Abstract
Allied health professionals (AHPs) are trusted sources of information and intervention for clients with autism spectrum disorder. However, the level of implementation of empirically-supported therapies and the accuracy of the knowledge they use to inform intervention selection is largely unknown. The present study explored the accuracy of AHPs’ knowledge and use of practices, and explored links to individual attitudes and organisational culture. Overall results from the 156 AHPs surveyed suggested general accuracy of knowledge, and use of empirically supported treatments, with accuracy linked to use. Use of practices unsupported by research was linked to organisational culture and openness to new interventions. The presence of misinformation and the impact on selection and use of effective practices are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is a high-incidence (e.g., Centers for Disease Control 2016) neurodevelopmental disorder characterised by core impairments in social communication and interaction, as well as by restricted, repetitive patterns of behaviour, interests, or activities (American Psychiatric Association [APA] 2013). High quality intervention can improve outcomes (e.g., see reviews by (NAC) 2015; Wong et al., 2015), but no single intervention or therapy is universally recommended (Lord and Bishop 2010; Lord et al. 2005; Roberts et al. 2016; Trembath and Vivanti 2014). ASD has been described as a “fad magnet” (e.g., Metz et al. 2005, p. 246) with over 1000 different interventions with varying efficacy and safety available (e.g., Research Autism 2017). To address the challenge of navigating this wide variety of interventions, practice guidelines have been developed in some countries (e.g., Australia: Early Intervention for Children with ASDs: ‘Guidelines for Good Practice’, Prior and Roberts, 2012; USA: National Standards Project (NSP), NAC 2015; UK: National Collaborating Centre for Mental Health [NCCMH], NCCMH 2013). These guidelines include a general emphasis on an evidence-based practice approach that promotes the integration of the best available research evidence with practitioner expertise, based on understanding of the individual’s strengths, needs, values, and preferences (Sackett et al. 1996). While the best available research evidence is available in the form of systematic reviews (e.g., NAC 2015; Wong et al. 2015), in allied healthcare, the extent of translation of empirically supported treatments (ESTs) for clients with ASD to real world clinical practice and barriers/facilitators to uptake has received little attention, and is the focus of this study.
Allied health professionals (AHPs) play a key role in the field of ASD in implementing interventions, recommending the use of strategies to families, and upskilling parents as co-therapists (as outlined in Ridge and Guerin 2011). This means that AHPs, including psychologists, speech pathologists and occupational therapists, can be highly influential in the choice of treatments and interventions received by children with ASD in the community. In selecting interventions for their children, parents may well assume that AHPs are aware of the evidence base of various practices (Auert et al. 2012), tend to trust their advice (Carlon et al. 2015; Deyro et al. 2016), and rate them highly as sources of information (Deyro et al. 2016; Hennel et al. 2016). Furthermore, parents are likely to expect therapists to use only evidence-based interventions, and overwhelmingly express support for the evidence-based practice (EBP) framework (Auert et al. 2012). AHPs, conversely, report feeling challenged by high levels of misinformation about effectiveness of interventions and, in the words of Ridge and Guerin (2011), “described a tendency in the field of ASD for the proliferation of exaggerated claims on treatment benefits” (p. 246). In order to make informed intervention choices, support children with ASD and their families, and ultimately achieve optimal outcomes, it is crucial that AHPs are well trained and thoroughly versed in the latest research on ASD (Paynter et al. 2017; Roberts et al. 2016). A serious problem arises when therapists employ ineffective practices, or recommend using them to parents (Miller et al. 2012). Thus, gauging AHPs’ attitudes towards the EBP framework, as well as their knowledge and use of ESTs is important.
There is strong support for the EBP framework among AHPs, as evidenced by research and widespread acknowledgement of its importance among professional bodies. For example, Vallino-Napoli and Reilly (2004), as well as Zipoli and Kennedy (2005), reported that the majority of speech-language pathologists they had surveyed in Australia and in the United States, respectively, maintained positive attitudes toward research and EBP, and wished to keep abreast of clinical developments. Furthermore, positive attitudes to EBP have also been linked to the use of ESTs in early intervention practitioners including AHPs (Paynter and Keen 2015; Paynter et al. 2017). Finally, research with early intervention practitioners including AHPs, suggests greater use of ESTs than practices unsupported by research (e.g., Paynter and Keen 2015; Paynter et al. 2017; Stahmer et al. 2005). However, across these studies, use of practices shown to be ineffective in research (e.g., facilitated communication), and with insufficient evidence (e.g., music therapy) are reported to be used by at least some participants; in addition, AHPs do not always implement ESTs (Wilkinson et al. 2012). This raises the question of why professionals use unsupported treatments, and/or do not use ESTs, despite generally positive attitudes to the concept of EBP.
Greater use of ESTs, and lower use of unsupported practices, has been linked to individual (e.g., knowledge, attitudes) and organisational (e.g., culture) factors. Paynter and Keen (2015) found early intervention staff (including AHPs) in a single organisation in Australia reported using a blend of practices categorised as unsupported (i.e. lacking empirical evidence), emerging (i.e. limited empirical support), and ESTs (i.e. sufficient research support) (as determined by the Wong et al. 2015, review). Greater use of ESTs was linked to location (with those working in metropolitan areas reporting greater EST use than those in regional areas), more positive individual attitudes to EBP generally, perception of a more supportive organisational culture towards EBP, and greater self-reported knowledge of the individual practices (Paynter and Keen 2015). Paynter et al. (2017) replicated these findings across a number of EI providers. Taken together these findings suggest the potential roles of individual, as well as organisational, factors on utilisation of ESTs.
Cheung et al. (2013) likewise found organisational factors impacted on EST implementation. Speech-language pathologists working with children with ASD in Australia mostly agreed that EBP is necessary, but reported they experienced barriers to implementation including an uncongenial workplace culture, insufficient support, lack of time, high costs, and the limited availability and accessibility of resources (Cheung et al. 2013). Thus, organisational factors may both enable (via supportive organisational culture as per Paynter and Keen 2015; Paynter et al. 2017) and form barriers (Cheung et al. 2013) to implementation of ESTs.
Sources of information available to individuals from, and through, their organisations may also influence EST uptake. Nail-Chiwetalu and Ratner (2007) showed for example, that in the United States, speech-language pathologists most often consulted with a colleague, participated in continuing education activities, and searched the open Internet for information to inform practice. Few respondents in their study reported relying on scholarly journal articles for assistance with clinical cases. A decade later, Paynter et al. (2017) likewise found a reliance on other AHPs and internal/external professional development more so than research or scholarly sources to inform ASD early intervention choices, implying a sustained preference for sourcing information in this way. Paynter et al. (2017) acknowledged that these information sources can be helpful when they are of high quality and provide instruction on the use of ESTs. However, they also noted that these sources can be problematic if they are inaccurate or endorse unsupported practices whereby they may pave the way for misinformation, which may consequently be perpetuated within an organisational or professional system.
Emerging research suggests that parents and AHPs are sometimes inaccurate in their understanding of the evidence base of intervention practices which may consequently impact on selection of interventions. For example, parents of children with ASD have been found to show inaccurate categorisation of interventions in terms of their empirical support (e.g., Deyro et al. 2016). Further, one study (Kadar et al. 2012) suggests that inaccurate knowledge of treatment efficacy may relate to the use of specific practices in AHPs. Kadar et al. (2012) found that occupational therapists reported frequently using therapies associated with, or based on, sensory integration, believing erroneously that it was an empirically supported practice yet evidence at this time was weak (e.g., Case-Smith and Arbesman 2008) and a growing body of evidence described it as both unsupported and not recommended (e.g., Lang et al. 2012). Finally, previous research with EI staff, including AHPs, found significant correlations between self-reports of perceived knowledge of practices and their greater use (Paynter and Keen 2015; Paynter et al. 2017), suggesting that knowledge may be an important, and modifiable, factor that affects use. This research, however, investigated perceived rather than actual knowledge, that is, self-rating of how much one knows about a treatment rather than accurate ratings of its evidence base. There is thus a need to probe ways in which AHPs’ use of intervention practices is related to their knowledge of the evidence base supporting these interventions, specifically the accuracy of this knowledge.
To summarise, AHPs not only work directly with people with ASD as intervention providers, but are also an important, valuable, and trusted source of information regarding available interventions (Ridge and Guerin 2011). Parents of children with ASD assume that AHPs keep abreast of research and use only practices backed by adequate empirical support (Carlon et al. 2015; Deyro et al. 2016). Yet, the extent to which these assumptions hold in real world practice is largely unknown. Emerging evidence attests to a continued use of ineffective practices (e.g., Kadar et al. 2012; Miller et al. 2012), which may in part be due to false beliefs about the evidence-base of treatments (e.g., Kadar et al. 2012) and/or questionable reliability of sources (e.g., colleagues) used to verify the evidence base of treatments (e.g., Paynter et al. 2017). Furthermore, the implementation of ESTs has been linked to individual attitudes to EBP, as well as to the support for EBP within an organisational culture (e.g., Paynter and Keen 2015; Paynter et al. 2017). To date, understanding of the evidence base of strategies, use of strategies, individual and organisational support for EBP, and sources of information, have not been explored in a single study with AHPs who work with people with ASD in the community. Such research would add to our understanding about the translation of research to practice and factors that may hinder or facilitate uptake in order to achieve optimal outcomes for people living with ASD. The present study targeted this gap in the literature by exploring AHPs’ levels of knowledge regarding the evidence base of common ASD intervention practices as well as factors associated with greater use of ESTs. AHPs included in the study included speech pathologists, occupational therapists, psychologists, and behaviour analysts following from previous research (e.g., Paynter and Keen 2015; Paynter et al. 2017). Consistent with previous research, we also explored links to organisational culture and attitudes to EBP, as well as sources of information accessed by AHPs. The following research questions were addressed:
-
1.
How accurately do AHPs classify the evidence base of ASD intervention strategies?
-
2.
Do AHPs use ESTs more than emerging or unsupported practices?
-
3.
What are the interrelationships between ASD accuracy of categorisation of the evidence base of strategies, use of ESTs and unsupported practices, and organisational, attitudinal and demographic variables?
-
4.
Are there differences between allied health subgroups in accuracy of classification of practices, and use of ESTs and unsupported practices?
-
5.
What sources of information do AHPs access to inform treatment selection and how trustworthy do they find these sources?
It was anticipated that accuracy in categorising practices according to their evidence base would be positively linked to the use of ESTs. Further, it was hypothesised that AHPs would use more ESTs than emerging or unsupported practices. The use of ESTs was expected to be positively linked to more supportive individual and organisational cultures towards EBP. No specific predictions were made in terms of group differences or sources of information due to the paucity of research in this area.
Method
Participants
This study was conducted with approval from the Human Research Ethics Committee of the authors’ university (Griffith University Research Ethical Clearance Reference Number 2016/495). Recruitment was conducted via social media (e.g., Australian allied health special interest groups on Facebook), and email requests to the authors’ professional networks and relevant practitioners drawn from ASD provider lists in Australia. Inclusion criteria included the participant being an allied health professional (speech language pathologist, psychologist, behaviour analyst, or occupational therapist) who was currently working with individuals with ASD. One hundred and seventy participants commenced the survey, however 14 ceased at the demographics section, and were thus excluded from the study. Postcodes collected of employment location were consistent with Australian postcodes for 92% of participants, although country was not specifically verified. Demographic information for the 156 included participants is shown in Table 1.
The majority of participants were female (94.2%), between the ages of 26 and 35 years (43.2%), and worked as part of a multi-disciplinary team (39.4%). Half (50.3%) of the participants held a postgraduate degree as their highest qualification (note this is not required for registration in Australia). This included 34/35 psychologists, 10/17 behaviour analysts, 12/35 occupational therapists, and 25/68 speech pathologists who answered this question, with a statistically significant moderately strong association of role and qualification, χ2(3) = 39.63, p < .001, φ = 0.506. The majority of participants were speech language pathologists (43.9%), followed by psychologists (22.6%), occupational therapists (21.9%), and behaviour analysts (11.6%). Time in profession ranged between 1 month and 39 years (M = 10.44 years, SD = 8.79 years), and time in current role between 1 month and 31.5 years (M = 4.72 years, SD = 5.17 years). Time working with individuals with ASD ranged between 1 month and 34 years (M = 10.11 years, SD = 8.17 years), with the majority of participants working with individuals between the ages of 0–5 years (91.6%) targeting social skills (95.5%). As seen in Table 2, therapists ranged in which area they most commonly worked in with their clients with ASD. For example, the most common areas were: speech pathologists in communication; occupational therapists in school readiness and adaptive behaviour; psychologists in social skills; and behaviour analysts in social skills, communication, and challenging behaviour.
Measures
The online survey included 149 questions across five subject areas as described below.
Demographics
Questions included age bracket, location of work, type of practice (e.g., multidisciplinary, sole practice), age group of clients with ASD, highest academic qualification, current role and profession, time working with individuals with ASD.
Practice Use and Knowledge of the Evidence Base
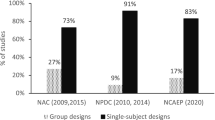
The measure was a modified version of the Early Intervention Practices Scale Revised (Paynter et al. 2017) which was adapted from the Early Intervention Practices Scale (Paynter and Keen 2015). The measure included a list of 45 practices with brief definitions including practices categorised as established (EST: n = 29), emerging (n = 6), or unsupported by research (n = 10) based on recent reviews (Wong et al. 2015; NAC 2015). For further information on scale development please see Paynter and Keen (2015) and Paynter et al. (2017). The use scale was retained from these earlier scales, and evidence category was added to test accuracy of knowledge of each intervention’s evidence base. Participants were asked to categorise each practice from five possible categories including harmful, ineffective, unestablished, emerging, or established with definitions provided for each as per National Autism Centre categories as used in Deyro et al. (2016). Ratings of use were summed across items in each category to create an EST use (α = .90), emerging use (α = .68), and unsupported use (α = .74). As emerging showed lower reliability (in terms of internal consistency) beyond initial comparisons which were required to address the research question, the focus of analyses was on EST and unsupported use. Accuracy of categorisation was calculated as a total score as outlined in the “Results” section.
Organisational Culture
The Organisational Culture Questionnaire (Russell et al. 2010) includes three scales: resources (four items), culture (three items) and supervisor (single item), as well as a total score (all eight items). Participants rated their level of agreement with each item from 1 = Not at all to 10 = To a great extent. To better reflect the areas in which allied health professionals might work, the authors made minor wording changes for the term “organisation” to “workplace” throughout this questionnaire. All scales with multiple items showed good reliability in the current study (total, α = .94; resources, α = .88; culture, α = .94).
Attitudes to EBPs
The Evidence-based Practices Attitudes Scale (EBPAS: Aarons 2004) includes four subscales: requirements (three items), appeal (four items), openness (four items), and divergence. Participants rated statements on a 5-point scale from 0 = Not at all to 4 = To a very great extent. Adequate (openness α = .64) to good (requirements α = .92; appeal α = .83; total α = .79) reliability was found for most scales, with poor reliability found for the divergence scale (α = .58) which was consequently eliminated from further analysis.
Sources of Information
The Sources of Information Scale was a modified version of a scale developed for parents (Carlon et al. 2015) that was subsequently adapted and used in previous research (Paynter et al. 2017). The scale included 18 items identifying possible sources of information that could be accessed when learning about intervention practices used for individuals with ASD (e.g. professional bodies such as Speech Pathology Australia) rated on a dichotomous yes/no to whether participants received information from each. Additionally, a 5-point rating of trust of sources from 0 = Not at all trustworthy to 4 = Very trustworthy, or not applicable was used.
Procedure
Data was collected between July and November of 2016 using the SurveyMonkey online platform. Participants first read the information sheet, then indicated consent in order to proceed to the survey. Participants then completed the remainder of the survey which took approximately 30 min. All responses to the survey were anonymous.
Results
Data Screening
Missing values analysis revealed non-completions at the item level (7.1–36.5% with 25% overall missing), however data were missing completely at random (Little’s MCAR test Chi-Square = 4243, df = 4243, p = .998) thus listwise deletion was used for each analysis. Upon inspection of box plots, several outliers were identified, investigation revealed however that only one participant demonstrated a pattern of careless responding on the intervention practices scale (as they answered all questions the same). This participant’s data were consequently removed from further analysis. Three univariate outliers (all on the EBPAS scales with one on the appeal, openness, and attitude total scales) were found to be genuine data points and were not influential data points and were thus retained. An additional outlier was detected during screening for the total accuracy of categorisation by allied health role analysis. Removal of the outlier did not alter the results of the analysis and it was therefore retained. Three within groups outliers were identified when screening for the average use of unsupported practices by allied health role analysis. These participants were removed from the analysis due to being influential cases.
Violations of normality were detected for behaviour analyst scores on average use of unsupported practices (standardised skew and kurtosis z > 3.29). However, as ANOVAs are robust to these violations (Maxwell and Delaney 2004), and for ease of interpretation, these were analysed without transformation. Where violations of homogeneity of variances exist in the group comparisons (Levene’s p < .05), Welch’s F statistics have been used.
Accuracy of Categorisation of the Evidence Base of Practices
To evaluate accuracy of categorisation against the original scale (Paynter et al. 2017) participant categorisation of the evidence base of strategies was recoded into three categories, whereby practices categorised as harmful, ineffective, or unsupported were grouped together into a single category of “unsupported,” and emerging, and established were retained, see Table 3. Modal responses were consistent with categorisation for most practices, for example, the strategies most often categorised as established (reinforcement, functional behavioural assessment, discrete trial teaching, PECS, and modelling) were most commonly categorised as established by participants. However, a number of ESTs were rarely correctly classified as established including technology aided-instruction (7.69%), self-management (15.93%), exercise (16.10%), peer-mediated instruction (19.47%), and time delay (22.12%). Some participants inaccurately reported a number of unsupported practices as being established including facilitated communication (n = 14), academic interventions (n = 43), and multisensory environments (n = 15).
Accuracy of categorising individual practices within a category were summed to create a total accuracy score for unsupported (α = .73), emerging (α = .29), and established practices (α = .87), as well as a total score (α = .77). The emerging scale showed poor reliability with Cronbach’s α = .29, and was thus omitted from further analyses beyond initial comparisons below; all other scales showed adequate to good reliability. Mean accurate classification of unsupported practices was 6.61/10 (SD = 2.44, range 1–10), emerging was 2.23/6 (SD = 1.33, range 0–6), and for established was 13.48/29 (SD = 6.19, range 0–24). Participants significantly differed in their percentage accuracy of classification for each of the three categories, F (2, 206) = 37.99, p < .001, ηp2 = 0.27. Post hoc analysis with a Bonferroni adjustment showed participants correctly classified a greater percentage of unsupported (M = 66.06, SD = 2.40) than emerging practices (M = 37.18, SD = 2.18, p < .001), or ESTs (M = 46.49, SD = 2.09, p < .001). ESTs were correctly classified a greater percentage of the time than emerging strategies, p = .025. Overall, participants who rated all practices (n = 104), accurately classified 22.47 practices (SD = 6.17) of the 45 practices, with a range of 8–34.
Use of Practices
Each practice was used at least on rare occasions by at least one participant (see Table 4). The most frequently used practices (in order from most to least) were modelling (M = 3.30), reinforcement (M = 3.06), visual supports (M = 3.05), antecedent-based interventions (M = 2.96), and parent-implemented interventions (M = 2.88). These five practices all fall under the established category. The least used practices were (in order from least to most): holding therapy (M = 0.01), auditory integration training (M = 0.19), brushing/Wilbarger Protocol (M = 0.41), PROMPT method (M = 0.56), and facilitated communication (M = 0.73). These five practices all fall under the unsupported practice category.
A one-way repeated measures ANOVA was conducted to determine whether statistically significant difference existed in participants’ reported use of ESTs, emerging practices, and unsupported practices. The assumption of sphericity was violated as determined by Mauchley’s test of sphericity (p < .05). Therefore, a Greenhouse–Geisser correction was applied (ε = 0.904). Participants reported statistically significant differences in their use of the three classifications of practices, F (1.808, 184.45) = 204.447, p < .001, ηp2 = 0.668. Post hoc analysis with a Bonferroni adjustment revealed that participants used ESTs (M = 2.16, SD = 0.64) more frequently than both emerging (M = 1.50, SD = 0.77) and unsupported (M = 0.74, SD = 0.57) practices (all p’s < .001). Emerging practices were also used more frequently than unsupported practices (p < .05).
Correlations with Use
Correlations between EST and unsupported practice use, accuracy of categorisation, attitudes (to EBP), and organisational culture (support for EBP) are shown in Table 5. Use of EST was significantly correlated to accuracy of categorisation, showing those who more accurately categorised established practices were more likely to report using them (r = .50, p < .001). Higher use of unsupported practices was linked to lower accuracy of categorising these practices (r = − .50, p < .001). No significant correlations were observed between use of ESTs and any attitudinal or organisational culture variables. Use of EST was significantly correlated with time working with people with ASD (r = .21, p = .03), but not overall time in the profession. Openness to new strategies showed a small, but significant, correlation with use of unsupported practices (r = .21, p = .03). Organisational culture (culture subscale) showed a small, significant negative correlation, with use of unsupported practices whereby a less supportive perceived organisational culture was associated with greater use of unsupported practices (r = − .24, p = .02).
Professional Group Comparisons
Total Accuracy of Categorisation
Total accuracy of categorisation differed significantly according to participant’s allied health role, Welch’s F(3, 44.73) = 17.92, p < .001, ηp2 = 0.546. Overall, behaviour analysts showed the highest accuracy (M = 28.64), followed by psychologists (M = 24.12), speech pathologists (M = 22.10), and occupational therapists (M = 18.63; see Table 6). Games-Howell post hoc analysis revealed that behaviour analysts showed significantly higher overall accuracy in classifying interventions compared to speech pathologists (p < .001), occupational therapists (p < .001), and psychologists (p = .006). Psychologists were also found to be significantly higher in their accuracy of categorisation than occupational therapists (p = .004). No other significant group differences were observed.
Average Use of Unsupported Practices
Average use of the ten unsupported practices differed significantly according to participant’s allied health role, Welch’s F(3, 39.48) = 9.31, p < .001, ηp2 = 0.414. Occupational therapists reported highest use with a mean of 1.05/5 suggesting they used unsupported practices “on rare occasions”. The next highest use was reported by speech pathologists, followed by psychologists, with least use reported by behaviour analysts. Games-Howell post hoc analysis revealed that speech pathologists reported using unsupported practices significantly more frequently than both psychologists (p = .020), and behaviour analysts (p = .009). Similarly, occupational therapists were also found to use unsupported practices significantly more frequently than psychologists (p = .001) and behaviour analysts (p = 001). No other significant group differences were found.
Average Use of ESTs
Average use of the 29 ESTs differed significantly according to participants’ allied health role, Welch’s F(3, 42.34) = 3.949, p = .014, ηp2 = 0.219. Behaviour analysts reported using ESTs the most, with a mean of 2.54/5, suggesting they used ESTs “sometimes”. This was followed by speech pathologists, psychologists, and occupational therapists (see Table 6). However, a Games-Howell post hoc analysis revealed that the only significant difference was that behaviour analysts reported using ESTs more frequently than psychologists (p = .025).
Sources of Information
The results for 99 participants who completed the sources of information and ratings of trustworthiness are presented in Table 7. Participants rated research literature as the most trusted source of information (M = 4.60) between somewhat and very trustworthy, with 99.0% of participants reporting having accessed research literature. The most frequently accessed, as well as next highly trusted, sources of information were workshops and external professional development (100%, M = 4.57), other therapists (99.0%, M = 3.92), and internal professional development and training (95.9%, M = 4.38).
The least commonly accessed sources were complementary and alternative medical practitioners (CAMs) (28.2), positive partnerships website (45.5%), social media (49.5%), and print media/television (54.5%). The least trusted sources were CAMs (M = 2.07), social media (M = 2.14), print media/television (M = 2.37), and friends and relatives (M = 2.51). These were rated between untrustworthy and neither trustworthy nor untrustworthy.
Discussion
The present study explored AHP’s accuracy of knowledge of the evidence base of common ASD interventions, and how this related to their use. Further, we explored the links between individual attitudes, organisational culture, and use, comparisons across professions, and sources of information accessed. Overall, modal responses indicated accurate categorisation of practices; ESTs were used more than emerging, or unsupported practices; and accuracy of categorisation was linked to use as hypothesised. In contrast to expectations, attitudinal and organisational variables were not linked to use of ESTs, but organisational culture, and openness to using new strategies were linked to use of unsupported practices. Differences between subgroups of AHPs emerged in use and accuracy of categorisation. Finally, the most used sources of information were workshops/external professional development, other AHPs, and professional development/training, with the most trusted being research literature, although this was not the most accessed. These findings extend previous research into intervention choices of AHPs.
Consistent with previous research with early intervention practitioners (e.g., Paynter and Keen 2015; Paynter et al. 2017; Stahmer et al. 2005), overall, participants in this study reported using more ESTs than emerging or unsupported practices, yet all practices including unsupported, were used at least occasionally by a small number of practitioners. For example, some participants reported using unsupported practices multiple times per week including holding therapy, auditory integration training, brushing/Wilbarger Protocol, PROMPT, and facilitated communication. A potential reason for this, is that although overall practitioners tended to accurately classify practices on their evidence base at a group level, significant variability between individual participants was found with some classifying as few as 8 of the 41 practices correctly. This accuracy of classification was, as predicted, linked to use, thus suggesting misinformation about the evidence base links to use or non-use of ESTs as well as unsupported practices. Consistent with this suggestion, a number of participants misclassified some unsupported practices including facilitated communication, academic interventions, and multisensory environments, as established practices. This is contrast, for example, to the significant literature clearly showing the ineffectiveness of FC as well as demonstration of harms (e.g., Sigafoos and Schlosser 2012; Boynton 2012), combined with explicit statements against use of FC by professional organisations (e.g., see discussions in Gorman 1998; Lilienfeld 2005; Lilienfeld et al. 2014; Mostert 2010). False beliefs about the effectiveness of this strategy may thus lead to its continued use in the community (e.g., Trembath et al. 2015). These beliefs may be perpetuated within a profession or organisation with participants reporting sourcing information most commonly from their colleagues and internal/external professional development and trusting these sources.
In addition to accuracy of knowledge of the evidence base of unsupported practices, attitudes to EBP and organisational culture support were also explored as predictors of use of unsupported practices. Openness to using new practices was significantly linked to greater use of unsupported practices which is a novel finding with previous research investigating links to EST use only (Paynter and Keen 2015; Paynter et al. 2017). It may be that this openness can make a practitioner vulnerable to unsupported practices that may be promoted through highly trusted, but poor quality, sources. Alternatively, it may be that openness encourages an “early adopter” mentality in some individuals who may be willing to try new practices that have yet to be subjected to empirical research. How such individuals may seek and incorporate new evidence to change or adapt their practice as research emerges, and whether use persists if evidence of ineffectiveness emerges, is an important question for further research. Further, a more negative organisational culture towards EBPs was linked to greater use of unsupported practices. This is consistent with Cheung et al. (2013) finding that organisational factors can form barriers to implementation of ESTs, which may then lead practitioners to using unsupported practices instead.
In contrast to previous studies (Cheung et al. 2013; Paynter and Keen 2015; Paynter et al. 2017), organisational and attitudinal factors were not significantly linked to use of ESTs in AHPs. This difference may reflect more positive organisational cultures and/or attitudes towards EBPs by AHPs as a group compared to participants drawn from more diverse professions including educators and paraprofessionals. Some evidence for this suggestion, is seen in the higher perceived organisational culture support and attitudes to EBP (requirements subscale) in professionals (including AHPs) compared to paraprofessionals in Paynter and Keen’s (2015) study. Alternatively, it may be that other factors (such as beliefs of the evidence base of strategies as shown in this study) predict use of ESTs in AHPs in Australia which may differ from practitioners working in EI (Paynter and Keen 2015; Paynter et al. 2017). For example, we found that experience working with clients with ASD was linked to greater use of ESTs, and that there were differences between professions in reported use and accuracy of categorisation.
Group comparisons across professions showed differences in both level of use of ESTs and accuracy. Highest levels of EST use and accuracy were found in behaviour analysts who are specifically trained in interventions based on the principles of applied behaviour analysis. This finding is perhaps not surprising given behavioural interventions have arguably been the most well researched interventions for individuals with ASD and have a strong evidence base with many of these interventions listed in reviews (e.g., Wong et al. 2015). This study also found that groups differed both in qualifications and in the type of support they provided which may impact EST use. For example, psychologists who often reported working in mental health could draw on only a small number of ESTs (e.g., cognitive behaviour interventions). In contrast, behaviour analysts, who most commonly reported working with challenging behaviour, could draw from 21 ESTs. Some AHPs may thus have a more limited range of ESTs available to inform practice and this may explain differing rates of EST use. Further, practitioners may be more familiar with practices related to their workplace and be less able to categorise practices more commonly used by other professions. However, given the emphasis on multidisciplinary approaches to intervention as being best practice (e.g., Prior and Roberts 2012) and trust of parents in AHPs to inform treatment choices (Carlon et al. 2015; Deyro et al. 2016) understanding of the evidence base of a range of ASD practices is argued to be valuable for all practitioners.
The present study demonstrates a number of strengths including addressing a novel, but important, area of AHPs use of ASD intervention practices and related factors, and by including accuracy of knowledge of the evidence base, attitudes, organisational culture, and sources of information in a single study. Nevertheless, a number of limitations should be acknowledged when interpreting these findings. Data were drawn from self-reports on questionnaire measures. Respondents were provided with a list of intervention practices that limited opportunities for them to rate practices they may know about or use that were not included. As with previous research of this nature (e.g., Paynter and Keen 2015; Paynter et al. 2017), reliance on self-report leaves unanswered questions about frequency and fidelity of use of these practices by AHPs. Further, it does not capture novel or new practices that may be available in the field. In addition, the “perceived evidence scale” combined the three categories of harmful, ineffective, and unsupported into a single “unsupported” categorisation for comparison to the original scale, which poses a potential limitation. For example, the factors linked to using a new practice without research support yet (e.g., may link to openness to using new strategies) may be different to those linked to using a practice that has been shown to be ineffective (e.g., may link to misinformation about the evidence-base). Thus, research using direct observation or interview methods may be beneficial to elucidate the full spectrum of practices and potential factors linked to use in future research. Further, particularly given our predominantly Australian sample, collection of country of origin data and international comparison would be valuable to understand similarities and differences in practice internationally.
Our focus was on the best available evidence, i.e. ESTs identified via systematic reviews, and we did not capture the decision-making process and consideration of practitioner expertise and individual client factors encapsulated in the broader EBP framework. It is possible, some use of emerging, or even unsupported practices, was driven by consideration of these additional factors. How practitioners balance what may be conflicting pressures in these three domains is an important area for future research. Further, how practitioners select treatments when the evidence-base is limited requires further investigation as AHPs may need to draw more heavily on emerging practices. It is important that we better understand how they do this within the broader EBP framework. Thus, while research into interventions for ASD is expanding, what practitioners can do in real world settings while the research “catches up” with clinical realities is an important matter for future research.
In summary, AHPs play a vital role in the translation of research to practice as they implement interventions and information they provide about intervention practices to other professionals and families is often valued and trusted, increasing their circle of influence beyond their own practice. It is therefore critical that research evidence informs both their clinical work and the information they provide to others. This research has highlighted some gaps in knowledge translation for AHPs with evidence of inaccurate categorisation of the evidence base of strategies by some practitioners linked to use of ineffective and even harmful strategies. This has implications for AHP undergraduate education programs and ongoing professional development. As AHPs rate peers in professional networks above research literature as highly valued and trustworthy sources of information, research needs to focus on ways of disseminating accurate information to practitioners via these most valued and trusted sources. Finally, the challenges across subgroups of AHPs in knowledge translation may vary depending on professional role and work context. Some professionals may require greater support in using an evidence-based framework when the research evidence is limited. Our findings emphasise the need for effective strategies for knowledge translation to allied health professionals to support high quality intervention for individuals with ASD in the community to support achievement of the best possible outcomes.
References
Aarons, G. A. (2004). Mental health provider attitudes toward adoption of evidence-based practice: The Evidence-Based Practice Attitude Scale (EBPAS). Mental Health Services Research, 6(2), 61–74.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Auert, E. -J., Trembath, D., Arciuli, J., & Thomas, D. (2012). Parents’ expectations, awareness, and experiences of accessing evidence-based speech-language pathology services for their children with autism. International Journal of Speech-Language Pathology, 14(2), 109–118.
Boynton, J. (2012). Facilitated Communication—what harm it can do: Confessions of a former facilitator. Evidence-Based Communication Assessment and Intervention, 6(1), 3–13. https://doi.org/10.1080/17489539.2012.674680.
Carlon, S., Carter, M., & Stephenson, J. (2015). Decision-making regarding early intervention by parents of children with autism spectrum disorder. Journal of Developmental and Physical Disabilities, 27(3), 285–305.
Case-Smith, J., & Arbesman, M. (2008). Evidence-based review of interventions for autism used in or of relevance to occupational therapy. The American Journal of Occupational Therapy, 62(4), 416–429.
Centers for Disease Control and Prevention. (2016). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2012. Surveillance Summaries, 65(3), 1–23.
Cheung, G., Trembath, D., Arciuli, J., & Togher, L. (2013). The impact of workplace factors on evidence-based speech-language pathology practice for children with autism spectrum disorders. International Journal of Speech-Language Pathology, 15(4), 396–406.
Deyro, M. C., Simon, E. W., & Guay, J. (2016). Parental awareness of empirically established treatments for autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 31(3), 184–195.
Gorman, B. J. (1998). Facilitated communication in America: Eight years and counting. Skeptic, 6(3), 64–71.
Hennel, S., Coates, C., Symeonides, C., Gulenc, A., Smith, L., Price, A. M. H., & Hiscock, H. (2016). Diagnosing autism: Contemporaneous surveys of parent needs and paediatric practice. Journal of Paediatrics and Child Health, 52(5), 506–511.
Kadar, M., McDonald, R., & Lentin, P. (2012). Evidence-based practice in occupational therapy services for children with autism spectrum disorders in Victoria, Australia. Australian Occupational Therapy Journal, 59(4), 284–293.
Lang, R., O’Reilly, M., Healy, O., Rispoli, M., Lydon, H., Streusand, W., … Lancioni, G. (2012). Sensory integration therapy for autism spectrum disorders: A systematic review. Research in Autism Spectrum Disorders, 6(3), 1004–1018.
Lilienfeld, S. O. (2005). Scientifically unsupported and supported interventions for childhood psychopathology: A summary. Pediatrics, 115(3), 761–764. https://doi.org/10.1542/peds.2004-1713.
Lilienfeld, S. O., Marshall, J., Todd, J. T., & Shane, H. C. (2014). The persistence of fad interventions in the face of negative scientific evidence: Facilitated communication for autism as a case example. Evidence-Based Communication Assessment and Intervention, 8(2), 62–101. https://doi.org/10.1080/17489539.2014.976332.
Lord, C., & Bishop, S. L. (2010). Autism spectrum disorders: Diagnosis, prevalence, and services for children and families. Social Policy Report Society for Research in Child Development, 24(2), 1–21.
Lord, C., Wagner, A., Rogers, S., Szatmari, P., Aman, M., Charman, T., … Guthrie, D. (2005). Challenges in evaluating psychosocial interventions for autistic spectrum disorders. Journal of Autism and Developmental Disorders, 35(6), 695–708.
Maxwell, S. E., & Delaney, H. D. (2004). Designing experiments and analyzing data: A model comparison perspective (Vol. 2nd). Mahwah: Lawrence Erlbaum Associates.
Metz, B., Mulick, J. A., & Butter, E. M. (2005). Autism: A late-20th-century fad magnet. In J. W. Jacobson, R. M. Foxx, & J. A. Mulick (Eds.), Controversial therapies for developmental disabilities: Fad, fashion and science in professional practice (pp. 237–263) Mahwah: Lawrence Erlbaum Associates.
Miller, V. A., Schreck, K. A., Mulick, J. A., & Butter, E. (2012). Factors related to parents’ choices of treatments for their children with autism spectrum disorders. Research in Autism Spectrum Disorders, 6(1), 87–95.
Mostert, M. P. (2010). Facilitated communication and its legitimacy—Twenty-first century developments. Exceptionality, 18(1), 31–41. https://doi.org/10.1080/09362830903462524.
Nail-Chiwetalu, B., & Ratner, N. B. (2007). An assessment of the information-seeking abilities and needs of practicing speech-language pathologists. Journal of the Medical Library Association, 95(2), 182.
National Autism Centre. (2015). Findings and Conclusions: National Standards Project Phase 2. Retrieved September 29, 2017, from http://www.nationalautismcenter.org/national-standards-project/phase-2/.
National Collaborating Centre for Mental Health. (2013). Autism: The management and support of children and young people on the Autism Spectrum. Leicester: British Psychological Society.
Paynter, J., Ferguson, S., Fordyce, K., Joosten, A., Paku, S., Stephens, M., … Keen, D. (2017). Utilisation of evidence-based practices by ASD early intervention service providers. Autism, 21(2), 167–180.
Paynter, J., & Keen, D. (2015). Knowledge and use of intervention practices by community-based early intervention service providers. Journal of Autism and Developmental Disorders, 45(6), 1614–1623.
Prior, M., & Roberts, J. (2012). Early Intervention for Children with Autism Spectrum Disorders: ‘Guidelines for Good Practice’. Retrieved September 29, 2017, from http://www.fahcsia.gov.au/sites/default/files/documents/11_2012/early_intervention_practice_guidlines.pdf.
Research Autism. (2017). Interventions, Treatments and Therapies for Autism. Retrieved September 29, 2017, from http://www.researchautism.net/interventions.
Ridge, K., & Guerin, S. (2011). Irish clinicians’ views of interventions for children with autistic spectrum disorders. Autism, 15(2), 239–252.
Roberts, J. M. A., Williams, K., Smith, K., & Campbell, L. (2016). Autism spectrum disorder: Evidence-based/evidence-informed good practice for supports provided to preschool children, their families and carers. National Disability Insurance Agency, Australia.
Russell, D. J., Rivard, L. M., Walter, S. D., Rosenbaum, P. L., Roxborough, L., Cameron, D., … Avery, L. M. (2010). Using knowledge brokers to facilitate the uptake of pediatric measurement tools into clinical practice: A before-after intervention study. Implementation Science, 5, 92.
Sackett, D., Rosenberg, W. C., Gray, J. A. M., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t: It’s about integrating individual clinical expertise and the best external evidence. British Medical Journal, 312, 71–72.
Sigafoos, J., & Schlosser, R. (2012). An experiential account of facilitated communication. Evidence-Based Communication Assessment and Intervention, 6(1), 1–2. https://doi.org/10.1080/17489539.2012.710992.
Stahmer, A. C., Collings, N. M., & Palinkas, L. A. (2005). Early intervention practices for children with autism: Descriptions from community providers. Focus on Autism and Other Developmental Disabilities, 20(2), 66–79. https://doi.org/10.1177/10883576050200020301.
Trembath, D., Paynter, J., Keen, D., & Ecker, U. K. H. (2015). “Attention: Myth Follows!” facilitated communication, parent and professional attitudes towards evidence-based practice, and the power of misinformation. Evidence-Based Communication Assessment and Intervention, 9(3), 113–126.
Trembath, D., & Vivanti, G. (2014). Problematic but predictive: Individual differences in children with autism spectrum disorders. International Journal of Speech-Language Pathology, 16(1), 57–60.
Vallino-Napoli, L. D., & Reilly, S. (2004). Evidence-based health care: A survey of speech pathology practice. Advances in Speech Language Pathology, 6(2), 107–112.
Wilkinson, S. A., Hinchliffe, F., Hough, J., & Chang, A. (2012). Baseline evidence-based practice use, knowledge, and attitudes of allied health professionals: A survey to inform staff training and organisational change. Journal of Allied Health, 41(4), 177–184.
Wong, C., Odom, S. L., Hume, K. A., Cox, A. W., Fettig, A., Kucharczyk, S., … Schultz, T. R. (2015). Evidence-based practices for children, youth, and young adults with autism spectrum disorder: A comprehensive review. Journal of Autism and Developmental Disorders, 45(7), 1951–1966.
Zipoli, R. P., & Kennedy, M. (2005). Evidence-based practice among speech-language pathologists: Attitudes, utilization, and barriers. American Journal of Speech-Language Pathology, 14(3), 208–220.
Acknowledgments
We thank the allied health professionals who participated in this research.
Funding
This study received funding from the School of Applied Psychology at Griffith University (Internal Seed Funding Grant). David Trembath is supported by a National Health and Medical Research Council ECR Fellowship (GNT1071881).
Author information
Authors and Affiliations
Contributions
JP conceived the study, co-ordinated the study, assisted with design and completion of statistical analyses, and drafted the manuscript. RS collected and analysed data and contributed to manuscript preparation. SL-S contributed to manuscript preparation and interpretation of findings. DT assisted with the design and co-ordination of the study, selection of analyses, and contributed to manuscript preparation. DK assisted with the design and co-ordination of the study, selection of analyses, and contributed to manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Paynter, J., Sulek, R., Luskin-Saxby, S. et al. Allied Health Professionals’ Knowledge and Use of ASD Intervention Practices. J Autism Dev Disord 48, 2335–2349 (2018). https://doi.org/10.1007/s10803-018-3505-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-018-3505-1