Abstract
The aim of our study was to evaluate the frequencies of myeloid dendritic cells (mDCs) and plasmacytoid dendritic cells (pDCs) in children with ASD. Subjects were 32 children with ASD and 30 healthy children as controls. The numbers of mDCs and pDCs and the expression of CD86 and CD80 on the entire DCs were detected by flow cytometry. ASD children had significantly higher percentages of mDCs and pDCs when compared to controls. We found significant inverse relationships between serum 25-hydroxyvitamin D levels and the frequencies of mDCs and pDCs in autistic children. Our data suggested that DCs could play a role in the clinical course of ASD. The relationship of DCs to immune disorders in ASD remains to be determined.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is a complex neurodevelopmental syndrome. It begins before 3 years of age. ASD is characterized by pervasive deficits in social interaction, impairment in verbal and nonverbal communication, and stereotyped patterns of interests and activities (Bjørklund et al. 2016; Wang et al. 2014). The pathogenesis of ASD is bewildering. The chemosensory immune system participates in neurodevelopment, regulating neuronal proliferation, synapse formation and plasticity, along with removing apoptotic neurons (Wang et al. 2014). Hundreds of studies over the last 4 decades have recognized altered immune responses in individuals with ASD. Drug, environmental and food allergies, asthma, seizures, unexplained skin rashes, and persistent intestinal yeast infections have been described (Gurney et al. 2006; Sakamoto et al. 2015; Schieve et al. 2011). Signs of immune tolerance loss e.g. allergies, over-reaction to vaccines/infections and undiagnosed autoimmune disorders are simply more common in individuals with ASD (Kern et al. 2014; Ruggeri et al. 2014).
Dendritic cells (DCs) are highly phagocytic for both microbes and damage-associated molecular pattern molecules of endogenous tissues (Breece et al. 2013; Steinman 2007). After binding of these antigens/ligands, DCs mobilize for migration, produce immune cell converting chemokines, and make co-stimulatory molecules to prime naïve T cells or stimulate effector T cells while secreting cytokines that control neighboring immune cells (Banchereau et al. 2000; Steinman 2007; Ueno et al. 2007). Moreover; DCs induce central and peripheral tolerance. DCs in the periphery continuously capture and present low dose non-immunogenic antigens to T cells with limited or absent co-stimulation to maintain tolerance either by deletion, the induction of unresponsiveness or generation of adaptive T regulatory cells (Steinman 2007). Myeloid dendritic cells frequency is increased in ASD (Breece et al. 2013). Both myeloid dendritic cells, and plasmacytoid dendritic cells, are impaired in ASD, where plasmacytoid phenotypes seem to be associated with developmental regression in ASD and an increase in the amygdala volume (Breece et al. 2013).
Since the data on the frequencies of DCs and their expression of CD86 and CD80 in children with ASD are generally very limited and entirely absent studies in Egypt, our aims were, first, to evaluate the frequencies of circulating myeloid dendritic cells (mDCs) and plasmacytoid dendritic cells (pDCs) and their expression of costimulatory molecules in children with ASD by flow cytometry in the largest tertiary care center in Upper Egypt. Second, to evaluate any associations between the frequencies of circulating DCs with clinical, behavioral and laboratory data for ASD children.
Patients and Methods
This study has been carried out in accordance with the code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. All procedures are approved by the Ethical Committee of Assiut University, Egypt. Participants were informed of the intervention composition, the safety profile, and the study requirements. An informed consent was taken from all the participants’ caregivers before the start of the study in accordance with Ethical Committee guidelines (Assiut University).
Study Design
This was a case-controlled study undertaken in Assiut University hospitals Assiut city, Egypt.
Participants
Subjects were 32 children with ASD selected from a sample of 50 autistic children. All study populations were in a good nutritional state. Eighteen children with ASD were excluded, ten patients did not meet the inclusion criteria and/or have one or more of the exclusion criteria (summarized in Table 1) and eight families declined to participate in the study. All patients were recruited from the neuropediatric clinics of Assiut University hospitals and two private centers for ASD in Assiut city, Upper Egypt. The study included 30 age and sex matched healthy children as a control group.
Methods
Initial Clinical and Psychiatric Assessment
The diagnosis of ASD was established by two senior child psychiatrists before participants were initiated into the study. The diagnosis of our patients was confirmed using the Diagnostic and Statistical Manual of Mental Disorders 5th edition (American Psychiatric Association 2013). Structured parent interviews of at least 2 h that probed for autistic manifestations, later on, another session was conducted to assess ASD symptom severity using the Childhood Autism Rating Scale (CARS; Schopler et al. 2010). CARS evaluates behavior in 14 domains that are affected by ASD, plus one parameter of general impression of autism. The examiner assigned a score of 1–4 for each domain: one indicates normal behavior appropriate for age (no signs of autism), while four indicates a severe deviance with respect to normal behavior (severe symptoms of autism). Single item scores are summed. The maximum CARS score is 60, while the cut off for autism is 30. A total score of 15–29.5 is considered non-autistic. Scores of 30.5–37 are rated as mild-moderate autistic, and 37. 5–60 as severely autistic (Geier et al. 2013; Schopler et al. 2010).
The Aberrant Behavior Checklist (ABC) was done for all ASD patients, as well. The ABC is a 58-item behavior rating scale used to measure behavior problems across five subscales (irritability, hyperactivity, social withdrawal, stereotypic behavior and inappropriate speech). Items are rated on a 4-point scale {ranging from zero (not at all a problem) to three (severe)}, with higher scores reflecting more severe problems (Aman et al. 1985).
A detailed history was taken from parents, including family history of consanguinity, similar conditions of ASD, social activities, self-care, and time of onset of autistic manifestations.
Laboratory Investigations
All patients and controls underwent laboratory tests which included complete blood picture (CBC) with differential count, blood urea nitrogen and serum creatinine. Serum level of 25-hydroxycholecalciferol (25 (OH)D) was estimated using the 25-OH Vit D ELISA Kit; Immundiagnostik AG, Germany.
Flow Cytometric Detection of DCs Frequencies and Phenotype
Dendritic cells in whole peripheral blood samples were enumerated using fluoroisothiocyanate (FITC)-conjugated monoclonal antibodies (MoAbs) against lineage markers (includes anti-CD3, anti-CD14, anti-CD19), phycoerythrin (PE)-conjugated anti-CD123, PE-conjugated anti-CD11c and peridinium-chlorophyll-protein (Per-CP)-conjugated anti-HLA-DR. All monoclonal antibodies were purchased from Becton Dickinson Biosciences, CA USA. To determine blood DCs numbers, 100 µl of blood sample was stained with 10 µl of FITC-conjugated lineage specific markers (CD3, CD14, and CD19), 10 µl of Per-CP-conjugated anti-HLA-DR, and 10 µl of PE-conjugated DCs markers (anti-CD11c or anti-CD123). The expression of co-stimulatory molecules, CD86 and CD80 on DCs was analyzed in whole blood samples in parallel with DCs frequency, 100 µl of blood sample was stained with 10 µl of FITC-conjugated lineage specific markers (CD3, CD14 and CD19), 10 µl of Per-CP-conjugated anti-HLA-DR, and 10 µl PE-conjugated CD86 or CD80. The tubes were incubated for 15 min at room temperature in the dark. RBC lysis was done. After one wash, the cells were resuspended in phosphate buffer saline (PBS), and analyzed by FACSCalibur flow cytometry with CellQuest software (Becton Dickinson Biosciences, CA, USA). Fifteen thousand events were analyzed, and an isotype-matched negative control was used with each sample. The numbers of CD11c+ (mDCs) and CD123+ (pDCs) and the expression of CD86 and CD80 on the entire DCs population (HLA-DR+ lineage specific− events) were detected by flow cytometry as shown in Fig. 1. The frequencies of mDCs and pDCs were recorded as percentages of total monocytes and lymphocytes populations. CD86 and CD80 levels were recorded as a percentage of expression and as a geometric mean of fluorescence intensity (MFI).
Flow cytometric detection of dendritic cells in ASD children. A Forward and side scatter histogram was used to define the lymphocyte and monocytes population (R1). B R2 gate containing entire dendritic cells (HLA-DR+ lineage specific− populations) within the lymphocytes and monocytes population was selected, compared with the negative isotype control (not shown). Then, the percentage of mDCs (HLA-DR+ lineage specific− CD11c+) (R3) and the pDCs (HLA-DR+ lineage specific−CD123+) (R4) were determined (C, D). E, F Show the geometric mean of fluorescence intensity (MFI) of expression of CD86 and CD80 on the entire DC population. The positivity was defined as fluorescence (red histogram) higher than that of the isotype control (open histogram). (Color figure online)
Statistical Analysis
Data analysis was done by statistical package for social sciences (SPSS), version 16. All data were expressed as the mean ± standard error of mean (SEM). differences between the groups were examined for statistical significance using the Mann–Whitney U test. A p value of ≤0.05 denoted the presence of a statistically significant difference. The Spearman correlation coefficient was used to examine the correlation among different studied parameters.
Results
Patients’ characteristics, including age, sex, age at diagnosis, ABC scores and CARS classification of ASD are shown in Table 2. Subjects were 2.5–5 years old [mean age 2.9 years (SD 1.3)]. The study included 22 males (68.75%) with male to female ratio 2.2:1. The control group included 20 males (66.7%) and 10 females (33.3%) with age ranged from 3 to 6 years with mean age 3.1 years (SD 1.8). There were no significant differences in mean age and sex distributions between ASD patients and controls. Twenty ASD children (62.5%) were diagnosed before the age of 3 years, while twelve patients (37.5%) were diagnosed after 3 years of age. The baseline CARS scores ranged from 30 to 52.5 [mean 35.9 (SD 7.2)]. 43.75% of our patients had severe autism while 56.25% had mild/moderate autism. The mean ABC scores and SD for the patients group were: irritability (24.7 ± 4.5), hyperactivity (25.8 ± 12.1), lethargy/social withdrawal (19.3 ± 5.5), inappropriate speech (6.1 ± 1.9) and stereotypic behavior (6.4 ± 3.1) (Table 2).
Table 3 shows some laboratory parameters in ASD patients and controls. There were no statistically significant differences in platelet and white blood cell counts in the peripheral blood between ASD group and the controls. The mean hemoglobin levels, blood urea nitrogen and serum creatinine were comparable between patients and healthy children. Serum 25-OHD levels were significantly lower in ASD children compared to controls (mean ± SEM; 22.3 ± 11.8 vs. 40.1 ± 14.8; p < 0.001).
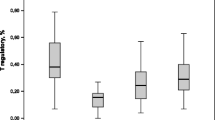
Table 4 shows the frequencies of DCs and their expression of costimulatory molecules CD86 and CD80 in patients with ASD and healthy controls. After controlling for age and sex, ASD children had significantly higher percentages of myeloid dendritic cells (mDCs) when compared to controls (mean% ± SEM; 2.44% ± 0.20 versus 1.54% ± 0.09; p = 0.006). The frequencies of plasmacytoid dendritic cell (pDCs) populations were statistically significantly higher in patients with ASD as compared to controls (mean% ± SEM; 1.98% ± 0.35 versus 1.18% ± 0.05; p = 0.036) (Table 4). The expression of costimulatory molecules CD86 on the entire DCs showed a significant upregulation in patients with ASD compared with healthy individuals (mean% ± SEM; 49.67% ± 4.67 versus 23.16% ± 1.39; p = 0.001). Moreover, the expression of costimulatory molecules, CD80 on the entire DCs showed similar results with significantly higher expression in ASD children compared to controls (mean% ± SEM; 55.37% ± 2.94 versus 39.42% ± 4.7; p = 0.001) (Table 4). The mean fluorescent intensity (MFI) of CD86 expression on the entire DCs was significantly higher in ASD children compared to controls (mean ± SEM; 149.36 ± 9.52 vs. 111.26 ± 8.26; p = 0.003). Similar result was noted in MFI of CD80 expression on the entire DCs (mean ± SEM; 76.07 ± 3.18 vs. 52.05 ± 3.59; p = 0.001) (Table 4).
The frequencies of mDCs had significant positive correlations with the severity of ASD (r = 0.51; p ˂ 0.01), CARS scores of emotional response (r = 0.48; p˂0.01) and social-emotional understanding (r = 0.82; p ˂ 0.001). In addition, the frequencies of mDCs had significant positive correlations with ABC parameters; hyperactivity (r = 0.48; p ˂ 0.05) and stereotypic behavior (r = 0.48; p ˂ 0.05). Plasmacytoid DCs populations had a significant positive correlation with severity of ASD (r = 0.49; p = 0.05). There were no significant correlations between the frequencies of pDCs or costimulatory molecules, CD86 and CD80 with CARS and ABC subscales. Interestingly, there were significant negative relationships between serum 25-OHD levels and the frequencies of both mDCs (r = −0.67; p = 0.001) and pDCs populations (r = −0.7; p ˂ 0.001). There were no significant correlations between mDCs and pDCs percentages and patients age, sex and age at onset of autistic manifestations.
Discussion
We determined the frequency of DCs and their expression of costimulatory molecules CD86 and CD80 in patients with ASD and healthy controls. Our study showed mDCs were significantly increased in children with ASD compared with healthy controls. This is in agreement with Breece et al. 2013; who reported the frequency of the myeloid DC population (mDC1) was significantly higher in autistic children (4.6%) compared with normal children (3.7%, p = 0.03). This represented about 25% increase in mDC1 in children with ASD. Furthermore, the frequency of mDC2 myeloid DCs was increased, by approximately 40% in children with ASD (3.49%) compared with healthy controls (Breece et al. 2013). In our work, the percentage of pDCs populations were significantly higher in patients with ASD as compared to controls. However, our findings are contradictory to the previous study (Breece et al. 2013), which reported that there was no difference in the frequency of pDCs populations between ASD patients and controls. For the first time, the analysis of data herein showed a significant upregulation in the expression of costimulatory molecules CD80 and CD86 on the entire DCs in patients with ASD compared with healthy children. Moreover, the mean fluorescent intensity of CD86+ and CD80+ on the entire DCs were significantly higher in ASD group compared to controls.
The immune system and CNS are in continuous communication, with each applying some regulation over the other. Some neuropeptides produced by neurons act as chemo-attractants and recruit immune cells such as DCs down a chemical gradient to the source of the neuropeptide (Mead and Ashwood 2015). DCs have a key role in many immune functions (Steinman 2007). They are highly phagocytic and express many innate pattern-recognition receptors that capture pathogen-associated molecular pattern molecules on microbes or damage-associated molecular pattern molecules of endogenous tissues. Upon binding of these ligands/antigens, DCs undertake maturing stages that increase migration, express chemokine receptors for homing to lymphoid organs, produce chemokines to recruit other immune cells, upregulate MHC class II molecules and co-stimulatory molecules for priming of naïve T cells or stimulation of effector T cells and secrete large quantities of cytokines that polarize or modulate immune cells (Steinman 2007; Ueno et al. 2007).
The biology of DCs links innate and adaptive immune responses (Breece et al. 2013) and induce central and peripheral tolerance. DCs in the periphery continuously capture and present low dose non-immunogenic antigens to T cells with limited or absent co-stimulation to maintain tolerance either by deletion, induction of unresponsiveness (anergy) or generation of adaptive T regulatory cells (Careaga and Ashwood 2012; Steinman 2007).
Given the role of the innate immune system in both proper neuronal development and function, it is of great interest that many studies have confirmed abnormalities in innate immune function in ASD patients (Careaga and Ashwood 2012). Significant alterations in the function of cells of the myeloid lineage, namely monocytes and macrophages, have been directly and indirectly reported in a number of studies in children with ASD (Careaga and Ashwood 2012). Monocytes and macrophages share many similarities to their CNS localized counterparts, the microglia, and may even contribute to the microglial population (Wilson et al. 2010). Prominent microglia cell activation and infiltration of monocytes and macrophages is observed in brain specimens of individuals with ASD (Voineagu et al. 2011).
Breece et al. 2013 found a significant positive association between mDC1 frequencies and measures of left amygdala volume (p = 0.004) and right amygdala volume (p = 0.02), in children with ASD after adjusting for age and sex, and using overall brain volume as a covariate. Moreover, they reported a significant positive association between mDC2 cells and right amygdala volume (p = 0.05). The frequencies of pDC1 plasmacytoid dendritic cells were also positively associated with left (p = 0.02) and right amygdala volumes (p = 0.03). In healthy controls, mDC1 frequencies were associated with left amygdala volume (p = 0.02) and right amygdala volume (p = 0.003); however, no associations were observed between mDC2, pDC1 or pDC2 frequencies and amygdala volumes in controls (Breece et al. 2013).
The results of our work revealed significantly positive correlations between mDCs and pDCs with the severity of ASD classified by CARS. Our study is the first to report a positive association between DCs populations and classifications of autism.
Regarding ASD core manifestations, there were significantly positive correlations between mDCs with emotional response, social-emotional understanding, hyperactivity and stereotypic behavior. In line with our findings, a previous report (Breece et al. 2013) documented significant positive associations between elevated frequencies of DCs with the severity of gastrointestinal symptoms and increased repetitive behaviors in ASD children. Taken together these data suggest that genetic mechanisms in ASD may impact important controlling processes relevant to innate immune function including the function of DCs that may be important in neuronal and mucosal development.
Remarkably, we found significant inverse relationships between serum 25-OHD levels and the frequencies of mDCs and pDCs populations in children with ASD. Vitamin D has an important role in brain homeostasis, neurodevelopment, ageing, and significantly, in gene regulation. Also, it has been shown to bind to more than 2700 genes and to regulate the expression of more than 200 of them (Cannell and Grant 2013; Eyles et al. 2013; Bjørklund et al. 2016; Saad et al. 2016a). Many researchers suggested that vitamin D has a key role as a neuroactive steroid, which can affect neuronal differentiation, axonal connectivity and brain structure and function. Furthermore, vitamin D deficiency during pregnancy is linked with several adverse effects in the fetus, e.g. intrauterine growth restriction (Eyles et al. 2013; Bjørklund et al. 2016). Growing data have shown an association between the risk for ASD and vitamin D insufficiency in patients with ASD. Our previous data (Saad et al. 2016a) showed 57% (70/122) of children with ASD had vitamin D deficiency, and 30% (36/122) had vitamin D insufficiency. We found a significant negative relationship between serum 25(OH)D levels and severity of autism (Saad et al. 2016a). Vitamin D has been reported as a chief modulator of the immune system, playing an important role in the regulation of both innate and adaptive immune responses (Ferreira et al. 2015; Saad et al. 2016b), While affecting the immune system at multiple levels, the main target of vitamin D in immune population is the DCs. In DCs, vitamin D can generate in vitro a stable maturation-resistant tolerogenic phenotype, with low expression of HLA-DR, low expression of costimulatory molecules and increased interleukin 10 (IL-10)/IL-12p70 ratios that are maintained even after removal of the compound (van Halteren et al. 2002). Significantly, introduction of an antigen in parallel with vitamin D can induce antigen-specific tolerogenic DCs with the ability to induce infectious tolerance, changing the behavior of other proinflammatory mature DCs through the induction of antigen-specific regulatory T cells, and causing the perpetuation of the tolerogenic response. In addition, 1,25(OH)2D3-conditioned fully differentiated DCs lose their ability to activate autoreactive T cells, stimulating instead the generation of regulatory T cells, Tregs (Ferreira et al. 2014, 2015; van Halteren et al. 2002). Reintroduction of such 1,25D3-DCs in vivo leads to immune modulation (Ferreira et al. 2014), which represents a reliable strategy for the promotion or restoration of antigen-specific tolerance through vaccination strategies. Although the immunomodulatory properties of vitamin D on DC phenotype and function are well outlined, the intracellular and molecular mechanisms leading to these effects strongly suggest olfaction (Ferreira et al. 2015).
Conclusion
Many systemic and cellular immune abnormalities have been found in individuals with ASD. Our study shows significant higher frequencies of circulating mDCs and pDCs populations in autistic children. These increased frequencies were associated with significantly positive correlations with the severity of ASD and some of the behavioral core manifestations of ASD. We found significant inverse relationships between serum 25-OHD levels and the frequencies of mDCs and pDCs populations in children with ASD. Our data suggested that DCs could play a role in the clinical course of ASD. The relationship of DCs to immune disorders in ASD children remains to be determined. Further longitudinal study with a larger sample size is warranted to explore the mechanisms and functions of DCs in ASD patients.
Abbreviations
- 25 (OH)D:
-
25-hydroxycholecalciferol
- ABC:
-
Aberrant behavior checklist
- ASD:
-
Autism spectrum disorder
- CARS:
-
Childhood autism rating scale
- DCs:
-
Dendritic cells
- mDCs:
-
Myeloid dendritic cells
- pDCs:
-
Plasmacytoid dendritic cells
References
Aman, M. G., Singh, N. N., Stewart, A. W., & Field, C. J. (1985). The aberrant behavior checklist: A behavior rating scale for the assessment of treatment effects. American Journal of Mental Deficiency, 89(5), 485–491.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders 5. Washington, DC: American Psychiatric Association.
Banchereau, J., Briere, F., & Caux, C. (2000). Immunobiology of dendritic cells. Annual Review of Immunology, 18, 767–811.
Bjørklund, G., Saad, K., Chirumbolo, S., Kern, J. K., Geier, D. A., Geier M. R. et al. (2016). Immune dysfunction and neuroinflammation in autism spectrum disorder. Acta Neurobiologiae Experimentalis (Wars), 76(4), 257–268.
Breece, E., Paciotti, B., Nordahl, C. W., Ozonoff, S., Van de Water, J. A., Rogers, S. J., et al. (2013). Myeloid dendritic cells frequencies are increased in children with autism spectrum disorder and associated with amygdala volume and repetitive behaviors. Brain, Behavior, and Immunity, 31, 69–75.
Cannell, J. J., & Grant, W. B. (2013). What is the role of vitamin D in autism? Dermatoendocrinology, 5(1), 199–204.
Careaga M, Ashwood P. Autism spectrum disorders: From immunity to behavior. In: Yan Q (ed) Psychoneuroimmunology methods and protocols. New York: Humana Press, pp 219–240.
Eyles, D. W., Burne, T. H., McGrath, J. J., & Vitamin, D. (2013). effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Frontiers in Neuroendocrinology, 34, 47–64.
Ferreira, G. B., Gysemans, C. A., Demengeot, J., da Cunha, J. P., Vanherwegen, A. S., Overbergh, L., et al. (2014). 1,25-Dihydroxyvitamin D3 promotes tolerogenic dendritic cells with functional migratory properties in NOD mice. Journal of immunology (Baltimore, Md.: 1950), 1, 192.
Ferreira, G. B., Vanherwegen, A. S., Eelen, G., Gutiérrez, A. C., Van Lommel, L., Marchal, K., et al. (2015). Vitamin D3 induces tolerance in human dendritic cells by activation of intracellular metabolic pathways. Cell Reports, S2211–1247(15), 711–725.
Geier, D. A., Kern, J. K., & Geier, M. R. (2013). A comparison of the autism treatment evaluation checklist (ATEC) and the childhood autism rating scale (CARS) for the quantitative evaluation of autism. Journal of Mental Health Research in Intellectual Disabilities, 6(4), 255–267.
Gurney, J. G., McPheeters, M. L., & Davis, M. M. (2006). Parental report of health conditions and health care use among children with and without autism: National Survey of Children’s Health. Archives of Pediatrics and Adolescent Medicine, 160, 825–830.
Kern, J. K., Geier, D. A., Sykes, L. K., Homme, K. G., & Geier, M. R. (2014). Medical conditions in autism and events associated with initial onset of autism. OA. Autism: The International Journal of Research and Practice, 2(1), 9.
Mead, J., & Ashwood, P. (2015). Evidence supporting an altered immune response in ASD. Immunology Letters, 163(1), 49–55.
Ruggeri, B., Sarkans, U., Schumann, G., & Persico, A. M. (2014). Biomarkers in autism spectrum disorder: the old and the new. Psychopharmacology, 231(6), 1201–1216.
Saad K, Abdel-Rahman AA, Elserogy YM, Al-Atram AA, Cannell JJ, Bjørklund G et al. (2016a) Vitamin D status in autism spectrum disorders and the efficacy of vitamin D supplementation in autistic children. Nutrition Neuroscience, 19(8):346–351.
Saad K, Abdel-rahman AA, Elserogy Y, Al-Atram AA, El-Houfey AA, Othman HA et al. (2016b). Randomized-controlled trial of vitamin d supplementation in children with autism spectrum disorder. Journal of Child Psychology and Psychiatry. doi:10.1111/jcpp.12652.
Sakamoto, A., Moriuchi, H., Matsuzaki, J., Motoyama, K., & Moriuchi, M. (2015). Retrospective diagnosis of congenital cytomegalovirus infection in children with autism spectrum disorder but no other major neurologic deficit. Brain and Development, 37, 200–205.
Schieve, L. A., Gonzalez, V., Boulet, S. L., Visser, S. N., Rice, C. E., Van Naarden Braun K, & Boyle, C. A. (2011). Concurrent medical conditions and health care use and needs among children with learning and behavioral developmental disabilities, National Health Interview Survey, 2006–2010. Research in Developmental Disabilities, 33, 467–476.
Schopler E, Van Bourgondien M E, Wellman GJ. (2010) Childhood autism rating scale. 2nd. CARS-2. Los Angeles, CA: Western Psychological Services.
Steinman, R. M., Lasker Basic Medical Research Award (2007). Dendritic cells: versatile controllers of the immune system. Natural Medicines, 13(10), 1155–1159.
Ueno, H., Klechevsky, E., Morita, R., Aspord, C., Cao, T., Matsui, T., et al. (2007). Dendritic cell subsets in health and disease. Immunological Reviews, 219, 118–142.
van Halteren, A. G., van Etten, E., de Jong, E. C., Bouillon, R., Roep, B. O., & Mathieu, C. (2002). Redirection of human autoreactive T-cells Upon interaction with dendritic cells modulated by TX527, an analog of 1,25 dihydroxyvitamin D (3). Diabetes, 51(7), 2119–2125.
Voineagu, I., Wang, X., Johnston, P., Lowe, J. K., Tian, Y., Horvath, S., et al. (2011). Transcriptomic analysis of autistic brain reveals convergent molecular pathology. Nature, 474, 380–384.
Wang, T. T., DU, L., Shan, L., & Jia, F. Y. (2014). Research advances in immunological dysfunction in children with autism spectrum disorders. Zhongguo Dang Dai Er Ke Za Zhi, 16(12), 1289–1293.
Wilson, E. H., Weninger, W., & Hunter, C. A. (2010). Trafficking of immune cells in the central nervous system. The Journal of Clinical Investigation, 120, 1368–1379.
Acknowledgments
The authors would like to extend their sincere appreciation to the Deanship of Scientific Research at king Saud University for its funding this Research group No. (RG-1435-019).
Author Contributions
KE, KS, AAA, MH, AA and YE designed the study, followed the patients, analyzed the data, and drafted the manuscript. AZ performed all laboratory investigations in the study. All authors were involved in the critical analysis of the final version of the manuscript. All authors approved the manuscript as submitted and agree to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors do not have potential conflict of interest.
Rights and permissions
About this article
Cite this article
Saad, K., Zahran, A.M., Elsayh, K.I. et al. Frequency of Dendritic Cells and Their Expression of Costimulatory Molecules in Children with Autism Spectrum Disorders. J Autism Dev Disord 47, 2671–2678 (2017). https://doi.org/10.1007/s10803-017-3190-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-017-3190-5