Abstract
Objective
To study the efficacy of the aromatase inhibitor letrozole in controlled ovarian hyperstimulation (COH).
Material and methods
In this prospective simply randomized clinical trial, one hundred forty patients with unexplained infertility undergoing intrauterine insemination (IUI) therapy were randomized to receive either letrozole or clomiphene citrate (CC)-gonadotropin. The patients were selected among patients referred to one university hospital and one private infertility clinic. A letrozole dose of 5 mg/day (n = 70) was given on days 3–7 of the menstrual cycles. Clomiphen citrate a dose of 100 mg/day was given like letrozole but combined with human menopausal gonadotropin (hMG) dose of 75 IU/ml administered every day starting on day 6. Ovulation was triggered with urinary hCG (10,000 IU) when the leading follicle(s) reached 18 mm in diameter. A single IUI was performed 36 hours later. The luteal phase was supplemented with micronized progesterone vaginally. Ovarian stimulation response (E2 levels and number of follicles) was primary outcome.
Results
There were no differences in demographic characteristics between groups. The number of mature follicles (1.8 ± 0.7 vs. 2.46 ± 2.3; P = 0.042) and serum E2 level on the day of hCG (310 ± 135.4 vs. 1,670.7 ± 1021.8 pg/ml, respectively; P < 0.0001) were significantly lower in letrozole group. A significantly higher endometrial thickness was observed at the time of hCG administration in patients that received letrozole (9.7 ± 1.6 mm vs. 7.8 ± 2 mm; P < 0.001).Clinical pregnancy rates also were significantly higher in letrozole group (32.8% vs. 14.3%, respectively; P < 0.01).
Conclusion
The aromatase inhibitor letrozole appears to constitute a good alternative to CC-gonadotropin in patients with unexplained infertility undergoing COH cycles combined with IUI therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clomiphene citrate (CC) is the most commonly prescribed agent for ovulation induction for the treatment of subfertility associated with oligo-ovulation [1] and could be used as a superovulation regimen for timed intercourse or intrauterine insemination (IUI) cycles, when favorably combined with exogenous gonadotropins. Clomiphene citrate is an antiestrogenic agent resulting in a 60–85% ovulation rate and 10–20% pregnancy rate per cycle [2–6].This disparity seems to be due to the antiestrogenic mechanism of action of cc which involves lasting estrogen receptor (ER) depletion. Because of its long half-life (2 weeks), cc accumulates in the body and may have a negative effect on the quality and quantity of cervical mucus, endometrial development, which may cause implantation failure, luteal phase defects and significant thinning of the endometrium, which is dose dependent [8–10].These adverse effects of cc on the endometrium may explain in part the relatively poor pregnancy rates associated with cc despite the high rate of ovulation. Recently, aromatase inhibitor has been investigated as a potential ovulation induction agent [11].Because it does not deplete estrogen receptors in central and peripheral target tissues, it typically results in mono-ovulation and it may have no negative impact on endometrium and cervical mucus [12–13].The aromatase inhibitors have a relatively short half-life (45 h) [14] compared with CC and therefore would be eliminated from the body rapidly [15].
One prospective pilot study has been performed and the results showed that letrozole cycles have a significantly higher pregnancy rate than CC in gonadotropin-combined IUI cycles. These researches believed that their favorable outcomes could be attributed to a thicker endometrium and a lower level of E2 [16]. Another prospective pilot study showed that the use of letrozole-combined gonadotropins versus cc-gonadotropin in IUI cycles, had a significantly lower serum E2 level on the day of hCG and the number of mature follicles than CC-gonadotropin cycles. However they found comparable pregnancy rate and endometrial thickness on the day of hCG administration between the two groups [17].
The present prospective trial study is an attempt to compare and determine clinical outcomes of letrozole to that of CC-gonadotropin in patients with unexplained infertility.
Material and methods
This study was begun after obtaining consent from deputy of research and the medical ethics committee of Tehran University of Medical Science. In this simply randomized clinical trial, the patients were enrolled from Jan 2005 to 2006. One university hospital and one private infertility clinic participated in this trial.
One hundred forty infertile couples eligible for superovulation and IUI for first time were recruited. All couples with the duration of infertility that lasted one year or more underwent a routine infertility workup. Tubal patency was confirmed by hysterosalpingography in all subjects. Semen parameters were interpreted by the world health organization (1999) criteria.
The patients had several timed intercourses and were superovulated by CC with or without gonadotropins at least two times before enrollment. We excluded couples when the female age was >35 years old, having moderate endometriosis, or a basal serum FSH > 10 mIU/ml.
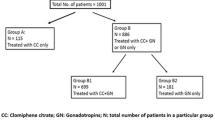
The patients were visited and examined by two gynecologists. A series of blind envelops numbered from 1 to 140 had been prepared [letrozol group (A): envelopes numbered 1–70 and CC-gonadotropin group (B): Envelopes numbered 71–140]. Each patient was invited by the clinic secretary to pull out an envelope and was placed in either the letrozole group (group A: envelopes number 1–70) or cc-gonadotropin group (group B: envelopes number 71–140) [18]. The patients in the letrozole group (Group A) received 5 mg letrozole (Femara, Novartis, Quebec, Canada) for 5 days from day 3 of their menstrual cycle. In the CC-gonadotropin group (Group B) clomiphene citrate 100 mg was given for 5 days starting from day 3 of menstrual cycle. In addition, human menopausal gonadotropin (hMG, Pergonal, Serono) 75 IU was administered every day, starting on day 6 until human chorionic gonadotropin (hCG) administration. The condition of the ovaries was determined by transvaginal ultrasonography.
Sonography was done every other day from day 10 of the cycle by a single radiologist. When mature leading follicle (s) reached>18 mm in diameter, urinary hCG (Profasi, Serono, Italy) in a dose of 10000 IU was given and IUI was performed 36–40 hours later.
The main outcome measurement was pregnancy rate. Clinical pregnancy was defined when an intrauterine gestational sac(s) was visible by ultrasonography. Our secondary outcome measurements were the number of mature follicles 18 mm or more (in diameter), serum level of E2 and endometrial thickness measured on the day of hCG administration and abortion rates.
Blood samples were collected on the day of hCG administration. The concentration of serum E 2 was measured by a radioimmunoassay (RIA) kit (TKE21, diagnostic products corporation, Los Angeles, CA).The statistician involved in this trial was blind to the kind of treatment, whereas patients and gynecologists were not blind to the kind of treatment because of known different administration methods of these two drugs. SPSS version 12.0 software was used for statistical analysis and t teat and chi-square test were used as appropriate. P value less than 0.05 was considered statistically significant.
Results
The mean age of female was 26.3 ± 4.1 years old (range, 22–35) and the mean duration of infertility was 3.66 ± 1.9 years (range, 1–9). The female age and duration of infertility were comparable between the two groups (Table 1).
The number of mature follicles and serum levels of E2 on the day of hCG administration were significantly lower in letrozole group. No cancelled cycles occurred due to excessive stimulation or occurrence of ovarian hyperstimulation syndrome. Mean endometrial thickness was significantly lower in CC group while clinical pregnancy rates were higher in letrozol group (Table 2).
Twin pregnancy was occurred in two patients of 23 pregnant women in letrozol group and two out of 10 pregnant patients in CC group. However three patients (13%) in letrozol group and one patient (10%) in CC group experienced abortion.
Discussion
The results of this study suggest that women with unexplained infertility experience higher pregnancy rate when they received letrozole in comparison with CC-gonadotropin. However, the characteristics of patients were not different between the two groups including female age, duration of infertility and infertility factor.
We found that the serum levels of E 2 and the number of mature follicles were significantly lower in the letrozole group. This concurs with the findings of a pervious report [16, 17].Therefore we believe that the pregnancy rate appears to be unaffected by lower levels of E2 in patients superovulated with letrozole. A recent report indicates that ovarian stimulation with letrozole and the resultant lower peak E2 levels may be beneficial in breast cancer patients who wish to preserve their fertility before chemotherapy [19].
According to the results of the present study, the mean endometrial thickness on the day of hCG administration was significantly higher in subjects taking letrozole than patients received CC-gonadotropins. This finding is in line with the results obtained by Mitwally et al. [20] and Sohrabvand et al [21]. It is probable that the cause of endometrial thickening in patients receiving letrozole is because of improved vascularization as compared with clomiphene citrate [22].Another study also showed that clomiphene citrate can cause inadequate endometrial thickness in 15–50% of patients and have negative effects on the quality or quality of the cervical and endometrial mucosa [22].These complications may be attributed to the anti-estrogenic effect and the relatively longer half-life of clomiphene citrate [11].
To correct the negative impact of CC, the next step could be the induction of ovulation with gonadotropins which increase both the cost and risk associated with treatment.
A recent retrospective analysis found that the multiple pregnancy rates were significantly lower in letrozole + FSH than in CC + FSH cycles [20].In our study, twin pregnancy was comparable in both groups. One patient in CC group and three patients in letrozole group had abortion (the difference not being significant).
In summary, the results of this study seem to suggest that aromatase inhibitors may be a good alternative for CC-gonadotropins without increasing both the cost and risk associated with gonadotropines. It could even be used as a first line treatment for ovulation induction or augmentation in infertility management.
References
Beck JI, Boothroyd C, Proctor M, Farquhar C, Hughes E. Oral anti-oestrogens and medical adjuncts for subfertility associated with anovulation. Cochrane Database Syst Rev 2005;25(1):CD002249.
Dickey RP, Taylor SN, Curole DN, Rye PH, Pyrzak R. Incidence of spontaneous abortion in clomiphene pregnancies. Hum Reprod 1996;11(12):2623–8.
Gorlitsky GA, Kase NG, Speroff L. Ovulation and pregnancy rates with clomiphene citrate. Obstet Gynecol 1978;51(3):265–9.
Garcia J, Jones GS, Wentz AC. The use of clomiphene citrate. Fertil Steril 1977;28(7):707–17.
Hammond MG. Monitoring techniques for improved pregnancy rates during clomiphene ovulation induction. Fertil Steril 1984;42(4):499–509.
Gysler M, March CM, Mishell DR, Bailey EJ. A decades experience with an individualized clomiphene treatment regimen including its effects on the postcoital teat. Fertil Steril 1982;37:161–7.
Randall JM, Templeton A. Cervical mucus score and in vitro sperm mucus interaction in spontaneous and clomiphene citrate cycles. Fertil Steril 1991;56(3):465–8.
Gonen Y, Casper RF. Sonographic determination of a possible adverse effect of clomiphene citrate on endometrial growth. Hum Reprod 1990;5(6):670–4.
Eden JA, Place J, Carter GD, Jones J, Alaghband-Zadeh J, Pawson ME. The effect of clomiphene citrate on follicular phase increase in endometrial thickness and uterine volume. Obstet Gynecol. 1989;73(2):187–90.
Opsahl MS, Robins ED, O’Connor DM, Scott RT, Fritz MA. Characteristics of gonadotropin response, follicular development, and endometrial growth and maturation across consecutive cycles of clomiphene citrate treatment. Fertil Steril 1996;66(4):533–9.
Mitwally MF, Casper RF. Use of an aromatase inhibitor for induction of ovulation in patients with an inadequate response to clomiphene citrate. Fertil Steril. 2001;75(2):305–9.
Casper RF. Letrozole: ovulation or superovulation? Fertil Steril 2003 Dec;80(6):1335–7.
Mitwally MF, Casper RF. Aromatase inhibitors in ovulation induction. Semin Reprod Med 2004;22(1):61–78.
Kilic-Okman T, Kucuk M, Altaner S. Comparison of the effects of letrozole and clomiphene citrate on ovarian follicles, endometrium, and hormone levels in the rat. Fertil Steril 2003;80(6):1330–2.
Ivoson T, Smith I, Ahern J, Smithers D, Trunel P, Dowseh M. Phase I study of the oral nonsteroidal aromatase inhibiter COS 20267 in post menopausal patients with advanced breast cancer. Cancer Res 1993;53:266–70.
Mitwally MF, Casper RF. Aromatase inhibition reduces gonadotrophin dose required for controlled ovarian stimulation in women with unexplained infertility. Hum Reprod 2003;18(8):1588–97.
Jee BC, Ku SY, Suh CS, Kim KC, Lee WD, Kim SH. Use of letrozole versus clomiphene citrate combined with gonadotropins in intrauterine insemination cycles: a pilot study. Fertil Steril 2006;85(6):1774–7.
Netter J. Applied linear statistical models. Richard D. Irwin Inc., Homewood, IL, USA; 1974. p. 833.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol 2005;23(19):4347–53.
Mitwally MF, Biljan MM, Casper RF. Pregnancy outcome after the use of an aromatase inhibitor for ovarian stimulation. Am J Obstet Gynecol 2005;192(2):381–6.
Sohrabvand F, Ansari Sh, Bagheri M. Efficacy of combined metformin–letrozole in comparison with metformin–clomiphene citrate in clomiphene-resistant infertile women with polycystic ovarian disease. Hum Reprod. 2006;21(6):1432–5.
Fisher SA, Reid RL, Van Vugt DA, Casper RF. A randomized double-blind comparison of the effects of clomiphene citrate and the aromatase inhibitor letrozole on ovulatory function in normal women. Fertil Steril 2002;78(2):280–5.
Acknowledgment
This research has been supported by Tehran University of Medical Sciences and we would like to thank the staff of Vali-e Asr infertility Research Center and The Royan Institute for their cooperation throughout the stages of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sh. Tehrani nejad, E., Abediasl, Z., Rashidi, B.H. et al. Comparison of the efficacy of the aromatase inhibitor letrozole and clomiphen citrate gonadotropins in controlled ovarian hyperstimulation: a prospective, simply randomized, clinical trial. J Assist Reprod Genet 25, 187–190 (2008). https://doi.org/10.1007/s10815-008-9209-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-008-9209-2