Abstract
Impairments in social interaction and communication are critical features of ASD but the underlying processes are poorly understood. An under-explored area is the social motor synchronization that happens when we coordinate our bodies with others. Here, we explored the relationships between dynamical measures of social motor synchronization and assessments of ASD traits. We found (a) spontaneous social motor synchronization was associated with responding to joint attention, cooperation, and theory of mind while intentional social motor synchronization was associated with initiating joint attention and theory of mind; and (b) social motor synchronization was associated with ASD severity but not fully explained by motor problems. Findings suggest that objective measures of social motor synchronization may provide insights into understanding ASD traits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impairments in social interaction and communication are critical features of autism spectrum disorder (ASD). These impairments negatively affect typical social-cognitive development in multiple settings and are associated with poor clinical outcomes (American Psychiatric Association 2013; Howlin et al. 2004). One noteworthy characteristic of most social interactions is the coordination that occurs in turn-taking and jointly created actions. For example, neonates have been found to coordinate their body movements to human speech almost immediately after birth (Condon and Sander 1974a, b), 4- and 9-month-olds coordinate their gaze and vocalizations based on when mothers start or stop talking (Feldstein et al. 1993; Jasnow and Feldstein 1986), the footsteps of two people walking together often become synchronized (Zivotofsky and Hausdorff 2007), and bodily activity is synchronized during conversation (Schmidt et al. 2014). Such interpersonal synchronization remains an overlooked dimension of non-facial social communication in ASD research.
In its broadest sense, interpersonal synchronization refers to a variety of social communication activities and constructs such as joint attention, imitation, turn-taking, non-verbal social communicative exchanges, affect sharing and engagement (Charman 2011) and involves synchronization in both time and content (Delaherche et al. 2012; Kinsbourne and Helt 2011). Importantly, interpersonal synchronization can arise either intentionally when there is an explicit social goal or spontaneously without conscious awareness when there is not an explicit goal. Social motor synchronization is a specific sub-type of interpersonal synchrony that focuses exclusively on non-verbal social communicative exchanges that involves the synchronization of the bodies of two people engaged in a social interaction.
Interpersonal synchrony has been found to play important roles in social development. For example, the type of interactional synchrony Condon and Sander (1974a, b) found in mother–infant interactions has been proposed to be important not only for language learning but also for the development of social relations and intersubjectivity. More recent researchers (Feldman 2007; Jaffe et al. 2001; Trevarthen and Delafield-Butt 2013) have argued that movement abnormalities may have numerous consequences for cognitive and emotional development. Other research has shown that bodily coordination influences infant and toddler’s social perceptions. For example, although 9-month old infants had not yet developed the social preference for synchronously moving objects, by 12-months infants demonstrate a preference for social stimuli that moved synchronously with them (Tunçgenç et al. 2015). Toddlers have been found to prefer to play with or help adults who have mimicked their actions (Carpenter et al. 2013; Fawcett and Liszkowski 2012). In adults, research has shown that synchronizing one’s body with another person results in increases in interpersonal responsiveness, social rapport and other-directedness (Bernieri et al. 1994; Lakin and Chartrand 2003), positive self-other relations (Miles et al. 2009; Seger and Smith 2009), cooperation (Reddish et al. 2014, 2013; Valdesolo et al. 2010; Wiltermuth and Heath 2009), and verbal communication and comprehension (Semin 2007; Shockley et al. 2009).
Conversely, research also suggests interpersonal synchrony breaks down in social pathology. For example, lower levels of synchronization are associated with marital dissatisfaction (Julien et al. 2000), as well as psychological disorders such as schizophrenia (Varlet et al. 2012; Ramseyer and Tschachter 2011) and borderline personality disorder (Gratier and Apter-Danon 2009). Synchronization of speech and gesture is also disrupted in ASD (de Marchena and Eigsti 2010), as is the timing of facial mimicry (Oberman et al. 2009). In addition, Landa et al. (2011) found that an interpersonal synchrony intervention that created many opportunities for practicing initiating and responding to joint attention and sharing positive affect resulted in improvements in imitation but not joint attention or shared positive affect.
Some preliminary evidence also indicates that individuals with ASD may have social motor synchronization difficulties. For example, Fitzpatrick et al. (2013) and Fitzpatrick et al. (under review) found that school-age children with ASD had lower social motor synchronization abilities than controls, and Marsh et al. (2013) found that preschoolers with ASD were less able to exhibit spontaneous social rocking than controls. Similarly, Fitzpatrick et al. (2016) found that adolescents with ASD performed worse on social motor synchronization tasks than controls.
Given the importance of social bodily coordination, one might argue that the ability to successfully engage in social motor synchronization is important for understanding the processes underlying the social deficits evident in ASD. An early dysfunction in the ability for social motor synchronization could lead to difficulties in building social and emotional bonds with caregivers, learning language, understanding and responding to social cues, and developing joint attention. Joint attention is a set of behaviors that allow for a person to gain, follow, and share in the attention of another person. Typically, joint attention begins to develop around 9 months of age and continues developing into the child’s second year of life (Mundy 2009; Mundy and Newell 2007; Tomasello 1999). In addition, joint attention has been correlated with individual differences in the development of social competence later in life (Vaughan Van Hecke et al. 2007). One theory of autism proposes that impaired development of joint attention is a critical feature of the disorder (e.g., Mundy et al. 1990) and deficiencies in joint attention hinder the development of social skills and language ability. In contrast, Leekam et al. (1997) have suggested that poor joint attention skills may be due to difficulties making self-generated, spontaneous responses rather than a lack of joint attention skill. As a consequence, they have attributed joint attention problems to a lack of social motivation.
However, perhaps a disruption in social motor synchronization ability during the neonatal period is a critical deficit, disrupting the development of joint attention during the second half of infancy. Tunçgenç et al. (2015) have found that synchrony begins to guide social preferences at around 12 months. A neonatal deficit in social motor synchronization might disrupt the development of this ability. This early social motor synchronization deficit could, in turn, have cascading consequences for difficulties in developing other social cognitive functions, like theory of mind (ToM) and cooperation. Theory of mind is defined as the ability to understand the thoughts and beliefs of others and develops between the second and fourth year of life. Whereas verbal theory of mind tasks suggest that theory of mind develops after 4-years-of age (e.g., Wellman et al. 2001), non-verbal theory of mind tasks and tasks that demonstrate emulation of unfulfilled goals suggest that theory of mind begins to emerge much earlier (Carpenter et al. 2001, 2002; Meltzoff 1995; Onishi and Baillargeon 2005; Woodward 1998). Warneken et al. (2006) also suggest that ToM emerges before 4-years as their research found that typically developing children between 18 and 24 months successfully completed complex cooperation tasks that require understanding the goal of another, sharing the goal, and coordinating actions.
One prominent theory of autism proposes that a defining feature of ASD is a deficit in theory of mind skills (Baron-Cohen et al. 1985; Happé 1993). According to this theory, an inability to understand the perspectives and emotions of other people underlies the social interaction problems evident in autism (Peterson and Siegal 2000). Some researchers are exploring whether performance on ToM tasks may be a consequence of other processes, such as neuromotor impairments (Dowd et al. 2010; Gernsbacher et al. 2008). In contrast, there is growing evidence questioning whether there is a lack of ToM since contextual factors related to ToM tasks affect performance and many children with ASD perform as well if not better than their typically-developing counterparts. Alternatively, the finding that children with ASD had poorer social competence on complex cooperation tasks (Colombi et al. 2009; Liebal et al. 2008) raises questions about whether the nature of the ToM deficits are a result of an inability to share goals or coordinate complex action sequences. Again, however, one could argue that specific impairments in social motor synchrony could also be an underlying mechanism influencing the development of ToM.
A social motor synchrony model of autism might also provide a framework for understanding the incredible heterogeneity evident in the disorder. If the mechanisms responsible for basic social motor synchronization become damaged at different points in development that would have different consequences for the types of behavioral disruptions that would ensue. For example, an infant born with a dysfunction in social motor synchronization would be expected to have more profound problems—the inability to develop language, joint attention, and theory of mind. In contrast, if the mechanisms underlying social motor synchronization become damaged after the age of two, the behavioral symptomology could be very different—the child could have started to develop language, joint attention, and theory of mind.
However, other researchers have argued that the critical deficit in ASD may lie in a general attention processing impairment that leads to disruptions in social interactions of those with ASD (Hayes 1987; O’Riordan et al. 2001). For example, the “sticky attention” hypothesis claims that individuals with autism have trouble switching their attention from objects because their attention gets “stuck” on the objects (Landry and Bryson 2004). Other research contends that the fundamental problem lies with an inability of social stimuli to capture attention (Chawarska et al. 2010). The claim is that the problem is a fundamentally social one, rather than a problem with attention (e.g., Fischer et al. 2014; Klin et al. 2003; Schultz 2005). Certainly, attention would appear to play a role in social motor synchrony. The ability to attend to the rhythms of another person is important for being able to produce the rhythm oneself and combine sensory information and motor production (Phillips-Silver et al. 2010). In fact, spontaneous synchronization with both social and non-social rhythmic stimuli appears to be determined by the amount of information picked up and attended to by a person (Varlet et al. 2015).
Given the importance of social motor synchrony for developing, initiating, and maintaining social connections, understanding its relationship to ASD traits is well warranted. The research reported here is designed to explore how social motor synchronization is related to ASD traits. We are extending the work of (a) Fitzpatrick et al. (2013) preliminary findings that children with ASD had difficulty performing social motor synchronizing tasks and (b) Fitzpatrick et al. (under review) who found that social motor synchronization differentiated children with and without ASD such that children with ASD exhibited weaker and less stable patterns of social motor synchronization that were not fully explained by poor motor skill. Rather than examining group differences, our focus is on evaluating social synchronization relationships across the full range of social and communicative abilities. This is important because ASD is considered to be a spectrum disorder due to the wide variation in the way it affects individuals, with the level of disability and the combination of problems varying greatly from individual to individual. In addition, given the work of Baron-Cohen et al. (2001), we know that autistic traits can be found in typically developing populations.
Our approach involves relying on the tools of behavioral dynamics, which provides researchers with methodologies and techniques that enable a fine-grained analysis of an individual’s movements as they unfold in time. These techniques result in dynamical measures that can be used to identify the patterning and strength of coordinative processes. In addition, the degree to which the movement variability (i.e., statistical noise) inherent in a coordinative process is stochastic or deterministic (i.e., random versus that produced by chaotic dynamics) can also be determined (Richardson et al. 2007, 2008a, b, 2014; Thiel et al. 2002). Such innovative techniques provide a new way to understand the complex, interactive and time-dependent emergent nature of social interactions.
Here, we explored the relationships between dynamical measures of social motor synchronization and motor control ability (reported in Fitzpatrick et al., under review) and clinical and social cognitive assessments of autistic traits. We implemented the multi-method research methodology piloted by Fitzpatrick et al. (2013) with a larger and more diverse sample and added clinical assessments to the experimental protocol.
Method
Participants
A total of 103 children, 50 with a diagnosis of ASD and 53 controls, participated. Five of the children in the ASD group were classified as non-spectrum and were eliminated from the analysis, resulting in a final sample of 98 children (mean age of ASD group 103.8 months, range 72–129 months; mean age of controls 99.70 months, range 75–131). There were 76 white, 14 African-American, 6 multi-racial, and 2 Asian participants. The gender, ethnicity, and age distributions of the participants are found in Table 1.
All parents of participants gave informed, written consent for their children to take part in the study, and releases were also obtained for the video recordings. A waiver of written assent was granted for this study because many of the children were too young to fully understand the assent process. Participants received a $100 gift certificate for participating in the study. The project was approved by the Cincinnati Children’s Hospital Medical Center’s (CCHMC) Institutional Review Board and participants were recruited from CCHMC and local communities through print advertising, a recruitment brochure, email, social media, and community events.
Male and female participants were eligible for the study if they were between the ages of 6 years, 0 months and 10 years, 11 months and had previously been diagnosed with ASD or were typically developing children with no developmental disorders or clinical diagnoses (non-ASD). They had to be able to speak in at least short phrases to ensure they understand task demands. All participants had a nonverbal mental age of at least 24 months. Nonverbal mental age was calculated from the age equivalent scores of the Differential Abilities Scales, 2nd Edition (DAS-II, calculations explained below). Males and females of all races/ethnicities were eligible for participation.
The tasks in this study required the ability to use words to communicate and complete simple motor tasks for 5–10 min while seated at a table. The following exclusion criteria were applied to ensure standardized testing procedures. Children who could not complete simple motor tasks due to limited language abilities, deafness, blindness, serious motor impairment (e.g., severe cerebral palsy), or nonverbal mental age below 24 months were excluded. Participants were also excluded if they are unable to walk independently, or if they had any other medical condition that precluded the valid administration of the study measures. Information regarding disorders and medical conditions was obtained during the parent pre-screening interview. Children who had a genetic disorder (e.g. Fragile X, Down syndrome) were excluded. Children with non-ASD developmental disorders (e.g., intellectual disability, receptive–expressive language disorder) or clinical diagnoses (e.g., Attention Deficit Hyperactivity Disorder, anxiety, learning disorder) were excluded from the study. Children whose caregivers were not familiar with their early developmental history (e.g., foster children) were excluded because the study measures rely on the caregiver to report about both the child’s current and past behaviors and symptoms. Participants for whom English was not a primary spoken language were also excluded.
The participants with ASD had previously been diagnosed by a licensed clinical psychologist or medical doctor based on DSM-IV_TR criteria (American Psychiatric Association 2000) and diagnosis was confirmed using the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2, Lord et al. 2012). The ADOS-2 is a semi-structured, standardized assessment of communication, social interaction, and play for individuals who have been referred because of possible autism. Five participants were administered Module 2 and 40 were administered Module 3. The mean ADOS social affect (SA), restricted and repetitive behavior (RRB) and comparison scores for the ASD group are reported in Table 2. There were technical difficulties with two participants (one from each diagnostic group) and the video recording of the session could not be used for data coding of the social cognitive measures.
Clinical Phenotyping
The Clinical Evaluation of Language Fundamentals-4 (CELF 4) and Differential Abilities Scales, 2nd Edition (DAS-II) were administered at the first visit. The CELF-4 (Semel et al. 2003) is a standardized language assessment appropriate for individuals 5 through 21 years of age. The concepts and following directions subscale (C & FD) was chosen to verify the child’s ability to understand directions during the experimental protocol and the formulated sentences subscale (FS) was administered to assess the child’s ability to communicate with sentences. The DAS-II (Elliot 2007) was used as a measure of cognitive ability. The School Age form was used for 74 participants. The Early Years form was used for 24 participants (21 were 6-years old and 3 failed to receive the minimum score on a subtest of the DAS-II School Age). The general conceptual ability score (GCA) measured verbal ability and the special nonverbal composite score (SNC) measured nonverbal ability. Nonverbal mental age was calculated from the DAS age equivalent scores. For the Early Years form, the average of the age equivalent scores (in months) that make up the Special Nonverbal Composite (SNC, Copying, Pattern Construction, Picture Similarities, and Matrices) was calculated. For the School-age form, the average of the age equivalent scores (in months) that make up the Special Nonverbal Composite (SNC, Matrices, Sequential & Quantitative Reasoning, Recall of Designs, & Pattern Construction) was calculated.
In addition, a parent completed the Social Responsiveness Scale (SRS) and Achenbach Child Behavior Checklist (CBCL) at the first visit. The SRS (Constantino and Gruber 2005) is a rating scale that measures the severity of autism spectrum symptoms as they occur in natural social settings. The CBCL (Achenbach and Rescorla 2001) provides a measure of behavioral and emotional problems. The attention problems, social problems, and ADHD subscales were used in data analysis because these are common co-occurring problems in ASD.
Social Cognitive Behavioral Tasks
The social cognitive coordination between the child and the experimenter was measured with tasks that have been used successfully in children with and without ASD, ranging in age from 5 to 17 years. All of the tasks were video-recorded using a Microsoft Kinect camera. The camera was placed at a height of 1.5, 3 m away from corner of the table-top closest to the participant and experimenter at approximately a 45-degree angle. A custom software application (http://www.xkiwilabs.com) using the free Windows Kinect SDK version 1.5 (Microsoft LTD) was used to record the video images at an approximate image rate of 30 Hz. The videos were coded by two research assistants who were blind to the diagnosis group of the participants.
Joint Attention Tasks
Responding to Joint Attention (RJA) was assessed by using the gaze-monitoring task (Leekam et al. 1997; Warreyn et al. 2005). The child received 1 point for each correct fixation on the picture or object the examiner looked at, for a total of 4 possible points. Initiating joint attention (IJA) was assessed using the active joint attention task (eye contact in ambiguous situations) developed by Warreyn et al. (2005), in which the experimenter covers the child’s hands while he/she is playing with a toy (blocking task), or offers the child a toy but withdraws before the child can take it (teasing task), to see if the child will make eye contact with the experimenter. There were two trials of the blocking task and two trials of the teasing task. The child received 1 point for each trial in which eye contact was made, for a maximum of 4 points.
Cooperation Tasks
Two cooperation tasks were used. The first was a double-tube task adopted from Gräfenhain et al. (2009). The child took turns in either catching pegs dropped down a tube (child catching trials) or dropping the pegs down the tube (child dropping trials). After 15 s of playing, the experimenter stopped his role for 10 s and then resumed playing (behavioral interruption trial). The experimenter and child switched roles after six trials. There were six catching trials, and the child received 0 points for no attempt to play, 1 point if attempted catch but missed, 2 points if caught peg, for a maximum total of 12 points. There were six dropping trials, and the child received 0 points for no attempt to play, 1 point if dropped the peg, an additional 1 point if he/she tapped or counted 3 times, and 1 point if alternated tubes, for a maximum score of 17 points. There were two behavioral interruption trials and the child received 0 points for disengagement, 1 point for individual attempt, and 2 points for partner orientation. The percent correct catching trials and dropping trials was calculated.
The second cooperation task was a turn-taking drumming game described in Fitzpatrick et al. (2013). Three cylinders and a drum stick were placed on one side of a turntable. The experimenter picked up the drum stick and tapped the cylinders in sequence, put the drum stick on the turntable and rotated the cylinders in front of the child to take a turn. After 15 s of playing, the experimenter stopped his role for 10 s and then resumed playing (behavioral interruption trial). There were six trials of the turn-taking game. The child received 1 point for no attempt to play, 1 point for drumming, .5 points for drumming in sequence, 1 point for placing the drum stick on turn-table, .5 points for handing the experimenter the drum stick, 1 point for turning turn-table for a maximum 3.5 points per trial, 21 points possible for the task. The percent correct turn taking trials was then calculated. The behavioral interruption trial was coded as above, the sum of all three behavioral interruption trials was calculated, and the percentage of trials in which the child re-engaged the experimenter was then calculated from the sum.
Theory of Mind Tasks
Children completed four theory of mind (ToM) tasks—three verbal and one non-verbal—to measure understanding of intentionality. The “Smarties” candy task (Luckett et al. 2002; Perner et al. 1987) was the first verbal task. In this task children are shown a familiar confectionery carton and asked what they thought was inside. Once children have responded with whatever candy it says, the lid is removed from the carton to reveal the true contents—a pencil. The lid is replaced, and children are asked what another child, who has not seen inside the carton, will think is inside. To succeed on the Smarties task, children are required to understand that another child who is not aware of information to the contrary will be likely to assume that the carton contains the candy. The child received 1 point for each false belief, reality, memory, and justification question answered correctly, for a total of 4 points. The Contents False Belief task (Wellman and Liu 2004) was the second verbal task. In this task, the child judges another person’s false belief about what is in a distinctive container when child knows what it is in the container. The child received 1 point for each question answered correctly for a total of 2 points. The “Sally-Ann” theory of mind task (Baron-Cohen et al. 1985) was used as the third verbal task and children received 1 point for each correct answer on the false belief, reality, and memory questions, for a total of 3 points. The choose-a-drawing task (Peterson 2002) was used as the non-verbal task. In this task, the child picks a drawing of what is in a box, sees what is in a box, and judges the knowledge of another person who does not see what is in a box. The child received 1 point for each false belief and reality question answered correctly, for a total of 2 points. Due to the lengthy experimental procedure, the experimenter did not always ask each child all 11 questions. Therefore, a mean was calculated for each of the four tasks (number correct/total number of questions for each task) and the sum of the mean for each ToM task was calculated and used as the ToM total score (out of a possible 4 points) in the data analysis.
Social Motor Synchronization Tasks
Children completed a battery of simple social motor imitation and synchrony tasks as an assessment of social motor synchronization. Namely, four action sequences were used that involved the interpersonal coordinating of objects, bodies, and faces. Children were instructed to tap a drumstick on a drum cylinder or use their finger to tap on a drum cylinder, tap in space, or tap their body (on their shoulders, arms and head). These sequences were completed as an imitation task after the experimenter demonstrated (social motor coordination imitation battery) or a synchronization task performing the sequences with the experimenter (social motor coordination synchrony battery). The social motor battery can be characterized as an intentional social motor synchronization task. In addition, an interpersonal hand-clapping task (patacake) was used as second social motor synchronization task that was somewhat less stereotyped, more dynamic, required more precise movement timing, and was more socially interactive. This task is a spontaneous social motor synchronization task as the synchronization arises implicitly. These tasks were reported in Fitzpatrick et al. (under review). In this paper, the weighted coherence from these tasks was used to evaluate the relationship between social motor synchronization ability and clinical and social cognitive measures of social skill, relationships that were not evaluated in Fitzpatrick et al. (under review). Weighted coherence is a dynamical measure of the coordination that occurred between the child and experimenter by estimating the degree of correlation between their movements. The movements were measured by sensors placed on the wrists. A coherence of 1 reflects perfect correlation of the movements (absolute synchrony) and 0 reflects no correlation (no synchrony).
Motor Control Tasks
Motor control ability was assessed with a two-handed drumming task that was either performed in-phase (so the two drum sticks moved together and hit the drum at the same time) or anti-phase (the two drum sticks moved and hit the drum in an alternating fashion). These motor tasks were reported in Fitzpatrick et al. (under review). Weighted coherence was used to assess the degree of synchronization between the two limbs. Of interest in this paper is how these measures of motor control ability are related to clinical and social cognitive measures of social skill, relationships that were not evaluated in Fitzpatrick et al. (under review).
Procedure
Participants completed two sessions, no more than 1-month apart. In the first session, clinical phenotyping was completed and lasted approximately 3 h. The examiner who conducted the clinical assessment has extensive experience in the assessment of children with ASD and has obtained research reliability on ADOS-2. After the screening for medical and psychopathology was conducted, participants completed the appropriate ADOS-2 module based on their language- and developmental level, and the DAS-II and CELF-4 were administered. Only the ASD group completed the ADOS-2. The SRS and CBCL were completed by a parent for participants in both groups.
In the second visit, the social cognitive, social motor synchronization tasks, and motor coordination tasks were completed. The study was conducted in a 10 ft by 12 ft laboratory room at Cincinnati Children’s Hospital Medical Center (University of Cincinnati, Cincinnati, OH). Children came into the laboratory room and were asked to sit at a 2 ft wide × 4 ft long × 2 ft high table next to the seated experimenter [see Fitzpatrick et al. (under review) for a depiction of the experimental arrangement]. Four Polhemus Latus transmitters were attached to the underside of the tabletop, one in each corner, to create a 10 × 12 × 8 ft capture volume around the table. As soon as the child was seated, the four Polhemus wireless sensors were placed in wristbands and slipped over the child’s and experimenter’s wrists (one sensor on each wrist of the child and experimenter). In order to ensure fidelity of the lengthy experimental protocol, the order of presentation of the experimental conditions was identical for all participants: (1) imitation or synchrony sequence (completed in order, object–object, body–object, body–body, body–alone, face–body); (2) Smarties ToM task; (3) motor control tasks (completed in the following order, single-handed drumming, in-phase drumming, anti-phase drumming); (4) interpersonal hand-clapping; (5) choose-a-drawing ToM; (6) IJA task; (7) double-tube cooperation task; (8) RJA task; (9) contents false belief ToM; (10) turn-table cooperation task; (11) Sally-Anne ToM task. Half of the participants in each diagnostic group were randomly assigned to complete the imitation sequence and half randomly assigned to complete the synchrony sequence.
Behavioral coding of the social cognitive tasks was conducted by two research assistants (CC and AG) blind to diagnostic group. CC was the primary coder for 85 participants and AG was the primary coder for 13 participants. Both coders coded 40 participants and inter-rater reliability was calculated for each task: initiating joint attention, r (39) = .96; responding to joint attention, r (40) = .89; cooperation total, r (40) = .90; behavioral interruption, r (41) = .71; and theory of mind total, r (40) = .99.
To summarize the research design, the clinical phenotyping dependent variables were chronological age, CELF (FD and FS score), DAS (GCA and SNC scores) ADOS (SA, RRB, Comparison Score), SRS, and CBCL (Attention Problems, Social Problems, and ADHD scores). Social cognitive dependent variables were IJA, RJA, spontaneous imitation, behavioral interruption, and ToM. Social synchronization dependent variables were interpersonal hand-clapping coherence and social motor battery coherence. Motor control dependent measures were in-phase drumming coherence and anti-phase drumming coherence. Diagnostic group (ASD, control) was a between-subjects variable.
Group differences in clinical phenotyping and social cognitive tasks were evaluated with independent samples t-tests. Correlations were calculated using pooled data from both groups to evaluate the relationship between social motor synchronization, motor control, and clinical, and social cognitive variables. We conducted the correlations with data from both groups in order to include an unrestricted range of social and communicative abilities to reflect the full spectrum of abilities and ensure sufficient power. A factor analysis was conducted with the data from the ASD participants only to understand the relationship between ASD severity and social motor synchronization because ADOS scores were not available for the control group.
Results
Group Differences in Clinical Phenotyping
The groups did not differ in chronological age and the DAS-II GCA scaled score for both groups was in the normal range of 85–115, although the score of the ASD group was slightly lower than the control group (see Table 2). As seen in Table 2, independent samples t-tests revealed significant group differences for all the clinical phenotyping measures. The children in the ASD group had higher scores for attention problems, social problems, ADHD, and social impairments than the children in the control group.
Group Differences in Social Cognitive Measures
The majority of the social cognitive measures differentiated the two diagnosis groups, as seen in Table 3. Children with ASD had significantly lower scores than controls on responding to joint attention, cooperation, and theory of mind. In contrast, the children in the ASD group had higher scores than controls on measures of behavioral interruption. There were no significant differences in initiating joint attention.
Relationship Between Social Motor Synchronization and Clinical Measures
Fitzpatrick et al. (under review) previously reported that children with ASD had lower social motor synchronization scores in both the interpersonal hand-clapping task and the social motor battery. To evaluate the relationship between social motor synchronization ability and clinical measures of social skill, bivariate correlations were calculated between the clinical measures reported here and the weighted coherence scores for the interpersonal hand-clapping and social motor battery. As seen in Table 4, interpersonal hand-clapping coherence was significantly correlated with all the clinical measures except for the measures of language and intelligence (CELF-4 FD, DAS-II GCA, and DAS-II SNC). Interpersonal hand-clapping coherence was negatively correlated with ADOS-2, SRS, and the CBCL measures of attention problems, social problems, and ADHD. Similarly, the social motor battery coherence was (a) negatively correlated with SRS and CBCL measures; and (b) not correlated with measures of language and intelligence (CELF-4 FD, CELF-4 FS, DAS-II GCA, and DAS-II SNC). However, the coherence observed for the social motor battery was not correlated with the ADOS-2.
Relationship Between Social Motor Synchronization and Social Cognitive and Motor Measures
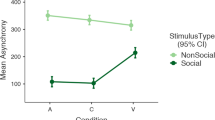
Bivariate correlations were also calculated to examine the relationship between social motor synchronization ability and social cognitive and motor measures. As seen in Table 5, interpersonal hand-clapping coherence had significant, positive correlations with RJA, cooperation, ToM, and in-phase drumming and a significant, negative correlation with behavioral interruption. Interpersonal hand-clapping coherence was not correlated with IJA, or anti-phase drumming. Similarly, social motor battery coherence was positively correlated with ToM and was not correlated with IJA, RJA, cooperation, or in-phase or anti-phase drumming (Table 5).
Relationship Between Motor Ability and Clinical and Social Cognitive Measures
In-phase drumming weighted coherence was negatively correlated with SRS, CBCL attention problems, social problems, ADHD, and behavioral interruption (see Table 6). In-phase drumming coherence was positively correlated with RJA, and ToM. No other correlations were significant. In contrast, anti-phase drumming coherence had significant negative correlations only with CBCL attention problems and behavioral interruption. No other correlations were significant.
Factor Analysis
We ran a factor analysis with the data from the ASD participants and included variables that measured a range of behaviors and assessed a range of social and communicative abilities—social motor synchronization ability (interpersonal hand-clapping and social motor battery coherence), motor ability (in-phase drumming coherence), autism severity (ADOS-2 comparison score), attention (CBCL ADHD), communication ability and social responsiveness (SRS), cooperation (cooperation total), joint attention (RJA), and theory of mind (ToM total). Some of the behaviors were measured multiple ways so we chose the measure with the strongest correlation for inclusion in this factor analysis.
The performed factor analysis satisfied several adequacy criteria. First, all items correlated at least .4 with at least one other item, suggesting reasonable factorability. Second, the Kaiser–Meyer–Olkin measure of sampling adequacy was .55 (above the recommended value of .5), and Bartlett’s test of sphericity was significant (χ2 (36) = 70.52, p = .001). Additionally, the communalities were all above .5, confirming that each item shared some common variance with other items.
A factor analysis using varimax (orthogonal) rotation found that the four factors explained 74.04% of the variance. The loadings <0.40 were excluded. The results of this solution are shown in Table 7. Four items, the ADOS-2 composite, theory of mind, cooperation, and interpersonal hand-clapping coherence loaded onto Factor 1 and explained 23.69% of the variance. We interpret Factor 1 as indexing the more implicit cognitive knowledge needed to understand another’s mentalizing in order to behaviorally cooperate in a spontaneous and less conscious manner. Two items loaded onto Factor 2: attention and social responsiveness, and explained an additional 20.83% of the variance. Factor 2 gauges the ability to perceptually attend to social information in order to respond to others. The third factor loaded two items: RJA and motor ability, and explained an additional 16.90% of the variance and indexes the motor underpinning of responding to others. The final factor was comprised of theory of mind and social motor battery coherence, and explained an additional 12.61% of the variance. Factor 4 captures the more explicit cognitive ability of understanding another’s mental state in order to intentionally perform joint actions.
Interestingly, the two social motor synchrony measures loaded onto separate factors (1 and 4), but both loaded with theory of mind, suggesting that social motor synchronization may be an embodied measure of our ability to understand another’s mental state. However, the implicit knowledge needed for more spontaneously arising synchronization (Interpersonal Hand-clapping in Factor 4) may have different underlying mechanisms from the explicit knowledge needed for more intentionally synchronization actions performed with another person (Social Motor Battery in Factor 1). The other two factors seem to establish the importance of perceptual motor abilities in our social interactions. The ability to pick up perceptual information and the ability to coordinate motor movements are important for responding to others socially. Also of note is the finding that neither of the social motor synchrony measures loaded onto the same factor as motor ability, suggesting that social motor synchronization difficulties cannot be accounted for by pure motor deficits.
Discussion
The goal of this study was to explore the relationships between dynamical measures of social motor synchronization and assessments of ASD traits. The results overall demonstrate that dynamical measures of social motor synchronization ability were related to various measures of social competence (i.e., the perceptual, cognitive and emotional skills that facilitate communication and interaction with others) that index ASD traits and provide preliminary support for a social motor synchrony model of autism. They suggest that objective dynamical measures of social motor synchronization have the ability to provide new insights into understanding ASD and could ultimately aid clinical diagnosis and prognosis.
Social Motor Synchronization is Related to Experimental and Clinical Measures of Social Cognition
Group differences reflecting differences in autism traits were found for both measures of social motor synchronization as well as measures of social cognition. Significant group differences for this data were previously reported for social motor synchronization for both interpersonal hand-clapping and social motor battery (Fitzpatrick et al., under review). However, significant group differences were also found for all the social cognitive measures except for initiating joint attention. Children with ASD had significantly lower scores than controls on measures of responding to joint attention, cooperation, and ToM. Interestingly, scores of the ASD children were significantly higher on measures of behavioral interruption during a cooperation game, which may indicate the importance of social context in influencing whether a child persists in engaging another person when they are non-responsive. These finding points to difficulties in being able to know when to engage another person based on social context.
Importantly, we found significant correlations between both types of social motor synchronization (interpersonal hand clapping and social motor battery) and behavioral interruption and ToM. However, only interpersonal hand-clapping (spontaneous social motor synchronization) was correlated with RJA and cooperation and only the social motor battery (intentional social motor synchronization) was correlated with IJA. These correlations suggest that the different types of synchronization tasks may be tapping into different dimensions of cognitive competence needed for social interactions. The more fluid, implicit, and dynamic exchange characteristic of the interpersonal clapping game which arises spontaneously is somewhat different from the more stereotyped and explicitly intentional interaction during the social motor battery. These different social motor interactions may require slightly different cognitive processes to maintain. This interpretation is reinforced by the factor analysis in which interpersonal hand-clapping coherence and social motor battery loaded on separate factors. This interpretation is also consistent with the findings of Fitzpatrick et al. (2016) who found deficits in spontaneous and intentional social motor synchronization in ASD and control adolescents, with spontaneous and intentional social motor synchronization also loading onto separate factors. This disruption in both spontaneous and intentional social motor synchronization may be a unique feature of ASD traits, as Varlet et al. (2012) found that participants with schizophrenia had a different pattern of social motor synchronization deficit. In particular, participants with schizophrenia were equivalent to controls in spontaneous social motor synchronization but had deficits in intentional social motor synchronization. Future research is planned to explore social motor synchronization in more spontaneous and less scripted tasks as found, for example, in the coordination of body movements during conversations (Ramseyer and Tschachter 2011; Schmidt et al. 2014). More research is needed to distinguish the social motor synchronization deficits evident in ASD from other disorders.
In addition, social motor synchronization ability was correlated with a number of clinical measures—SRS and CBCL attention, social problems, and thought problems sub-scales typically thought to be ASD traits. The finding that problems in social motor synchronization are associated with problems in social and emotional skills underscores the need for a fuller understanding of the role of social motor synchronization in ASD. As coordinating one’s movements with another person typically helps to facilitate social connection (e.g., Hove and Risen 2009; Wiltermuth and Heath 2009), these findings raise the possibility that children with ASD have disruptions in social motor synchronization ability that may interfere with the formation of social bonds (Feldman 2007). Further research is necessary to differentiate whether social motor synchronization ability is a critical deficit that causes disruptions in the development of social and emotional skills Relately, research is needed to investigate whether disruptions in social motor synchrony are the consequence of other underlying mechanisms: neuromotor impairments (Dowd et al. 2010; Gernsbacher et al. 2008), attention processing (Hayes 1987; Landry and Bryson 2004; O’Riordan et al. 2001) or social attention (Chawarska et al. 2010; Fischer et al. 2014; Klin et al. 2003; Schultz 2005) are all potential underlying mechanisms that should be explored.
Social Motor Synchronization Varies with ASD Severity and may Provide Insights into the Heterogeneous ASD Population
The ADOS-2 comparison score was used as an index of ASD severity and the only clinical or social cognitive measure that was correlated with it was ToM. No other relationships were significant. This finding reinforces the extensive literature that points to the importance of ToM for characterizing ASD traits (Baron-Cohen et al. 1985; Happé 1993). Interestingly, however, there was a significant correlation between ADOS-2 comparison score and interpersonal hand-clapping coherence and both social motor synchronization measures were correlated with SRS and CBCL. These findings suggest that dynamical measures of social motor synchronization ability are better able to capture the unique and complex constellation of ASD traits.
These findings are also consistent with some researchers who have argued that traditional tasks may not be sufficient measures of the type of social adaptation skills needed in actual social interactions (e.g., Klin 2000). It has been argued that tasks and measurement techniques that are better able to capture the essential qualities of social performance in naturalistic situations are needed. Measuring social motor synchronization ability could be such a technique. Its evaluation of the embodied social stability over time may be an avenue into understanding the heterogeneity in ASD and for researching ASD traits across the spectrum. Moreover, such an objective measure of social impairment could make an important contribution to phenotype studies, etiology studies, as well as studies evaluating the effectiveness of different treatments for specific ASD clinical profiles. For example, clinical measures of social functioning in ASD and schizophrenia are non-specific and highly variable, in part because most rely on subjective patient and parent report and/or clinician ratings. Thus, identifying objective biomarkers with well-defined mechanistic underpinnings will greatly enhance targeting of interventions to particular subgroups of patients. However, because our sample did not include participants across the spectrum, more research is needed to evaluate these potential implications.
Social Motor Synchronization Differences are not Fully Explained by a Motor Control Deficit
While previous research (Fitzpatrick et al., under review; Isenhower et al. 2012) has found that children with ASD displayed a motor deficit both in terms of their ability to synchronize their arms during a drumming task (as indicated by lower coherence scores) and the ability to make consistent, smooth movements (as indicated by higher variability), only interpersonal hand-clapping coherence was correlated with in-phase drumming coherence. The correlation between interpersonal hand-clapping coherence and anti-phase drumming was not significant nor was the social motor battery coherence correlated with either in-phase or anti-phase drumming performance. Additionally, in-phase drumming coherence loaded on a separate factor than either interpersonal hand clapping or social motor coordination battery. This finding suggests that although children with ASD exhibited poorer motor coordination, social motor synchronization may not be fully explained by a motor control deficit. Rather than an over-arching neuromotor impairment contributing to ASD traits (Dowd et al. 2010; Gernsbacher et al. 2008), our results suggest that the underlying mechanism is a social motor synchronization one, as evidenced by the finding that social motor synchronization loaded onto the two factors that contained ToM (i.e., ability to understand another’s mental state). In addition, two factors in the factor analysis seem to indicate that there is a non-social perceptual motor deficit that is not explicitly tied to social knowledge (e.g., ToM) but to attentional processes. We found that one of these factors indexed the motor underpinnings of responding to others (motor ability and responding to joint attention) while the other factor was related to the ability to perceptually attend to social information (SRS and CBCL ADHD). These factors raise the possibility that perceptual and motor processes play a role in social interactions that is somewhat different from social cognition and likely have different underlying mechanisms. The incredible heterogeneity in autism may be due to the fact that it is possible to have disruptions in some of these processes, but not others. Additional research is needed to explore the role of motor execution and attention processes in contributing to ASD traits and to determine whether the mechanisms are separate, independent, and can break down in isolation.
Limitations
Several limitations of this study should be noted and taken into account when evaluating the implications of the findings. First, only higher functioning individuals with ASD were evaluated in this study. Therefore, caution is needed before generalizing our findings to lower functioning individuals. In addition, our groups were only matched on age (not IQ or language level, for example), which could be responsible for some group differences seen. Finally, in order to ensure fidelity of the experimental procedure, order of presentation of conditions was the same for all participants and could contribute to potential order effects. It is possible that since children have been shown to prefer adults with whom they synchronize and/or imitate (Carpenter et al. 2013; Fawcett and Liszkowski 2012; Tunçgenç et al. 2015), performance on subsequent tasks could be affected by the prior motor coordination. While our initial findings are promising, additional research is needed to research these issues.
Conclusion and Clinical Implications
Research efforts to identify the critical deficit or deficits underlying ASD have largely been contradictory and inconclusive. While the research presented here is not able to definitively identify the critical deficit(s) or underlying mechanisms, nor provide definitive support for a social motor synchrony model of autism, it does provide a promising pathway for future research. Our findings suggest that spontaneous, more implicit social motor synchronization is related to ASD traits in a different way than more explicit, intentional social motor synchronization, although both are related to social knowledge. Quantification of social motor synchronization ability using dynamical measures thus reflects a potential neurophysiological biomarker that is significantly associated with social functioning and severity of ASD traits. Alternatively, perceptual (i.e., attention) and motor processes were found to be related more to social performance than social knowledge. Furthermore, our results provide evidence that social motor synchronization ability is related to ASD traits across a range of social and communicative abilities and extends the literature that has found group differences in synchronization ability for children with and without ASD (e.g., Fitzpatrick et al. 2013, 2016; Fitzpatrick et al., under review; Marsh et al. 2013). Given that ASD traits are distributed across a spectrum and can be found in typically developing populations (Baron-Cohen et al. 2001), it is important to investigate the continuum of ASD traits that are included across both control and ASD subgroups.
These findings have potentially important clinical implications for early diagnosis and early intervention because social motor synchronization can be easily and objectively measured at an early age. For example, Ferronato, Domellöf, and Rönnqvist (2014) argue that coupling between motor activity and acoustic stimuli is evident very early in postnatal life and is important for the development of gesturing, language, and social communication. They call for more research to evaluate these couplings in pre-term, at risk infants. We would argue that disruptions in the synchronization of motor activity and acoustic stimuli could also be helpful in identifying children at-risk for autism and targeting them for early intervention services. In addition, social motor synchronization ability does not depend on language ability and as such may be a useful tool for (a) assessing individuals across a range of autism severity; and (b) designing social-motor based interventions appropriate for individuals from mild to severe ASD. Additionally, the factor analysis findings identifying separate components of social ability may provide a framework for understanding the heterogeneity in autism because different individuals may have different clusters of abilities and weaknesses and this method of evaluating specific impairments for each individual could be used to develop targeted treatments.
Since social motor synchronization has been largely overlooked as a contributor to ASD traits, its relationship to them need careful and systematic investigation in order to isolate the difference between cause and effect. While the research reported here is not able to answer these questions, it is an important first step. Given the evidence that that social motor synchronization may be an embodied measure of our ability to understand another’s mental state, further research that relies on objective dynamical measures of social motor synchronization and perceptual and motor processes is needed to determine whether enhancing social motor synchronization ability has the potential to increase social competence in clinically relevant ways. Research is needed to determine whether social synchronization interventions can improve social skills in children with ASD as well as provide insights to aid clinical diagnosis and prognosis of ASD.
References
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles: An integrated system of mult-informant assessment. University of Vermont: Burlington.
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th edn.). Arlington, VA: American Psychiatric Publishing.
Baron-Cohen, S., Leslie, A. M., & Frith, U. (1985). Does the autistic child have theory of mind? Cognition, 21, 37–46.
Baron-Cohen, S., Wheelwright, S., Skinner, R., Martin, J., & Clubley, E. (2001). The autism-spectrum quotient (AQ): Evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. Journal of Autism and Developmental Disorders, 31, 5–17.
Bernieri, F. J., Davis, J. M., Rosenthal, R., & Knee, C. (1994). Interactional synchrony and rapport: Measuring synchrony in displays devoid of sound and facial affect. Personality and Social Psychology Bulletin, 20(3), 303–311.
Carpenter, M., Call, J., & Tomasello, M. (2002). Understanding ‘prior intentions’ enables 2-year-olds to imitatively learn a complex task. Child Development, 73, 1431–1441.
Carpenter, M., Pennington, B. F., & Rogers, S. J. (2001). Understanding of others’ intentions in children with autism. Journal of Autism and Developmental Disorders, 31(6), 589–599.
Carpenter, M., Uebel, J., & Tomasello, M. (2013). Being mimicked increases prosocial behavior in 18-month-old infants. Child Development, 84, 1511–1518. doi:10.1111/cdev.12083.
Charman, T. (2011). Commentary: Glass half full or half empty? Testing social communication interventions for young children with autism. Commentary on Landa, Holman, O’Neill and Stuart (2011). Journal of Child Psychology and Psychiatry, 52(1), 22–23.
Chawarska, K., Volkmar, F., & Klin, A. (2010). Limited attentional bias for faces in toddlers with autism spectrum disorders. Archives of General Psychiatry, 67(2), 178–185.
Colombi, C., Liebal, K., Tomasello, M., Young, G., Warneken, F., & Rogers, S. (2009). Examining correlates of cooperation in Autism: Imitation, joint attention, and understanding intentions. Autism, 13(2), 143–163.
Condon, W. S., & Sander, L. W. (1974a). Neonate movement is synchronized with adult speech: Interactional participation and language acquisition. Science, 183, 99–101.
Condon, W. S., & Sander, L. W. (1974b). Synchrony demonstrated between movements of the neonate and adult speech. Child Development, 45, 456–462.
Constantino, J. N., & Gruber, C. P. (2005). Social Responsiveness Scale. Los Angeles: Western Psychological Services.
de Marchena, A., & Eigsti, I. M. (2010). Conversational gestures in autism spectrum disorder: Asynchrony but not decreased frequency. Autism Research, 3, 311–322.
Delaherche, E., Chetouani, M., Mahdhaoui, A., Saint-Georges, C., Viaux, S., & Cohen, D. (2012). Interpersonal synchrony: A survey of evaluation methods across disciplines. IEEE Transactions on Affective Computing, 3(3), 349–365.
Dowd, A. M., Rinehart, N. J., & McGinley, J. (2010). Motor function in children with autism: Why is this relevant to psychologists? Clinical Psychologist, 14, 90–96.
Elliot, C. D. (2007). Differential Ability Scales II. New York: Pearson Education, Inc.
Fawcett, C., & Liszkowski, U. (2012). Mimicry and play initiation in 18-month-old infants. Infant Behavior and Development, 35, 689–696. doi:10.1016/j.infbeh.2012.07.014.
Feldman, R. (2007). Parent-infant synchrony: Biological foundations and developmental outcomes. Current Directions in Psychological Science, 16(6), 340–345.
Feldstein, S., Jaffe, J., Beebe, B., Crown, C. L., Jasnow, M., Fox, H., & Gordon, S. (1993). Coordinated interpersonal timing in adult-infant vocal interactions: A cross-site replication. Infant Behavior and Development, 16, 455–470.
Ferronato, P. A. M., Domellöf, E., & Rönnqvist, L. (2014). Early influence of auditory stimuli on upper-limb movements in young human infants: An overview. Frontiers in Psychology, 18(1043), 1–8. doi:10.3389/fpsyg.2014.01043.
Fischer, J., Koldewyn, K., Jiang, Y. V., & Kanwisher, N. (2014). Unimpaired attentional disengagement and social orienting in children with autism. Clinical Psychological Science, 2(2), 214–223.
Fitzpatrick, P., Diorio, R., Richardson, M. J., & Schmidt, R. C. (2013). Dynamical methods for evaluating the time-dependent unfolding of social coordination in children with autism. Frontiers in Integrative Neuroscience, 7(21), 1–13.
Fitzpatrick, P., Frazier, J. A., Cochran, D. M., Mitchell, T., Coleman, C., & Schmidt, R. C. (2016). Impairments of social motor synchrony evident in autism spectrum disorder. Frontiers in Psychology, 7, 1323. doi:10.3389/fpsyg.2016.01323.
Fitzpatrick, P., Romero, V., Amaral, J., Duncan, A., Barnard, H., Richardson, M. J., & Schmidt, R. C. (under review). Evaluating the importance of social motor synchronization and motor skill for understanding autism.
Gernsbacher, M. A., Stevenson, J. L., Khandakar, S., & Goldsmith, H. H. (2008). Why does joint attention look atypical in autism? Child Development Perspectives, 2, 38–45.
Gräfenhain, M., Behne, T., Carpenter, M., & Tomasello, M. (2009). Young children’s understanding of joint commitments. Developmental Psychology, 45, 1430–1443.
Gratier, M., & Apter-Danon, G. (2009). The musicality of belonging: Repetition and variation in mother-infant vocal interaction. In S. Malloch & C. Trevarthen (Eds.), Communicative musicality: Narratives of expressive gesture and being human. Oxford: Oxford University Press.
Happé, F. G. (1993). Communicative competence and theory of mind in autism: A test of relevance theory. Cognition, 48(2), 101–119.
Hayes, R. (1987). Training for work. In D. J. Cohen & A. M. Donnellan (Eds.), Handbook of autism and pervasive developmental disorders. Silver Springs, MD: Winston.
Hove, M. J., & Risen, J. L. (2009). It’s all in the timing: Interpersonal synchrony increases affiliation. Social Cognition, 27, 949–961.
Howlin, P., Goode, S., Hutton, J., & Rutter, M. (2004). Adult outcome for children with autism. The Journal of Child Psychology and Psychiatry, 45(2), 212–229.
Isenhower, R. W., Marsh, K. L., Richardson, M. J., Helt, M., Schmidt, R. C., & Fein, D. (2012). Rhythmic bimanual coordination is impaired in children with autism spectrum disorder. Research in Autism Spectrum Disorders, 6, 25–31.
Jaffe, J., Beebe, B., Feldstein, S., Crown, C. L., & Jasnow, M. (2001). Rhythms of dialogue in infancy. Monographs of the Society for Research in Child Development, Series 264, 66(2), 1–132.
Jasnow, M., & Feldstein, S. (1986). Adult-like temporal characteristics of mother–infant vocal interactions. Child Development, 57, 754–761.
Julien, D., Brault, M., Chartrand, E., & Begin, J. (2000). Immediacy behaviours and synchrony in satisfied and dissatisfied couples. Canadian Journal of Behavioral Science, 32, 84–90.
Kinsbourne, M., & Helt, M. (2011). Entrainment, mimicry, and interpersonal synchrony. In D. A. Fein (Ed.), The neuropsychology of autism (pp. 339–365). New York, NY: Oxford University Press.
Klin, A. (2000). Attributing social meaning to ambiguous visual stimuli in higher-functioning autism and Asperger syndrome: The social attribution task. Journal of Children Psychological Psychiatry, 41, 831–846.
Klin, A., Jones, W., Schultz, R., & Volkmar, F. (2003). The enactive mind, or from actions to cognition:lessons from autism. Philosophical Transactions of the Royal Society of London. Series B:Biological Sciences, 358(1430), 345–360.
Lakin, J. L., & Chartrand, T. L. (2003). Using nonconscious behavioral mimicry to create affiliation and rapport. Psychological Science, 14(4), 334–339.
Landa, R. J., Holman, K. C., O’Neill, A. H., & Stuart, E. A. (2011). Intervention targeting development of socially synchronous engagement in toddlers with autism spectrum disorder: A randomized controlled trial. Journal of Child Psychology and Psychiatry, 52, 13–21.
Landry, R., & Bryson, S. E. (2004). Impaired disengagement of attention in young children with autism. Journal of Child Psychology and Psychiatry, 45(6), 1115–1122.
Leekam, S., Baron-Cohen, S., Perrett, D., Milders, M., & Brown, S. (1997). Eye-direction detection: A dissociation between geometric and joint attention skills in autism. British Journal of Developmental Psychology, 15(1), 77–95.
Liebal, K., Colombi, C., Rogers, S., Warneken, F., & Tomasello, M. (2008). Cooperative activities in children with autism. Journal of Autism and Developmental Disorders, 38, 224–238.
Lord, C., Rutter, M., DiLavore, P. C., Risi, S., Gotham, K., & Bishop, S. (2012). Autism diagnostic observation schedule, second edition (ADOS-2) (Part I): Modules 1–4 [Manual]. Torrance, CA: Western Psychological Services.
Luckett, T., Powell, S. D., Messer, D. J., Thornton, M. E., & Schulz, J. (2002). Do children with autism who pass false belief tasks understand the mind as active interpreter? Journal of Autism and Developmental Disorders, 32(2), 127–140.
Marsh, K. L., Isenhower, R. W., Richardson, M. J., Helt, M., Verbalis, A. D., Schmidt, R. C., & Fein, D. (2013). Autism and social disconnection in interpersonal rocking. Frontiers in Integrative Neuroscience, 7(4), 1–8.
Meltzoff, A. N. (1995). Understanding the intentions of others: Re-enactment of intended acts by 18-month-old children. Developmental Psychology, 31(5), 838–850.
Miles, L. K., Nind, L. K., & Macrae, C. (2009). The rhythm of rapport: Interpersonal synchrony and social perception. Journal of Experimental Social Psychology, 45(3), 585–589.
Mundy, P. (2009). Lessons learned from autism: An information-processing model of joint attention and social cognition. In D. Cicchetti & M. R. Gunnar (Eds.), Minnesota symposium on child psychology: Meeting the challenge of translational research in child psychology (Vol. 35, pp. 59–113). Hoboken, NJ: Wiley.
Mundy, P., & Newell, L. (2007). Attention, joint attention, and social cognition. Current Directions in Psychological Science, 16, 269–274.
Mundy, P., Sigman, M., & Kasari, C. (1990). A longitudinal study of joint attention and language development in autistic children. Journal of Autism and developmental Disorders, 20(1), 115–128.
Vaughan Van Hecke, A., Mundy, P. C., Acra, C. F., Block, J. J., Delgado, C. E., Parlade, M. V., Meyer, J. A., Neal, A. R., & Pomares, Y. B. (2007). Infant joint attention, temperament, and social competence in preschool children. Child Development, 78, 53–69.
O’Riordan, M. A., Plaisted, K. C., Driver, J., & Baron-Cohen, S. (2001). Superior visual search in autism. Journal of Experimental Psychology: Human Perception and Performance, 27(3), 719–730.
Oberman, L. M., Winkielman, P., & Ramachandran, V., S (2009). Slow echo: Facial EMG evidence for the delay of spontaneous, but not voluntary, emotional mimicry in children with autism spectrum disorders. Developmental Science, 12, 510–520.
Onishi, K. H., & Baillargeon, R. (2005). Do 15-month-old infants understand false beliefs? Science, 308, 255–258.
Perner, J., Leekam, S., & Wimmer, H. (1987). Three-year olds’ difficulty with false-belief: The case for a conceptual deficit. British Journal of Developmental Psychology, 5, 125–137.
Peterson, C. C. (2002). Drawing insight from pictures: The development of concepts of false drawing and false belief in children with deafness, normal hearing, and autism. Child Development, 73(5), 1442–1459.
Peterson, C. C., & Siegal, M. (2000). Insights into theory of mind from deafness and autism. Mind & Language, 15(1), 123–145.
Phillips-Silver, J., Aktipis, C. A., & Bryant, G. (2010). The ecology of entrainment: Foundations of coordinated rhythmic movement. Music Perception: An Interdisciplinary Journal, 28(1), 3–14.
Ramseyer, F., & Tschachter, W. (2011). Nonverbal synchrony in psychotherapy: Coordinated body movement reflects relationship quality and outcome. Journal of Consulting and Clinical Psychology, 79, 284–295.
Reddish, P., Bulbulia, J., & Fischer, R. (2014). Does synchrony promote generalized prosociality? Religion, Brain & Behavior, 4, 3–19.
Reddish, P., Fischer, R., & Bulbulia, J. (2013). Let’s dance together: Synchrony, shared intentionality and cooperation. PLoS ONE, 8, 1–13.
Richardson, M. J., Dale R., & Marsh, K. L., (2014). Complex dynamical systems in social and personality psychology: Theory, modeling and analysis. In H. T. Reis, and C. M. Judd. (Eds.). Handbook of research methods in social and personality psychology (2nd edn.). New York, NY: Cambridge University Press.
Richardson, M. J., Kay, B. A., & Schmidt, R. C. (2007). Distinguishing the noise and attractor strength of coordinated limb movements using recurrence analysis. Biological Cybernetics, 96, 59–78.
Richardson, D., Dale, R., & Shockley, K. (2008a). Synchrony and swing in conversation: Coordination, temporal dynamics and communication. In I. Wachsmuth, M. Lenzen & G. Knoblich (Eds.) Embodied communication. Oxford: Oxford University Press.
Richardson, M. J., Lopresti-Goodman, S., Mancini, M., Kay, B. A., & Schmidt, R. C. (2008b). Comparing the attractor strength of intra- and interpersonal interlimb coordination using cross recurrence analysis. Neuroscience Letters, 438, 340–345.
Schmidt, R. C., Nie, L., Franco, A., & Richardson, M. J. (2014). Bodily synchronization underlying joke telling. Frontiers in Human Neuroscience, 8, 633. doi:10.3389/fnhum.2014.00633.
Schultz, R. T. (2005). Developmental deficits in social perception in autism: The role of the amygdala and fusiform face area. International Journal of Developmental Neuroscience, 23(2), 125–141.
Seger, C. & Smith, E. R. (2009). The effect of synchrony with a computerized avatar on implicit prejudice. Poster presented at Society for Social and Personality Psychology (SPSP), Tampa, FL.
Semel, E. M., Wiig, E. H., & Secord, W. A. (2003). Clinical evaluation of language fundamentals-4. San Antonio, TX: Psychological Corp/Harcourt.
Semin, G. R. (2007). Grounding communication: Synchrony. In A. Kruglanski and E. T. Higgins (Eds.), Social psychology: Handbook of basic principles (2nd edn., pp. 630–649). New York: Guilford Publications.
Shockley, K., Richardson, D. C., & Dale, R. (2009). Conversation and coordinative structures. Topics in Cognitive Science, 1, 305–319.
Thiel, M., Romano, M. C., Kurths, J., Meucci, R., Allaria, E., & Arecchi, F. T. (2002). Influence of observational noise on the recurrence quantification analysis. Physica D, 171, 138–152.
Tomasello, M. (1999) The cultural origins of human cognition. Cambridge: Harvard University Press.
Trevarthen, C., & Delafield-Butt, J. T. (2013). Autism as a developmental disorder in intentional movement and affective engagement. Frontiers in Integrative Neuroscience, 7, 49. doi:10.3389/fnint.2013.00049.
Tunçgenç, B., Cohen, E., & Fawcett, C. (2015). Rock with me: The role of movement synchrony in infants’ social and nonsocial choices. Child Development, 86, 976–984.
Valdesolo, P., Ouyang, J., & DeSteno, D. (2010). The rhythm of joint action: Synchrony promotes cooperative ability. Journal of Experimental Social Psychology, 46(4), 693–695.
Varlet, M., Bucci, C., Richardson, M. J., & Schmidt, R. C. (2015). Constraints on spontaneous entrainment. Human Movement Science, 41, 265–281.
Varlet, M., Marin, L., Raffard, S., Schmidt, R. C., Capdevielle, D., Boulenger, J. P., Del-Monte, J., & Bardy, B. G. (2012). Impairments of social motor coordination in schizophrenia. PLoS ONE, 7, e29772.
Warneken, F., Chen, F., & Tomasello, M. (2006). Cooperative activities in young children and chimpanzees. Child Development, 77(3), 640–663.
Warreyn, P., Roeyers, H., Oelbrandt, T., & De Groote, I. (2005). What are you looking at? Joint attention and visual perspective taking in young children with autism spectrum disorder. Journal of Developmental and Physical Disabilities, 17(1), 55–73.
Wellman, H. M., Cross, D., & Watson, J. (2001). Meta-analysis of theory-of-mind development. The truth about false belief. Child Development, 72, 655–684.
Wellman, H. M., & Liu, D. (2004). Scaling of theory of mind tasks. Child Development, 75, 523–541.
Wiltermuth, S. S., & Heath, C. (2009). Synchrony and cooperation. Psychological Science, 20, 1–5.
Woodward, A. L. (1998). Infants selectively encode the goal object of an actor’s reach. Cognition, 69, 1–34.
Zivotofsky, A. Z., & Hausdorff, J. M. (2007). The sensory feedback mechanisms enabling couples to walk synchronously: An initial investigation. Journal of NeuroEngineering and Rehabilitation, 4(1), 28–33.
Acknowledgments
Research reported in this article was supported by the National Institute of Mental Health of the National Institutes of Health under award number R21MH094659. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Health.
Author Contributions
Study conception and design: PF, MR, RS; Acquisition of data: VR, JA, AD, HB; Analysis and interpretation of data: PF, MR, RS, VR; Drafting of manuscript: PF, MR, RS, VR, JA, AD, HB; Critical revision: PF, MR, RS, VR. All authors have made substantial contributions to the manuscript and have given final approval to the submitted and revised manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
All parents of participants gave informed, written consent for their children to take part in the study, and releases were also obtained for the video recordings.
Rights and permissions
About this article
Cite this article
Fitzpatrick, P., Romero, V., Amaral, J.L. et al. Social Motor Synchronization: Insights for Understanding Social Behavior in Autism. J Autism Dev Disord 47, 2092–2107 (2017). https://doi.org/10.1007/s10803-017-3124-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-017-3124-2