Abstract
We conducted meta-analyses of 67 studies on the association between neonatal proxies of impaired gas exchange and intellectual disability (ID) or autism spectrum disorders (ASD). Neonatal acidosis was associated with an odds ratio (OR) of 3.55 [95 % confidence interval (95 % CI) 2.23–5.49] for ID and an OR of 1.10 (95 % CI 0.91–1.31) for ASD. Children with a 5-min Apgar score of <7 had an OR of 5.39 (95 % CI 3.84–7.55) for ID and an OR of 1.67 (95 % CI 1.34–2.09) for ASD. O2 treatment was associated with an OR of 4.32 (95 % CI 3.23–5.78) for ID and an OR of 2.02 (95 % CI 1.45 to 2.83) for ASD. Our meta-analysis demonstrates an increased risk of ID and (to a lesser extent) ASD in children with neonatal hypoxia. Moreover, our findings raise the possibility that concomitant ID might account for the observed association between the gas exchange proxies and ASD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perinatal impaired gas exchange (hypoxia and hypercarbia) is a determinant of mortality in the neonatal period (Victory et al. 2004; Casey et al. 2001). Impaired gas exchange has also been associated with neurological outcomes including seizure, cerebral palsy and neonatal encephalopathy (Scafidi and Gallo 2008; Martinez-Biarge et al. 2011). Hypoxia and hypercarbia alter cell energy metabolism which can subsequently lead to cell death (Scafidi and Gallo 2008). Brain tissue is particularly sensitive to disturbances in energy metabolism during the perinatal period (du Plessis and Volpe 2002; de Haan et al. 2006). Several studies suggest that impaired gas exchange in the perinatal period may be associated with neurodevelopmental abnormalities such as intellectual disability (ID) and autism spectrum disorders (ASD) but results are mixed (Gardener et al. 2011; Gonzalez and Miller 2006).
Whereas measurement of impaired gas exchange would ideally include a combination of clinical, laboratory, and pathology data, clinical proxies are typically used in neonatal units (Goldenberg et al. 1984; Gonzalez and Miller 2006). Many of these proxies are related to resuscitative efforts of the newborn, which reflects some degree of cardiorespiratory compromise (Kattwinkel et al. 2010). Despite limitations, such measures have an advantage of being measured in virtually every newborn. For example the Apgar score, introduced by Virginia Apgar in 1953 is a measure of well-being in the immediate neonatal period and is routinely assessed worldwide (Apgar 1953). Standards measurements take place at 1 and 5 min after birth. In recent years, there has been a growing debate over the utility of Apgar score for the prediction of asphyxia (American Academy of Pediatrics 2006; Watterberg et al. 2015). Nevertheless, universal measurement of Apgar score provides researchers with an opportunity for an in-depth exploration of its clinical values. Several other measures have been used as proxies of impaired gas exchange including delayed onset of breathing, need for resuscitation and/or ventilation, and metabolic acidosis (Scafidi and Gallo 2008). In the present study we aimed to systematically and quantitatively review the evidence for the hypothesis that proxies of impaired gas exchange are associated with increased risk of ID and ASD.
Methods
We performed our meta-analysis in accordance to the latest guidelines on meta-analysis of observational studies (Stroup et al. 2000).
Search Strategy and Eligibility Criteria
A.M. and J.M. independently searched Medline and Web of Science core collection since inception through July 2015 for English language studies using the search terms: [(perinatal) OR (neonatal) OR (prenatal) OR (birth) OR (asphyxia) OR (hypoxia) OR (anoxia) OR (Apgar) OR (“fetal distress”) OR (“respiratory distress”)] AND [(autism) OR (“autistic disorder”) OR (“mental retardation”) OR (“intellectual disability”)]. We also manually searched references of several relevant review articles on the subject.
We included all published peer-reviewed population or clinic-based studies with a healthy comparison group that assessed the relationship between proxies of impaired gas exchange and ID or ASD. Definition of ID and ASD were based on the author criteria. Neurodevelopmental comorbidities were not considered as exclusion criteria. The studies were required to include one or more proxies of impaired gas exchange namely: acidosis, Apgar score, need for resuscitation or oxygenation, apnea or delayed crying and breathing, respiratory distress syndrome, and asphyxia/hypoxia (as defined by the author).
Exclusion criteria were: (1) assessing proxies as a part of a larger optimality score (without separate data), (2) failure to separate data on ID or ASD and including them as a broader term e.g. “neurodevelopmental disability”, (3) providing insufficient information to extract estimates and (4) limiting the study to high risk groups such as neonatal ICU survivors or preterm individuals.
Selection of the Studies and Data Extraction
Two independent reviewers (A.M. and J.M.) screened search output for eligible studies and discussed any discordance with a third reviewer (A.R.) to reach a final conclusion. Overlap of reports from the same study was investigated by the author names, location, and date. In the case of overlap, we selected the most suitable report based on a combination of quality, sample size, publication year, and adequate data presentation. Estimates for each study were extracted by A.M. independently on two separate occasions. In the case of inadequate presentation of data, we contacted the corresponding authors to obtain the data. We extracted the following data for each study.
-
1.
Setting (population-based or clinical)
-
2.
Definition of ID or ASD
-
3.
Characteristics of subjects
-
4.
Proxies of impaired gas exchange as risk factors
-
5.
Results in the form of 2 × 2 contingency table, or odds ratio (OR) and 95 % confidence intervals (95 % CI). Adjusted estimates were also extracted if available.
-
6.
In the case of ID, we also extracted mean and SD of IQ, if available for the exposed and unexposed groups.
We assessed the quality of each study using the Newcastle–Ottawa scale for assessment of observational studies in systematic reviews (Wells et al. 2011). This nine-point scale evaluates quality of studies in domains of sample selection, comparability, and outcome or exposure. This scale has been used widely in systematic reviews and is recommended by Cochrane’s Collaboration (Higgins 2012).
Statistical Analysis
Stata/MP V.14.0 (StataCorp, College Station, TX) was used for all data analysis. Meta-analysis and meta-regression were performed using “metan” and “metareg” commands respectively. We calculated pooled ORs (95 % CIs) for each proxy-outcome combination if two or more studies were available. Some studies reported results for subtypes of ID (mild, moderate, severe, profound) or ASD [autistic disorder, pervasive developmental disorder (PDD), Asperger’s syndrome]. In such cases the contingency table was used to recalculate the combined OR (95 % CI). If the values for 2 × 2 tables were not available, but the control group for each subtype was different, all ORs (95 % CI) were included in the meta-analysis separately. If neither was available and we could not obtain data from the author, the OR from the most representative group (usually that with the largest sample size) was included. Some studies reported relative risks. We recalculated ORs and 95 % CIs for these studies or requested data from the authors. We also carried out a meta-analysis of studies that compared continuous IQ scores between individuals with and without proxies of impaired gas exchange using standardized mean difference (SMD). In the case of Apgar score, if more than one cut-off was used for definition of a low Apgar score, we pooled data for each cut-off separately. Because few studies reported adjusted ORs, only crude estimates were used for the main meta-analyses. To study the effect of multivariable adjustment on the estimates, we also performed a sensitivity analysis using the adjusted estimates.
Publication bias was assessed using Peters regression test (Peters et al. 2006). When there was a risk of publication bias in subgroups in the absence of heterogeneity, trim and fill method was used within that subgroup to correct for potentially unpublished studies (Duval and Tweedie 2000). Agreement between the standard estimates and the estimates calculated by trim and fill method ensures that the findings are robust to bias (Peters et al. 2007).
We used a fixed or random effect model based on heterogeneity status. I2 statistics, and p value from heterogeneity Chi squared (I2 > 50 % or p < 0.1 meaning heterogeneous) were used to assess for heterogeneity. We then investigated heterogeneity using random-effect meta-regression. Meta-regression was performed only if at least ten studies were available. We performed meta-regression for year of publication (both as continuous and categorical with categories of before 1990, 1990 and thereafter), sample size (both as continuous and categorical with categories of <1000, >1000), country (North America versus other countries), type of study (population-based vs. clinic-based), disorder type for ASD (autism or ASD), IQ score cut-off for ID. Standard meta-regression methods can lead to false positive findings in the case of significant heterogeneity. To reduce the risk of false positive results, we used Monte Carlo simulation with 1000 permutations to report the p values.
We also performed sensitivity analyses for different pooling methods (fixed vs. random), population based studies, high quality studies (quality score >6), studies with adjusted estimates, IQ cut-off score of <70 (for ID), and autism and ASD subgroups (for ASD).
Results
Search Results and Study Characteristics
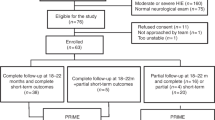
A total of 12,119 potentially relevant reports were identified. After excluding 3134 duplicates, 8649 reports were further excluded by screening titles and abstracts. We identified 19 additional studies by searching in the references of relevant review articles. Out of 355 full-text papers, a total of 67 studies (34 studies of ID and 31 studies of ASD, 2 studies of both) were eligible for meta-analysis (see eFigure 1 for specific reasons of exclusion) (Akesson 1966; Atladottir et al. 2015; Benaron et al. 1960; Bilder et al. 2009, 2013; Buchmayer et al. 2009; Burd et al. 1999; Burstyn et al. 2010, 2011; Camp et al. 1998; Campbell et al. 1950; Cans et al. 1999; Cassimos et al. 2015; Chapman et al. 2008; Comi et al. 1999; Corah et al. 1965; Darke 1944; Deykin and MacMahon 1980; Dodds et al. 2011; Drage et al. 1969; Duan et al. 2014; Dweck et al. 1974; Ehrenstein et al. 2009; Finegan and Quarrington 1979; Fisch et al. 1975; Froehlich-Santino et al. 2014; Gillberg et al. 1990; Gillberg and Gillberg 1983; Glasson et al. 2004; Graham et al. 1962; Handley-Derry et al. 1997; Jonas et al. 1989; Kamper 1978; Khaiman et al. 2015; Lamont and Dennis 1988; Langridge et al. 2013; Larsson et al. 2005; Lawlor et al. 2006; Lord et al. 1991; Louhiala 1995; Mamidala et al. 2013; Maramara et al. 2014; Mason-Brothers et al. 1990; Mrozek-Budzyn et al. 2013; Nath et al. 2012; Odd et al. 2009; Piven et al. 1993; Polo-Kantola et al. 2014; Rantakallio and von Wendt 1985; Robertson and Finer 1993; Schreiber 1943; Seidman et al. 1991; Sonnander and Gustavson 1987; Steffenburg et al. 1989; Stein et al. 2006; Stromme 2000; Sugie et al. 2005; Sussmann et al. 2009; Taylor et al. 1985; Thorngren-Jerneck and Herbst 2001; Usdin and Weil 1952; van Handel et al. 2007; Visser et al. 2013; von Wendt and Rantakallio 1987; Williams et al. 2008; Zhang et al. 2010; Maimburg and Vaeth 2006). Upon contact with the authors, we were able to retrieve data for two large studies (Langridge et al. 2013; Chapman et al. 2008). The most widely used proxy of impaired gas exchange was 5-min Apgar score <7, measured in 17 studies. eTable 1 and eTable 2 summarize the main characteristics of the studies included in the meta-analysis.
Meta-analysis
Results of meta-analyses are presented in Table 1. In the analyses of different proxies of impaired gas exchange, results of regression test for small study effect were significant for one meta-analysis. We observed slight changes in pooled estimates following the use of trim and fill method to correct for small study effect (Table 1). The measure for inter-study heterogeneity was significant for three out of eight meta-analyses for ID, and two out of ten meta-analyses for ASD (Table 1). Therefore, for the main analyses we used random effect models in these cases, whereas in the rest of the meta-analyses we used fixed effect models.
Acidosis
Two studies for ID (Dweck et al. 1974; Cans et al. 1999) and two studies for ASD (Maimburg and Vaeth 2006; Burstyn et al. 2011) investigated the association between neonatal acidosis and the outcomes of interest (Table 1). Acidosis at birth was associated with an OR of 3.55 (95 % CI 2.23–5.49) for ID, whereas it only slightly increased the risk of ASD (OR 1.10; 95 % CI 0.91–1.31).
Apgar Score
An Apgar score of <7 at 1 min was associated with an OR of 3.28 (95 % CI 2.31–4.65) for ID (Louhiala 1995; Taylor et al. 1985; Stromme 2000) and an OR of 1.40 (95 % CI 1.26–1.55) for ASD (Mason-Brothers et al. 1990; Polo-Kantola et al. 2014; Burstyn et al. 2010) (Table 1). Children with an Apgar score of < 7 at 5 min (Cans et al. 1999; Chapman et al. 2008; Ehrenstein et al. 2009; Jonas et al. 1989; Lamont and Dennis 1988; Louhiala 1995; Stromme 2000; Sussmann et al. 2009; Taylor et al. 1985; Thorngren-Jerneck and Herbst 2001; Seidman et al. 1991) had an OR of 5.39 (95 % CI 3.84–7.55) for ID and an OR of 1.67 (95 % CI 1.34–2.09) for ASD (Buchmayer et al. 2009; Burstyn et al. 2010; Mrozek-Budzyn et al. 2013; Bilder et al. 2009; Mason-Brothers et al. 1990; Dodds et al. 2011) (Fig. 1). Furthermore, there was a progressive increase in the risk of ID (but not ASD) with a decrease in the 5-min Apgar score cut-off, although the number of studies for each cut-off (except for the cut-off score of 7) was small (Fig. 1).
Apnea and Respiratory Distress
Meta-analysis of five studies for neonatal apnea showed an OR of 2.93 (95 % CI 1.45–5.92) for ID (Benaron et al. 1960; Camp et al. 1998; Jonas et al. 1989; Sonnander and Gustavson 1987; Usdin and Weil 1952) (Table 1). Similarly, meta-analysis of five studies showed an OR of 2.89 (95 % CI 1.46–5.72) for ASD (Deykin and MacMahon 1980; Glasson et al. 2004; Mamidala et al. 2013; Stein et al. 2006; Zhang et al. 2010). Respiratory distress was associated with an OR of 2.70 (95 % CI 2.28–3.19) for ID (Atladottir et al. 2015; Fisch et al. 1975; Gillberg et al. 1990; Kamper 1978) and an OR of 1.55 (95 % CI 1.34–1.78) for ASD (Steffenburg et al. 1989; Piven et al. 1993; Finegan and Quarrington 1979; Gillberg and Gillberg 1983; Bilder et al. 2009; Lord et al. 1991; Sugie et al. 2005; Mrozek-Budzyn et al. 2013; Froehlich-Santino et al. 2014; Dodds et al. 2011; Buchmayer et al. 2009; Atladottir et al. 2015).
Resuscitation and Ventilation
A meta-analysis of four studies (Odd et al. 2009; Sonnander and Gustavson 1987; Langridge et al. 2013; Sussmann et al. 2009) showed that neonatal resuscitation was associated with a slightly increased risk of ID (OR 1.56; 95 % CI 1.47–1.66) (Table 1). The only study (Langridge et al. 2013) that addressed the association between resuscitation and risk of ASD found a slightly increased risk of ASD (OR 1.22; 95 % CI 1.08–1.37). O2 treatment was associated with an OR of 4.32 (95 % CI 3.23–5.78) for ID (Bilder et al. 2013; Cans et al. 1999; Gillberg et al. 1990; Jonas et al. 1989; Kamper 1978; Taylor et al. 1985) and an OR of 2.02 (95 % CI 1.45–2.83) for ASD (Finegan and Quarrington 1979; Froehlich-Santino et al. 2014; Gillberg and Gillberg 1983; Lord et al. 1991; Mason-Brothers et al. 1990; Mrozek-Budzyn et al. 2013; Piven et al. 1993; Steffenburg et al. 1989; Bilder et al. 2009) (Fig. 2).
Undefined Hypoxia/Asphyxia
We found several studies that assessed the association between ID/ASD and hypoxia/asphyxia without defining the latter (Table 1). Meta-analysis of six studies (Darke 1944; Akesson 1966; Schreiber 1943; Rantakallio and von Wendt 1985; Campbell et al. 1950; Graham et al. 1962) showed a significantly increased risk of ID in children with undefined asphyxia/hypoxia (OR 3.29; 95 % CI 1.81–5.96). Slightly higher estimates were found for the association between ASD and undefined asphyxia/hypoxia (OR 3.84; 95 % CI 1.95–7.56) (Comi et al. 1999; Froehlich-Santino et al. 2014; Visser et al. 2013; Mamidala et al. 2013; Duan et al. 2014; Sugie et al. 2005; Maramara et al. 2014; Khaiman et al. 2015; Nath et al. 2012).
Meta-regression and Sensitivity Analysis
In all five meta-analyses where there was significant heterogeneity, we used a random-effect model. In only one meta-analyses on the association between 5-min Apgar score and ID was there a sufficient number of studies to allow for a meta-regression analysis. None of the tested variables in the meta-regression could explain the heterogeneity.
We performed several sensitivity analyses to assess the effect of various conditions on the estimates (Table 2). The difference in the estimates between random and fixed-effect models were <10 % with one exception; there was a 60 % difference in the pooled estimates between random-effect and fixed-effect meta-analyses of the association between ASD and apnea. The number of studies with adjusted estimates was small. Overall, analyses of studies with adjusted estimates were associated with <20 % change in the estimates, except for the meta-analysis of the association between undefined asphyxia/hypoxia and ASD. In general, meta-analyses of population-based and high-quality studies had little effect on the estimates, except for the association between ID and undefined asphyxia/hypoxia and the association between ASD and apnea. Meta-analyses of autism often resulted in larger estimates than meta-analyses of ASD, although the 95 % CIs always overlapped.
The number of studies that provided mean and standard deviation for IQ was small. A meta-analysis of two studies using hypoxic ischemic encephalopathy as the definition of asphyxia/hypoxia yielded a SMD of −0.72 (95 % CI −1.32 to 0.12); a meta-analysis of two studies of undefined asphyxia/hypoxia yielded an SMD of −0.26 (95 % CI −0.50 to 0.02). A meta-analysis of two studies of apnea yielded as SMD of 0.13 (95 % CI −0.19 to 0.45) (eFigure 2).
Discussion
The results of this meta-analysis show that the presence of proxies of impaired gas exchange in the neonate is strongly associated with increased risk of ID. Presence of these proxies in the neonate is also associated with increased risk of ASD but to a lesser extent. A number of systematic reviews on the association between prenatal complications and neurodevelopmental disorders have been published (Gardener et al. 2009, 2011; Bass et al. 2004). Our meta-analysis is the largest to date and is unique in three important ways. First, to the best of our knowledge, it is the first meta-analysis of the association between prenatal nonhereditary risk factors and ID. Second, it focuses on the proxies of impaired gas exchange as a means to assess possible hypoxic brain damage. And third, it provides us with insight about the differences between ID and ASD in their relation to neonatal altered gas exchange status.
With regard to ID, several inferences can be made from our findings. First, the direction of association between ID and proxies of impaired gas exchange was consistent across measures and studies. Second, the magnitude of association was particularly strong for proxies that are more reliable measures of impaired oxygenation such as acidosis or O2 treatment. Third, when cut-offs were available for an indicator (e.g. Apgar score), lower cut-off values were associated with larger estimates indicating a dose–response relationship. Low 5-min Apgar score often indicates poorer neonatal condition than low 1-min Apgar score. In our analysis, there was a stronger relation between low 5-min Apgar score and ID risk than low 1-min Apgar score and ID. Fourth, the association was robust to various analysis methods. Importantly, analyses of high quality studies, adjusted estimates, and population-based studies did not attenuate the results. Taken together, these findings are consistent with the assumption that neonatal exposure to impaired gas exchange might have detrimental effects on the brain with subsequent impairment in cognitive function (Bass et al. 2004).
With regard to ASD, the association between proxies of impaired gas exchange and ASD were qualitatively different. Associations were weaker, particularly for measures with more direct relation to impaired gas exchange, such as acidosis or O2 treatment. Furthermore, compared to meta-analyses of ID, there was little evidence of a dose–response relationship between proxies with cut-off score and ASD. It is important to note that a large proportion of patients with ASD also have some degree of ID (Baio 2012; Fombonne et al. 1997; Leonard et al. 2011; Oliveira et al. 2007; Wong and Hui 2008). This suggests that concomitant ID might account for the observed association between the gas exchange proxies and ASD. A recent study of the association between low Apgar score and ASD and/or ID has addressed this issue (Schieve et al. 2015). The authors found that ASD per se has a weak relation with low Apgar score, which increases to stronger association when ID accompanies ASD, and is strongest when ID happens without ASD. Another study showed that the association of resuscitation with ASD with ID is not different from that of ASD without ID (Langridge et al. 2013). Taken together, these findings suggest that the nature of the relation of ID accompanying ASD to impaired gas exchange is different from that of ID per se.
Our findings must be interpreted in the context of our study’s limitations. Our meta-analysis was based on observational studies. Therefore, although we found a strong, consistent association between proxies of impaired gas exchange and ID, our results cannot definitely attest to whether this association is causal (Weed 2000). However, given that it is impossible to conduct experimental studies of impaired gas exchange and neurodevelopmental outcomes in human, our meta-analysis provides the most rigorous synthesis of the current evidence. Moreover, meta-analysis, even at its best, only provides a rough solution to the problem of causality by addressing some of its aspects. For example, in the case of our meta-analysis there may be unknown factors that could account for the observed association. Unfortunately we were unable to assess the effect of sex as a potential effect modifier due to a small number of studies providing data. Sex-specific fetal programming can modify the brain’s vulnerability to prenatal stress and is therefore crucial to investigate in more depth in future studies (Mueller and Bale 2008).
Our meta-analysis could not verify the biological plausibility behind the association. However, evidence shows that neonatal brain tissue is extremely sensitive to hypoxic-ischemic damage (de Haan et al. 2006). Immaturity of the brain vasculature and autoregulation at birth, along with white matter vulnerability, contribute to brain injury following exposure to hypoxia/ischemia (Armstrong-Wells et al. 2010). In addition, hypoxic/ischemic insult induces inflammation, formation of free radicals and excitotoxicity, all of which can lead to exacerbation of neuronal damage and death (Armstrong-Wells et al. 2010; du Plessis and Volpe 2002). Regions that are involved in cognitive function, such as the hippocampus and cortex, are commonly injured following neonatal hypoxia (de Haan et al. 2006). Nevertheless, the detailed interplay between hypoxia and intellectual dysfunction has yet to be investigated.
Several other methodological considerations warrant further attention. We tried to minimize heterogeneity by separately analyzing various proxies. This approach resulted in meaningful reduction in heterogeneity compared with previous meta-analyses. For example, in their comprehensive meta-analysis of prenatal and perinatal risk factors for ASD, (Gardener et al. 2011) pooled apnea and respiratory distress together, which resulted in significant heterogeneity. We could significantly reduce the heterogeneity by analyzing these proxies separately. Nevertheless, heterogeneity due to variable design, definition of the conditions, and outcome measures was still an issue. Furthermore, even within a single measure, definitions could be different. This was particularly true for undefined hypoxia/asphyxia that in both ASD and ID were associated with significant heterogeneity. Furthermore, unclear definition of asphyxia/hypoxia makes it less useful than other proxies of impaired gas exchange. Another important limitation of our study was lack of more objective evidence of impaired gas exchange with the exception of a few studies that considered acidosis. At the same time however, the measures used represent real-world standard clinical practice and therefore they are both important and practical to study. Notably, these measures are not screening tools because most neonates with presence of these proxies do not develop disability, and most neonates with developmental disability have normal clinical course at the time of birth (Nelson and Ellenberg 1981).
Our study underscores the need for more thorough investigations into the role of altered gas exchange status in neurodevelopmental disorders. To increase the validity of these measurements, more direct measures of hypoxia/hypercarbia such as blood gas values and blood PH are needed. Neuroimaging studies can be particularly helpful in detecting functional and structural consequences of hypoxia/ischemia (Sie et al. 2000; Maneru et al. 2003). An important factor in our study was the definition of impaired gas exchange. Several other perinatal factors, from cord accidents and placental abnormalities to maternal disorders might be associated with hypoxia, acidemia, and hypercarbia in the neonate (Scafidi and Gallo 2008). We did not include all possible related measures because some of them were even less strongly related to asphyxia/hypoxia than currently used measures, making interpretation more difficult. Nevertheless, the measures that we included in our study have their own caveats. For example, low Apgar score can be a result of medications, infections, congenital anomalies, hypoxia and prematurity (Freeman and Nelson 1988), few of which were controlled for in the included studies. Apgar score of less than three might be a more valid measure of disturbed gas exchange status, but was unreported in most studies. Similarly, a need for O2 treatment might reflect some degree of hyperoxygentation and thus hyperoxic damage (Bancalari and Claure 2012; Casey et al. 2001).
In summary, our results show that presence of proxies of impaired gas exchange is associated with higher risk of ID. Moreover, our findings suggest that the ASD has a weak association with clinical proxies of impaired gas exchange. Future studies might focus on more objective measures of impaired gas exchange such as blood gas values and placental pathology as well as the effect of important modifiers such as sex and severity on the association between hypoxia/asphyxia and neurodevelopmental outcomes.
References
Akesson, H. O. (1966). Condition at birth and mental deficiency. Acta Genetica et Statistica Medica, 16(3), 283–304.
American Academy of Pediatrics. (2006). The APGAR score. Advances in Neonatal Care, 6(4), 220–223.
Apgar, V. (1953). A proposal for a new method of evaluation of the newborn infant. Current Researches in Anesthesia & Analgesia, 32(4), 260–267.
Armstrong-Wells, J., Bernard, T. J., Boada, R., & Manco-Johnson, M. (2010). Neurocognitive outcomes following neonatal encephalopathy. NeuroRehabilitation, 26(1), 27–33. doi:10.3233/NRE-2010-0533.
Atladottir, H. O., Schendel, D. E., Parner, E. T., & Henriksen, T. B. (2015). A descriptive study on the neonatal morbidity profile of autism spectrum disorders, including a comparison with other neurodevelopmental disorders. Journal of Autism and Developmental Disorders,. doi:10.1007/s10803-015-2408-7.
Baio, J. (2012). Prevalence of autism spectrum disorders: Autism and developmental disabilities monitoring network, 14 Sites, United States, 2008. Morbidity and Mortality Weekly Report. Surveillance Summaries. Vol. 61, Number 3. Centers for Disease Control and Prevention.
Bancalari, E., & Claure, N. (2012). Control of oxygenation during mechanical ventilation in the premature infant. Clinics in Perinatology, 39(3), 563–572. doi:10.1016/j.clp.2012.06.013.
Bass, J. L., Corwin, M., Gozal, D., Moore, C., Nishida, H., Parker, S., et al. (2004). The effect of chronic or intermittent hypoxia on cognition in childhood: A review of the evidence. Pediatrics, 114(3), 805–816. doi:10.1542/peds.2004-0227.
Benaron, H., Tucker, B., Andrews, J., Boshes, B., Cohen, J., Fromm, E., et al. (1960). Effect of anoxia during labor and immediately after birth on the subsequent development of the child. American Journal of Obstetrics and Gynecology, 80(6), 1129–1142.
Bilder, D. A., Pinborough-Zimmerman, J., Bakian, A. V., Miller, J. S., Dorius, J. T., Nangle, B., et al. (2013). Prenatal and perinatal factors associated with intellectual disability. American Journal on Intellectual and Developmental Disabilities, 118(2), 156–176. doi:10.1352/1944-7558-118.2.156.
Bilder, D., Pinborough-Zimmerman, J., Miller, J., & McMahon, W. (2009). Prenatal, perinatal, and neonatal factors associated with autism spectrum disorders. Pediatrics, 123(5), 1293–1300. doi:10.1542/peds.2008-0927.
Buchmayer, S., Johansson, S., Johansson, A., Hultman, C. M., Sparen, P., & Cnattingius, S. (2009). Can association between preterm birth and autism be explained by maternal or neonatal morbidity? Pediatrics, 124(5), e817–e825. doi:10.1542/peds.2008-3582.
Burd, L., Severud, R., Kerbeshian, J., & Klug, M. G. (1999). Prenatal and perinatal risk factors for autism. Journal of Perinatal Medicine, 27(6), 441–450. doi:10.1515/jpm.1999.059.
Burstyn, I., Sithole, F., & Zwaigenbaum, L. (2010). Autism spectrum disorders, maternal characteristics and obstetric complications among singletons born in Alberta, Canada. Chronic Diseases in Canada, 30(4), 125–134.
Burstyn, I., Wang, X., Yasui, Y., Sithole, F., & Zwaigenbaum, L. (2011). Autism spectrum disorders and fetal hypoxia in a population-based cohort: Accounting for missing exposures via Estimation-Maximization algorithm. BMC Medical Research Methodology, 11, 2. doi:10.1186/1471-2288-11-2.
Camp, B. W., Broman, S. H., Nichols, P. L., & Leff, M. (1998). Maternal and neonatal risk factors for mental retardation: defining the ‘at-risk’ child. Early Human Development, 50(2), 159–173.
Campbell, W. A., Cheeseman, E. A., & Kilpatrick, A. W. (1950). The effects of neonatal asphyxia on physical and mental development. Archives of Disease in Childhood, 25(124), 351–359.
Cans, C., Wilhelm, L., Baille, M. F., du Mazaubrun, C., Grandjean, H., & Rumeau-Rouquette, C. (1999). Aetiological findings and associated factors in children with severe mental retardation. Developmental Medicine and Child Neurology, 41(4), 233–239.
Casey, B. M., McIntire, D. D., & Leveno, K. J. (2001). The continuing value of the Apgar score for the assessment of newborn infants. New England Journal of Medicine, 344(7), 467–471. doi:10.1056/NEJM200102153440701.
Cassimos, D. C., Syriopoulou-Delli, C. K., Tripsianis, G. I., & Tsikoulas, I. (2015). Perinatal and parental risk factors in an epidemiological study of children with autism spectrum disorder. International Journal of Developmental Disabilities, 2047387715Y, 0000000004.
Chapman, D. A., Scott, K. G., & Stanton-Chapman, T. L. (2008). Public health approach to the study of mental retardation. American Journal of Mental Retardation, 113(4), 278–291. doi:10.1352/0895-8017(2008)113[102:PHATTS]2.0.CO;2.
Comi, A. M., Zimmerman, A. W., Frye, V. H., Law, P. A., & Peeden, J. N. (1999). Familial clustering of autoimmune disorders and evaluation of medical risk factors in autism. Journal of Child Neurology, 14(6), 388–394.
Corah, N. L., Anthony, E. J., Painter, P., Stern, J. A., & Thurston, D. L. (1965). Effects of perinatal anoxia after seven years. Psychological Monographs: General and Applied, 79(3), 1.
Darke, R. A. (1944). Late effects of severe asphyxia neonatorum: A preliminary report. The Journal of Pediatrics, 24(2), 148–158.
de Haan, M., Wyatt, J. S., Roth, S., Vargha-Khadem, F., Gadian, D., & Mishkin, M. (2006). Brain and cognitive-behavioural development after asphyxia at term birth. Developmental Science, 9(4), 350–358. doi:10.1111/j.1467-7687.2006.00499.x.
Deykin, E. Y., & MacMahon, B. (1980). Pregnancy, delivery, and neonatal complications among autistic children. American Journal of Diseases of Children, 134(9), 860–864.
Dodds, L., Fell, D. B., Shea, S., Armson, B. A., Allen, A. C., & Bryson, S. (2011). The role of prenatal, obstetric and neonatal factors in the development of autism. Journal of Autism and Developmental Disorders, 41(7), 891–902. doi:10.1007/s10803-010-1114-8.
Drage, J. S., Berendes, H. W., & Fisher, P. D. (1969). The Apgar scores and four-year psychological examination performance. Perinatal Factors Affecting Human Development, 185, 222–227.
du Plessis, A. J., & Volpe, J. J. (2002). Perinatal brain injury in the preterm and term newborn. Current Opinion in Neurology, 15(2), 151–157.
Duan, G., Yao, M., Ma, Y., & Zhang, W. (2014). Perinatal and background risk factors for childhood autism in central China. Psychiatry Research, 220(1–2), 410–417. doi:10.1016/j.psychres.2014.05.057.
Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463.
Dweck, H. S., Huggins, W., Dorman, L. P., Saxon, S. A., Benton, J. W, Jr, & Cassady, G. (1974). Developmental sequelae in infants having suffered severe perinatal asphyxia. American Journal of Obstetrics and Gynecology, 119(6), 811–815.
Ehrenstein, V., Pedersen, L., Grijota, M., Nielsen, G. L., Rothman, K. J., & Sorensen, H. T. (2009). Association of Apgar score at five minutes with long-term neurologic disability and cognitive function in a prevalence study of Danish conscripts. BMC Pregnancy Childbirth, 9, 14. doi:10.1186/1471-2393-9-14.
Finegan, J. A., & Quarrington, B. (1979). Pre-, peri-, and neonatal factors and infantile autism. Journal of Child Psychology and Psychiatry, 20(2), 119–128.
Fisch, R. O., Bilek, M. K., Miller, L. D., & Engel, R. R. (1975). Physical and mental status at 4 years of age of survivors of the respiratory distress syndrome. Follow-up report from the collaborative study. Journal of Pediatrics, 86(4), 497–503.
Fombonne, E., Du Mazaubrun, C., Cans, C., & Grandjean, H. (1997). Autism and associated medical disorders in a French epidemiological survey. Journal of the American Academy of Child and Adolescent Psychiatry, 36(11), 1561–1569. doi:10.1016/S0890-8567(09)66566-7.
Freeman, J. M., & Nelson, K. B. (1988). Intrapartum asphyxia and cerebral palsy. Pediatrics, 82(2), 240–249.
Froehlich-Santino, W., Londono Tobon, A., Cleveland, S., Torres, A., Phillips, J., Cohen, B., et al. (2014). Prenatal and perinatal risk factors in a twin study of autism spectrum disorders. Journal of Psychiatric Research, 54, 100–108. doi:10.1016/j.jpsychires.2014.03.019.
Gardener, H., Spiegelman, D., & Buka, S. L. (2009). Prenatal risk factors for autism: comprehensive meta-analysis. British Journal of Psychiatry, 195(1), 7–14. doi:10.1192/bjp.bp.108.051672.
Gardener, H., Spiegelman, D., & Buka, S. L. (2011). Perinatal and neonatal risk factors for autism: a comprehensive meta-analysis. Pediatrics, 128(2), 344–355. doi:10.1542/peds.2010-1036.
Gillberg, C., Enerskog, I., & Johansson, S. E. (1990). Mental retardation in urban children: A population study of reduced optimality in the pre-, peri- and neonatal periods. Developmental Medicine and Child Neurology, 32(3), 230–237.
Gillberg, C., & Gillberg, I. C. (1983). Infantile autism: A total population study of reduced optimality in the pre-, peri-, and neonatal period. Journal of Autism and Developmental Disorders, 13(2), 153–166.
Glasson, E. J., Bower, C., Petterson, B., de Klerk, N., Chaney, G., & Hallmayer, J. F. (2004). Perinatal factors and the development of autism: A population study. Archives of General Psychiatry, 61(6), 618–627. doi:10.1001/archpsyc.61.6.618.
Goldenberg, R. L., Huddleston, J. F., & Nelson, K. G. (1984). Apgar scores and umbilical arterial pH in preterm newborn infants. American Journal of Obstetrics and Gynecology, 149(6), 651–654.
Gonzalez, F. F., & Miller, S. P. (2006). Does perinatal asphyxia impair cognitive function without cerebral palsy? Archives of Disease in Childhood Fetal and Neonatal Edition, 91(6), F454–F459. doi:10.1136/adc.2005.092445.
Graham, F. K., Ernhart, C. B., & Thurston, D. (1962). The relationship of neonatal apnea to development at three years. Research Publications Association for Research in Nervous and Mental Disease, 39, 159–168.
Handley-Derry, M., Low, J. A., Burke, S. O., Waurick, M., Killen, H., & Derrick, E. J. (1997). Intrapartum fetal asphyxia and the occurrence of minor deficits in 4- to 8-year-old children. Developmental Medicine and Child Neurology, 39(8), 508–514.
Higgins, J. (2012). Green S. Cochrane handbook for systematic reviews of interventions Version 5.1. 0 (updated March 2011). The Cochrane Collaboration, 2011. www.cochrane-handbook.org.
Jonas, O., Roder, D., Esterman, A., Macharper, T., & Chan, A. (1989). Pregnancy and birth risk factors for intellectual disability in South Australia. European Journal of Epidemiology, 5(3), 322–327.
Kamper, J. (1978). Long term prognosis of infants with severe idiopathic respiratory distress syndrome. I. Neurological and mental outcome. Acta Paediatrica Scandinavica, 67(1), 61–69.
Kattwinkel, J., Perlman, J. M., Aziz, K., Colby, C., Fairchild, K., Gallagher, J., et al. (2010). Part 15: neonatal resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 122(18 Suppl 3), S909–S919. doi:10.1161/CIRCULATIONAHA.110.971119.
Khaiman, C., Onnuam, K., Photchanakaew, S., Chonchaiya, W., & Suphapeetiporn, K. (2015). Risk factors for autism spectrum disorder in the Thai population. European Journal of Pediatrics, 174(10), 1365–1372.
Lamont, M. A., & Dennis, N. R. (1988). Aetiology of mild mental retardation. Archives of Disease in Childhood, 63(9), 1032–1038.
Langridge, A. T., Glasson, E. J., Nassar, N., Jacoby, P., Pennell, C., Hagan, R., et al. (2013). Maternal conditions and perinatal characteristics associated with autism spectrum disorder and intellectual disability. PLoS One, 8(1), e50963. doi:10.1371/journal.pone.0050963.
Larsson, H. J., Eaton, W. W., Madsen, K. M., Vestergaard, M., Olesen, A. V., Agerbo, E., et al. (2005). Risk factors for autism: Perinatal factors, parental psychiatric history, and socioeconomic status. American Journal of Epidemiology, 161(10), 916–925. doi:10.1093/aje/kwi123. (discussion 926–918).
Lawlor, D. A., Najman, J. M., Batty, G. D., O’Callaghan, M. J., Williams, G. M., & Bor, W. (2006). Early life predictors of childhood intelligence: Findings from the Mater-University study of pregnancy and its outcomes. Paediatric and Perinatal Epidemiology, 20(2), 148–162. doi:10.1111/j.1365-3016.2006.00704.x.
Leonard, H., Glasson, E., Nassar, N., Whitehouse, A., Bebbington, A., Bourke, J., et al. (2011). Autism and intellectual disability are differentially related to sociodemographic background at birth. PLoS One, 6(3), e17875. doi:10.1371/journal.pone.0017875.
Lord, C., Mulloy, C., Wendelboe, M., & Schopler, E. (1991). Pre- and perinatal factors in high-functioning females and males with autism. Journal of Autism and Developmental Disorders, 21(2), 197–209.
Louhiala, P. (1995). Risk indicators of mental retardation: changes between 1967 and 1981. Developmental Medicine and Child Neurology, 37(7), 631–636.
Maimburg, R. D., & Vaeth, M. (2006). Perinatal risk factors and infantile autism. Acta Psychiatrica Scandinavica, 114(4), 257–264. doi:10.1111/j.1600-0447.2006.00805.x.
Mamidala, M. P., Polinedi, A., Praveen Kumar, T. V. P., Rajesh, N., Vallamkonda, O. R., Udani, V., et al. (2013). Prenatal, perinatal and neonatal risk factors of Autism Spectrum Disorder: A comprehensive epidemiological assessment from India. Research in developmental disabilities, 34(9), 3004–3013. doi:10.1016/j.ridd.2013.06.019.
Maneru, C., Serra-Grabulosa, J. M., Junque, C., Salgado-Pineda, P., Bargallo, N., Olondo, M., et al. (2003). Residual hippocampal atrophy in asphyxiated term neonates. Journal of Neuroimaging, 13(1), 68–74.
Maramara, L. A., He, W., & Ming, X. (2014). Pre- and perinatal risk factors for autism spectrum disorder in a New Jersey cohort. Journal of Child Neurology, 29(12), 1645–1651. doi:10.1177/0883073813512899.
Martinez-Biarge, M., Diez-Sebastian, J., Kapellou, O., Gindner, D., Allsop, J. M., Rutherford, M. A., et al. (2011). Predicting motor outcome and death in term hypoxic–ischemic encephalopathy. Neurology, 76(24), 2055–2061. doi:10.1212/WNL.0b013e31821f442d.
Mason-Brothers, A., Ritvo, E. R., Pingree, C., Petersen, P. B., Jenson, W. R., McMahon, W. M., et al. (1990). The UCLA-University of Utah epidemiologic survey of autism: Prenatal, perinatal, and postnatal factors. Pediatrics, 86(4), 514–519.
Mrozek-Budzyn, D., Majewska, R., & Kieltyka, A. (2013). Prenatal, perinatal and neonatal risk factors for autism: Study in Poland. Central European Journal of Medicine, 8(4), 424–430. doi:10.2478/s11536-013-0174-5.
Mueller, B. R., & Bale, T. L. (2008). Sex-specific programming of offspring emotionality after stress early in pregnancy. Journal of Neuroscience, 28(36), 9055–9065. doi:10.1523/JNEUROSCI.1424-08.2008.
Nath, S., Roy, R., & Mukherjee, S. (2012). Perinatal complications associated with autism: A case control study in a neurodevelopment and early intervention clinic. Journal of the Indian Medical Association, 110(8), 526–529.
Nelson, K. B., & Ellenberg, J. H. (1981). Apgar scores as predictors of chronic neurologic disability. Pediatrics, 68(1), 36–44.
Odd, D. E., Lewis, G., Whitelaw, A., & Gunnell, D. (2009). Resuscitation at birth and cognition at 8 years of age: A cohort study. Lancet, 373(9675), 1615–1622. doi:10.1016/s0140-6736(09)60244-0.
Oliveira, G., Ataide, A., Marques, C., Miguel, T. S., Coutinho, A. M., Mota-Vieira, L., et al. (2007). Epidemiology of autism spectrum disorder in Portugal: Prevalence, clinical characterization, and medical conditions. Developmental Medicine and Child Neurology, 49(10), 726–733. doi:10.1111/j.1469-8749.2007.00726.x.
Peters, J. L., Sutton, A. J., Jones, D. R., Abrams, K. R., & Rushton, L. (2006). Comparison of two methods to detect publication bias in meta-analysis. JAMA, 295(6), 676–680. doi:10.1001/jama.295.6.676.
Peters, J. L., Sutton, A. J., Jones, D. R., Abrams, K. R., & Rushton, L. (2007). Performance of the trim and fill method in the presence of publication bias and between-study heterogeneity. Statistics in Medicine, 26(25), 4544–4562. doi:10.1002/sim.2889.
Piven, J., Simon, J., Chase, G. A., Wzorek, M., Landa, R., Gayle, J., et al. (1993). The etiology of autism: pre-, peri- and neonatal factors. Journal of the American Academy of Child and Adolescent Psychiatry, 32(6), 1256–1263. doi:10.1097/00004583-199311000-00021.
Polo-Kantola, P., Lampi, K. M., Hinkka-Yli-Salomaki, S., Gissler, M., Brown, A. S., & Sourander, A. (2014). Obstetric risk factors and autism spectrum disorders in Finland. Journal of Pediatrics, 164(2), 358–365. doi:10.1016/j.jpeds.2013.09.044.
Rantakallio, P., & von Wendt, L. (1985). Risk factors for mental retardation. Archives of Disease in Childhood, 60(10), 946–952.
Robertson, C. M., & Finer, N. N. (1993). Long-term follow-up of term neonates with perinatal asphyxia. Clinics in Perinatology, 20(2), 483–500.
Scafidi, J., & Gallo, V. (2008). New concepts in perinatal hypoxia ischemia encephalopathy. Current Neurology and Neuroscience Reports, 8(2), 130–138.
Schieve, L. A., Clayton, H. B., Durkin, M. S., Wingate, M. S., & Drews-Botsch, C. (2015). Comparison of perinatal risk factors associated with autism spectrum disorder (ASD), intellectual disability (ID), and co-occurring ASD and ID. Journal of Autism and Developmental Disorders, 45(8), 2361–2372. doi:10.1007/s10803-015-2402-0.
Schreiber, F. (1943). Cerebral anoxia at birth as a cause of mental deficiency. Journal of Exceptional Children, 9, 227–230.
Seidman, D. S., Paz, I., Laor, A., Gale, R., Stevenson, D. K., & Danon, Y. L. (1991). Apgar scores and cognitive performance at 17 years of age. Obstetrics and Gynecology, 77(6), 875–878.
Sie, L. T., van der Knaap, M. S., Oosting, J., de Vries, L. S., Lafeber, H. N., & Valk, J. (2000). MR patterns of hypoxic–ischemic brain damage after prenatal, perinatal or postnatal asphyxia. Neuropediatrics, 31(3), 128–136. doi:10.1055/s-2000-7496.
Sonnander, K., & Gustavson, K. H. (1987). Reduced optimality as an indicator of developmental status at 18 months and school achievement at 8 years. Neuropediatrics, 18(3), 131–137. doi:10.1055/s-2008-1052465.
Steffenburg, S., Gillberg, C., Hellgren, L., Andersson, L., Gillberg, I. C., Jakobsson, G., et al. (1989). A twin study of autism in Denmark, Finland, Iceland, Norway and Sweden. Journal of Child Psychology and Psychiatry, 30(3), 405–416.
Stein, D., Weizman, A., Ring, A., & Barak, Y. (2006). Obstetric complications in individuals diagnosed with autism and in healthy controls. Comprehensive Psychiatry, 47(1), 69–75. doi:10.1016/j.comppsych.2005.01.001.
Stromme, P. (2000). Aetiology in severe and mild mental retardation: A population-based study of Norwegian children. Developmental Medicine and Child Neurology, 42(2), 76–86.
Stroup, D. F., Berlin, J. A., Morton, S. C., Olkin, I., Williamson, G. D., Rennie, D., et al. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA, 283(15), 2008–2012.
Sugie, Y., Sugie, H., Fukuda, T., & Ito, M. (2005). Neonatal factors in infants with Autistic Disorder and typically developing infants. Autism, 9(5), 487–494. doi:10.1177/1362361305057877.
Sussmann, J. E., McIntosh, A. M., Lawrie, S. M., & Johnstone, E. C. (2009). Obstetric complications and mild to moderate intellectual disability. British Journal of Psychiatry, 194(3), 224–228. doi:10.1192/bjp.bp.106.033134.
Taylor, D. J., Howie, P. W., Davidson, J., Davidson, D., & Drillien, C. M. (1985). Do pregnancy complications contribute to neurodevelopmental disability? Lancet, 1(8431), 713–716.
Thorngren-Jerneck, K., & Herbst, A. (2001). Low 5-minute Apgar score: A population-based register study of 1 million term births. Obstetrics and Gynecology, 98(1), 65–70.
Usdin, G. L., & Weil, M. L. (1952). Effect of apnea neonatorum on intellectual development. Pediatrics, 9(4), 387–394.
van Handel, M., Swaab, H., de Vries, L. S., & Jongmans, M. J. (2007). Long-term cognitive and behavioral consequences of neonatal encephalopathy following perinatal asphyxia: A review. European Journal of Pediatrics, 166(7), 645–654. doi:10.1007/s00431-007-0437-8.
Victory, R., Penava, D., Da Silva, O., Natale, R., & Richardson, B. (2004). Umbilical cord pH and base excess values in relation to adverse outcome events for infants delivering at term. American Journal of Obstetrics and Gynecology, 191(6), 2021–2028. doi:10.1016/j.ajog.2004.04.026.
Visser, J. C., Rommelse, N., Vink, L., Schrieken, M., Oosterling, I. J., van der Gaag, R. J., et al. (2013). Narrowly versus broadly defined autism spectrum disorders: Differences in pre- and perinatal risk factors. Journal of Autism and Developmental Disorders, 43(7), 1505–1516. doi:10.1007/s10803-012-1678-6.
von Wendt, L., & Rantakallio, P. (1987). Mild mental retardation in northern Finland. Upsala Journal of Medical Sciences, Suppl 44, 47–51.
Watterberg, K. L., Aucott, S., Benitz, W. E., Cummings, J. J., Eichenwald, E. C., Goldsmith, J., et al. (2015). The Apgar Score. Pediatrics, 136(4), 819–822. doi:10.1542/peds.2015-2651.
Weed, D. L. (2000). Interpreting epidemiological evidence: How meta-analysis and causal inference methods are related. International Journal of Epidemiology, 29(3), 387–390.
Wells, G. A., Shea, B., O’Connell, D., et al. (2011). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, ON: Ottawa Hospital Research Institute. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 5 Aug 2015.
Williams, K., Helmer, M., Duncan, G. W., Peat, J. K., & Mellis, C. M. (2008). Perinatal and maternal risk factors for autism spectrum disorders in New South Wales, Australia. Child: Care, Health and Development, 34(2), 249–256. doi:10.1111/j.1365-2214.2007.00796.x.
Wong, V. C., & Hui, S. L. (2008). Epidemiological study of autism spectrum disorder in China. Journal of Child Neurology, 23(1), 67–72. doi:10.1177/0883073807308702.
Zhang, X., Lv, C. C., Tian, J., Miao, R. J., Xi, W., Hertz-Picciotto, I., et al. (2010). Prenatal and perinatal risk factors for autism in China. Journal of Autism and Developmental Disorders, 40(11), 1311–1321. doi:10.1007/s10803-010-0992-0.
Acknowledgments
This work was supported by the Seaver Foundation. AM is a Seaver Fellow.
Author Contributions
AM, AR, and PB developed the idea and drafted the protocol. AM and JM searched the literature, screened the studies and extracted the data. AM and AR conducted the analyses. PB provided statistical consultations. AM and JM wrote the first draft. All authors read, critically revised, and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Modabbernia, A., Mollon, J., Boffetta, P. et al. Impaired Gas Exchange at Birth and Risk of Intellectual Disability and Autism: A Meta-analysis. J Autism Dev Disord 46, 1847–1859 (2016). https://doi.org/10.1007/s10803-016-2717-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-016-2717-5