Abstract
The chronicity of sleep disturbance and its relation to co-occurring symptoms in children with autism spectrum disorder (ASD) are not well understood. The current study examined longitudinal relations among sleep and co-occurring symptoms in a large well-characterized sample of 437 children with ASD assessed at baseline and follow-up (M = 3.8 years later). Twenty-three percent experienced worsening sleep problems over time, while 31.5% showed improvement. Path analysis indicated that sleep problems at baseline predicted later development of ADHD symptoms in younger children and somatic complaints in older children. For younger children, sensory over-responsivity predicted future sleep problems. Findings suggest that sensory over-reactivity may contribute to sleep problems in some children with ASD, and that sleep problems may result in poor daytime functioning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized primarily by impairments in social communication and by repetitive or restricted patterns of behavior or interests (American Psychiatric Association 2013). However, these diagnostic features are frequently accompanied by a myriad of additional co-occurring symptoms and conditions, ranging from medical to psychiatric problems (Bauman 2010; Kielinen et al. 2004; Leyfer et al. 2006; Simonoff et al. 2008). Sleep disturbance is among the most common and detrimental of these co-occurring problems, affecting between 50 and 80% of children with ASD (Couturier et al. 2005; Krakowiak et al. 2012; Richdale and Schreck 2009; Souders et al. 2009). Problems falling asleep, decreased total sleep time, and frequent night awakenings appear to be the most common types of sleep disturbance among children with ASD (Elrod and Hood 2015; Malow and McGrew 2008; Richdale and Schreck 2009) and these problems can have a negative impact on quality of life and well-being for both children and their families (Delahaye et al. 2014; Hodge et al. 2013; Hoffman et al. 2008).
Given the prevalence of sleep problems in this population (Couturier et al. 2005; Krakowiak et al. 2012; Richdale and Schreck 2009; Souders et al. 2009), understanding the persistence and chronicity of sleep disturbance in children with ASD is important for both clinicians and researchers. Humphreys et al. (2014) examined differences in parent-reported sleep duration between children with ASD and typically developing (TD) children using a prospective longitudinal design. Data from the Avon Longitudinal Study of Parents and Children were used to compare children with ASD to TD children across 8 time points, from 6 months through 11 years of age. The results indicated that by 30 months of age, children with ASD demonstrated less sleep duration and greater night-time awakenings than TD children, and this difference persisted across time (Humphreys et al. 2014).
Other prior studies have varied quite a bit in terms of the time frame included and in participant age range. This is an important consideration, given normative changes in sleep from early childhood through adolescence (Iglowstein et al. 2003; Ohayon et al. 2004). Some studies have focused primarily on young children. For example, in a short-term longitudinal study, Anders et al. (2012) examined various indicators of sleep and daytime functioning over 6 months in a sample of 68 children with autism compared to children with intellectual disability (ID) and TD (between the ages of 24 and 66 months at baseline). Sleep patterns remained relatively stable across the 6-month period, with children with autism receiving less total sleep than children with ID or TD across time points.
Others have included samples that spanned early childhood through late adolescence, without specific consideration of potential developmental shifts. For example, earlier work by Richdale and Prior (1995) examined this issue in a sample of 39 children and adolescents with autism who were between 32 months and 19 years of age. Parents completed sleep diaries and were also asked about “past sleep behavior;” however, the time frame for these questions was not described. The results suggested that 72% had a history of parent-reported sleep problems, but the total percentage reporting current problems was not reported across groups. In a different study of 56 children with ASD (ages 3–16 years), sleep problems were present for 78.6% of the sample at baseline and persisted at 2-year follow-up for 91% of that group. Additionally, sleep problems developed in 22% of those with no problems at baseline (Mannion and Leader 2016). However, differences across age or developmental level were not specifically examined within these broad samples.
Several groups have focused primarily on school-age children and early adolescents. For example, Allik et al. (2008) examined sleep patterns using actigraphy at baseline and 2–3 years later in a small sample of 16 school-age (8–13 years) children with Asperger syndrome and 16 TD children. Sleep duration and sleep efficiency decreased in both groups. In a study of 46 high-functioning children with ASD (between the ages of 7 and 12 years at baseline), overall improvement in sleep was found at 1-year follow-up for the ASD group. Specifically, 78% scored above clinical cutoff for sleep disturbance on the CSHQ at baseline, dropping to 65% at follow-up (May et al. 2015). In a more recent study of 23 children with ASD and 32 TD children (ages 6–12 years), Fletcher and colleagues examined changes in sleep from baseline to 1-year follow-up. The results indicated that persistent parent-reported sleep problems were more common in the ASD group (76%) than the TD group (30%); however, the percentage experiencing sleep problems at each time point was not reported. The two groups had similar trajectories in overall sleep profile, with a decrease in overall sleep duration for both (Fletcher et al. 2017).
These prior studies provide some insights into the course of sleep problems in autism. Most notably, children with ASD have more trouble sleeping than TD children and these problems appear to persist over time. However, these prior study samples were small and not fully representative of the larger ASD population. Additionally, age-related issues were not specifically addressed. Most did not include children with low IQ scores (Allik et al. 2008; Fletcher et al. 2017; May et al. 2015), included convenience samples, and consisted of restricted age ranges. Therefore, future research is needed to explore the chronicity of sleep disturbance in a larger and more representative sample.
Researchers and clinicians have also been interested in understanding potential predictors and consequences of sleep disturbance in children with ASD (e.g., Hoshino et al. 1984; Richdale and Prior 1995; Wiggs and Stores 2004). Identifying factors that contribute to the development or worsening of sleep difficulties may provide targets for early intervention or prevention. By the same token, understanding the consequences of sleep disturbance may have implications for treatment of common co-occurring challenges. To that end, several cross-sectional studies have been conducted to identify correlates of sleep disturbance in this population, as described in recent reviews (Cohen et al. 2014; Hollway and Aman 2011; Mannion and Leader 2014). Studies have consistently found significant correlations between sleep disturbance and behavioral problems (Goldman et al. 2009, 2011; Hollway et al. 2013; Mayes and Calhoun 2009; Mazurek and Sohl 2016; Patzold et al. 1998), stereotyped and repetitive behavior (Gabriels et al. 2005; Hundley et al. 2016; Schreck et al. 2004), sensory over-responsivity (Mazurek and Petroski 2015; Reynolds et al. 2012), and anxiety (DeVincent et al. 2007; Hollway et al. 2013; Mazurek and Petroski 2015; Wiggs and Stores 2004) among children with ASD. Additionally, some medical problems have been correlated with sleep disturbance in children with ASD, including epilepsy (Accardo and Malow 2015; Malow 2006) and gastrointestinal problems (Klukowski et al. 2015; Mannion et al. 2013). In one of the largest studies to examine potential correlates of sleep disturbance in children with ASD, Hollway et al. (2013) tested components of their theoretical bidirectional framework (Hollway and Aman 2011). In a large sample of 1583 children (ages 2–17) enrolled in the Autism Treatment Network, 45 potential predictors were examined using hierarchical regression modeling (including demographic factors, IQ, emotional/behavioral functioning, and medical comorbidities). The results revealed that anxiety was the strongest cross-sectional predictor of sleep disturbance, and that higher IQ, autism symptom severity, sensory sensitivities, and GI problems were also associated with sleep disturbance (Hollway et al. 2013). Although all of these studies provide important insights into correlates of sleep problems in children with ASD, they were all cross-sectional, meaning that it is not clear whether sleep problems contribute to later development of co-occurring symptoms, whether the reverse is true, or whether there are bidirectional relationships between certain sets of symptoms.
Two previously cited longitudinal studies offer preliminary findings on the role of co-occurring symptoms. In their 2015 study, May and colleagues conducted a series of hierarchical linear regression analyses to examine whether baseline sleep problems predicted future behavioral problems (and vice versa). They found that for the entire sample (ASD and TD), baseline sleep disturbance predicted anxiety, but not behavioral problems, at 1-year follow-up. However, these analyses were conducted on the combined sample, and comprehensive models accounting for change in both behavioral and sleep variables were not conducted. As a result, directional relationships among sleep and behavioral factors in children with ASD could not be determined from the reported results. In their 1-year follow-up study of 23 children with ASD and 32 TD children, Fletcher et al. (2017) found that change in anxiety over time was associated with changes in severity of sleep disturbance.
While these studies offer emerging evidence about the course of sleep disturbance and its association with co-occurring symptoms, research to date has been limited by small sample sizes and an inability to account for complex relationships among both sleep and multiple co-occurring problems over time. Based on prior research, several co-occurring symptoms have particular relevance to sleep, including behavior problems (e.g., aggression, hyperactivity and inattention), repetitive behavior, internalizing symptoms (anxiety and somatic complaints), and sensory over-reactivity. However, the timing of their occurrence in relation to sleep disturbance in children with ASD is unknown.
Current Study
The chronicity of sleep disturbance and its relation to co-occurring symptoms in children with ASD are thus not well understood. Longitudinal analysis would provide important insights into the nature, course, and development of these potentially interrelated symptoms, offering new directions for targeted treatments. A large sample, robust approach to analysis, and comprehensive assessment of key co-occurring challenges is necessary to elucidate the timing and directionality of these relationships. The purpose of the current study was to examine the chronicity of sleep disturbance and to examine the complex longitudinal relations among sleep problems and co-occurring symptoms in a large and well-characterized sample of children and adolescents with ASD.
Methods
Participants and Procedures
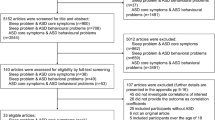
The sample included 437 children who were initially enrolled in the Autism Treatment Network (ATN) Registry study when they were between 2 and 10 years of age and were subsequently recruited to participate in a longitudinal ATN Call-Back study an average of 3.8 years after initial enrollment.
The ATN is a multi-site network of autism centers across the US and Canada specializing in best-practice approaches for diagnosis and treatment of children with ASD. The ATN Registry database contains a common set of measures collected across all sites. At enrollment, all participants were assessed by ATN clinicians using a standard battery, which included clinical assessment and interview based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (American Psychiatric Association 2000), behavioral observation using the Autism Diagnostic Observation Schedule (ADOS) (Lord et al. 2000), cognitive and adaptive assessment, and a range of measures assessing medical and behavioral characteristics. Eligibility criteria included meeting DSM-IV criteria for ASD (American Psychiatric Association 2000) and parental fluency in English.
The ATN Call-Back Study was initiated in 2015 to examine longitudinal changes in key symptom domains among children who were initially enrolled in the ATN Registry at one of 12 ATN sites between the target years of 2011 and 2013. Each site was provided with a randomly selected list of potentially eligible participants, with an initial target enrollment of 50 participants per site. The AS-ATN Registry and Call-Back studies were both approved by the Institutional Review Board at each site, informed written consent was obtained from all parents, and children provided assent when applicable and appropriate. The final sample for the current study included 437 children with ASD who completed measures at enrollment and follow-up.
Measures
Child and Family Characteristics
Demographic data were collected at enrollment, including age, sex, race and ethnicity, household income, and caregiver education level. The primary caregiver’s education level at baseline was an ordinal variable: less than 8th grade, some high school, finished high school, some college, bachelor’s degree, or post-graduate degree. Since education level and household income were moderately correlated (r = .446, p < .001), and household income had more missing data (18.8% missing) than caregiver education (2.3% missing), we used only education level as a proxy for the family’s socioeconomic status. Intelligence (IQ) was assessed at enrollment using one of a range of different tests. The specific tests, percentage of the sample receiving each test, and scores used as a proxy for overall IQ are as follows: Bayley Scales of Infant and Toddler Development—Third Edition (Bayley 2006) (1.8%, Cognitive Composite score), Differential Ability Scales—Second Edition (Elliot 2007) (5.0%, General Conceptual Ability score), Wechsler Abbreviated Scale of Intelligence—Second Edition (Wechsler 2011) (1.2%, Full Scale IQ score), Wechsler Intelligence Scale for Children—Fourth Edition (Wechsler 2003) (3.0%, Full Scale IQ score), Wechsler Preschool and Primary Scale of Intelligence—Third Edition (Wechsler 2002) (6.1%, Full Scale IQ score), Stanford Binet Scales of Intelligence—Fifth Edition (Roid 2003) (37.8%, Full Scale IQ score), and the Mullen Scales of Early Learning (Mullen 1995) (25.2%, Early Learning Composite score). Intellectual testing could not be completed for some participants (19.9%) due to difficulties participating or understanding task demands.
Sleep Medications
Medications and their primary indications were recorded by ATN clinicians at each assessment. Medications for which “sleep” was checked as a primary indication were of interest in the current study.
Children’s Sleep Habits Questionnaire (CSHQ)
The Children’s Sleep Habits Questionnaire (CSHQ) (Owens et al. 2000) was used to assess overall sleep problems. The CSHQ is a 45-item scale that includes parent-reported items assessing key sleep domains. Most items are rated on a 3-point scale (ranging from 1 = rarely to 3 = usually). The Total Sleep Disturbance score (sum of 33 items) was examined in the current study as an index of overall sleep problems. Cronbach’s alpha for the CSHQ was .626 at baseline and .697 at follow-up. The original development sample for the CSHQ included children between 4 and 10 years of age (Owens et al. 2000). However, the CSHQ has demonstrated good psychometric properties when used with toddlers as young as 2 years of age, including convergent validity, as evidenced by significant correlations between CSHQ scores and actigraphy and parent diary (Goodlin-Jones et al. 2008). A total CSHQ score of 41 is considered to be the clinical cut-off for identification of probable sleep problems (Owens et al. 2000).
Child Behavior Checklist
The Child Behavior Checklist (CBCL) (Achenbach and Rescorla 2001) was used as a measure of several specific co-occurring symptoms. The CBCL is a widely-used parent-report questionnaire assessing both internalizing and externalizing symptoms. Items are rated on a 3-point scale, and are used to generate scores on both empirically derived Syndrome Scales and DSM-Oriented Scales. For the purposes of the current study, T-scores from select subscales that are common across both the Preschool (for ages 1.5–5 years) and School-Age (for ages 6–18 years) versions were used to assess key co-occurring symptoms. Aggression was assessed using the Aggressive Behavior Syndrome Scale, which includes items assessing both physical aggression and oppositional and defiant behaviors. Inattention and Hyperactivity were assessed by the Attention Deficit/Hyperactivity DSM-Oriented Scale, which includes items assessing problems with attention, hyperactivity, and impulsivity. Anxiety was assessed by the Anxiety Problems DSM-Oriented Scale. The DSM-Oriented scale was chosen for the current study because it includes only items specific to anxiety, while the Anxious/Depressed Syndrome Scale includes affective symptoms. Finally, somatic complaints were assessed by the Somatic Complaints Syndrome Scale, which is a measure of general somatic symptoms, including gastrointestinal symptoms, headaches, and general aches, for example.
Aberrant Behavior Checklist
Repetitive behavior was assessed using the Stereotypic Behavior subscale of the Aberrant Behavior Checklist (ABC) (Aman and Singh 1986). The ABC is a 58-item rating scale assessing problem behavior in individuals with developmental disabilities. Parent-reported items are rated on a 4-point scale, comprising five separate subscales. The Stereotypic Behavior subscale includes 7 parent-reported items focusing on repetitive behaviors and stereotyped movements. Although originally developed for use among adults with developmental disabilities, the psychometric properties of the ABC have been established for use with toddlers (Karabekiroglu and Aman 2009; Sigafoos et al. 1997), school-aged children, and adolescents in subsequent research (Brown et al. 2002; Kaat et al. 2014).
Short Sensory Profile
Sensory over-responsivity (SOR) was assessed using a subset of items from the Short Sensory Profile (SSP) (McIntosh et al. 1999). The SSP assesses atypical sensory response and includes 38 parent-reported items rated on a 5-point scale ranging from 1 (Always) to 5 (Never). Cronbach’s alpha for the SSP was .765 at baseline, and .753 at follow-up. Consistent with prior research (Mazurek et al. 2013; Mazurek and Petroski 2015), an SOR score was calculated as a sum of item scores on the following scales: Tactile Sensitivity, Taste/Smell Sensitivity, Movement Sensitivity, and Visual/Auditory Sensitivity. Note that lower total SOR scores indicate greater difficulties with sensory over-responsivity.
Statistical Analyses
To examine the chronicity of sleep problems, we ran three groups of analyses using SPSS. We executed (1) a simple correlation between total sleep problems at baseline and follow-up, (2) a linear regression model with total sleep at baseline and IQ, age, gender, and caregiver education predicting total sleep at follow-up, controlling for time between assessments, and (3) descriptive statistics on the indices of changes in sleep.
Regarding indices of change in sleep, participants first were categorized into one of three groups, based on the magnitude of individual change in total sleep problems relative to the standard deviation of the baseline mean. Participants whose total sleep problems did not change more than one-half of a standard deviation in either direction from baseline to follow-up were categorized as “relatively stable.” Those whose total sleep problems changed more than one-half a standard deviation from their baseline score were classified as “improved” or “worsened,” depending on the direction of change (see Norman et al. 2003). The percentages of children falling at or above the clinical cut-off on the CSHQ at baseline and follow-up were also examined (Owens et al. 2000).
To examine the relations among sleep problems and participant characteristics, we first conducted simple correlations. We then conducted an analysis of variance, with the factor variable being whether sleep improved, worsened, or remained stable.
To test the relations among sleep problems and co-occurring symptoms, we ran two sets of analyses. First, we examined the simple correlations between sleep problems and aggression, attention problems, anxiety, somatic complaints, repetitive behavior, hyperactivity, and SOR. Second, we ran separate path analyses for each co-occurring symptom (using SPSS AMOS 24; Arbuckle 2016) to compare fit statistics across four models: unconditional (independent observed variables with error terms correlated within time points), unidirectional (sleep problems predicting co-occurring symptoms), unidirectional (co-occurring symptoms predicting sleep problems), and a cross-lagged bidirectional model. In each model, sleep problems at baseline was assumed to predict sleep problems at follow-up, and co-occurring symptoms at baseline were assumed to predict co-occurring symptoms at follow-up. All of these models included gender, age at baseline, IQ, caregiver education, and time between assessments as exogenous, correlated, covariates.
Since there were only two time points, only a linear trend could be estimated with confidence. The individual path models were evaluated for relative fit using χ2 comparisons, wherein each model is compared to the current best-fitting model, and the best-fitting model for each co-occurring symptom is determined by the p-value of the respective change in χ2 for the accompanying degree of freedom gained or lost.
Results
Missing Data
Data from the CSHQ were missing for 44 participants (10%) at baseline, and 18 participants (4.1%) at follow-up. Incomplete cases did not differ from complete cases on IQ [t(348) = − .996, p = .320], gender [χ2 (1) = .080, p = .777], ethnicity [χ2 (1) = .139, p = .710], or caregiver education [χ2 (5) = 7.603, p = .180]. Younger children were more likely to have incomplete sleep data at baseline [t(435) = − 4.062, p < .001] and follow-up [t(435) = − 3.952, p < .001].
Participant Characteristics
Regarding sample characteristics, participants ranged in age from 2 to 10 years at enrollment (M = 5.07, SD = 2.14). The majority of the sample was male (82.6%) and Caucasian (86.0%). Household income ranged from 0–$24,999 to $100,000 or above, with a median range of $50,000–$74,999. The majority of respondents were biological parents (88%), and the majority of primary caregivers had attended some college (29.3%) or attained a bachelor’s degree (31.1%). The time between assessments ranged from 1.9 to 5.5 years across the sample (M = 3.83, SD = 0.63). Full Scale IQ ranged from 40 to 132 (M = 76.24, SD = 22.23). Medications used for sleep included clonidine (2.5% of participants at baseline, 12.4% at follow-up), risperidone (2.7% at baseline, 9.2% at follow-up), guanfacine (2.5% at baseline, 15.8% at follow-up), melatonin (12.1% at baseline, 35.2% at follow-up), and other unspecified medications used for sleep (9.8% at baseline, 12.0% at follow-up). Descriptive statistics for participant characteristics are shown in Table 1.
Age Groups
Younger and older age groups (2–3-year-olds and 4–10-year-olds) did not differ in gender [χ2 (1) = .557, p = .456], caregiver education [χ2 (5) = 3.759, p = .585], ethnicity [χ2 (1) = .170, p = .680], or time between assessments [t(435) = − .749, p = .454, d = .07]. Younger children did have significantly lower IQs [t(317.67) = − 6.814, p < .001, g = .71] and took less sleep medication at baseline [t(422.156) = − 4.694, p < .001, g = .42] and follow-up [t(398.546) = − 2.612, p = .009, g = .25]. In terms of our variables of interest, age groups did not differ in baseline sleep problems [t(391) = .134, p = .894, d = − .01], follow-up sleep problems [t(417) = 1.426, p = .155, d = − .14], or total change in sleep problems [t(214.033) = .260, p = .795, g = − .03]. The relative proportions of sleep change categories (i.e., improved, worsened, or relatively stable over time) did not differ across age groups [χ2 (2) = 2.762, p = .251].
Chronicity of Sleep Problems
Seventy percent of the total sample scored at or above clinical cut-off for sleep problems at baseline, and 65.4% at follow-up. When examining age groups separately, 68.4% of younger children scored within the clinical range at baseline and 67.9% at follow-up. Among the older group, 70.8% scored within the clinical range at baseline and 63.8% at follow-up. Descriptive statistics for the individual subscales of the CSHQ are shown in Table 2.
A simple correlation between total sleep problems at baseline and follow-up showed a moderate positive relationship (younger group: r = .523, p < .001; older group: r = .620, p < .001). A linear regression model found total sleep problems at baseline was a significant predictor of total sleep problems at follow-up, even after accounting for the effects of additional relevant variables (younger group: R2 change = .266, p < .001; older group: R2 change = .359, p < .001). When examining the change in CSHQ Total Sleep Disturbance among children with complete data at both baseline and follow-up (using change categories previously described, which were based on the magnitude of individual change in total sleep problems relative to the standard deviation of the baseline mean), 22.9% of children showed worsening of sleep problems over time, 45.6% of children had relatively stable sleep scores from baseline to follow-up, and 31.5% of children showed improvement in sleep problems. A Chi square goodness of fit test found that the distribution of sleep change categories was similar in younger children [χ2 (2) = 3.476, p = .176], but was significantly different in older children [χ2 (2) = 29.012, p < .001], with more individuals in the “stable” group.
The relationship between previous sleep problems and future sleep problems was strong and positive, regardless of whether individuals’ sleep problems improved over time (r = .846, p < .001), worsened over time (r = .847, p < .001), or remained relatively stable over time (r = .950, p < .001). In other words, those with few sleep problems tended to have few sleep problems in the future, even if they worsened slightly, and those with more sleep problems tended to have more sleep problems in the future, even if they improved slightly. This shows moderate stability in the change in sleep problems over time.
Relations Among Sleep and Participant Characteristics
Age, IQ, gender, and time between assessments were unrelated to total sleep problems at baseline or follow-up for both younger and older children (r’s and t > .05). However, caregiver education was significantly related to sleep problems for younger children at follow-up (rs = − .251, p = .001) and older children at baseline (rs = − .131, p = .038) and follow-up (rs = − .169, p = .007), wherein lower levels of education were associated with greater sleep problems.
Whether a child met clinical cut-off for sleep problems was unrelated to age, gender, ethnicity, race, caregiver education, IQ, or sleep medications at baseline for the younger group (p’s > .05). At baseline, older children who met the clinical cut-off for sleep problems took significantly more sleep medications [t(181.356) = − 2.213, p = .028, g = .27].
Whether a younger child met clinical cut-off for sleep problems at follow-up was unrelated to gender, ethnicity, race, IQ, or time between assessments (p’s > .05). However, children in the younger age group with clinically significant levels of sleep problems were significantly older [t(157) = − 2.029, p = .044, d = .35] and took significantly more sleep medications [t(126.854) = − 2.933, p = .004, g = .44] at follow-up than children who did not meet the clinical cut-off. In addition, the distribution of caregiver education was significantly different for young children with and without clinical sleep problems at follow-up [χ2 (5) = 14.968, p = .011]. Specifically, parents of young children with clinically significant sleep problems at follow-up had a wider distribution and less education (less than 8th grade: 0.9%; some high school: 0.9%; finished high school: 22.6%; some college or an associate’s degree: 29.2%; bachelor’s degree: 29.2%, post-graduate degree: 17%) than parents of young children without clinically significant sleep problems at follow-up (less than 8th grade: 0%; some high school: 2%; finished high school: 2%; some college or associate’s degree: 23.5%; bachelor’s degree: 49%; post-graduate degree: 23.5%). At follow-up, older children with and without clinically significant sleep problems were similar in age, IQ, time between assessments, gender, caregiver education, ethnicity, and race (p’s > .05). However, older children with clinically significant sleep problems at follow-up took significantly more sleep medication at follow-up [t(255.591) = − 3.550, p < .001, g = .40] than older children who did not reach the clinical cutoff for sleep problems.
The change in sleep problems over time was unrelated to a child’s age [F(2, 372) = .464, p = .629, η2 = .002], IQ [F(2, 302) = .460, p = .632, η2 = .003], gender [χ2 (2) = .095, p = .954], caregiver education [χ2 (10) = 6.788, p = .745], ethnicity [χ2 (2) = .730, p = .694], race [χ2 (2) = 3.782, p = .151], or the time between assessments [F(2, 373) = .250, p = .779, η2 = .001]. Children whose sleep problems improved over time took significantly more sleep medications at baseline, and children whose sleep problems worsened over time took significantly fewer sleep medications at baseline [F(2, 372) = 4.310, p = .014, η2 = .023]. Additionally, children whose sleep problems improved over time had significantly greater sleep problems at baseline (M = 51.26, SD = 8.49) than children whose sleep problems worsened (M = 42.31, SD = 7.12) or remained stable (M = 44.0, SD = 7.92) [F(2, 372) = 40.702, p < .001, η2 = .180].
Relations Among Sleep and Co-occurring Symptoms
Sleep problems were significantly related to most co-occurring symptoms at baseline and follow-up for both younger and older children. Table 3 shows descriptive statistics and a correlation matrix of these variables.
As described above, four separate path analysis models were examined for each type of co-occurring symptom, controlling for covariates. Fit statistics across all models are shown in Tables 4 and 5. For younger children, sensory over-responsivity predicted future sleep problems, and sleep problems predicted future inattention/hyperactivity. For older children, sleep problems predicted future somatic complaints.
Discussion
The current study offers the first large-scale exploration of the longitudinal relationships between sleep and a range of co-occurring symptoms in children with ASD. These findings provide important clinical implications and offer new insights into the development and consequences of symptoms over time. Regarding the course and persistence of sleep disturbance in the current sample, 23.9% of the sample experienced worsening of sleep problems over time, while 31.5% showed improvement in symptoms. Those with more severe initial sleep problems were more likely to improve over time. Although previous studies of smaller and less-representative samples found that sleep problems persist (at a group level) for a majority of children with ASD (e.g., May et al. 2015; Mannion and Leader 2016), this was the first study to report on clinically significant indices of change in sleep among children with ASD. Given normative changes in sleep across early childhood (Iglowstein et al. 2003), we examined sleep patterns among younger (2–3-year-old) and older (4–10-year-old) children separately. As the first study to examine potential developmental differences in sleep patterns among children with ASD, these results add to our understanding of sleep in children with ASD across childhood. There were no differences between younger and older children in sleep problems at either baseline or follow-up, or in sleep change category. Additionally, change in sleep problems over time was not related to child age. These findings suggest that children with ASD may not experience the same age-related changes in sleep that other children typically experience (Iglowstein et al. 2003; Ohayon et al. 2004), which adds new information to previous reports of poor overall sleep in children with ASD compared to TD children (e.g., Anders et al. 2012; Humphreys et al. 2014). However, further longitudinal research is needed to better characterize sleep duration and disturbance at regular intervals from early childhood through late adolescence in individuals with ASD. In the current study, older children with ASD who met clinical cut-off for sleep problems took more sleep medications at both baseline and follow-up, while this was only true at follow-up among younger children. This suggests that sleep medications may be more commonly utilized among older children and those with more severe sleep disturbance.
In terms of longitudinal predictors of sleep disturbance, the current study found that demographic factors were largely unrelated to the persistence of sleep problems over time; with the exception of caregiver education (considered a proxy for socioeconomic status, SES), wherein higher levels were associated with fewer sleep problems. This is consistent with research from the general population, which has found that children from families with lower SES demonstrate greater sleep problems than those with higher SES (El-Sheikh et al. 2010; Simonds and Parraga 1982; Stein et al. 2001). Low SES may affect child sleep for a number of reasons, including decreased parental resources for facilitating sleep or bedtime routines, lack of space for bedding or separate sleeping arrangements, poor temperature control, or noisy or crowded sleep environments (Doane et al. 2018).
Overall, the results revealed that many co-occurring symptoms were related to sleep changes. Consistent with prior research indicating a relationship between sensory problems and sleep in children with ASD (Mazurek and Petroski 2015; Reynolds et al. 2012), the current study also found significant cross-sectional correlations between sleep problems and sensory over-responsivity (SOR) in both younger and older children. Interestingly, the results revealed a significant longitudinal relationship between SOR and sleep after accounting for covariates among younger children. Specifically, the results indicated that SOR was a longitudinal predictor of sleep problems in very young children; however, these variables were not significantly associated in the longitudinal models for older children. These results suggest that the relations among co-occurring symptoms and sleep disturbance may change over time, and that consideration of sensory reactivity may be particularly important for understanding sleep among young children. This is consistent with other findings indicating a stronger relationship between sensory reactivity and sleep onset, sleep duration, and night awakenings in younger versus older children with ASD (Mazurek and Petroski 2015). Together, these results suggest that very young children with ASD with high levels of SOR may be especially sensitive to sensory-related aspects of the sleep environment. These environmental stimuli (such as background noise, light, room temperature, bedding, or sleepwear) may interfere with onset or maintenance of sleep.
The current findings also offer new information about the effects of sleep disturbance upon daytime behavior in children with ASD. Specifically, the results indicate that sleep disturbance is a longitudinal predictor of the development of hyperactivity and attention problems in very young children. This extends previous findings of cross-sectional associations between these variables (Goldman et al. 2009; Mazurek and Sohl 2016) by providing information about timing and directionality. The best-fitting models showed that sleep disturbance had negative longitudinal effects on attention and hyperactivity in children with ASD, above and beyond the effects of other relevant variables. Again, this is highly consistent with evidence from the general population. For example, sleep restriction and sleep disruption have resulted in daytime problems with both attention and impulsivity in prior studies (Anders et al. 1978; Dahl et al. 1991; Fallone et al. 2001; Weinberg and Brumback 1990), and longitudinal research has shown that shorter sleep duration before age three predicts hyperactivity, impulsivity, and poor cognitive performance at age six (Touchette et al. 2009). These findings are particularly relevant for children with ASD, who are known to be at increased risk for significant inattention and hyperactivity (Frazier et al. 2001; Gadow et al. 2005; Mayes et al. 2012). Given that sleep disturbance may cause or exacerbate neurocognitive functioning, it is possible that treating sleep problems in this population may have a positive impact on attention and behavioral regulation, leading to improved functioning and engagement with learning and other daily tasks. Further research is needed to test this hypothesis within the context of well-designed treatment studies. Interestingly, although sleep problems were correlated with ADHD symptoms for both age groups, longitudinal models did not show significant relationships between these variables in older children after accounting for covariates. Future longitudinal research assessing these variables across multiple time points would be helpful to examine changes in trajectories and relations among symptoms over time.
Finally, the longitudinal relationship between sleep problems and development of somatic symptoms in older children with ASD is also consistent with prior research in the general population. Sleep is important for overall health, and sleep deprivation has detrimental effects on immune function and regulation of the endocrine systems (see for review, Bryant et al. 2004). Longitudinal and experimental studies have also found that sleep disturbance leads to the development and exacerbation of pain in both the general population and a range of other clinical populations (see for review, Finan et al. 2013). Sleep problems are also common among children with a range of different medical conditions, including those that frequently co-occur with ASD, such as gastrointestinal problems and seizure disorders (Lewandowski et al. 2011). This result is also somewhat consistent with cross-sectional associations between sleep problems and somatic aspects of anxiety reported in a small sample of children (ages 8–12) with ASD (Richdale and Baglin 2015), although the somatic symptoms assessed in that study were specifically related to the experience of fear or anxiety. Future studies involving comprehensive assessment of specific types of somatic symptoms would be helpful to more fully examine the relationship between sleep and pain in children with ASD.
The current findings are consistent with prior research documenting significant associations between sleep problems and anxiety in children with ASD (Fletcher et al. 2017; Hollway et al. 2013; Mazurek and Petroski 2015; Richdale and Baglin 2015). The current results also indicted significant cross-sectional correlations between anxiety and sleep problems for both age groups at baseline. However, regarding longitudinal relationships, the results did not indicate a significant predictive relationship between anxiety and sleep problems in either age group after accounting for covariates. This is somewhat surprising, given prior results from the general population. Studies of TD adolescents and adults have found that anxiety is a longitudinal predictor of insomnia, occurring prior to the onset of insomnia in the majority of cases (Jansson and Linton 2006; Johnson et al. 2006). By contrast, a large-scale population-based longitudinal study found that sleep problems in infancy and toddlerhood predicted the development of anxiety symptoms at age three, with little evidence of bidirectional associations (Jansen et al. 2011). Additional research using more comprehensive measures of anxiety and physiological arousal in children with ASD may be helpful to more fully explore the relations among these variables over time. It will also be informative to examine the potential relations among specific types of sleep disturbance and anxiety, as it is possible that certain types of sleep problems may be more likely to predict or be predicted by anxiety than others.
Limitations and Future Directions
Although the current study benefitted from a very large sample of well-characterized children with ASD, there are some limitations that should be noted. All measures of our primary variables of interest were parent-report. Although parents are able to rely on extensive experience and observation of the child’s functioning and behavior across a wide range of real-world settings and environments, it may be challenging for parents to accurately report on internally experienced symptoms, such as anxiety or somatic symptoms. However, given that many children with ASD have trouble reporting on their own emotional experiences, parent-report of these symptoms is generally recommended in children with ASD (Lopata et al. 2010; Mazefsky et al. 2011). Recent efforts have also focused on developing more appropriate and autism-specific measures of core and co-occurring symptoms, including anxiety and restricted and repetitive behaviors (see for example, Honey et al. 2012; Rodgers et al. 2016; Scahill et al. 2015; Scahill 2017). Future studies would benefit from further examination of the relations among sleep disturbance and co-occurring symptoms using these autism-specific tools, as they may provide a more valid measurement of core constructs in this population.
It is also important to consider potential limitations of the CSHQ for assessment of sleep, given that parents of children who are older or more independent may be less accurate reporters of their children’s sleep quality or night awakenings (Markovich et al. 2015). The current study assessed cognitive functioning and autism symptoms at baseline but not at follow-up. Examining how sleep problems relate to autism severity and cognitive functioning over time would provide additional insights into the course and consequences of these difficulties in children with ASD. Additionally, the primary variables in the current study represented symptoms (as assessed by parent-report rating scales) rather than clinically diagnosed disorders. It is important to note that the course and correlates of clinically diagnosed co-morbid disorders may be different from the current findings.
Future studies should seek to include multi-method assessments of variables of interest, including both parent-report and objective measures of sleep and behavior such as actigraphy, polysomnography, direct behavioral observation, and measures of physiological arousal. Longitudinal studies using repeated measurements across multiple time points would also provide a much more nuanced understanding of trajectories of various types of sleep and co-occurring symptoms across time from early childhood to adolescence.
Although this study was the first large-scale longitudinal study of sleep problems in children with ASD, future work is needed to examine the effects of specific treatments and interventions on sleep outcomes over time. For example, treatment-outcome research would be helpful to determine whether treatment of sleep problems prevents or reduces inattention and hyperactivity in early childhood. Additionally, future research should consider the relative effectiveness of various treatments for sleep disturbance (e.g., medication, behavioral treatment, or cognitive-behavioral therapy) across childhood or at different stages of development. All of these issues will require additional study in order to guide the development of clinical treatment guidelines.
References
Accardo, J. A., & Malow, B. A. (2015). Sleep, epilepsy, and autism. Epilepsy & Behavior, 47, 202–206.
Achenbach, T., & Rescorla, L. (2001). Manual for the achenbach system of empirically based assessment school-age forms profiles. Burlington: ASEBA.
Allik, H., Larsson, J. O., & Smedje, H. (2008). Sleep patterns in school-age children with Asperger syndrome or high-functioning autism: A follow-up study. Journal of Autism and Developmental Disorders, 38(9), 1625–1633.
Allison, P. D. (1990). Change scores as dependent variables in regression analysis. Sociological Methodology, 20, 93–114.
Aman, M. G., & Singh, N. N. (1986). Aberrant behavior checklist: Manual. East Aurora, NY: Slosson.
American Psychiatric Association. (2000). Diagnostic and Statistical Manual, Fourth Edition, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Association.
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Washington, DC: American Psychiatric Association.
Anders, T., Iosif, A. M., Schwichtenberg, A. J., Tang, K., & Goodlin-Jones, B. (2012). Sleep and daytime functioning: A short-term longitudinal study of three preschool-age comparison groups. American Journal on Intellectual and Developmental Disabilities, 117(4), 275–290.
Anders, T. F., Carskadon, M. A., Dement, W. C., & Harvey, K. (1978). Sleep habits of children and the identification of pathologically sleepy children. Child Psychiatry & Human Development, 9(1), 56–63.
Arbuckle, J. L. (2016). Amos 24.0 [Computer Program]. Chicago: IBM SPSS.
Bauman, M. L. (2010). Medical comorbidities in autism: Challenges to diagnosis and treatment. Neurotherapeutics, 7(3), 320–327.
Bayley, N. (2006). Bayley scales of infant and toddler development: Bayley-III. San Antonio: Harcourt Assessment, Psychological Corporation.
Bonnet, M. H., & Arand, D. L. (1998). Heart rate variability in insomniacs and matched normal sleepers. Psychosomatic Medicine, 60(5), 610–615.
Bonnet, M. H., & Arand, D. L. (2010). Hyperarousal and insomnia: State of the science. Sleep Medicine Reviews, 14(1), 9–15.
Broman, J., & Hetta, J. (1994). Electrodermal activity in patients with persistent insomnia. Journal of Sleep Research, 3(3), 165–170.
Brown, E. C., Aman, M. G., & Havercamp, S. M. (2002). Factor analysis and norms for parent ratings on the Aberrant Behavior Checklist-Community for young people in special education. Research in developmental disabilities, 23(1), 45–60.
Bryant, P. A., Trinder, J., & Curtis, N. (2004). Sick and tired: Does sleep have a vital role in the immune system? Nature Reviews Immunology, 4(6), 457–467.
Cohen, S., Conduit, R., Lockley, S. W., Rajaratnam, S. M., & Cornish, K. M. (2014). The relationship between sleep and behavior in autism spectrum disorder (ASD): A review. Journal of Neurodevelopmental Disorders, 6(1), 44.
Couturier, J. L., Speechley, K. N., Steele, M., Norman, R., Stringer, B., & Nicolson, R. (2005). Parental perception of sleep problems in children of normal intelligence with pervasive developmental disorders: Prevalence, severity, and pattern. Journal of the American Academy of Child & Adolescent Psychiatry, 44(8), 815–822.
Dahl, R. E., Pelham, W. E., & Wierson, M. (1991). The role of sleep disturbances in attention deficit disorder symptoms: A case study. Journal of Pediatric Psychology, 16(2), 229–239.
de Zambotti, M., Covassin, N., De Min Tona, G., Sarlo, M., & Stegagno, L. (2011). Sleep onset and cardiovascular activity in primary insomnia. Journal of Sleep Research, 20(2), 318–325.
Delahaye, J., Kovacs, E., Sikora, D., Hall, T. A., Orlich, F., Clemons, T. E., … Kuhlthau, K. (2014). The relationship between health-related quality of life and sleep problems in children with autism spectrum disorders. Research in Autism Spectrum Disorders, 8(3), 292–303.
DeVincent, C. J., Gadow, K. D., Delosh, D., & Geller, L. (2007). Sleep disturbance and its relation to DSM-IV psychiatric symptoms in preschool-age children with pervasive developmental disorder and community controls. Journal of Child Neurology, 22(2), 161–169.
Doane, L. D., Breitenstein, R. S., Beekman, C., Clifford, S., Smith, T. J., & Lemery-Chalfant, K. (2018). Early life socioeconomic disparities in children’s sleep: The mediating role of the current home environment. Journal of Youth and Adolescence. https://doi.org/10.1007/s10964-018-0917-3.
Elliot, C. (2007). Differential Ability Scales-II. San Antonio: The Psychological Corporation.
Elrod, M. G., & Hood, B. S. (2015). Sleep differences among children with autism spectrum disorders and typically developing peers: A meta-analysis. Journal of Developmental and Behavioral Pediatrics: JDBP, 36(3), 166–177.
El-Sheikh, M., Kelly, R. J., Buckhalt, J. A., & Benjamin Hinnant, J. (2010). Children’s sleep and adjustment over time: The role of socioeconomic context. Child development, 81(3), 870–883.
Fallone, G., Acebo, C., Arnedt, J. T., Seifer, R., & Carskadon, M. A. (2001). Effects of acute sleep restriction on behavior, sustained attention, and response inhibition in children. Perceptual and Motor Skills, 93(1), 213–229.
Finan, P. H., Goodin, B. R., & Smith, M. T. (2013). The association of sleep and pain: An update and a path forward. The Journal of Pain, 14(12), 1539–1552.
Fletcher, F. E., Foster-Owens, M. D., Conduit, R., Rinehart, N. J., Riby, D. M., & Cornish, K. M. (2017). The developmental trajectory of parent-report and objective sleep profiles in autism spectrum disorder: Associations with anxiety and bedtime routines. Autism, 21(4), 493–503.
Frazier, J. A., Biederman, J., Bellordre, C. A., Garfield, S. B., Geller, D. A., Coffey, B. J., & Faraone, S. V. (2001). Should the diagnosis of attention-deficit/hyperactivity disorder be considered in children with pervasive developmental disorder? Journal of Attention Disorders, 4(4), 203–211.
Gabriels, R. L., Cuccaro, M. L., Hill, D. E., Ivers, B. J., & Goldson, E. (2005). Repetitive behaviors in autism: Relationships with associated clinical features. Research in Developmental Disabilities, 26(2), 169–181.
Gadow, K. D., Devincent, C. J., Pomeroy, J., & Azizian, A. (2005). Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism, 9(4), 392–415.
Goldman, S. E., McGrew, S., Johnson, K. P., Richdale, A. L., Clemons, T., & Malow, B. A. (2011). Sleep is associated with problem behaviors in children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders, 5(3), 1223–1229.
Goldman, S. E., Surdyka, K., Cuevas, R., Adkins, K., Wang, L., & Malow, B. A. (2009). Defining the sleep phenotype in children with autism. Developmental Neuropsychology, 34(5), 560–573.
Goodlin-Jones, B. L., Sitnick, S. L., Tang, K., Liu, J., & Anders, T. F. (2008). The Children’s Sleep Habits Questionnaire in toddlers and preschool children. Journal of Developmental & Behavioral Pediatrics, 29(2), 82–88.
Hodge, D., Hoffman, C. D., Sweeney, D. P., & Riggs, M. L. (2013). Relationship between children’s sleep and mental health in mothers of children with and without autism. Journal of Autism and Developmental Disorders, 43(4), 956–963.
Hoffman, C. D., Sweeney, D. P., Lopez-Wagner, M. C., Hodge, D., Nam, C. Y., & Botts, B. H. (2008). Children with autism: Sleep problems and mothers’ stress. Focus on Autism and Other Developmental Disabilities, 23(3), 155–165.
Hollway, J. A., & Aman, M. G. (2011). Sleep correlates of pervasive developmental disorders: A review of the literature. Research in Developmental Disabilities, 32(5), 1399–1421.
Hollway, J. A., Aman, M. G., & Butter, E. (2013). Correlates and risk markers for sleep disturbance in participants of the autism treatment network. Journal of Autism and Developmental Disorders, 43(12), 2830–2843.
Honey, E., Rodgers, J., & McConachie, H. (2012). Measurement of restricted and repetitive behaviour in children with autism spectrum disorder: Selecting a questionnaire or interview. Research in Autism Spectrum Disorders, 6(2), 757–776.
Hoshino, Y., Watanabe, H., Yashima, Y., Kaneko, M., & Kumashiro, H. (1984). An investigation on sleep disturbance of autistic children. Psychiatry and Clinical Neurosciences, 38(1), 45–51.
Humphreys, J. S., Gringras, P., Blair, P. S., Scott, N., Henderson, J., Fleming, P. J., & Emond, A. M. (2014). Sleep patterns in children with autistic spectrum disorders: A prospective cohort study. Archives of Disease in Childhood, 99(2), 114–118.
Hundley, R. J., Shui, A., & Malow, B. A. (2016). Relationship between subtypes of restricted and repetitive behaviors and sleep disturbance in autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(11), 3448–3457.
Iglowstein, I., Jenni, O. G., Molinari, L., & Largo, R. H. (2003). Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics, 111(2), 302–307.
Jansen, P. W., Saridjan, N. S., Hofman, A., Jaddoe, V. W., Verhulst, F. C., & Tiemeier, H. (2011). Does disturbed sleeping precede symptoms of anxiety or depression in toddlers? The generation R study. Psychosomatic Medicine, 73(3), 242–249.
Jansson, M., & Linton, S. J. (2006). The role of anxiety and depression in the development of insomnia: Cross-sectional and prospective analyses. Psychology and Health, 21(3), 383–397.
Johnson, E. O., Roth, T., & Breslau, N. (2006). The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. Journal of Psychiatric Research, 40(8), 700–708.
Kaat, A. J., Lecavalier, L., & Aman, M. G. (2014). Validity of the aberrant behavior checklist in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(5), 1103–1116.
Karabekiroglu, K., & Aman, M. G. (2009). Validity of the Aberrant Behavior Checklist in a clinical sample of toddlers. Child Psychiatry and Human Development, 40(1), 99–110.
Kielinen, M., Rantala, H., Timonen, E., Linna, S., & Moilanen, I. (2004). Associated medical disorders and disabilities in children with autistic disorder: A population-based study. Autism, 8(1), 49–60.
Klukowski, M., Wasilewska, J., & Lebensztejn, D. (2015). Sleep and gastrointestinal disturbances in autism spectrum disorder in children. Development Period Medicine, 19(2), 157–161.
Krakowiak, P., Goodlin-Jones, B., Hertz-Picciotto, I., Croen, L. A., & Hansen, R. L. (2012). Sleep problems in children with autism spectrum disorders, developmental delays, and typical development: A population-based study. Journal of Sleep Research, 21(2), 231–231.
Lewandowski, A. S., Ward, T. M., & Palermo, T. M. (2011). Sleep problems in children and adolescents with common medical conditions. Pediatric Clinics of North America, 58(3), 699–713.
Leyfer, O. T., Folstein, S. E., Bacalman, S., Davis, N. O., Dinh, E., Morgan, J., … Lainhart, J. E. (2006). Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders, 36(7), 849–861.
Lopata, C., Toomey, J., Fox, J., Volker, M., Chow, S., Thomeer, M., et al. (2010). Anxiety and depression in children with HFASDs: Symptom levels and source differences. Journal of Abnormal Child Psychology, 38(6), 765–776.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Leventhal, B. L., DiLavore, P. C., … Rutter, M. (2000). The autism diagnostic observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223.
Malow, B. A. (2006). Searching for autism symptomatology in children with epilepsy—a new approach to an established comorbidity. Epilepsy Currents, 6(5), 150.
Malow, B. A., & McGrew, S. G. (2008). Sleep disturbances and autism. Sleep Medicine Clinics, 3(3), 479–488.
Mannion, A., & Leader, G. (2014). Sleep problems in autism spectrum disorder: A literature review. Review Journal of Autism and Developmental Disorders, 1(2), 101–109.
Mannion, A., & Leader, G. (2016). An investigation of comorbid psychological disorders, sleep problems, gastrointestinal symptoms and epilepsy in children and adolescents with autism spectrum disorder: A two year follow-up. Research in Autism Spectrum Disorders, 22, 20–33.
Mannion, A., Leader, G., & Healy, O. (2013). An investigation of comorbid psychological disorders, sleep problems, gastrointestinal symptoms and epilepsy in children and adolescents with autism spectrum disorder. Research in Autism Spectrum Disorders, 7(1), 35–42.
Markovich, A. N., Gendron, M. A., & Corkum, P. V. (2015). Validating the Children’s Sleep Habits Questionnaire against polysomnography and actigraphy in school-aged children. Frontiers in Psychiatry, 5, 188.
May, T., Cornish, K., Conduit, R., Rajaratnam, S. M., & Rinehart, N. J. (2015). Sleep in high-functioning children with autism: Longitudinal developmental change and associations with behavior problems. Behavioral Sleep Medicine, 13(1), 2–18.
Mayes, S. D., & Calhoun, S. L. (2009). Variables related to sleep problems in children with autism. Research in Autism Spectrum Disorders, 3(4), 931–941.
Mayes, S. D., Calhoun, S. L., Mayes, R. D., & Molitoris, S. (2012). Autism and ADHD: Overlapping and discriminating symptoms. Research in Autism Spectrum Disorders, 6(1), 277–285.
Mazefsky, C. A., Kao, J., & Oswald, D. P. (2011). Preliminary evidence suggesting caution in the use of psychiatric self-report measures with adolescents with high-functioning autism spectrum disorders. Research in Autism Spectrum Disorders, 5(1), 164–174.
Mazurek, M. O., & Petroski, G. F. (2015). Sleep problems in children with autism spectrum disorder: Examining the contributions of sensory over-responsivity and anxiety. Sleep Medicine, 16(2), 270–279.
Mazurek, M. O., & Sohl, K. (2016). Sleep and behavioral problems in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(6), 1906–1915.
Mazurek, M. O., Vasa, R. A., Kalb, L. G., Kanne, S. M., Rosenberg, D., Keefer, A., … Lowery, L. A. (2013). Anxiety, sensory over-responsivity, and gastrointestinal problems in children with autism spectrum disorders. Journal of Abnormal Child Psychology, 41(1), 165–176.
McIntosh, D., Miller, L., Shyu, V., & Dunn, W. (1999). Development and validation of the short sensory profile. Sensory Profile Manual. 59–73.
Mullen, E. M. (1995). Mullen scales of early learning. Circle Pines: American Guidance Service.
Norman, G. R., Sloan, J. A., & Wyrwich, K. W. (2003). Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care, 41(5), 582–592.
Ohayon, M. M., Carskadon, M. A., Guilleminault, C., & Vitiello, M. V. (2004). Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep, 27(7), 1255–1273.
Owens, J. A., Spirito, A., & McGuinn, M. (2000). The children’s sleep habits questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep, 23(8), 1043–1052.
Patzold, L. M., Richdale, A. L., & Tonge, B. J. (1998). An investigation into sleep characteristics of children with autism and Asperger’s disorder. Journal of Paediatrics and Child Health, 34(6), 528–533.
Reynolds, S., Lane, S. J., & Thacker, L. (2012). Sensory processing, physiological stress, and sleep behaviors in children with and without autism spectrum disorders. OTJR: Occupation, Participation and Health, 32(1), 246–257.
Richdale, A. L. (1999). Sleep problems in autism: Prevalence, cause, and intervention. Developmental Medicine and Child Neurology, 41(1), 60–66.
Richdale, A. L., & Baglin, C. L. (2015). Self-report and caregiver-report of sleep and psychopathology in children with high-functioning autism spectrum disorder: A pilot study. Developmental Neurorehabilitation, 18(4), 272–279.
Richdale, A. L., & Prior, M. R. (1995). The sleep/wake rhythm in children with autism. European Child & Adolescent Psychiatry, 4(3), 175–186.
Richdale, A. L., & Schreck, K. A. (2009). Sleep problems in autism spectrum disorders: Prevalence, nature, & possible biopsychosocial aetiologies. Sleep Medicine Reviews, 13(6), 403–411.
Riemann, D., Spiegelhalder, K., Feige, B., Voderholzer, U., Berger, M., Perlis, M., & Nissen, C. (2010). The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Medicine Reviews, 14(1), 19–31.
Rodgers, J., Wigham, S., McConachie, H., Freeston, M., Honey, E., & Parr, J. R. (2016). Development of the anxiety scale for children with autism spectrum disorder (ASC-ASD). Autism Research, 9(11), 1205–1215.
Roid, G. H. (2003). Stanford-Binet Intelligence Scales, Fifth Edition: Technical manual. Itasca: Riverside Publishing.
Roid, G. H., Miller, L. J., Pomplun, M., & Koch, C. (2013). Leiter-3: Leiter International Performance Scale. Torrance: Western Psychological Services.
Scahill, L. (2017). 27.4 Overcoming measurement challenges of anxiety in youth with autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 56(10), S41.
Scahill, L., Aman, M. G., Lecavalier, L., Halladay, A. K., Bishop, S. L., Bodfish, J. W., … Cook, E. H. (2015). Measuring repetitive behaviors as a treatment endpoint in youth with autism spectrum disorder. Autism, 19(1), 38–52.
Schreck, K. A., Mulick, J. A., & Smith, A. F. (2004). Sleep problems as possible predictors of intensified symptoms of autism. Research in Developmental Disabilities, 25(1), 57–66.
Sigafoos, J., Pittendreigh, N., & Pennell, D. (1997). Parent and teacher ratings of challenging behaviour in young children with developmental disabilities. British Journal of Learning Disabilities, 25(1), 13–17.
Simonds, J. F., & Parraga, H. (1982). Prevalence of sleep disorders and sleep behaviors in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 21(4), 383–388.
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child & Adolescent Psychiatry, 47(8), 921–929.
Souders, M. C., Mason, T. B., Valladares, O., Bucan, M., Levy, S. E., Mandell, D. S., … Pinto-Martin, J. (2009). Sleep behaviors and sleep quality in children with autism spectrum disorders. Sleep, 32(12), 1566–1578.
Stein, M. A., Mendelsohn, J., Obermeyer, W. H., Amromin, J., & Benca, R. (2001). Sleep and behavior problems in school-aged children. Pediatrics, 107(4), e60–e60.
Stepanski, E., Glinn, M., Zorick, F., Roehrs, T., & Roth, T. (1994). Heart rate changes in chronic insomnia. Stress and Health, 10(4), 261–266.
Touchette, E., Cote, S. M., Petit, D., Liu, X., Boivin, M., Falissard, B., … Montplaisir, J. Y. (2009). Short nighttime sleep-duration and hyperactivity trajectories in early childhood. Pediatrics, 124(5), e985–e993.
van Breukelen, G. J. (2013). ANCOVA versus CHANGE from baseline in nonrandomized studies: The difference. Multivariate Behavioral Research, 48, 895–922.
Vgontzas, A. N., Tsigos, C., Bixler, E. O., Stratakis, C. A., Zachman, K., Kales, A., … Chrousos, G. P. (1998). Chronic insomnia and activity of the stress system: A preliminary study. Journal of Psychosomatic Research, 45(1), 21–31.
Wechsler, D. (2002). The Wechsler Preschool and Primary Scale of Intelligence (3rd ed.). San Antonio: The Psychological Corporation.
Wechsler, D. (2003). Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV). San Antonio: NCS Pearson.
Wechsler, D. (2011). Wechsler Abbreviated Scale of Intelligence-Second Edition (WASI-II). San Antonio: NCS Pearson.
Weinberg, W. A., & Brumback, R. A. (1990). Primary disorder of vigilance: A novel explanation of inattentiveness, daydreaming, boredom, restlessness, and sleepiness. The Journal of Pediatrics, 116(5), 720–725.
Wiggs, L., & Stores, G. (2004). Sleep patterns and sleep disorders in children with autistic spectrum disorders: Insights using parent report and actigraphy. Developmental Medicine and Child Neurology, 46(6), 372–380.
Acknowledgments
The authors are extremely grateful to all the families who participated in this study. This Network activity was supported by Autism Speaks and cooperative agreement UA3 MC11054 through the U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Research Program to the Massachusetts General Hospital. This work was conducted through the Autism Speaks Autism Treatment Network.
Funding
This Network activity was supported by Autism Speaks and cooperative agreement UA3 MC11054 through the U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Research Program to the Massachusetts General Hospital. This work was conducted through the Autism Speaks Autism Treatment Network.
Author information
Authors and Affiliations
Contributions
MM collaborated on design and conceptualization of the study and drafted the manuscript; KD collaborated on study design, performed the statistical analyses, and helped to draft and critically review the manuscript; AN collaborated on study design and critically reviewed the manuscript; BM collaborated on study design and interpretation of data and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Mazurek, Dr. Dovgan, Dr. Neumeyer, and Dr. Malow declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mazurek, M.O., Dovgan, K., Neumeyer, A.M. et al. Course and Predictors of Sleep and Co-occurring Problems in Children with Autism Spectrum Disorder. J Autism Dev Disord 49, 2101–2115 (2019). https://doi.org/10.1007/s10803-019-03894-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-019-03894-5