Abstract
We examined the stability of cognitive and adaptive behaviour standard scores in children with autism spectrum disorder (ASD) between diagnosis and school entry approximately age 6. IQ increased 18 points in 2-year-olds, 12 points in 3-year-olds, and 9 points in 4-year-olds (N = 281). Adaptive behaviour scores increased 4 points across age groups (N = 289). At school entry, 24 % of children met criteria for intellectual disability (cognitive and adaptive behaviour scores <70). No children with both scores ≥70 at diagnosis later met criteria for intellectual disability. Outcomes were more variable for children with initial delays in both areas (in 57 %, both scores remained <70). Findings are relevant to clinical decision-making, including specification of intellectual disability in young children with ASD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children with autism spectrum disorder (ASD) are often diagnosed during the preschool years. Best-practice early assessments include measures of cognitive development and adaptive behaviour, in addition to measures of autism symptoms (Johnson and Myers 2007; Goldstein et al. 2008). In school-aged children with ASD, standard scores on cognitive and adaptive measures are considered to provide meaningful prognostic information (Nordin and Gillberg 1998). Cognitive standard scores are often relatively stable in this age group (Eaves and Ho 1996; Sigman and McGovern 2005), whereas adaptive behaviour standard scores tend to decrease somewhat over time (Gabriels et al. 2007; Magiati et al. 2011).
In younger children with ASD, the stability of both cognitive and adaptive behaviour scores is less clear. In children with and without special needs, scores are often considered to be less predictive of later abilities when collected during the preschool years (Kamphaus 1993). Some authors have noted that the behavioural, social, and language difficulties associated with ASD may make scores especially unstable in this population (e.g., Rapin 2003). In addition, the irregular profile of skills associated with ASD (Joseph et al. 2002) may reduce score stability, as the skills tapped by cognitive and adaptive measures change significantly over the preschool period.
Previous studies exploring early cognitive stability in children with ASD have produced mixed results. In a seminal study with a relatively large sample, Lord and Schopler (1989a) found moderate increases between initial assessment and follow-up approximately 4 years later in 3 cohorts initially assessed at age 2–3 (mean gain 15 points), 4–5 (mean gain 12 points), and 6–7 (mean gain 11 points). Many children experienced large changes in IQ (12 % changed by 20 points or more) and a significant proportion moved either into or out of the intellectual disability range (approximately 25 % in each direction). More recent studies have typically reported either moderate gains in IQ over time (e.g., Eaves and Ho 2004; reported a 12-point gain in verbal IQ and 4-point gain in performance IQ), or stable mean scores (Dietz et al. 2007; Jónsdóttir et al. 2007; Stevens et al. 2000). However, Turner et al. (2006) reported a relatively large (23-point) mean gain in their sample of 2-year-olds re-assessed at age 9. Even in studies in which mean scores were relatively stable, individual scores have often been quite variable. For example, Dietz et al. (2007) found that approximately one-third of their sample of 2-year-olds with ASD gained at least 15 IQ points, and that large gains were more common in children with ASD than in either typically developing children or children with intellectual disabilities without ASD.
Gains in cognitive scores may be less likely in older preschoolers than in 2- to 3-year-olds (Lord and Schopler 1989a, b). In addition, gains may be less likely in children who initially have average cognitive skills or severe cognitive delays. For example, Jónsdóttir et al. (2007) found that individual scores were more stable in children with IQs greater than 70 or lower than 35 than in those with mild-moderate cognitive delays. In addition, Hedvall et al. (2014) found that skill level was more stable in children with average intellectual skills (IQ > 84; 69 % stayed in average range) or intellectual disability (IQ < 70; 88 % stayed in intellectual disability range) than in those with intermediate skills (IQ 70–84; 39 % stayed in borderline intellectual functioning range).
Even fewer studies have examined changes in adaptive behaviour standard scores over time in preschool children with ASD. Lord and Schopler (1989b) reported relative stability between preschool and school-age on the Vineland Social Maturity Scale (Doll 1965; non-significant decrease of 5 points, where the standard deviation is 15 points). Similarly, Eaves and Ho (2004) found a small decrease of 4 points between ages 2 and 4 using the 1984 version of the Vineland Adaptive Behavior Scales (VABS; Sparrow et al. 1984). In a recent study with a relatively large sample, Hedvall et al. (2014) found that skill level on the latest version of the VABS (VABS-II, Sparrow et al. 2005), classified as low, below average, average, above average, or high, remained the same for 67 % of children, moved to a higher level for 23 %, and moved to a lower level for 10 %. Trajectories differed across IQ groups, with scores increasing in children with average cognitive functioning and decreasing in all domains but communication in those with cognitive delays. In a paper related to this one (Szatmari et al. 2015), members of our research team used a semi-parametric, group-based modelling approach to characterize developmental trajectories of adaptive behaviour standard scores in preschool children. We found three distinct trajectory groups: a lower functioning group with a worsening trajectory (29 % of sample), a moderately functioning group with a stable trajectory (50 % of sample) and a higher functioning group with an improving trajectory (21 % of sample). Earlier age at diagnosis, higher baseline IQ, and higher baseline language scores increased the likelihood of membership in the latter two groups.
Cognitive and adaptive behaviour scores are significantly correlated in samples with ASD (Kanne et al. 2011; Perry et al. 2009; Ray-Subramanian et al. 2011). In previous studies using the VABS or the VABS-II, mean cognitive scores were often higher than mean adaptive behaviour scores in those with average or borderline IQ, and lower than mean adaptive behaviour scores in those with cognitive delays (Kanne et al. 2011; Perry et al. 2009). This pattern was also recently reported in preschool children assessed with the Adaptive Behavior Assessment System-II (Rivard et al. 2015).
Many studies of cognitive and adaptive behaviour scores in young children with ASD have been limited by relatively small samples. In addition, new measures of cognitive and adaptive behaviour may affect the stability of scores (e.g., increased coverage of early adaptive behaviour on the VABS-II, Sparrow et al. 2005; updated cognitive batteries tapping a wider range of skills across the preschool period, Roid and Sampers 2004). Diagnostic practices are changing, as are autism interventions and access to treatment, and the developmental trajectories of current cohorts of preschoolers with ASD may differ from those of children born only a decade ago.
An understanding of the stability of early scores in children with ASD is important clinically, affecting decisions related to measure selection, feedback to families, access to public services, and treatment planning. The prognostic value of very low scores may be especially important, as these scores affect clinical decision-making about the presence of intellectual disability. The Diagnostic and Statistical Manual of Mental Disorders (DSM), Fifth Edition, notes that “appropriate assessment of intellectual functioning in ASD is essential” (American Psychiatric Association 2013, p. 40), and provides specifiers to distinguish between individuals on the autism spectrum with or without an accompanying intellectual impairment. To support clinical decision-making, additional research is needed on the stability of cognitive and adaptive behaviour scores at specific ages and skill levels during the preschool period.
Objectives
In this study, we characterized trajectories of cognitive and adaptive behaviour standard scores in a representative sample of preschoolers with ASD, from diagnosis to school entry. Our first objective was to determine the concurrent relationship between IQ and adaptive behaviour standard scores at different ages and cognitive levels. We hypothesized that IQ would be higher than adaptive behaviour in children without cognitive delays, but lower than adaptive behaviour in children with cognitive delays. Next, we examined the stability of adaptive behaviour standard scores over time, considering changes in mean scores, individual scores, and individual ability levels. We anticipated that adaptive behaviour scores would be relatively stable, but that slopes would be affected by cognitive level. Our third objective was to examine the stability of mean and individual IQ scores. We hypothesized that IQ would increase at least moderately over time, and that age and cognitive level would influence slopes. As clinicians often consider information from cognitive and adaptive behaviour measures concurrently when considering a child’s prognosis, our final objective was to determine the stability of overall ability level (combining cognitive and adaptive behaviour scores) between diagnosis and school entry. We anticipated that overall ability level would remain stable for most children, but that IQ gains would be associated with changes for some.
Method
Participants and Procedure
Participants were enrolled in an on-going longitudinal study examining developmental trajectories of children with ASD (Pathways in ASD study). For each analysis, subsamples were selected from a larger group of 369 Pathways in ASD study participants (83.7 % boys). Children were recruited through five regional ASD referral centres across Canada: Halifax, Montreal, Hamilton, Edmonton, and the Greater Vancouver/Fraser Valley regions of British Columbia. All families provided informed consent prior to participation, and local Research Ethics Boards approved the research protocol at each site.
To enrol in the Pathways in ASD study, children had to have a recent (i.e., within 4 months) clinical diagnosis of ASD, confirmed by the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2002), the Autism Diagnostic Interview-Revised (ADI-R; Rutter et al. 2003), and an expert clinician using DSM, Fourth Edition, Text Revision, criteria (American Psychiatric Association 2000). Mean autism symptom severity, as measured using the Social Responsiveness Scale (Constantino and Gruber 2002), fell at the high end of the moderate range (75.71, SD = 13.21). Additional inclusion criteria were as follows: chronological age between 2 years, 0 months and 5 years, 0 months; absence of cerebral palsy or other neuromotor disorders that would interfere with study assessments; and absence of known genetic or chromosomal abnormalities or severe visual or hearing impairment. To ensure independence of observations, only one child per family was recruited to the study.
Parents of most children were born in Canada, although 27 % of primary caregivers were born in one of 51 other countries. For 82 % of children, English was the primary language spoken at home. Estimated annual family income varied—with 26 % under $40,000CND, 37 % between $40,000 and $80,000CND, and 37 % at $80,000CND or more. Children also received a wide range of interventions prior to school entry. For example, at least 63 % received behavioural intervention (43 % for at least 11 h/week), at least 66 % received speech/language therapy, and at least 39 % received occupational/physical therapy (percentages may be higher as detailed information about services was missing at one or more time points for some children).
Information was drawn from three time points in the larger Pathways in ASD study. The first point was at or soon after diagnosis (2.72 months after diagnosis on average, SD = 2.45), at age 41.17 months (SD = 9.00). The second point was approximately 1 year later, at a mean age of 54.46 months (SD = 9.01). The third was at or near age 6 (M = 79.10 months; SD = 3.89). These time points are referred to as ‘diagnosis’, ‘one-year follow-up’, and ‘school entry’. Because children were diagnosed at different ages, the interval between one-year follow-up and school entry varied across children.
Testing typically took place in university clinics, hospitals, or research centres, with some assessments in children’s homes or childcare centres. Cognitive measures were administered as part of a larger assessment battery by trained and supervised psychometrists, graduate students, or research assistants. Adaptive behaviour was assessed through an interview with a primary caregiver either in person or by telephone. Although there was variability across sites, participants were often evaluated by the same individual across time points. Results from the five sites were compiled in a central database prior to analyses.
Measures
Cognitive Skills
At diagnosis and one-year follow-up, cognitive skills were determined using the Developmental Index of the Merrill-Palmer-Revised Scales of Development (M-P-R; Roid and Sampers 2004). The M-P-R Developmental Index was also used to index IQ for many children at school entry (N = 123). However, by school entry, many children were at the ceiling on the M-P-R. For these children, the Wechsler Preschool and Primary Scale of Intelligence—3rd edition (WPPSI-3; Wechsler 2002) was also administered, and that score was used (N = 139). By school entry, many children were also too old to obtain a valid standard score on the M-P-R. If a child was too old to obtain a valid standard score, but was not at the ceiling of the scale, a ratio IQ was derived (M-P-R developmental index age equivalent score divided by chronological age, multiplied by 100; N = 48). At all time points, if raw scores on the M-P-R were too low to obtain a valid standard score, a score one point lower than the lowest possible standard score for that child’s age was assigned (N = 42 at diagnosis, N = 47 at one-year follow-up; N = 57 at school entry). The above decisions reflect common practices when assessing school-aged children at varying skill levels (e.g., Eaves and Ho 2004; Jónsdóttir et al. 2007). For some analyses, children were grouped into one of three cognitive levels: no delay (IQ ≥ 70), mild-moderate delay (IQ 40-69), and severe delay (IQ < 40).
The M-P-R is a measure of cognitive development for children aged 24–78 months. It was designed to measure the following abilities outlined in the Cattell-Horn-Carroll theory of cognitive development: fluid reasoning, crystallized ability, short-term memory, speed of processing, and visualization (Roid and Sampers 2004). The Developmental Index (DI; in standardization sample, M = 100, SD = 15) combines information about non-verbal reasoning with information about receptive language and fine motor skills. The M-P-R differs from some cognitive batteries in that it does not include expressive language skills within the global intellectual ability scale. Scores on the M-P-R are strongly correlated with scores on other measures of intellectual ability, including the Bayley Scales of Infant Development (M-P-R DI correlates .92 with Bayley Mental Scale; Roid and Sampers 2004).
The Wechsler Preschool and Primary Scale of Intelligence—3rd edition (WPPSI-3; Wechsler 2002) is a widely used measure of cognitive skills designed for children aged 30–87 months. The Full Scale IQ (in standardization sample, M = 100, SD = 15) combines information about non-verbal skills with information about verbal skills (includes both receptive and expressive abilities) and processing speed. The WPPSI-3 has strong internal consistency and test–retest reliability (Wechsler 2002). The absolute floor of the WPPSI-3 is significantly higher than that of the M-P-R (e.g., 40 for Full Scale IQ in 4- to 7-year-olds, versus 10 for the M-P-R DI). In addition, Full Scale IQ scores on the WPPSI-3 were significantly lower than DI scores on the M-P-R in a relatively high functioning sub-sample of 65 children in this study for whom those scores were available on both measures (completed both measures because a ceiling on the M-P-R was not obtained, as described previously: 90.14 (12.65) versus 97.74 (10.76), t (64) = 6.80, p < .001).
Adaptive Behaviour
Adaptive behaviour was assessed using the Vineland Adaptive Behavior Scales, Second Edition- Survey Edition (VABS-II; Sparrow et al. 2005). The VABS-II is a measure of adaptive behaviour designed for infants, children and adults. It captures information about a range of adaptive behaviour skills, including communication, socialization, daily living skills, and motor skills. Scores across domains are combined to produce an overall Adaptive Behavior Composite (ABC) score (in standardization sample, M = 100, SD = 15). Research staff administered the VABS-II by carrying out a semi-structured interview with a primary caregiver (usually mother), either in person or by telephone. The VABS-II has been shown to have adequate reliability and validity (Sparrow et al. 2005), and the validity of telephone administration has been established (Limperopoulos et al. 2006). For some analyses, children were grouped into one of two adaptive functioning levels: no delay (initial standard score ≥ 70), mild-moderate delay (initial standard score 40–69; there were no scores < 40).
Analyses
To explore differences between IQ and adaptive behaviour standard scores at specific ages and skill levels, we carried out a 3-way repeated measures ANOVA with measure (IQ or adaptive behaviour score) as the within-subjects variable and age cohort at diagnosis (age 2, 3, or 4 years) and cognitive level (severe delay, mild-moderate delay, or no delay) as the between-subjects variables. This was followed by separate repeated measures ANOVAs within each specific age group (age 2, 3, 4, and 6 years), as well as post hoc paired-sample t-tests.
A similar approach was used to explore trajectories of IQ and adaptive behaviour. Two separate 3-way repeated measures ANOVAs were carried out for each outcome, with time (diagnosis, one-year follow up, or school entry) as the within-subjects variable, and age cohort (age 2, 3, or 4 years) and cognitive level (severe delay, mild-moderate delay, or no delay) as the between-subjects variables. Degrees of freedom were corrected using the Huynh–Feldt estimates of sphericity. When scores on a measure changed significantly over time, repeated within-subjects contrasts were carried out to determine at which time point change took place. Individual change in IQ and adaptive behaviour standard scores between diagnosis and school entry were explored by determining the percentage of children whose scores changed by one, two, or three standard deviations, and by calculating the percentage of children who experienced a change in ability level (severe delay, mild-moderate delay, no delay).
Missing Data
For each analysis, some children from the Pathways in ASD dataset were excluded due to missing data. In all analyses, included children did not differ from excluded children with respect to age, autism severity, or adaptive behaviour at diagnosis (all p ≥ .17). Similarly, included children did not differ from excluded children with respect to IQ at diagnosis when exploring stability of IQ (p = .57 for mean scores, p = .17 for individual scores) or concurrent relationships between IQ and adaptive behaviour (p = .11 at diagnosis, p = .14 at school entry). However, for analyses exploring stability of adaptive functioning and overall level, included children had higher IQ at diagnosis than excluded children: t [352] = 2.15, p = .03 for mean change in adaptive behaviour scores, t [352] = 2.11, p = .04 for individual change in adaptive behaviour scores, t (352) = 2.32, p = .02 for individual change in overall level.
Results
Concurrent Relationships Between IQ and Adaptive Behaviour Standard Scores Across Age of Diagnosis and Cognitive Level
Our first objective was to determine the concurrent relations between IQ and adaptive behaviour at diagnosis (age 2, 3, or 4) and at school entry (at or near age 6). To be included in the analyses, both cognitive and adaptive measures had to be available and the two types of measure had to be administered within 6 months of each other (N = 357, with N = 323 at diagnosis and N = 299 at school entry). For included children, mean time between the administration of cognitive and adaptive measures was <2 weeks: .37 (1.38) months at diagnosis, .18 (1.16) months at school entry. IQ and adaptive functioning were moderately correlated at age 2 (0.56) and strongly correlated at ages 3, 4, and 6 (0.72–0.79). Correlations were stronger in 3-, 4- and 6-year-olds than in 2-year-olds (based on Fisher’s r-to-z transformation, p ≤ .04 across comparisons). Within specific cognitive levels at specific ages, correlations varied greatly (e.g., no correlation in 2-year-olds with mild-moderate or no cognitive delay, strong correlation in 4-year-olds with severe cognitive delay; see Table 1).
Table 1 shows mean IQ and adaptive behaviour scores at diagnosis (age 2, 3, or 4) and at school entry (at or near age 6). An overall repeated measures ANOVA showed a significant interaction between measure type, age, and cognitive level, F(4, 314) = 9.20, p < .001. Within each age group, cognitive level influenced the relationship between IQ and adaptive functioning: F(2, 112) = 145.70, p ≤ .001 at age 2, F(2, 139) = 249.14, p < .001 at age 3, F(2, 63) = 189.59, p < .001 at age 4, F(2, 296) = 506.17, p < .001 at age 6. In children without cognitive delays, adaptive behaviour scores were typically lower than IQ scores (however, no significant difference in 2-year-olds). In contrast, in children with cognitive delays (mild-moderate or severe), adaptive behaviour was consistently higher than IQ (all p ≤ .001). Differences between cognitive and adaptive scores were often very large (e.g., 48-point mean difference in 2-year-olds with severe cognitive delays).
Stability of Adaptive Behaviour Standard Scores
Our second objective was to characterize change and stability of adaptive behaviour standard scores from diagnosis to school entry; N = 289 when analyzing mean scores; N = 301 when analyzing individual scores. Age at diagnosis (2, 3, 4) and skill level (no cognitive delay, mild-moderate cognitive delay, severe cognitive delay) were considered in analyses.
Mean Scores
Adaptive behaviour standard scores increased significantly over time, from a mean score of 73.15 (SD = 10.06) to a mean score of 76.85 (SD = 14.24), F(1.91, 535.16) = 38.06, p < .001. Figure 1 displays changes in adaptive behaviour for different age groups at different cognitive levels. Slopes did not differ for different age cohorts, F(3.82, 535.16) = 1.13, p = .34. However, cognitive level did influence slopes, F(3.82, 535.16) = 3.40, p = .01.
In the no congitive delay and mild-moderate congitive delay groups, scores increased between diagnosis and one-year follow-up, F(1, 82) = 54.18, p < .001 and F(1, 103) = 21.84, p < .001, and did not change significantly between one-year follow-up and school entry, F(1, 82) = 1.39, p = .24 and F(1, 103) = .05, p = .82. Scores did not increase significantly for the severe delay group as a whole, F(1.71, 162.50) = 3.10, p = .06. However, there was a significant interaction between slope and age, F(3.42, 162.50) = 3.02, p = .03 and 4-year olds with severe delays did experience gains, F(1.30, 18.19) = 11.25, p = .002.
Individual Scores
Adaptive behaviour standard scores were relatively stable for most children (see Table 2). Scores increased by one or more standard deviation for approximately 15 % of 2- and 3-year-olds, and 9 % of 4-year-olds. Adaptive behaviour scores decreased by atleast 15 points for 11 % of 2-year-olds but decreases were very rare in older children.
Changes in adaptive functioning level (mild-moderate delay, ABC = 40–69; no delay, ABC ≥ 70) between diagnosis and school entry were also explored (no scores fell in the severe delay range). As shown in Fig. 2, most children with no adaptive behaviour delay at diagnosis had no delay at school entry. However, forty percent of children with adaptive behaviour delays at diagnosis moved to the no delay range.
Stability of IQ Scores
Our third objective was to examine the stability of IQ scores from diagnosis to school entry (N = 281 when analyzing mean scores; N = 299 when analyzing individual scores). Similar to analyses for adaptive behaviour, differences in age cohort (diagnosed at age 2, 3, or 4) and initial cognitive level (no cognitive delay, mild-moderate cognitive delay, severe cognitive delay) were considered.
Mean Scores
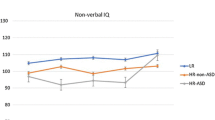
IQ increased significantly over time, from a mean score of 51.32 (SD = 28.40) to a mean score of 64.74 (SD = 34.34), F(1.89, 510.82) = 57.92, p < .001. Figure 3 shows slopes for different age groups at different cognitive levels. IQ slopes differed across the three age cohorts, F(3.76, 510.82) = 3.83, p = .01. In all age cohorts, scores increased significantly between diagnosis and school entry: 2-year-olds gained 18 IQ points on average, F(1.81, 157.61) = 22.66, p < .001, 3-year-olds gained 12 IQ points on average, F(1.83, 213.83) = 23.35, p < .001), and 4-year-olds gained 9 IQ points on average, F(2.00, 136.00) = 21.15, p < .001. The impact of skill level at diagnosis on IQ slopes varied in the three age cohorts, F(7.51, 510.82) = 3.47, p = .001.
In 2-year-olds, skill level did not significantly affect slope, F(3.62, 157.61) = 0.83, p = .50. Across skill levels, there were gains between diagnosis and one-year follow-up, F(1, 87) = 14.43, p < .001, and between one-year follow-up and school entry, F(1, 87) = 13.39, p < .001. In 3-year-olds, slopes also did not differ across cognitive groups, F(3.66, 213.83) = 2.07, p = .09. Scores increased between diagnosis and one-year follow-up, F(1, 117) = 43.78, p < .001), and did not change significantly between one-year follow-up and school entry, F(1, 117) = .059, p = .81. For those diagnosed at age 4, slopes did differ across cognitive groups, F(4.00, 136.00) = 10.06, p < .001. In 4-year-olds with severe delays, IQ improved between diagnosis and one-year follow-up, F (1, 23) = 8.21, p = .01, and there was a trend towards improvement between one-year follow-up and school entry, F(1, 23) = 4.12, p = .05. In 4-year-olds with mild-moderate delays, IQ increased in the year following diagnosis, F(1, 16) = 33.70, p < .001, and did not change between one-year follow-up and school entry, F(1, 16) = 0.491, p = .49. Lastly, in 4-year-olds without cognitive delays, there was no significant change in IQ in the year following diagnosis, F(1, 29) = 2.37, p = .14) and a decrease in IQ between one-year follow-up and school entry, F(1, 29) = 20.05, p < .001.
Individual Scores
Individual changes in IQ between diagnosis and school entry were also calculated (see Table 3). Scores increased by at least one standard deviation for approximately half of 2- and 3-year-olds, and approximately one-third of 4-year-olds. Many children experienced a gain of 30 points or more. Significant decreases in individual scores (by one or more standard deviations) took place for 12–14 % of each cohort.
Changes in cognitive level (severe delay, IQ < 40; mild-moderate delay, IQ 40–69; or no delay, IQ ≥ 70) between diagnosis and school entry were also explored. As shown in Fig. 4, scores were relatively evenly divided among the three cognitive levels at diagnosis. IQ range was very stable for children who initially scored in the no delay range (95 % remained in the no delay range). Range was also relatively stable for the severe delay group (56 % remained in the severe delay range; notably, however, 30 % moved to the no delay range). The IQ range was much less stable for the mild-moderate delay group (19 % remained in the mild-moderate delay range), with most children moving to the no delay range.
Stability of Overall Ability Level
Our final goal was to explore the stability of overall ability level between diagnosis and school entry, combining information from cognitive and adaptive behaviour measures (N = 263). At diagnosis, 33 % of the overall sample had delays in both cognitive skills and adaptive functioning (both scores <70; See Fig. 5). By school entry, 24 % of the sample met this criterion. No children who scored in the no delay range on both cognitive and adaptive behaviour measures at diagnosis had delays in both areas at school entry (3 % had delays in one area). Most children who had both a cognitive and adaptive delay at diagnosis remained delayed in at least one area (57 % remained delayed in both; 22 % moved to the no delay range). Overall ability level often improved for children who initially had delays in one area: 68 % had no delay at school entry, although outcomes were variable.
Discussion
We examined trajectories of cognitive and adaptive behaviour standard scores between diagnosis and school entry in young newly diagnosed children with ASD. The sample was relatively large and representative of the spectrum of clinically identified preschoolers. First, we examined the concurrent relationship between IQ and adaptive behaviour standard scores. Consistent with previous research (e.g., Kanne et al. 2011; Ray-Subramanian et al. 2011), adaptive behaviour and IQ were moderately to strongly correlated. Correlations were stronger in 3-, 4- and 6- year olds than in 2-year-olds. Within the sub-samples of 2-year olds with mild-moderate and no cognitive delay, there was no correlation between cognitive and adaptive functioning. Similar to previous studies (Kanne et al. 2011; Perry et al. 2009; Rivard et al. 2015), the relations between IQ and adaptive behaviour differed in children with and without cognitive delays. In children without cognitive delays, adaptive behaviour was typically lower than IQ (in 3-, 4- and 6-year-olds; no difference in 2-year-olds). However, in children with cognitive delays, adaptive behaviour was significantly higher than IQ. The difference between cognitive and adaptive scores in children with severe delays was very large (40–49 points). This may reflect a true underlying relative strength in adaptive functioning for some children with severe cognitive delays (e.g., the ability to learn routine skills despite significant cognitive limitations). However, it is likely also influenced, at least in part, by the psychometric properties of the measures used to assess adaptive behaviour and IQ. Although adaptive behaviour scores as low as 20 are possible on the VABS-II for preschool children, no children in our large, representative sample obtained a score under 40. This is similar to findings by Kanne et al. (2011) in a very large sample of 4- to 17- year-old verbal individuals with ASD (i.e., scatterplots suggest no scores under 40), and may call into question the true floor of the scale. In contrast, the absolute floor of the M-P-R DI for preschool children is 10, and many children scored at the floor.
These results highlight the importance of assessing both cognitive skills and adaptive functioning when estimating skill level in children with ASD. Although mean scores in the two areas were often similar, there were large differences for some subgroups, especially those with severe cognitive delays. Our results also emphasize the importance of considering age and developmental level when describing ability profiles in children with ASD. Higher functioning children may have significant challenges with everyday skills relative to their cognitive abilities, and require specialized educational supports despite having average IQ scores. In contrast, adaptive behaviour can be a relative strength for those with cognitive delays, and there may be value in focusing on the acquisition of functional skills, especially in individuals with very low IQ.
Adaptive behaviour standard scores were relatively stable over time. Whereas studies using older versions of the VABS have typically found no significant mean change in scores for young children (Lord and Schopler 1989b), or slight decreases (Eaves and Ho 2004), we found small increases following diagnosis using the VABS-II (4- point overall gain). As in other studies (Hedvall et al. 2014; Szatmari et al. 2015), cognitive level influenced adaptive behaviour trajectories. Similar to Hedvall et al. (2014), preschoolers without cognitive delays experienced gains on the VABS-II. However, Hedvall et al. (2014) found decreases for children with cognitive delays that were not replicated here. Also similar to findings by Hedvall et al. (2014), individual scores were relatively stable: scores changed by less than one standard deviation for 75–91 % of children in each age cohort, and range was stable for 60 % of children with initial delays, and 87 % of children without initial delays. See Szatmari et al. (2015) for additional information about developmental trajectories of adaptive functioning in the Pathways in ASD sample. Gains in adaptive behaviour scores took place in the year following diagnosis, as opposed to between 1-year follow-up and school entry. This may be a period of greater growth in adaptive skills. However, gains may also be an artifact of repeated interviewing using the same measure (e.g., between the first and second administration of the VABS-II, parents’ accuracy in describing their children’s abilities may improve).
The relative stability of adaptive behavior scores is meaningful clinically. It is important to assess adaptive behaviour at diagnosis, as scores may be relatively predictive of adaptive behaviour scores at school entry. Adaptive behaviour measures may be more consistent than cognitive measures across the preschool period because they capture information about everyday skills with familiar people, and are not limited by poor test-taking skills that may impair performance on early cognitive tests. Although relatively stable, adaptive scores may be inflated in some groups. As noted previously, adaptive scores were often much higher than cognitive scores in those with significant cognitive delays. In school-aged children with ASD, scores on earlier versions of the VABS appear to decrease with age (Gabriels et al. 2007; Magiati et al. 2011). Thus, it will be important to determine whether very early scores on the VABS-II continue to predict adaptive behaviour beyond age 6, especially for lower-functioning children.
Consistent with some previous research involving young children (Lord and Schopler 1989a; Turner et al. 2006), mean IQ scores increased significantly over time. Two-year-olds gained 18 IQ points on average (comparable to the 23-point gain reported by Turner et al. 2006), and more than half gained at least 15 points. Three-year-olds gained 12 IQ points on average, and nearly half gained at least 15 points. Mean scores also improved in 4-year-olds (gain of 9 points), and approximately one-third gained at least 15 points. In 4-year-olds without cognitive delays, there was a small decrease in IQ between one-year follow-up and school entry. This decrease was perhaps due to a change in measures, as opposed to a loss of skills (77 % of this sub-sample moved from the M-P-R to the WPPSI-3). Recall that scores on the WPPSI-3 were significantly lower than scores on the M-P-R at school entry in a subsample of children who completed both measures (see “Measures”).
Age and skill level influenced cognitive trajectories. Our results are consistent with those of Lord and Schopler’s (1989b), who found that gains are more likely in 2- to 3-year-olds than in older preschoolers. In addition, as reported by Jónsdóttir et al. (2007), changes in cognitive level were more likely in children with mild-moderate delays (19 % stayed in mild-moderate delay range), than in children with no cognitive delay (95 % stayed in no delay range) or severe cognitive delays (56 % stayed in severe delay range). Unlike most previous research, children in this study were assessed at multiple time points by the same teams, allowing for a greater understanding of when changes in cognitive scores take place. Gains typically took place in the year following diagnosis, with 2-year olds alone continuing to experience gains between one-year follow-up and school entry.
In higher-functioning children in all age groups, the transition from the M-P-R to the WPPSI-3 may have affected IQ stability. Changes from the M-P-R to the WPPSI are unlikely to have inflated gains over time, as scores on the WPPSI were lower than scores on the M-P-R in a subset who completed both measures. As in other studies that explored change over time between preschool and school age (Eaves and Ho 2004; Jónsdóttir et al. 2007), we were unable to get a valid standard score for all children on the same measure across all time points. Although different measures were used for some children at diagnosis and school entry, this reflects common clinical practice in the assessment of children with ASD, due to lack of measures that span wide age ranges and skill levels. Thus, our findings should link closely to findings in clinical settings.
Cognitive score gains could be due to a number of variables. True gains in underlying cognitive abilities (e.g., reasoning, problem solving) may occur during the preschool period in children with ASD. In addition, children with ASD often make significant language gains in the preschool-years, and these gains could influence cognitive trajectories. Gains may also reflect improved test-taking skills, such as reductions in disruptive behaviour, increases in motivation to attend and respond to unfamiliar adults, and gains in specific skills relevant to cognitive assessment (e.g., the ability to attend or to point). Gains in cognitive, language, and test-taking skills could also be attributable to maturation or to specific intervention effects. A growing body of research indicates that children receiving high quality early intensive behavioural intervention may make large gains relative to comparison groups (Reichow and Wolery 2009). Some prospective studies exploring developmental trajectories in preschoolers with ASD have linked larger gains to intervention effects (Turner et al. 2006), while others have found no such association (Eaves and Ho 2004). Children in this sample received a range of interventions, including speech therapy, occupational therapy and behavioural intervention. There were significant differences in service type, intensity, duration, onset, and offset across the sample. Research underway will explore the impact of specific types and intensity of interventions on outcomes for children in the Pathways in ASD study. Preliminary findings suggest that IQ gains may take place even in those who do not receive specific types of specialized support. For example, in a group of children in this study who did not receive behavioural intervention for 11 h/week or more at any time point, IQ increased from 58.21 (34.79) to 69.09 (38.59) between diagnosis and school entry, t(75) = −3.51, p = .001.
The present findings have important implications for clinicians considering the cognitive prognosis of young children with ASD. Results suggest that large decreases in cognitive scores are unlikely between diagnosis and school entry. Scores rarely decreased by 30 points or more, and only a few children with cognitive scores above 70 at diagnosis had cognitive scores in the intellectual disability range when starting school. It may therefore be useful to support families of children with higher initial cognitive scores in understanding that their child’s cognitive skills are likely to remain an area of relative strength compared to many children on the autism spectrum. Though large decreases appear to be rare in higher functioning children, small decreases may occur, especially when different tests are used at different time-points. It may be beneficial for psychologists to attend to the specific skill areas tapped by different intellectual ability measures, and to interpret this when discussing results with families and with other clinicians.
Results from this study are consistent with guidelines suggesting follow-up cognitive assessments in young children with ASD. While large decreases in cognitive functioning appear to be unlikely in preschool samples with ASD, large increases are common. Thirty-one percent of 2-year-olds, 24 % of 3-year-olds and 22 % of 4-year-olds gained at least 30 IQ points on the M-P-R between diagnosis and school entry. Score stability appeared to increase with age and repeated testing, and many children initially scoring in the mild-moderate delay range had cognitive scores in the no-delay range by age 6. Although large gains took place in many cases, it is important to note that approximately two-thirds of children who initially scored in the severe cognitive delay range continued to score below 70 at school entry. We agree with other research groups (e.g., Hedvall et al. 2014) that it is important to ensure that parents of cognitively lower functioning children are fully informed about their child’s current cognitive scores in addition to their ASD diagnosis. This may ideally be done in the context of discussing other important variables that will shape the child’s development (e.g., child temperament, talents).
Results from this study are relevant to decisions about the identification of concurrent intellectual disability in young children with ASD. In this sample, 24 % of children at school entry had delays in both cognitive skills and adaptive functioning consistent with such a diagnosis (vs. 33 % at initial assessment). This is relatively consistent with an estimated co-occurrence of intellectual disability of 37 % in a recent sample of 253 30- to 65- month-old children with ASD (Rivard et al. 2015). Recent changes in diagnostic guidelines (APA 2013) encourage clinicians to specify whether children with an ASD have an accompanying intellectual impairment. This specifier has the potential to provide valuable information for teachers, families, and individuals with ASD. There is increasing concern that parents are often not appropriately informed about the presence of intellectual disability in their children on the autism spectrum (e.g., Goin-Kochel et al. 2008; Hedvall et al. 2014). It is important that diagnoses of ASD do not overshadow diagnoses of intellectual disability because of the long-term implications of the combined impact of ASD and intellectual disability. However, it is also imperative to ensure that diagnostic labels are not applied prematurely. In this study, no children with scores above 70 on both cognitive and adaptive measures at the time of diagnosis met criteria for intellectual disability at school entry. Thus, early specification of the absence of an intellectual disability appears appropriate. In contrast, children who initially presented with both cognitive and adaptive delays often made gains (43 % had scores above 70 in at least one area; 22 % had scores above 70 in both areas). For these children, it may be appropriate to delay the specification of accompanying intellectual impairment, especially if children are very young or have milder delays. The possibility of a later intellectual disability diagnosis may nonetheless be important to introduce to families, as 57 % of children continued to have delays in both cognitive skills and adaptive functioning upon later assessment. Study findings support the usefulness of the term “global developmental delay” for some children who initially present with low ability scores (APA 2013), as this diagnosis recognizes that score stability may be lower in the preschool years. Consistent with current clinical guidelines (e.g., APA 2013), follow-up testing of preschool children is important, as the stability of ability scores appears to improve with age and repeated assessment. See also (Bennett et al., 2014) for related information about possible benefits of delaying the specification of language impairment in preschool children with ASD.
There are some limitations to this study. First, due to missing data, children included in some analyses (stability of adaptive behaviour scores and overall level) had a higher mean initial IQ scores than children who were excluded. Thus, children in those analyses may be somewhat higher functioning than the general population of children with ASD. This difference was small, and initial age, autism severity, and adaptive behaviour were consistent with that of the larger Pathways in ASD sample. A second limitation of this study is that cognitive skills were assessed using a measure that has not frequently been used in other ASD research. The M-P-R was selected as it is a revision of a widely used measure, it employs engaging materials appropriate to young children, and it assesses skill level across a wide age and ability range. It was therefore deemed especially suitable for a longitudinal study that included 2-year-olds. Although scores correlate strongly with scores on more established measures such as the Bayley Scales of Infant Development, the scale has unique properties (e.g., expressive language skills are not included within the global intellectual ability scale; the scale has a relatively low floor). Little previous research has explored longitudinal trajectories on the M-P-R or links between the M-P-R and scales used in older children. Authors have often treated IQ scores from varied measures as equivalent. Although multiple measures are often needed to capture skills across a range of ages and skill levels, the impact of measure selection is important to consider, especially when examining change over time. It is also important to note that individual assessments of cognitive skills were subject to the influence of behavioural dysregulation, which is common in children with ASD and can affect profiles of change over time. In addition, this study employed pre-determined test points (diagnosis, one-year follow-up, and school entry), and the interval between one-year follow-up and school entry differed across groups (3 years for 2-year-olds, 2 years for 3-year-olds, and 1 year for 4-year-olds). Additional assessment points would be needed to further establish when changes in skill level may take place within the preschool period.
Study findings are relevant to researchers, clinicians, and families. Key implications are that IQ scores often increase across the preschool period in children with ASD, whereas adaptive scores remain relatively stable. Younger children experience greater IQ gains between diagnosis and school entry, and changes in cognitive level are most likely in children with mild-moderate delays. Cognitive level also influences adaptive behaviour trajectories and the relationships between cognitive and adaptive scores. Study findings are especially relevant with the recent release of DSM-5 specifiers, which encourage clinicians to identify whether individuals with ASD have an accompanying intellectual impairment. In preschool children with ASD, specification of the absence of an intellectual impairment appears appropriate. However, specification of the presence of intellectual impairment may not be advisable without follow-up testing in many cases, due to possible increases in skill level over time. It is important that the presence of ASD does not overshadow diagnosis of intellectual disability. In children with very low scores, it may be appropriate to discuss the possibility of later specification of intellectual disability, and repeated assessment should be strongly encouraged. Study findings support the importance of follow-up assessments for young children with ASD. Prior-to-school assessments may be especially valuable, as they provide the opportunity to assess cognitive skills, adaptive skills, language skills, and school readiness at a key transition point for educational planning. Assessments should include measures of both adaptive and cognitive functioning, and scores on both measures should be considered when determining appropriate supports (e.g., children without cognitive delays may require support due to adaptive functioning delays). Our research team continues to follow the development of the children included in this study beyond school entry, which will allow for ongoing assessment of the predictive value of early cognitive and adaptive scores.
References
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Bennett, T. A., Szatmari, P., Georgiades, K., Hanna, S., Janus, M., Georgiades, S., et al. (2014). Language impairment and early social competence in preschoolers with autism spectrum disorders: a comparison of DSM-5 profiles. Journal of autism and developmental disorders, 44(11), 2797–2808.
Constantino, J. N., & Gruber, C. P. (2002). The social responsiveness scale. Los Angeles: Western Psychological Services.
Dietz, C., Swinkels, S. H., Buitelaar, J. K., Van Daalen, E., & Van Engeland, H. (2007). Stability and change of IQ scores in preschool children diagnosed with autistic spectrum disorder. European Child and Adolescent Psychiatry, 16(6), 405–410.
Doll, E. A. (1965). Vineland social maturity scale. Circle Pines: American Guidance Service.
Eaves, L. C., & Ho, H. H. (1996). Brief report: Stability and change in cognitive and behavioral characteristics of autism through childhood. Journal of Autism and Developmental Disorders, 26(5), 557–569.
Eaves, L. C., & Ho, H. H. (2004). The very early identification of autism: Outcome to age 41/2–5. Journal of Autism and Developmental Disorders, 34(4), 367–378.
Gabriels, R. L., Ivers, B. J., Hill, D. E., Agnew, J. A., & McNeill, J. (2007). Stability of adaptive behaviors in middle-school children with autism spectrum disorders. Research in Autism Spectrum Disorders, 1(4), 291–303.
Goin-Kochel, R. P., Peters, S. U., & Treadwell-Deering, D. (2008). Parental reports on the prevalence of co-occurring intellectual disability among children with autism spectrum disorders. Research in Autism Spectrum Disorders, 2(3), 546–556.
Goldstein, S., Naglieri, J. A., & Ozonoff, S. (Eds.). (2008). Assessment of autism spectrum disorders. New York: Guilford Press.
Hedvall, Å., Westerlund, J., Fernell, E., Holm, A., Gillberg, C., & Billstedt, E. (2014). Autism and developmental profiles in preschoolers: Stability and change over time. Acta Paediatrica, 103(2), 174–181.
Johnson, C. P., & Myers, S. M. (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120(5), 1183–1215.
Jónsdóttir, S. L., Saemundsen, E., Ásmundsdóttir, G., Hjartardóttir, S., Ásgeirsdóttir, B. B., Smáradóttir, H. H., & Smári, J. (2007). Follow-up of children diagnosed with pervasive developmental disorders: Stability and change during the preschool years. Journal of Autism and Developmental Disorders, 37(7), 1361–1374.
Joseph, R. M., Tager-Flusberg, H., & Lord, C. (2002). Cognitive profiles and social-communicative functioning in children with autism spectrum disorder. Journal of Child Psychology and Psychiatry, 43(6), 807–821.
Kamphaus, R. W. (1993). Clinical assessment of children’s intelligence: A handbook for professional practice. Needham Heights, MA: Allyn & Bacon.
Kanne, S. M., Gerber, A. J., Quirmbach, L. M., Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2011). The role of adaptive behavior in autism spectrum disorders: Implications for functional outcome. Journal of Autism and Developmental Disorders, 41(8), 1007–1018.
Limperopoulos, C., Majnemer, A., Steinbach, C. L., & Shevell, M. I. (2006). Equivalence reliability of the Vineland Adaptive Behavior Scale between in-person and telephone administration. Physical & occupational therapy in pediatrics, 26(1–2), 115–127.
Lord, C., Rutter, M., DiLavore, P. C., & Risi, S. (2002). ADOS: The autism diagnostic observation scale. Los Angeles, CA: Western Psychological Services.
Lord, C., & Schopler, E. (1989a). The role of age at assessment, developmental level, and test in the stability of intelligence scores in young autistic children. Journal of Autism and Developmental Disorders, 19(4), 483–499.
Lord, C., & Schopler, E. (1989b). Stability of assessment results of autistic and non-autistic language-impaired children from preschool years to early school age. Journal of Child Psychology and Psychiatry, 30(4), 575–590.
Magiati, I., Moss, J., Charman, T., & Howlin, P. (2011). Patterns of change in children with autism spectrum disorders who received community based comprehensive interventions in their pre-school years: A seven year follow-up study. Research in Autism Spectrum Disorders, 5(3), 1016–1027.
Nordin, V., & Gillberg, C. (1998). The long-term course of autistic disorders: Update on follow-up studies. Acta Psychiatrica Scandinavica, 97(2), 99–108.
Perry, A., Flanagan, H. E., Dunn Geier, J. D., & Freeman, N. L. (2009). Brief report: The Vineland adaptive behavior scales in young children with autism spectrum disorders at different cognitive levels. Journal of Autism and Developmental Disorders, 39(7), 1066–1078.
Rapin, I. (2003). Value and limitations of preschool cognitive tests, with an emphasis on longitudinal study of children on the autistic spectrum. Brain and Development, 25(8), 546–548.
Ray-Subramanian, C. E., Huai, N., & Weismer, S. (2011). Brief report: Adaptive behavior and cognitive skills for toddlers on the autism spectrum. Journal of Autism and Developmental Disorders, 41, 679–684.
Reichow, B., & Wolery, M. (2009). Comprehensive synthesis of early intensive behavioral interventions for young children with autism based on the UCLA young autism project model. Journal of autism and developmental disorders, 39(1), 23–41.
Rivard, M., Terroux, A., Mercier, C., & Parent-Boursier, C. (2015). Indicators of intellectual disabilities in young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 45(1), 127–137.
Roid, G. H., & Sampers, J. L. (2004). Merrill-Palmer-Revised scales of development. Wood Dale, IL: Stoelting Co.
Rutter, M., LeCouteur, A., & Lord, C. (2003). ADI-R: The autism diagnostic interview-revised. Los Angeles, CA: Western Psychological Services.
Sigman, M., & McGovern, C. W. (2005). Improvement in cognitive and language skills from preschool to adolescence in autism. Journal of Autism and Developmental Disorders, 35(1), 15–23.
Sparrow, S. S., Balla, D. A., & Cicchetti, D. V. (1984). Vineland adaptive behavior scales. Circle Pines, MN: American Guidance Service.
Sparrow, S.S., Cicchetti, D.V., & Balla, D.A. (2005). Vineland Adaptive Behaviour Scales: Second edition. Livonia, MN: Pearson Assessments.
Stevens, M. C., Fein, D. A., Dunn, M., Allen, D., Waterhouse, L. H., Feinstein, C., & Rapin, I. (2000). Subgroups of children with autism by cluster analysis: A longitudinal examination. Journal of the American Academy of Child and Adolescent Psychiatry, 39(3), 346–352.
Szatmari, P., Georgiades, S., Duku, E., Bennett, T. A., Bryson, S., Fombonne, E., Thompson, A., et al. (2015). Developmental trajectories of symptom severity and adaptive functioning in an inception cohort of preschool children with autism spectrum disorder. JAMA psychiatry, 72(3), 276–283.
Turner, L. M., Stone, W. L., Pozdol, S. L., & Coonrod, E. E. (2006). Follow-up of children with autism spectrum disorders from age 2 to age 9. Autism, 10(3), 243–265.
Wechsler, D. (2002). WPPSI-III administration and scoring manual. San Antonio, TX: The Psychological Corporation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Flanagan, H.E., Smith, I.M., Vaillancourt, T. et al. Stability and Change in the Cognitive and Adaptive Behaviour Scores of Preschoolers with Autism Spectrum Disorder. J Autism Dev Disord 45, 2691–2703 (2015). https://doi.org/10.1007/s10803-015-2433-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-015-2433-6