Abstract
This paper charted the cognitive and behavioural profiles from toddlerhood to middle childhood in 48 children diagnosed with ASD at 24-months. The Mullen Scales of Early Learning (MSEL) was administered at 24- and 48-months and the Wechsler Abbreviated Scale of Intelligence (WASI) at school age. Autism severity was derived using The Autism Diagnostic Observation Schedule (ADOS) Results: Developmental Disability/Intellectual Disability (DD/ID; Developmental Quotient <70) reduced from 64% at 24-months to 8% at outcome. Seventy-three percent of children continued to meet ADOS cut-off at school age. Conclusion: Diagnoses at 24-months, appear to be reliable and stable. Further research is needed to investigate whether early identification, which provides more opportunity to access early intervention, may in turn facilitate cognitive development over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances in diagnostic practice of Autism present the opportunity to study these neurodevelopmental conditions from earlier in a child’s developmental course than ever before. However, our understanding of the developmental trajectories associated with Autism remains limited, with few studies tracking development longitudinally from toddlerhood through to school age. Instead, there is greater knowledge of how early developmental profiles change throughout toddlerhood based on studies spanning periods of 1–2 years. Moreover, as most studies have investigated the development of high-risk and clinically referred cohorts of children, relatively little is known about how children with Autism, ascertained from low-risk community samples, grow and develop over time. The current study focused on a cohort of children identified prospectively and tracked longitudinally until school age.
Cognition
Much of our knowledge about early cognitive development in children with Autism derives from early intervention studies, where intervention outcomes are measured by gains in cognition (measured as developmental/intelligence quotients; DQ/IQ). Although studies have described the early changing dynamics of cognitive development in Autism, early scores are also thought to be least stable due to the rapid learning and development that can occur during the pre-school years (Joseph et al. 2002; Rapin 2003).
Early cognition was investigated in a cohort of 196 pre-school children with autism who were followed over a 2-year period, from 2 to 5 years of age (Hedvall et al. 2014). Children who tested with Developmental Disability (DD; IQ < 70) at time one were most likely to remain in that same range at follow-up. Further, cognitive outcomes were related to autism severity at both time points, in that a diagnosis of Autistic Disorder (AD; higher autism severity) was more strongly associated with DD at outcome in comparison to children with a diagnosis of Asperger’s Disorder or Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS). At time one, 54% of children with AD met criteria for DD, while at follow-up, 88% of these children met criteria for DD. Similarly, children who were within the average range of intellectual functioning at time one were more likely to test within the average range at follow-up.
Estimates of Intellectual Disability (ID) vary across samples and studies. Some suggest that two-thirds of individuals with Autism also have a co-occurring ID (Dykens and Lense 2011), while other studies report a 20% prevalence of ID, with the remainder of their sample testing with average and above average intellectual abilities (Charman et al. 2010). The term ‘unevenness’ is commonly used to describe the profile of differences in verbal and non-verbal abilities, with discrepancies across studies as to which profile is most commonly associated with Autism. A meta-analysis by Lincoln et al. (1998) found a consistently higher Performance Intelligence Quotient (PIQ) and lower Verbal Intelligence Quotient (VIQ), as reported across many studies. Other studies have found superior VIQ relative to PIQ indicating strength in language abilities within their samples (Siegel et al. 1996). Language and cognitive outcomes were investigated in a sample of 26 children who were diagnosed with autism at 2-years, followed up at 3-years and again at 7-years of age (Charman et al. 2005). At a group level, non-verbal IQ scores were stable from 2 to 7 years, though more individual variability in non-verbal outcomes was found at age 7 compared to the earlier time points. Further, children’s non-verbal communicative acts during a play-based interaction with the examiner at age 2-years, significantly predicted cognitive, language and social outcomes at 7-years of age.
One of the few studies to compare developmental difference in verbal and non-verbal abilities across younger and older children with Autism was conducted by Joseph et al. (2002) who reported an uneven rate of cognitive development in children between the ages of 3- and 13-years. Different profiles were associated with different ages; pre-school aged children had significantly lower verbal scores compared with non-verbal scores, but this discrepancy was found to dissipate with age; no significant differences in verbal and non-verbal abilities were evident by school age. Cognitive abilities at pre-school age were found to significantly predict cognitive outcomes at school age, in a longitudinal investigation by Stevens et al. (2000). At pre-school age, children were divided into either ‘high-functioning’ or ‘low-functioning’ subgroups (NVIQ greater than or less than 80). Those who were considered ‘high-functioning’ at pre-school age tested within the ‘normal’ cognitive range at school age. Early cognitive difficulties continued at school age, with 92% of the children who were considered ‘low-functioning’ at pre-school age remaining in the same cluster at school age.
Barbaro and Dissanayake (2012) described the early cognitive development of a very young sample of children with Autism from 12- to 24-months, prospectively identified via developmental surveillance (some of whom form the school age sample in the current study). The sample displayed an uneven profile of verbal and non-verbal abilities as measured by the Mullen Scale of Early Learning (MSEL; Mullen 1995), with higher scores on the non-verbal subtests and lower verbal skills, particularly in the area of receptive (understanding of) language.
Due to the paucity of research on long-term outcomes of low-risk cohorts diagnosed early, it is difficult to anticipate how these children will grow and develop over time. There is discrepancy in the literature surrounding whether early or later cognitive profiles are most indicative of long-term outcomes. Collectively, Joseph et al. (2002), McGovern and Sigman (2005) and Nordin and Gillberg (1998) found that school age cognitive scores were more indicative of potential long-term developmental outcomes for children with autism in comparison to early cognitive profiles. In contrast, Lord and Schopler (1989), who conducted one of the first studies to assess longer-term stability of cognition from 2- to 7-years of age, found that intelligence was largely stable from preschool to school age. Gains in DQ ranged from 4 to 20 DQ points over the course of the study, with the most considerable gains made between the ages of 2 and 3-years (15 points). Encouragingly, gains were also made by children who began with a DQ <70, resulting in some of these children moving out of the ID range at follow-up. However, despite evidence of considerable improvements, some children continued to meet criteria for ID at outcome, with these early difficulties extending from pre-school to school age. Turner et al. (2006) reported more positive outcomes in their 5-year follow-up, from 2- to 9-years of age. At 2-years of age, the mean DQ was 55.6, signifying widespread cognitive difficulties. However, by age 9, the incidence of ID had been reduced to only 28% of the sample. For the remainder of sample, 16% of children scored in the ‘borderline’ range while 56% of children scored within the average or above average range of intelligence at school age, emphasizing the importance of early diagnosis and timely intervention to promote cognitive gains later in childhood.
One of the most comprehensive longitudinal studies in the field was that conducted by Sigman et al. (1999) investigating cognition, language development and social competence in a cohort of 51 children with AD. Children were followed from 3 to 12-years of age, demonstrating substantial improvements in cognition by gaining an average of 22 IQ points over a 9-year period. At a group level, cognitive gains were largely stable. However, decline in cognition was also evident amongst individuals in this sample. Anderson et al. (2014) also conducted a lengthy follow-up over a 17-year period to ascertain which early abilities predicted cognitive outcomes in young adults with ASD. Children were followed up at 2, 3 and 19-years of age. Childhood IQ at age 2 and 3-years was the best predictor of cognitive outcome at 19-years of age. In 85% of cases, ID at 19-years of age could be accurately predicted by VIQ and NVIQ scores combined. Lower cognitive abilities and more severe ASD symptomatology at age 2-years was predictive of group membership in the VIQ <70 group at age 19. Young adults in the VIQ >70 group had shown more improvements in their verbal and non-verbal and social skills compared with children in the VIQ <70 group. More recently, Flanagan et al. (2015) investigated change in cognitive and adaptive behaviour scores in children with Autism from diagnosis at 2-years, to school entry at 6-years of age. The largest cognitive gains were made at age 2 (18-points) and 3-years (12-points). While all children demonstrated significant improvements in their cognitive scores between time of diagnosis and school entry, 24% of children tested with an Intellectual Disability (ID) at age 6-years.
Autism Symptoms
Developmental surveillance and screening methods have facilitated earlier detection of autism (Barbaro and Dissanayake 2009). Despite changes to the diagnostic criteria, earlier autism spectrum diagnoses are both reliable and stable throughout childhood, into adolescence (Lord et al. 2006; Moore and Goodson 2003). Fountain et al. (2012) established six trajectories to describe patterns of social communication functioning and repetitive behaviours in a cohort of 6975 children on the spectrum over a period of 12-years. These trajectories highlighted differential rates of improvement in symptoms, with rapid gains for some children, while others revealed slower and fewer improvements overall; the heterogeneity in outcomes was attributed to early autism symptom severity. Children with less severe symptoms at intake (Mean age; 2-years) demonstrated more rapid improvements in their social communication functioning; most children showed little change in their repetitive behaviours over time, irrespective of their early symptom severity. Not surprisingly, children with co-morbid diagnoses of ID were also more likely to be classified in the low functioning trajectory group, demonstrating the least improvement in their social communication over time.
In a 6-year follow-up study, Szatmari et al. (2015) identified two distinct developmental trajectories in their inception cohort: one group (11.5% of the sample) demonstrated reduced severity of autism symptoms over time, while the other, comprising 88.6% of the sample, were classified in a severe and stable trajectory indicating little change in their symptom expression over time. Additionally, children were classified into one of three trajectories on the basis of adaptive functioning: lower or worsening (29%), moderate stable functioning (49.9%), and higher improved functioning (20.9%). Improvements in adaptive functioning were not related to severity of autism symptomatology. Overall, 20% of children in the severe yet stable autism severity group were classified in the higher functioning and improving adaptive functioning groups at follow-up.
Reports of diagnostic stability most commonly describe high-risk and clinically referred samples, with these studies consistent in their reports of high short-term stability (between 70 and 100% stable) in samples of children diagnosed at 2-years (Chawarska et al. 2007; Sutera et al. 2007; Turner and Stone 2007). Excellent short-term stability was also reported in a sample of 196 pre-school children where it was found that 90% of children continued to receive an ASD diagnosis when followed up 2-years later (Hedvall et al. 2014). Further, stability was dependent on the original diagnostic subtype where a diagnosis of AD and Asperger’s Disorder were the most stable subtypes, with PDD-NOS found to be the least stable category.
Other studies have also revealed high long-term diagnostic stability with between 80 and 95% of children diagnosed with Autism during their pre-school years continuing to meet diagnostic criteria at school age. In a follow-up study conducted by McGovern and Sigman (2005), 46 of 48 children who received a diagnosis of autism at 2-years continued to meet threshold on the ADOS at 5-years of age, yielding a stability rate of 95%. Charman et al. (2005) revealed that all but one of the 26 children in their sample, diagnosed at 2-years, remained on the autism spectrum into middle childhood, aged 7-years. Turner et al. (2006) also reported excellent long-term stability in their sample of 58 children diagnosed with Autism at 2-years of age, with ~80% of children retaining their diagnosis when followed-up at 9-years. Lord et al. (2006) found that best estimate Autism diagnoses made at 2-years were mostly stable through to 9-years of age with only 1 of 84 children receiving a non-spectrum diagnosis. Considerable changes or improvements in symptom expression throughout childhood can result in diagnostic re-classification from ‘Autism’ to ‘non-spectrum’ at follow-up. Sutera et al. (2007) found (17%) of their sample no longer met diagnostic cut-off for Autism at 4-years. Similarly, Kleinman et al. (2008) found that although diagnoses made at 2-years using clinical judgment were stable in ~80% of cases, 19% of children experienced improvements in their symptomatology, moving off the spectrum at time 2 (between 42 and 82-months).
The stability of autism spectrum diagnoses in community samples has not been well established. As the uptake of developmental surveillance methods within the wider community becomes more widespread, further investigation is warranted to ascertain long-term stability of early community-based diagnoses of ASD. In Australia, these are typically made by a multidisciplinary team of community health professionals, including a Speech Therapist, Psychologist and Pediatrician. Available reports to date confirm that the stability of early Autism diagnoses made in the community range between 80 and 93%, and are thus comparable to that established with other samples. Using a large national web-based registry, Danials et al. (2011) investigated diagnostic stability in 7106 children diagnosed with Autism under DSM-IV criteria (AD, ASD or PDD-NOS). The diagnostic classification did affect stability of diagnosis in the long term, with AD diagnoses the most stable over time while diagnoses of ASD/PDD-NOS were least stable; 39% of children with a PDD-NOS diagnosis were given a different diagnosis (mostly AD), and 29% of children originally diagnosed with ASD were reclassified as AD.
Stability of early community diagnoses were further investigated by Guthrie et al. (2013) in their sample of 82 toddlers, derived from a larger general population cohort. Children received two diagnostic evaluations with the ADOS Toddler module (ADOS-T) between 15 and 24-months of age, and a follow-up assessment 12-months later. Despite some deferred diagnostic decisions (17% of cases), high rates of stability were reported overall, with early diagnoses made in the community found to predict follow-up diagnoses in 100% of cases.
As part of the Baby Siblings Research Consortium (BSRC), diagnostic stability was investigated in a large-scale sample of 418 later-born infants at familial risk for developing autism (Ozonoff et al. 2015). Children were assessed with the MSEL and ADOS at 3 time points, 18, 24 and 36-months with the aim of investigating stability of symptoms at 36-months of an ASD diagnosis made at 18 and 24-months. In keeping with stability rates in other clinically referred and community cohorts, stability of diagnosis made at 18-months was 93 and 82% when a diagnosis was made at 24-months.
Though Barbaro and Dissanayake (2016) have also recently reported that diagnostic stability for their cohort (from which the current school age sample was derived) was high (88.3%) between 24- and 48-months of age, there was evidence of movement within the spectrum with children moving between AD and ASD, and ASD to AD. Eaves and Ho (2004) also found agreement was high between the initial screening and the diagnosis made by professionals in the community, with 88% of children receiving a diagnosis of Autism (AD/ASD). Further, diagnoses were found to be stable with 93% of children retaining their diagnosis of Autism (AD/ASD) in the short-term between 2½ and 4½ years. These high rates of stability validate that early community diagnoses at 24-months are reliable and stable into the pre-school years.
The Current Study
The current study is one of a few of its kind to follow a cohort of children longitudinally from 24-months to school age. Moreover, the unique sample reported here was ascertained from a community-based cohort identified via developmental surveillance of early social attention and communication behaviours, during routine universally available Maternal Child Health check-ups at 12, 18 and 24-months (Barbaro and Dissanayake 2010; Barbaro et al. 2011). Our aim was to investigate developmental progress in cognition and autism symptom severity from 24-months to school age, as well as to investigate stability of ASD symptoms longitudinally. Following on from a recent paper including information on developmental profiles in this cohort between 24 and 48-months (Barbaro and Dissanayake 2016), it was hypothesised that children would demonstrate cognitive gains from 24-months to school age (7- to 9-years), with further reduction in the incidence of DD/ID from 48-months to school age expected. It was also hypothesised that the majority of children who met criteria for Autism at 24- and 48-months would continue to meet cut-off for Autism on the Autism Diagnostic Observation Schedule (ADOS-2; Lord et al. 2012) when assessed between 7 and 9-years of age.
Method
Participants
Participants were drawn from a larger cohort of 79 children who met criteria for an ASD at 24-months in the Social Attention and Communication Study (SACS; see Barbaro and Dissanayake 2010). Sixty-two of these children were followed-up at 48-months, where their pre-school outcomes were assessed (Barbaro and Dissanayake 2016). All families were invited to take part in the current study when their children were aged 7- to 9-years. Forty-eight children (36 males; 12 females) who attended the 48-month follow-up returned for the school age follow-up at (77.4% of sample). Ethics approval was obtained from the La Trobe University Human Ethics Committee prior to commencing the study.
The diagnostic evaluation at the 24-month assessment involved three components, including a standardized assessment of the child’s social communication behaviours (ADOS), and their cognitive development (MSEL) as well as a detailed developmental history gathered from the ADI-R (Lord et al. 1994). Information from all three assessments was used collectively to determine if the child was presenting with a behavioural profile consistent with an Autism Spectrum Disorder diagnosis. Following the assessment, all families were referred to a Pediatrician in their community, as is common practice, who confirmed the final diagnosis of Autism Spectrum Disorder at 24-months.
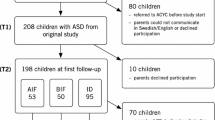
Figure 1 below outlines the recruitment process and participation breakdown for the current investigation. All families involved in the study whose child had a confirmed ASD diagnosis at 24-months were contacted for the school age follow-up (including those who did not attend at 48-months). Table 1 below presents the sample characteristics and diagnostic breakdown at each assessment age.
In the current sample, 48.9% of mothers had completed tertiary education (32.6% reaching undergraduate level, 16.3% completing postgraduate studies) while 31% of fathers had done so (19% undergraduate level, 12% postgraduate level). The most commonly reported level of education completed by fathers was secondary school (26%). The majority of children (77%) were attending a mainstream primary school with fewer children (18.8%) enrolled in a specialist education facility (4.2% of these children attended an autism specific school). A small number of children (4%) were enrolled in both a specialist education and mainstream settings part time. While type, intensity and duration of Early Intervention is not the focus of this paper, children did receive a wide range of community interventions, including both center-based group therapies and one-on-one home based programs such as Applied Behaviour Analysis (ABA). Speech therapy was the most prevalent intervention, received by 85% of the sample.
Measures
The Mullen Scales of Early Learning (MSEL; Mullen 1995) had been administered to assess developmental functioning at 24 and 48-months. The Fine Motor (FM) and Visual Reception (VR) subscales were used to assess non-verbal skills; Receptive Language (RL) and Expressive Language (EL) subscales were used as a measure of verbal skills. To investigate changes in children’s cognitive status over time, dividing the child’s mental age with their chronological age and multiplying by 100 created separate DQ scores for each of the four domains on the MSEL. The two verbal DQ scores (RL & EL) were averaged to create a Verbal Developmental Quotient (VDQ) at 24 and 48-months of age. Similarly, a Non-Verbal Developmental Quotient score (NVDQ) was derived from averaging the two non-verbal DQ scores (VR & FM). This allowed for the earlier verbal and performance scores from the MSEL to be charted alongside the Verbal (VIQ) and Performance (PIQ) scores derived from the Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler 1999) at school age. Although the MSEL and WASI scores are not numerically equivalent, they do provide a measure of verbal, non-verbal and overall functioning as well as DD/ID estimates at each time point.
The WASI was administered at school age to provide a brief and reliable measure of cognition. A Verbal Intelligence Quotient (VIQ) was derived from the similarities and vocabulary subtests and the block design and matrix reasoning subtests provided a measure of performance abilities (NVIQ).
The Autism Diagnostic Observation Schedule (ADOS-2; Lord et al. 2012) is a semi-structured play assessment conducted by an unfamiliar adult that assesses social communicative skills, play skills and other behaviours at school age. The ADOS-G (Lord et al. 2000) had been administered at 24 and 48-months. At 24-months, all children were assessed using Module 1. When followed up at pre-school age, 11 children were re-assessed using Module 1, while 37 were assessed using module 2. At school age, 7 children presented with phrase speech and were assessed using Module 2; the remaining 41 children demonstrated verbal fluency and were assessed using Module 3. In all modules, a total score is derived from the sum of the Social Affect (SA) section combined with the sum on the Restricted Repetitive Behavior section (RRB). In order to allow for comparability across age and different modules of the ADOS, the revised algorithm procedure (Gotham et al. 2009) was employed to ascertain diagnostic severity and diagnostic classification at school age. A child’s total score on the ADOS (SA + RRB) was then converted into a severity score, using these revised algorithms. This severity score corresponds with one of three classification ranges that have been calibrated so that children with a severity score of 1–3 are classified as non-spectrum, scores of 4–5 correspond with an ASD classification and scores of 6–10 received an Autism classification.
Procedure
Parents provided written informed consent upon arrival at the Olga Tennison Autism Research Centre (OTARC). They completed a Demographic Questionnaire and an Early Intervention History Form, while their child was assessed in a separate room. The ADOS was administered first followed by the WASI. A report summarising the assessment for each child was sent to the family. All assessments were conducted in a standardised manner by a researcher trained to research reliability on the ADOS. With parental permission, all sessions were digitally recorded to assist with scoring of tests.
Results
Cognitive scores from the MSEL at 24 and 48-months and the WASI at school age are presented by diagnostic subgroup in Table 2. The ASD stable group comprises children who continued beyond age 2-years to meet criteria for Autism on the ADOS at each time point. Children who fell below cut-off on the ADOS at either pre-school or school age were classified in the ASD non-stable group. The ASD pathways of this cohort are presented in Fig. 5 below.
As not all children assessed at 24 and 48-months returned for follow-up at pre-school and/or school age, analyses were undertaken on the developmental and behavioural profiles of those who did and did not return at each follow-up to determine if the sample at school age was representative of the original cohort seen and diagnosed at 24-months. The results revealed no significant differences in early cognition between those who did and did not return at 48-months (p = .70) and 7–9 years (p = .24). Similarly, there were no significant differences in autism severity between children who did and did not return at 48-months (p = .08) and those who did and did not return at 7–9 years (p = .18); therefore the children involved in the school age cohort appear representative of the original SACS cohort.
Cognitive Development
We first examined the percentage of children at each time point who had a DQ/IQ <70. At 24-months, 68% of children had a global developmental delay (DD), with intellectual disability reduced to 42% at preschool age (48-months). At the school age follow-up, only 8% of children had an ID. Though only a small proportion (8%) of children tested had an ID at school age, the standard deviation on cognitive scores in Table 2 shows a considerable range in abilities, indicating that some children scored in the average and above average ranges on the WASI with others within the ID range.
A 2 (Group) × 3 (Age) repeated measures ANOVA was conducted to investigate continuity and change in cognition across time. As evident in Fig. 2, both groups made substantial gains over time, with the ASD stable group gaining an average of 35 IQ points and the ASD non-stable group gaining 39 IQ points between toddlerhood and school age. The Group main effect was significant, F (46,1) = 6.92, p = .012, η2 = .131 with the ASD non-Stable group having higher developmental/intelligence quotients at each age relative to the ASD stable group. The main effect of Age was also significant, F (45,2) = 94.44, p < .001, η2 = .80, revealing substantial an improvement in cognition throughout childhood in both groups, with no significant interaction effect, F (45,2) = 1.57, p = .28, η2 = .065.
Verbal and Non-verbal Cognition
Additional 2 × 3 repeated measures ANOVAs were conducted to investigate gains in verbal and non-verbal development across time. A significant main effect of Group, F (46,1) = 7.74, p = .008 η2 = .144, revealed that the ASD stable group had lower verbal scores than the ASD non-stable group. The results also revealed a significant main effect of Age, F (45,2) = 133.01, p < .001, η2 = .85, confirming significant improvement in language development (expressive and receptive language skills) from 24-months through to school age in both groups, as evident in Fig. 3. There was no significant interaction effect, F (45,2) = 0.815, p = .449, η2 = .035.
A significant main effect for Group was also identified for non-verbal development, with the ASD non-stable group again demonstrating higher NV abilities at each time point F (46,1) = 5.02, p = .030, η2 = .098. A significant main effect of Age also confirmed overall improvement in non-verbal cognition from toddlerhood to school age, F (2,45) = 33.13, p < .001, η2 = .59; no significant Group × Age interaction effect was found, F (2, 45) = 2.44, p = .098, η2 = .098 (see Fig. 4).
Diagnostic Stability
In line with the current DSM 5 diagnostic criteria, the individual diagnostic subcategories (AD and ASD) were collapsed to form one diagnostic category ‘Autism Spectrum Disorder’ (ASD). Long-term stability of ASD symptoms was investigated to determine the percentage of children who continued to meet diagnostic criteria on the ADOS from 24-months through to school age. Overall, 73% of children continued to meet the threshold for Autism from toddlerhood through to school age.
Table 3 summarizes the four behavioural pathways (1 stable, 3 unstable) and the number of children within each. For the purpose of analysis, these pathways were consolidated into an ASD Stable group (n = 32) and a ASD non-stable group (n = 16), allowing for longitudinal comparison between groups on diagnostic severity from toddlerhood to school age (Fig. 5).
A mixed 2 (Group) × 3 (Age) repeated measures ANOVA revealed differences in autism severity, with significant main effects of Group, F (46,1) = 57.55, p < .001, η2 = .556, and Age, F (45, 2) = 4.64, p = .015, η2 = .171. A significant Group × Age interaction was also identified F (45, 2) = 6.11, p = .004, η2 = .214. Simple main effects revealed that while the ASD stable group had significantly higher autism severity at each age F (45,2) = 6.29 p = .004, η2 = .218 compared to the ASD non-stable group, as evident in Fig. 6, the severity of symptoms changed differently within each group across time. Symptoms in the stable group decreased significantly at pre-school age, but increased again at school age such that there was no difference in symptom severity between toddlerhood and school age. In contrast, the ASD non-stable group decreased in their autism severity between toddlerhood and school age, with the difference in severity between these times being significantly different F (45,2) = 4.92, p = .012, η2 = .179.
Discussion
The current study is one of few to follow a community-based cohort of children, who were prospectively identified and diagnosed with Autism at 24-months, longitudinally until school age. The findings indicate high stability of autism symptoms over time, and chart differential changes in autism severity and cognitive functioning from toddlerhood to school age.
Cognitive Development
Historically, the long-term prognosis for individuals with Autism, albeit variable, was reportedly poor (Howlin and Moss 2012). However, the few longitudinal studies available have reported improved short-term outcomes for children, with these improvements extending into school age (Sigman et al. 1999; Turner et al. 2006). Though children in the current study demonstrated variability in their rates and patterns of cognitive development, as anticipated, they made gains in cognition between 24-months and school age. However, the rates of improvement reported in the current study, where children were identified and diagnosed early, are substantially greater than those typically seen in most other cohorts, both in the short and long term. Indeed, the current findings are in marked contrast to some of the earlier longitudinal literature, despite cognitive gains that were reported. For example, Lord and Schopler (1989) found that cognitive difficulties (ID) extended from pre-school to school age in many cases. Flanaghan et al. (2015) found ID affected 24% of their sample at school age. Hedvall et al. (2014) found the incidence of DD increased from pre-school intake to the 2-year follow-up, affecting 88% of their sample, indicating that early cognitive difficulties experienced by children with AD persisted into their first school year. Further, in a longer-term follow-up by Anderson et al. (2014), found early cognition at age 2 and 3-years, predicted cognitive outcomes in young adults with ASD, at 19-years. Moreover, early non-verbal and verbal scores combined were found to accurately predict ID 17-years later in 85% of cases, suggesting that early cognitive difficulties in this sample were found to persist throughout childhood. In contrast, the current study, found that early cognitive difficulties did not continue on into the school years, with considerable improvements found over time as reflected by the decrease in DD/ID from 64% at 24-months to only 8% at school age, a considerably lower rate of DD than reported in most other studies.
The developmental profiles of children in the SACS cohort were first described as uneven; they showed relative strengths in performance abilities with lower verbal scores on the MSEL, particularly in the domain of receptive language (Barbaro and Dissanayake 2012). Interestingly, the children that were followed longitudinally and re-assessed at school age, continued to display a similar profiles of abilities, demonstrating higher non-verbal skills compared with verbal skills at each time point. The same profile that was established early in their developmental course in infancy and toddlerhood has continued into their school years. However, over time, all children, including those who did and did not continue to meet Autism criteria, showed improvement. These findings pertaining to the reduction in DD/ID from 24-months through to school age, confirms that children with Autism can make rapid developmental progress throughout childhood, particularly if identified early in life when verbal skills are emerging in typically developing children. Overall, the cohort made excellent gains, demonstrating an average 36-point increase in DQ/FSIQ from toddlerhood to school age. However, as with the changes in Autism severity, the changes in cognition were most marked in the ASD Non-Stable group of children who exceeded the ASD Stable group at each age.
The most encouraging finding is that, overall, the current cohort of children progressed in their development over time, despite the majority showing early cognitive difficulties as highlighted by the high incidence of children meeting criteria for a DD at 24-months. These cognitive gains indicate that children with autism have the potential to learn, irrespective of their early cognitive and behavioural difficulties.
Diagnostic Stability and Autism Severity
As expected, the majority of children diagnosed with ASD at 24-months continued to meet criteria for Autism at school age (73%). The high rate of stability over time found in the current study is comparable with reports from other long-term follow-up studies of high-risk and clinically referred samples. Eaves and Ho (2004) reported 82% stability in the short term similar to Barbaro and Dissanayake (2016) when children were followed-up at preschool age. Others have reported stability ranging from 80 to 88% in samples diagnosed at 2-years and followed through to middle childhood, at 9-years (Charman et al. 2005; Turner et al. 2006). Guthrie et al. (2013) found early community diagnoses remained stable in 84% of cases, despite an initial delay in diagnosis in some cases.
Monitoring children’s early social attention and communication behaviours at their routine 12-, 18- and 24-month health checks assisted in the earlier detection of children developing Autism (Barbaro and Dissanayake 2010). These early social attention and communication behaviours (i.e., eye contact, pointing, response to name) are important markers for identifying children who are at risk of developing autism in the community. Developmental surveillance within a universal health system ensures all children can be closely monitored, irrespective of any familial history of developmental conditions. Given the high rate of stability in meeting the ASD threshold found over time in this and other studies, it is possible to conclude that early identification and diagnosis (made at 24-months) is both reliable and stable from toddlerhood through to the early school years.
Despite the overall stability of meeting diagnostic thresholds, there was significant change in Autism Severity Scores over time, particularly when examined in the context of the Stable and Non-stable ASD groups. The former consistently showed greater autism severity over time compared to the latter group. Within the ASD Non-stable group, 6 children (12%) no longer met the ASD cut-off on the ADOS at pre-school age and 13 children (27%) no longer met threshold criteria by school age. It is important to note, however, that at each follow-up, the severity scores were derived solely from the ADOS and these, unlike at 24-months, were not diagnostic assessments. Therefore, it is not possible to conclude that children had lost their diagnosis of Autism by middle childhood, but rather that their scores no longer met the cut-off criteria on the ADOS. In fact, in many of these cases, children were borderline, scoring only 1–2 points below threshold. Additionally, the majority of these children continued to demonstrate mild autism related symptomatology (i.e., some restricted interests/stereotypies, or the presence of some repetitive behaviours). However, the two groups showed very different trajectories in symptom severity over time, as revealed by the simple main effects analysis.
Study Strengths and Limitations
Early detection and subsequent diagnosis of Autism in the cohort investigated here is likely to have promoted timely access to community based intervention services for children, which may have contributed to the positive developmental outcomes seen during school age. However, the study was not designed to capture details on intervention received, and as the type, intensity and duration of early intervention services received varied greatly, it is not possible to conclude that a specific intervention contributed more to these positive outcomes than others. Children demonstrated considerable improvements in their cognition since their first assessment at 24-months, with only a small percentage of children presenting with an ID by school age. Although the contribution of early intervention to these outcomes is not addressed in the current paper, the current outcomes are generally better than those reported in studies that have examined outcomes following early intervention (Smith and Iadarola 2015; Starr et al. 2016). Therefore, the results need replication with a larger sample, to determine if these outcomes are unique to the current prospectively identified community-based sample. As there were no significant differences in early cognitive and behavioural profiles between those children who did and did not return at each follow-up, we may, nonetheless, conclude that the current sample of children seen at school age are representative of the original cohort seen and diagnosed at 24-months (Barbaro and Dissanayake 2010).
Conclusions
The current study supports previous findings that early diagnoses of Autism in toddlerhood are largely stable, both in the short- and longer-term in children prospectively identified via community developmental surveillance. With 73% of children continuing to meet criteria for Autism (AD/ASD) from toddlerhood through to school age, it is possible to conclude that an early diagnosis made at 24-months is both reliable and stable during the early years, into school age.
Further, although the incidence of developmental disability was high at 24-months (68%), most children (91%) tested within the average range of intellectual functioning by school age. The majority of children identified and diagnosed at 24-months with Autism, made significant cognitive gains over time, both in their verbal and non-verbal abilities, despite some having met criteria for an ID in toddlerhood. It appears that early identification and diagnosis, in enabling early access to services, may have facilitated positive cognitive development over time in the current sample. However, the extent to which early detection (and subsequent diagnosis) has contributed to the positive outcomes seen in this cohort (as a result of access to intervention) can only be determined by comparison with children who were not diagnosed early, which remains a topic for further research.
References
Anderson, D. K., Liang, J. W., & Lord, C. (2014). Predicting young adult outcome among more and less cognitively able individuals with autism spectrum disorders. Journal of Child Psychology and Psychiatry and Allied Disciplines, 55(5), 485–494. doi:10.1111/jcpp.12178.
Barbaro, J., & Dissanayake, C. (2009). Autism spectrum disorders in infancy and toddlerhood: A review of the evidence on early signs, early identification tools, and early diagnosis disorders: Review of the retrospective. Journal of Developmental and Behavioral Pediatrics: JDBP, 30(5), 447–459.
Barbaro, J., & Dissanayake, C. (2010). Prospective identification of autism spectrum disorders in infancy and toddlerhood using developmental surveillance: the social attention and communication study. Journal of Developmental and Behavioral Pediatrics: JDBP, 31(5), 376–385. doi:10.1097/DBP.0b013e3181df7f3c.
Barbaro, J., & Dissanayake, C. (2012). Developmental profiles of infants and toddlers with autism spectrum disorders identified prospectively in a community-based setting. Journal of Autism and Developmental Disorders, 42(9), 1939–1948. doi:10.1007/s10803-012-1441-z.
Barbaro, J., & Dissanayake, C. (2016). Diagnostic stability of autism spectrum disorder in toddlers prospectively identified in a community-based setting: Predictors of change over time. Autism: The International Journal of Research and Practice. DOI:10.1177/1362361316654084.
Barbaro, J., Ridgway, L., & Dissanayake, C. (2011). Developmental surveillance of infants and toddlers by maternal and child health nurses in an Australian community-based setting: Promoting the early identification of autism spectrum disorders. Journal of Pediatric Nursing, 26(4), 334–347. doi:10.1016/j.pedn.2010.04.007.
Charman, T., Jones, C. R. G., Pickles, A., Simonoff, E., Baird, G., & Happé, F. (2010). Defining the cognitive phenotype of autism. Brain Research, 1380(1943), 10–21. doi:10.1016/j.brainres.2010.10.075.
Charman, T., Taylor, E., Drew, A., Cockerill, H., Brown, J.-A., & Baird, G. (2005). Outcome at 7 years of children diagnosed with autism at age 2: Predictive validity of assessments conducted at 2 and 3 years of age and pattern of symptom change over time. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 46(5), 500–513. doi:10.1111/j.1469-7610.2004.00377.x.
Chawarska, K., Klin, A., Paul, R., & Volkmar, F. (2007). Autism spectrum disorder in the second year: Stability and change in syndrome expression. Journal of Child Psychology and Psychiatry, 2(48), 128–138. doi:10.1111/j.1469-7610.2006.01685.x.
Danials, A. M., Rosenberg, R. E., Law, J. K., Lord, C., Kaufmann, W. E., & Law, P. A. (2011). Stability of initial autism spectrum diagnoses in community settings. Journal of Autism and Developmental Disorders, 41, 110–121. doi:10.1007/s10803-010-1031-x.
Dykens, E. M., & Lense, M. (2011). Intellectual disabilities and autism spectrum disorder: A cautionary note. In G. Amaral, L. Dawson, & D. Geschwind. (Eds.), Autism spectrum disorders (pp. 261–269). New York: Oxford University Press.
Eaves, L. C., & Ho, H. H. (2004). The very early identification of autism: outcome to age 4 1/2–5. Journal of Autism and Developmental Disorders, 34(4), 367–378. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15449513.
Flanagan, H. E., Smith, I. M., Vaillancourt, T., Duku, E., Szatmari, P., Bryson, S., Fombonne, E., Mirenda, P., Roberts, W., Volden, J., Waddell, C., Zwaigenbaum, L., Bennett, T., Elsabbagh, M., & Georgiades, S. (2015). Stability and change in the cognitive and adaptive behaviour scores of preschoolers with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(9):2691–2703.
Fountain, C., Winter, A. S., & Bearman, P. S. (2012). Six developmental trajectories characterize children with autism. Pediatrics, 129(5), e1112–e1120. doi:10.1542/peds.2011-1601.
Gotham, K., Pickles, A., & Lord, C. (2009). Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 36, 693–705. doi:10.007/s10803-008-0674-3.
Hedvall, Å., Westerlund, J., Fernell, E., Holm, A., Gillberg, C., & Billstedt, E. (2014). Autism and developmental profiles in preschoolers: Stability and change over time. Acta Paediatrica, 103(2), 174–181. doi:10.1111/apa.12455.
Guthrie, W., Swineford, L. B., Nottke, C., & Wetherby, A. M. (2013). Early diagnosis of autism spectrum disorder: Stability and change in clinical diagnosis and symptom presentation. Journal of Child Psychology and Psychiatry, 54(5), 582–590. doi:10.1111/jcpp.12008.
Howlin, P., & Moss, P. (2012). Adults with autism spectrum disorders. Canadian Journal of Psychiatry, 57(5), 275–283.
Joseph, R. M., Tager-Flusberg, H., & Lord, C. (2002). Cognitive profiles and social-communicative functioning in children with autism spectrum disorder. J Child Psychol Psychiatry, 43(6), 807–821. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12236615.
Kleinman, J. M., Ventola, P. E., Pandey, J., Verbalis, A. D., Barton, M., Hodgson, S., & Fein, D. (2008). Diagnostic stability in very young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 38(4), 606–615. doi:10.1007/s10803-007-0427-8.
Lincoln, A., Courchesne, E., Allen, M., Hanson, E., & Ene, M. (1998). Neurobiology of Asperger syndrome: Seven case studies and quantitative magnetic resonance imaging findings. In E. Schopler, G. Mesibov, & L. J. Kunce (Eds.), Asperger syndrome or high-functioning autism? (pp. 145–166). New York: Plenum.
Lord, C., & Schopler, E. (1989). The role of age at assessment, developmental level, and test in the stability of intelligence scores in young autistic children. Journal of Autism and Developmental Disorders, 19(4), 483–499. doi:10.1007/BF02212853.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism diagnostic interview-tevised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorder. Journal of Autism and Developmental Disorders, 24. doi:10.1007/BF/02172145.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Leventhal, B. L., DiLavore, P. C., Pickles, A., Rutter, M. (2000). The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficitis associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223.
Lord, C., Risi, S., DiLavore, P. S., Shulman, C., Thrum, A., & Pickles, A. (2006). Autism from 2 to 9 years of age. Archives of General Psychiatry, 63, 694–701.
Lord, C., Rutter, M. D., DiLavore, P. C., Risi, S., Gotham, K., & Bishop, S. L. (2012). Autism diagnostic observation schedule, 2nd edition (ADOS-2). Torrence: Western Psychological Services.
McGovern, C. W., & Sigman, M. (2005). Continuity and change from early childhood to adolescence in autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 46(4), 401–408. doi:10.1111/j.1469-7610.2004.00361.x.
Moore, V., & Goodson, S. (2003). How well does early diagnosis of autism stand the test of time? Autism: The International Journal of Research and Practice, 7(1), 47–63.
Mullen, E. M. (1995). Mullen scales of early learning. Circle Pines, MN: American Guidance Service.
Nordin, V., & Gillberg, C. (1998). The long-term course of autistic disorders: Update on follow-up studies. Acta Psychiatrica Scandinavica, 97, 99–108. doi:10.1111/j.1600-0447.1998.tb09970.x.
Ozonoff, S., Young, G. S., Landa, R. J., Brian, J., Bryson, S., Charman, T., & Iosif, A. M. (2015). Diagnostic stability in young children at risk for autism spectrum disorder: A baby siblings research consortium study. Journal of Child Psychology and Psychiatry and Allied Disciplines, 56(9), 988–998. doi:10.1111/jcpp.12421.
Rapin, I. (2003). Value and limitations of preschool cognitive tests, with an emphasis on longitudinal study of children on the autistic spectrum. Brain and Development, 25(8), 546–548. doi:10.1016/S0387-7604(03)00127-X.
Siegel, D., Minshew, N., & Goldstein, G. (1996). Wechsler IQ Profiles in Diagnosis of high-functioning autism. Journal of Autism and Developmental Disorders, 26(4), 389–406
Sigman, M., Ruskin, E., Arbelle, S., Corona, R., Dissanayake, C., Espinosa, M., Zierhut, C. (1999). Continuity and change in the social competence of children with autism, Down syndrome, and developmental delays. Monographs of the Society for Research in Child Development, i–139.
Smith, T., & Iadarola, S. (2015). Evidence base update for autism spectrum disorder. Journal of Clinical Child & Adolescent Psychology, 44(6), 897–922. doi:10.1080/15374416.2015.1077448.
Starr, E. M., Popovic, S., & Mccall, B. P. (2016). Supporting children with autism spectrum disorder at primary school: Are the promises of early intervention maintained? Current Developmental Disorders Reports, 46–56. doi:10.1007/s40474-016-0069-7.
Stevens, M. C., Fein, D. A., Dunn, M., Allen, D., Waterhouse, L. H., Feinstein, C., & Rapin, E. (2000). Subgroups of children with autism by cluster analysis: a longitudinal examination. Journal of the American Academy of Child & Adolescent Psychiatry, 39(3), 346–352. doi:10.1097/00004583-2000030000-00017.
Sutera, S., Pandey, J., Esser, E. L., Rosenthal, M. A., Wilson, L. B., Barton, M., & Fein, D. (2007). Predictors of optimal outcome in toddlers diagnosed with autism spectrum disorders. Journal of Autism and Developmental Disorders, 37(1), 98–107. doi:10.1007/s10803-006-0340-6.
Szatmari, P., Georgiades, S., Duku, E., Bennett, T. A., Bryson, S., Fombonne, E., Elsabbagh, M. (2015). Developmental trajectories of symptom severity and adaptive functioning in an inception cohort of preschool children with autism spectrum disorder. JAMA Psychiatry. doi:10.1001/jamapsychiatry.2014.2463.
Turner, L. M., & Stone, W. L. (2007). Variability in outcome for children with an ASD diagnosis at age 2. Journal of Child Psychology and Psychiatry and Allied Disciplines, 48(8), 793–802. doi:10.1111/j.1469-7610.2007.01744.x.
Turner, L. M., Stone, W. L., Pozdol, S. L., & Coonrod, E. E. (2006). Follow-up of children with autism spectrum disorders from age 2 to age 9. Autism: The International Journal of Research and Practice, 10(3), 243–265. doi:10.1177/1362361306063296.
Wechsler, D. (1999). The Wechsler abbreviated scale of intelligence. London: Pearson Assessment.
Acknowledgements
This research was not funded. Special acknowledgements to the families involved in the study and to the second and third authors for their guidance, support and contribution to this research project.
Author contributions
All authors made a substantial contribution to conception and design, drafting and revising of the article prior for publication. Authors have been listed in order of their contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Megan L. E. Clark, Josephine Barbaro and Cheryl Dissanayake declare a potential conflict of interest with Dr Giacamo Vivanti who was formally affiliated with the Olga Tennison Autism Research Centre.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all participant’s parents.
Rights and permissions
About this article
Cite this article
Clark, M.L.E., Barbaro, J. & Dissanayake, C. Continuity and Change in Cognition and Autism Severity from Toddlerhood to School Age. J Autism Dev Disord 47, 328–339 (2017). https://doi.org/10.1007/s10803-016-2954-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-016-2954-7