2022. Variables collected included age at initial ART cycle start (years), body mass index (BMI) (kg/m2), early follicular estradiol (E2) (pg/mL), follicle-stimulating hormone (FSH) (IU/mL), and anti-Mullerian hormone (AMH) (ng/mL) prior to cycle start, total gonadotropin dose (IUs), type of gonadotropins used (FSH and human menopausal gonadotropin (HMG)), number of stimulation days, number of total oocytes and metaphase 2 oocytes (MIIs) retrieved, number of 2-pronuclear (2PN) zygotes, number of blastocysts, number of blastocysts biopsied, and number of euploid, aneuploid, mosaic, and no diagnosis embryos.
For fertile patients, we obtained the reason for undergoing PGT-A, categorized as embryo banking or PGT-M for single gene disorder. For infertile patients, infertility diagnosis was ascertained by review of electronic medical records. Infertility diagnoses were characterized as male factor, ovulation disorder (including polycystic ovarian syndrome, hypothalamic amenorrhea, and unspecified ovulation disorders), endometriosis, tubal factor, uterine factor, diminished ovarian reserve (DOR), RPL, unexplained, or multifactorial.
Our primary outcome was aneuploidy rate, defined as the number of aneuploid embryos divided by the number of biopsied blastocysts. Secondary outcomes included the number and percentage of MIIs, 2PN fertilization rate, blastocyst formation rate, number of biopsied blastocysts, number of aneuploid embryos, number and rate of euploid embryos, number and rate of mosaic embryos, and number and rate of potentially transferrable embryos (defined as euploid plus mosaic embryos). Aneuploid embryos were defined as embryos with at least one whole chromosome full copy number aneuploidy or at least one full segmental aneuploidy. Mosaic embryos were defined as embryos with at least one whole chromosome or segmental intermediate copy number (reported as “mosaic”), but no whole chromosome full copy number or segmental aneuploidies. BMI, AMH, early follicular FSH and E2, total gonadotropin dose, and number of stimulation days were also compared.
Subgroup analyses were performed examining differences in the primary and secondary outcomes among patients aged < 35 years compared to patients aged ≥ 35 years.
Ovarian stimulation and laboratory techniques
Ovarian stimulation protocols were chosen by the treating physician based on age, ovarian reserve, and semen parameters. All patients received injectable gonadotropins: FSH and/or HMG. One of three ovarian stimulation protocol types was employed: gonadotropin-releasing hormone (GnRH) antagonist, GnRH antagonist with clomiphene citrate, or microdose leuprolide acetate flare. Oocyte retrieval was performed via ultrasound-guided transvaginal aspiration 35 h after trigger administration.
Conventional insemination was used for all cycles, which is standard in our lab, except where intracytoplasmic sperm injection (ICSI) was indicated based on semen parameters or male history; all PGT-M cycles used ICSI. Embryos then underwent trophectoderm biopsy for PGT-A after 5–7 days of culture. With the exception of select PGT-M cases, all PGT-A was performed at a single laboratory that used NGS alone before September 2019 and a combined NGS and single nucleotide polymorphism (SNP) approach after this date. The select PGT-M cases underwent single nucleotide polymorphism (SNP)-based PGT-A at another laboratory.
Analysis
Continuous variables were assessed for normality using the Kolmogorov-Smirnoff test, with all determined to be nonparametric. Therefore, Mann–Whitney U and Kruskal–Wallis tests were used to compare continuous variables. Fisher’s exact or chi-squared tests were used for categorical variables. Multiple linear regression was performed for modeling and adjustment of significant covariates to evaluate the outcome of the aneuploidy rate. An alpha error of 0.05 was considered statistically significant. Results are reported as median with interquartile ranges (IQRs) or percentages unless otherwise indicated.
Results
A total of 283 fertile patients met the inclusion criteria. These 283 fertile patients were matched to 849 infertile patients.
In the fertile group, the most common reason for undergoing PGT-A was embryo banking (n = 180, 63.6%), followed by PGT-M for single gene disorders (n = 103, 36.4%). Of the infertile patients, 695 (81.9%) had a single infertility diagnosis, with the most common diagnoses being ovulation disorder (210, 24.7%), male factor (186, 21.9%), DOR (108, 12.7%), tubal factor (67, 7.9%), endometriosis (42, 5.0%), unexplained (40, 4.7%), RPL (26, 3.1%), and uterine factor (22, 2.6%); the remaining 148 patients (17.4%) had two or more infertility diagnoses, with the most common shared diagnoses being ovulation disorder (69, 46.6%), male factor (61, 41.2%), tubal factor (54, 36.5%), and DOR (36, 24.3%).
In the infertile group, all PGT-A was performed at a single laboratory that used either NGS alone or a combined NGS/SNP approach (based on the date of the test); 94.4% of fertile patient cycles were also performed at this lab; the remaining 5.6% of fertile patient cycles all involved PGT-M, and PGT-A for these cycles was performed a different laboratory that uses SNP alone.
Table 1 displays patient demographics, hormonal markers of ovarian reserve, and ART cycle parameters in the fertile and infertile cohorts. Median age, AMH, and basal E2 were equivalent in both groups; in the fertile group, median BMI was slightly, but significantly, lower (22.1 vs. 22.5, p < 0.05) and basal FSH was slightly, but significantly, higher (6.9 vs. 6.5 IU/mL, p < 0.01) compared to the infertile cohort. Of note, AMH, FSH, and E2 were not available for every patient in our study (see Table 1 for details). The fertile cohort received a significantly higher median total gonadotropin dose than the infertile cohort (3450 vs. 3150 IUs, p < 0.01), but the median number of stimulation days was equivalent between the two groups (10 vs. 10, p = 0.21). There were no significant differences among stimulation protocols used in the two cohorts.
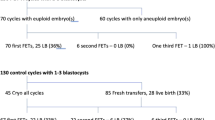
Table 2 summarizes ART and PGT-A outcomes in the two cohorts. Among fertile and infertile cohorts, there were no differences in the median number of total oocytes (17.0 vs. 17.0, p = 0.89) or MII oocytes (13.0 vs. 13.0, p = 0.96), mature oocyte rate (77.6% vs. 78.9%, p = 0.06), blastocyst formation rate (62.5% vs. 60.9%, p = 0.10), or the median number of biopsied blastocysts (6.0 vs. 6.0, p = 0.29); the 2PN fertilization rate was minimally, but significantly, higher in the fertile group (77.8 vs. 76.3%, p < 0.05).
In total, 2057 and 5918 biopsied blastocysts were evaluated in the fertile and infertile cohorts, respectively. The median number of aneuploid embryos was equivalent between the two groups (2.0 vs. 2.0, p = 0.27). The median number of euploid embryos produced was 3.0 in the fertile group (range: 0.0 to 14.0; IQR: 1.5 to 5.0) and 3.0 in the infertile group (range: 0.0 to 19.0; IQR: 1.0 to 5.0), with a slightly greater mean number of euploid embryos produced in the fertile group (3.7 vs. 3.3, p < 0.01). The median number of mosaic embryos produced was 1.0 in both groups, with a trend toward fewer mosaic embryos in the fertile group (mean 1.0 vs. 1.3, p < 0.01). There was no significant difference in the median number of potentially transferrable embryos among groups (4.0 vs. 4.0; p = 0.59). There were no differences in the median number of no diagnosis embryos (0.0 vs. 0.0, p = 0.43) produced in the two cohorts.
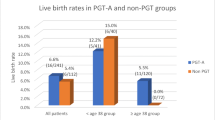
As shown in Fig. 1, there was no significant difference in aneuploidy rates among fertile and infertile patients (33.7%, 95% CI 31.7–30.6% vs. 31.8%, 95% CI 30.6–33.0%). Fertile patients yielded a slightly but significantly higher rate of euploid embryos among biopsied blastocysts compared to the infertile group, with a 50.8% (95% CI 48.6–52.9%) euploidy rate in fertile patients and 47.0% (95% CI 45.8–48.3%) euploidy rate in infertile patients (p < 0.01). Fertile patients also had a significantly lower mosaicism rate compared to infertile patients (13.3%, 95% CI 11.8–14.7% vs. 19.2%, 95% CI 18.2–20.2%). When considering the rate of potentially transferrable embryos (euploid plus mosaic embryos), there was no significant difference among cohorts, with a 64.0% (95% CI 62.0–66.1%) rate in the fertile cohort and a 66.3% (95% CI 65.1–67.5%) rate in the infertile cohort (p = 0.07). The percentage of patients who produced at least one euploid embryo was also similar in the fertile and infertile cohorts (90.1% vs. 87.3%, p = 0.25). When a multiple linear regression model was performed to control for significant covariates including total gonadotropins dose, BMI, day 2 FSH, and 2PN fertilization rate, fertile versus infertile continued to predict a statistically similar percentage of aneuploid embryos produced (B = − 0.487, p = 0.81).
Pre-implantation genetic testing for aneuploidy outcomes in fertile and infertile cohorts. Notes: (1) * denotes a significant difference between the fertile and infertile cohorts in this outcome (p < 0.01). (2) Fertile cohort, n = 283 patients and 2057 total biopsied blastocysts; infertile cohort, n = 849 patients and 5918 total biopsied blastocysts
Table 3 demonstrates PGT-A outcomes among patients < 35 years and ≥ 35 years. The similar aneuploidy rate in fertile and infertile patients held true in patients ≥ 35 years, but not in patients < 35 years. In patients < 35 years, there was a slightly higher aneuploidy rate in the fertile cohort (29.7%, CI 27.2–32.3% vs. 26.2%, CI 24.8–27.6%, p < 0.05). However, when adjusting for significant covariates in the < 35 years group (total gonadotropin dose, total IUs of FSH, AMH, and BMI), multiple linear regression showed that fertile vs. infertile did not predict the percentage of aneuploid embryos (B = − 1.009, p = 0.66). There were no significant covariates for which to control in the ≥ 35 years group. The higher euploidy rate and lower mosaicism rate among fertile patients held true in both patients < 35 years and ≥ 35 years. The percentage of patients with at least one euploid embryo produced was equivalent between the fertile and infertile cohorts in patients < 35 years (94.0% vs. 92.1%, p = 0.49) and in patients ≥ 35 years (84.5% vs. 80.4%, p = 0.32).
Discussion
Fertile ART patients had a similar aneuploidy rate, but a slightly higher euploidy rate and a slightly lower mosaicism rate than infertile ART patients. Notably, we found equivalent rates of potentially transferable embryos among fertile and infertile groups, accounting for the higher rate of mosaicism seen in the infertile cohort. To our knowledge, this is the largest study to evaluate PGT-A outcomes in fertile compared to infertile patients that controls for both patient age and number of oocytes retrieved. Our findings challenge prior studies that demonstrated higher aneuploidy rates [12] and equivalent euploidy rates [11] among infertile patients.
To our knowledge, this is the first study to address mosaicism rates in fertile compared to infertile patients. While several studies have shown that mosaic embryos can lead to successful live births [17, 18], the decision to transfer mosaic embryos is still debated, given the small, but non-zero risk of genetic abnormalities in offspring and the increased rates of implantation failure and miscarriage [19, 20]. Higher mosaicism rates demonstrated in our infertile cohort could align with their diagnoses of infertility, as some studies have shown that mosaic blastocysts have reduced reproductive potential and thus higher rates of mosaicism may contribute to infertility. However, non-selection studies have also demonstrated that low- and medium-grade mosaic embryos perform similarly to euploid embryos [21]: When regarding mosaic embryos as potentially transferrable embryos, our fertile and infertile cohorts had equivalent rates of transferrable embryos. While we report slightly higher rates of euploidy in fertile patients (50.6%, 95% CI 48.6–52.9%; compared to 47.0%, 95% CI 45.8–48.3%, p < 0.05), our finding of equivalent rates of transferrable embryos between the two groups suggests that a diagnosis of infertility may not in fact be associated with a lower rate of embryos that can result in live birth. When considering mosaic embryos as transferrable embryos, our results suggest clinically similar PGT-A outcomes among fertile and infertile patients. Therefore, our findings strengthen the validity of age-based PGT-A outcomes (reported in the literature or by specific institutions) as a counseling tool for fertile patients, despite these numbers being based on data derived from largely infertile patients [2, 3, 5, 6]. This information can be helpful to fertile ART patients when they are deciding how many ART cycles to pursue and how many embryos they would like to bank. Further research is warranted to evaluate the significance of the higher mosaicism rate among infertile patients.
The median number of MIIs, mature oocyte rate, blastocyst formation rate, and number of blastocysts biopsied did not differ between the fertile and infertile groups; 2PN fertilization rate was statistically higher in the fertile group (77.8% vs. 76.3%, p < 0.05), but this difference is unlikely to be clinically significant. The similar ART laboratory outcomes in the two cohorts suggest that a diagnosis of infertility does not have a significant negative impact on oocyte maturity, fertilization, or blastulation. While there were trends toward a greater mean number of euploid embryos (3.7 vs. 3.3, p < 0.05) and a lesser mean number of mosaic embryos (1.0 vs. 1.3, p < 0.01) in the fertile cohort, these trends are likely clinically insignificant given that the median number of aneuploid, euploid, and mosaic embryos did not differ between the fertile and infertile groups. Importantly, the median number of transferrable embryos was equivalent in fertile and infertile patients.
Compared to infertile patients aged < 35 years, fertile patients aged < 35 years had a slightly higher aneuploidy rate (29.7%, 95% CI 27.1–32.2% vs. 26.2%, 95% CI 24.8–27.6%, p < 0.05); however, after multiple linear regression was performed, it was found that fertile vs. infertile did not predict a difference in aneuploidy rate in this age group. Similarly, in patients aged ≥ 35 years, fertile patients had an equivalent aneuploidy rate. Mosaicism rates were slightly but significantly lower, and euploidy rates were slightly but significantly higher among fertile patients aged < 35 years and ≥ 35 years compared to infertile patients of the same age.
Compared to infertile patients, fertile patients had slightly, but significantly, lower BMI. This clinically insignificant difference likely did not influence ploidy yields, especially given that multiple studies have demonstrated no association between blastocyst euploidy and BMI [22, 23]. Fertile patients also received a significantly higher total gonadotropin dose compared to infertile patients, with a significantly higher dose of FSH (but not HMG) administered to fertile patients. Existing data on gonadotropin dose and ploidy is conflicting, with most studies finding no association [24,25,26]. Interestingly, several studies have found that higher total gonadotropin dose and mean daily FSH dose is associated with a higher rate of aneuploidy [27, 28], inconsistent with our results. Still, further investigation is needed to determine whether milder ovarian stimulation has an effect on PGT-A outcomes.
One major strength of this study is our relatively large sample size. Our study is one of the largest evaluating oocyte and embryo quality in fertile and infertile patients. Another strength is the exclusion of repeat ART cycles from the same patient: By including only the first ART cycle, we avoided repeated measure bias as well as potential confounding effects that may result from using data from prior cycles to modify protocols and trigger decisions. Our study is also unique in that it stratified results by age and matched patients by both age and number of oocytes retrieved, which allowed us to control for the effects of age and ovarian reserve.
An a priori power analysis revealed that a total sample size of 2740 biopsied embryos (n = 685 embryos from fertile patients and n = 2055 embryos from infertile patients) would detect a 5% difference in aneuploidy rate with 80% power, with an alpha error of 0.05. Therefore, we can conclude that we would be powered to detect a 5% or more difference in aneuploidy rates between the fertile and infertile cohorts. In addition, we were powered to detect a 5% or more difference in aneuploidy between the two cohorts in the < 35-year and ≥ 35-year subgroups.
One limitation of our study was the high incidence of multifactorial infertility among patients in the infertile group, which limited analysis of embryo ploidy by diagnostic subgroup. The presence of multiple infertility diagnoses is common in our institution, and patients with these diagnoses were not excluded as they represented a large proportion of our patient population. Our study was also limited to patients from a single high-volume urban academic institution. Our results therefore may not be generalizable to fertile patients with different demographics. Further studies with larger sample sizes from a wider range of geographic locations and center types are needed to validate our findings. Finally, as ploidy rates differ between PGT-A laboratories based on different thresholds for detecting euploidy/mosaicism/aneuploidy, our reported ploidy rates may differ from those reported by groups that use other PGT-A laboratories.
Importantly, our fertile study population is likely more representative of the general population, in which one in eight couples experience infertility, than of a patient population with proven fertility. Furthermore, patients may be more likely to pursue fertility preservation with embryo banking if they are found to have low AMH at a routine gynecology visit or initial fertility consultation; thus, our fertile group may, in fact, represent patients with lower fertility than the general population. Because our fertile cohort likely contains some infertile patients, the aneuploidy rate in our fertile cohort could be artificially elevated.
In conclusion, our study provides a valuable resource for counseling fertile patients without an infertility diagnosis about their predicted PGT-A outcomes. Currently, counseling of patients undergoing ART with PGT-A is focused on maternal age-based predictions, using data largely gathered from patients undergoing IVF due to infertility. Our study provides evidence that patients without a diagnosis of infertility may have a similar percentage of aneuploid embryos among biopsied embryos as their infertile counterparts. Patients seeking ART for reasons other than infertility can, therefore, be reassured that the percentage of transferrable embryos they obtain may be comparable to current age-based estimates. Further research is warranted to investigate the significance of the higher mosaicism rate seen in our infertile cohort, which confers an overall equivalent rate of potentially transferable embryos compared to fertile patients. Infertile patients pursuing ART may still be reassured that they are just as likely to obtain at least one euploid embryo per cycle compared to fertile patients.
Data Availability
The data that support the findings of this study are available from the corresponding author, EAC, upon reasonable request.
References
Hodes-Wertz B, Grifo J, Ghadir S, Kaplan B, Laskin CA, Glassner M, et al. Idiopathic recurrent miscarriage is caused mostly by aneuploid embryos. Fertil Steril. 2012;98:675–80.
Marquard K, Westphal LM, Milki AA, Lathi RB. Etiology of recurrent pregnancy loss in women over the age of 35 years. Fertil Steril. 2010;94:1473–7.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2:280–91.
Pylyp LY, Spynenko LO, Verhoglyad NV, Mishenko AO, Mykytenko DO, Zukin VD. Chromosomal abnormalities in products of conception of first-trimester miscarriages detected by conventional cytogenetic analysis: a review of 1000 cases. J Assist Reprod Genet. 2018;35:265–71.
Lee H, McCulloh DH, Hodes-Wertz B, Adler A, McCaffrey C, Grifo JA. In vitro fertilization with preimplantation genetic screening improves implanation and live birth in women age 40 through 43. J Assist Reprod Genet. 2015;32:435–44.
Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101:656–63.
Pantou A, Mitrakos A, Kokkali G, Petroutsou K, Tounta G, Lazaros L, Dimopoulos A, Sfakianoudis K, Pantos K, Koutsilieris M, Mavrou A, Kanavakis E, Tzetis M. The impact of preimplantation genetic testing for aneuploidies (PGT-A) on clinical outcomes in high risk patients. J Assist Reprod Genet. 2022;39:1341–9.
Simopoulou M, Sfakianoudis K, Maziotis E, et al. PGT-A: who and when? Alpha systematic review and network meta-analysis of RCTs. J Assist Reprod Genet. 2021;38:1939–57.
Roche K, Racowsky C, Harper J. Utilization of preimplantation genetic testing in the USA. J Assist Reprod Genet. 2021;38:1045–53.
Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109(3):429–436.
Taylor TH, Patrick JL, Gitlin SA, Crain JL, Wilson JM, Griffin DK. Blastocyst euploidy and implantation rates in young (<35 years) and old (≥35 years) presumed fertile and infertile patient population. Fertil Steril. 2014;102:1318–23.
Kort JD, McCoy RC, Demko Z, Lathi RB. Are blastocyst aneuploidy rates different between fertile and infertile populations? J Assist Reprod Genet. 2018;35:403–8.
Hoyos LR, Cheng CY, Brennan K, et al. Euploid rates among oocyte donors: is there an optimal age for donation? J Assist Reprod Genet. 2020;37:589–94.
Munne S, Alikani M, Ribustello L, et al. Euploidy rates in donor egg cycles significantly differ between fertility centers. Hum Reprod. 2017;32:743–9.
Leigh D, Cram DS, Rechitsky S, Handyside A, Wells D, Munne S, et al. PGDIS position statement on the transfer of mosaic embryos 2021. Reprod Biomed Online. 2022;45:19–25.
Practice Committee and Genetic Counseling Professional Group (GCPG) of the American Society for Reproductive Medicine. Clinical management of mosaic results from preimplantation genetic testing for aneuploidy (PGT-A) of blastocysts: a committee opinion. Fertil Steril. 2020;114:246–54.
Victor AR, Tyndall JC, Brake AJ, Lepkowsky LT, Murphy AE, Griffin DK, et al. One hundred mosaic embryos transferred prospectively in a single clinic: exploring when and why they result in healthy pregnancies. Fertil Steril. 2019;111:280–93.
Lee CI, Cheng EH, Lee MS, Lin PY, Chen YC, Chen CH, et al. Healthy live births from transfers of low-mosaicism embryos after preimplantation genetic testing for aneuploidy. J Assist Reprod Genet. 2020;37:2305–13.
Fragouli E, Alfarawati S, Spath K, Babariya D, Tarozzi N, Borini A, et al. Analysis of implantation and ongoing pregnancy rates following the transfer of mosaic diploid-aneuploid blastocysts. Hum Genet. 2017;136:805–19.
Zore T, Kroener LL, Wang C, Liu L, Buyalos R, Hubert G, Shamonki M. Transfer of embryos with segmental mosaicism is associated with a significant reduction in live-birth rate. Fertil Steril. 2019;111:69–76.
Capalbo A, Poli M, Rienzi L, Girardi L, Patassini C, Fabiani M, et al. Mosaic human preimplantation embryos and their developmental potential in a prospective, non-selection clinical trial. Am J Hum Genet. 2021;108(12):2238–47.
Stovezky YR, Romanski PA, Bortoletto P, Spandorfer SD. Body mass index is not associated with embryo ploidy in patients undergoing in vitro fertilization with preimplantation genetic testing. Fertil Steril. 2021;116:388–95.
Goldman KN, Hodes-Wertz B, McCulloh DH, Flom JD, Grifo JA. Association of body mass index with embryonic aneuploidy. Fertil Steril. 2015;103:744–8.
Massie JAM, Shahine LK, Milki A, Westphal L, Lathi R. Ovarian stimulation and the risk of aneuploid conceptions. Fertil Steril. 2011;95:970–2.
Barash OO, Hinckley MD, Rosenbluth EM, Ivani KA, Weckstein LN. Hum Reprod. 2017;32:2209–17.
Cascales A, Lledó B, Ortiz JA, Morales R, Ten J, Llácer J, et al. Effect of ovarian stimulation on embryo aneuploidy and mosaicism rate. Syst Biol Reprod Med. 2021;67:42–9.
Baart EB, Martini E, Eijkemans MJ, van Opstal D, Beckers NGM, Verhoeff A, et al. Milder ovarian stimulation for in-vitro fertilization reduces aneuploidy in the human preimplantation embryo: a randomized controlled trial. Hum Reprod. 2007;22:980–8.
Katz-Jaffe MG, Trounson AO, Cram DS. Chromosome 21 mosaic human preimplantation embryos predominantly arise from diploid conceptions. Fertil Steril. 2005;84:634–43.
Acknowledgements
The authors thankfully acknowledge the patients included in this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Emily A. Clarke and Asha K. Dahiya. The first draft of the manuscript was written by Emily A. Clarke, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and informed consent
This research study was conducted retrospectively from data obtained for clinical purposes. The study was performed with New York University Institutional Review Board approval (s13-00389).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clarke, E.A., Dahiya, A.K., Cascante, S.D. et al. Evaluation of pre-implantation genetic testing for aneuploidy outcomes in patients without infertility undergoing in vitro fertilization compared to infertile controls. J Assist Reprod Genet 40, 2697–2704 (2023). https://doi.org/10.1007/s10815-023-02941-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02941-6