Abstract
Objective The study was to examine nonverbal communication in young children with autism. Methods The participants were 23 young children with autism (mean CA = 32.79 months), 23 CA and MA-matched children with developmental delay and 22 18–20-month-old, and 22 13–15-month-old typically developing toddlers and infants. The abbreviated Early Social Communication Scales [Mundy et al. 1996, Early social communication scales (ESCS)] were used to test three types of nonverbal communicative skills, i.e., joint attention, requesting, and social interaction. Both frequency and proportion analyses were done in group comparisons. Results (1) Two- to three-year-old children with autism displayed deficits in joint attention ability, especially high-level skills. (2) The deficit in terms of frequency of communication was marked even compared with typically developing infants with younger mental age. (3) Young children with autism had different nonverbal communication profile compared with all three comparison groups. Conclusion Early social-communicative difficulties in autism involve early triadic communications involving joint attention and possibly dyadic turn-taking skills, which has implications for both early screening and early intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism is a neurodevelopmental disorder characterized by the early onset of impairments in reciprocal social interaction and communication and restricted repetitive behaviors or interests (Lord and Bailey 2002). Among the many psychological hypotheses explaining the psychopathology of autism, the deficit in joint attention is a prominent one used to explain its social and communicative deficits (Mundy 1995). There have been many reports supporting the unique impairment in both initiating and responding joint attention in infants to toddlers (Charman et al. 1997; Naber et al. 2008; Osterling et al. 2002; Sullivan et al. 2007), young children age before 3 years (DiLavore and Lord 1995; MacDonald et al. 2006; Rutherford and Rogers 2003; Stone et al. 1997); children before 4 years (Baron-Cohen 1989; Dawson et al. 2004; McDonald et al. 2006; Mundy et al. 1994; Sigman and Ruskin 1999; Toth et al. 2006), children before 5 years (Leekam and Ramsden 2006; Leekam et al. 2000; Mundy et al. 1986; Sigman et al. 1986), and children above 5 years (Attwood et al. 1988; Curcio 1978; Sigman and Ruskin 1999; Sigman and McGovern 2005; Wetherby and Prutting 1984). These studies showed that: (1) young children with autism display deficits in both initiating and responding joint attention, but the latter may remit with development; (2) higher IQ and lower mental age (MA) may be related to different joint attention deficits manifested by children with autism; (3) deficits of joint attention were observed from infants to adolescents in autism; (4) joint attention skills were concurrently associated with language and predicted long-term gains in expressive language.
The reports cited above have been very helpful in identifying specific deficits in joint attention by children with autism age 4–8 years. But the joint attention deficits in children with autism younger than 3 years of age are still inconclusive. Several studies using semi-structured or structured play-based methodology focused on the ages under 3 have been reported.
DiLavore and Lord (1995) found that five items from PL-ADOS (Pre-Linguistic Autism Diagnostic Observation Scale; DiLavore et al. 1995): two items for requesting and three items for joint attention, differentiated 2-year-old children with autism (mean CA = 32.0 months, mean MA = 18.5 months) from well-matched clinical controls, including in socially directed requests (i.e., eye contact coordinated with gesture and vocalization), initiation of and responses to joint attention However, longitudinal analyses revealed that by ages 4–5 years, the group with autism was different from the other groups only on initiating joint attention. Stone et al. (1997) developed the Prelinguistic Communication Assessment for measuring nonverbal communication. They found young children with autism (mean CA = 32.8 months, mean MA = 17 months) requested more often and commented less often than controls, and the group with autism also used less complex combinations of behaviors to communicate. Charman et al. (1997) using three active toy tasks ostensibly involving joint attention, found that 20-month-old children with autism (mean CA = 20.7 months, mean NVMA = 17.1 months) were impaired on alternate gaze, one form of joint attention. Rutherford and Rogers (2003), using the Early Social Communication Scales (ESCS, Mundy et al. 1996) for measuring nonverbal communication, found that young children with autism (mean CA = 33.93 months, overall mean MA = 20.01 months) manifested impairment on general joint attentional abilities. MacDonald et al. (2006) used a highly structured assessment protocol, which modified from ESCS and followed two groups with autism and typically development, aged 2–4. They found children with autism had relatively minor deficits in responding joint attention and more severe deficits in initiating joint attention. Naber et al. (2008) using two types of joint attention tasks with experimenter and subject’s mother and found children with autism spectrum disorders showed significantly less joint attention, including basic joint attention (frequencies of pointing and gaze following), associate Joint Attention (frequencies of following pointing and checking), and joint visual attention (joint attentional behaviors appeared during tasks, counted by percentage of time) at the age of 24 months. However, they reached about the same level of joint attention except for joint visual attention at the age of 42 months. These studies reveal that the constellation of communicative behaviors changes with age in young children with autism in the western culture. In this paper, we examined the joint attention deficits in very young children with autism from a eastern culture, Taiwanese children.
In order to examine these nonverbal communicative abilities, we used the abbreviated version of the ESCS (Mundy et al. 1996) as the assessment tool. For better exploration of early social communication in young children with autism, two strategies in methodology were used. First, we recruited three comparison groups, one clinical comparison group of developmental delay (DD) matched for CA and MA, and two typically developing groups, one MA matched to the autism and DD groups, and the other was 13–15 months old. The reason for recruiting the younger group with typical development was to examine the joint attention deficits in young children with autism whose MA passed the normal joint attention consolidation phase, 13–15 months reported by Adamson and McAuthor (1995) for typical development. Second, Stone et al. (1997) used rate, or proportion analyses of communicative acts to examine the nature of communication deficits in children with autism. We adopt this strategy to examine the nonverbal communication profile among our four groups of subjects. We hypothesized that young children with autism were not only having less communicative acts, especially in joint attention, but also having different communicative profile. We believe that this design will deepen our understanding of early socio-communication skills in young children with autism.
Method
Participants
The subjects were 104 children and infants. There were 28 children with autism, 24 with DD, 27 13–15-month old typically developing infants (TD1), and 25 18–20-month old typically developing children (TD2). The former two groups were recruited of four medical centers in northern Taiwan from child psychiatric outpatient clinics The children with autism group had received clinical diagnosis of autistic disorder using DSM-IV (APA 1994) and ICD-10 (WHO 1992) criteria by senior child psychiatrists. Diagnoses DD included speech and language delay (n = 10, 42%), Down’s syndrome (n = 3, 12%), and unspecified mental retardation (n = 11, 46%). All of the two clinical groups participated in early intervention program in hospitals (for autism, n = 21; for DD, n = 1), special preschools (for autism, n = 4; for DD, n = 13), or normal preschools (for autism, n = 3; for DD, n = 10). The two typical groups were recruited from preschools and pediatric clinics. Informed consent was obtained from parents prior to participation. These infants and children had no known physical, sensory, or mental handicap. They were full term (38 ± 2 weeks gestation) and normal birth weight (2,500–4,000 g). Several children did not complete the test battery due to fatigue or distress and were dropped out of the study, including five children with autism, one child with DD, four in the TD1, and three in the TD2. In addition, equipment failure involved one TD1 subject. Thus, 90 children completed the tasks: 23 with autism (22 boys and 1 girl), 23 with DD (12 boys and 11 girls), 22 TD1 (14 boys and 8 girls), and 22 TD2 (10 boys and 12 girls). For measuring participants’ mental function whose chronological age were under three and half years old, Bayley Infant Development Scale (Bayley 1993) was a suitable tool for the purpose. Table 1 presents descriptive and matching information in four groups. There were significant differences among the four groups in CA, MA, and IQ, (F(3,86) = 108.67, p < .001; F(3,86) = 12.45, p < .0001; F(3,86) = 86.52, p < .0001). As expected, post hoc comparison (Tukey HSD) showed TD1 was the youngest than children with autism, DD and TD2 groups (p < .01) in CA, and the groups with autism and DD had lower IQ scores than TD1 and TD2 groups (p < .01). In terms of MA, TD1 group had significantly lower scores than the other three groups (p < .01). There was no significantly differences in parents’ socioecomonic status, based on Hollingshead Two Factor Index of Social Status (Hollingshead 1958, unpublished manuscript) (F(3, 86) = 1.78, p > .05).
Procedures
This study is part of a larger longitudinal study by the first two authors and included three socio-cognitive tasks. Each child was seen twice with one or more of his or her parents in a university-based laboratory. The first visit measured child’s nonverbal communicative skills and other socio-cognitive abilities, and the second visit measured the child’s MA and IQ. We used an abbreviated version of the ESCS (Mundy et al. 1996) for measuring nonverbal communication. During the ESCS administration, the infant and tester were seated directly across from each other at a table. The child was seated on chair or on parent’s lap, facing the tester. A standard set of toys was placed next to the tester, in view of the child. The ESCS was administered in approximately 20 min. The tester presented a series of situations and toys designed to elicit initiations or responses involving requesting, joint attention, and social interaction.
Based on Mundy et al. (1996), we categorized behavior into high and low levels for scoring the child’s development of nonverbal communication. The joint attention category separated by initiating and responding joint attention, involved the coordination of the child’s and tester’s attention to objects or events. In initiating joint attention, these behaviors included Low Level responses involving: (1) eye contact while holding a toy; and (2) alternating eye gaze between the tester’s face and an active toy. High Level responses involved: (3) pointing to toys within reach, and (4) showing toys or extending toys toward the tester’s face. In responding joint attention, a separate index of the child’s capacity to respond appropriately to the tester’s pointing. Two measures were scored. Low Level scores involved responding to proximal pointing, that occurred when the tester points to six trials in two pages from a picture book. The High Level scores involved responding to distal pointing when the tester demonstrates a short-arm pointing across six trials according to whether or not a child turned his or her head (at least 45°) and eyes in the correct direction when the tester pointed to the left, to the right, and behind the child.
The requesting category included behaviors that were used to direct attention to objects or events in order to request aid in obtaining the object or repetition of an event. Here we only coded initiating requesting domain. Behaviors rated Low Level included: (1) eye contact when object moved out of reach or reaching to toys out of reach; and (2) appeal, means eye contact and reaching to toys out of reach. High Level behaviors included: (3) giving a toy to the tester, defined as extending a toy toward the experimenter’s hand; and (4) pointing, extending index finger to toys that were out of reach.
The social interaction behaviors separated by initiating and responding social interaction, involved eliciting attention or physical contact from the tester and engaging in turn-taking with objects. In initiating social interaction, no lower versus higher level behaviors are rated following Mundy et al. (1996). Behaviors observed within this category included: (1) initiates turn-taking, rolling car or ball back to the tester when the child receive it, (2) teases, engaging in a prohibited activity while smiling and making eye contact with the tester, (3) initiates song/tickle, rating after the first song/tickle task has been presented and the child makes eye contact and other gestures, claps, finger crossing table, or sings. In responding social interaction, Behaviors rated Low Level included: (1) eye contact when the tester has tickled the child and moved back to pause before next tickle episode; and (2) act, means vocalize or bang the table or reaching to the tester; and (3) appeal, combining an act with eye contact. Behaviors rated High Level included: (4) maintains turn-taking, highest number of consecutive turns is scored and coded 0 (no turn), 1 (one to three turns) and 2 (four or more turns); and (5) placing the hat, comb, and/ or glasses to the tester’s head after the tester leans forward and says “Can I play.” Because we rarely observed “tease” from our subjects in all four groups, we will not count this category of social interaction in this study.
To assess the interrater reliability of the ESCS in this study, 24 videotapes (26%) were randomly selected from four groups and rated by three independent observers, who did not attend the experiment and were blind to diagnosis of the subjects, to assess multiple rater agreement with generalizability analyses. Generalizability coefficients above .50 indicate adequate reliability (Mitchell 1979; Shavelson and Webb 1991). The generalizability coefficients for the low and high-level scores used in this study ranged from .60 (low level responding social interaction) to .98 (high level responding social interaction). The mean of the generalizability coefficients was .87.
Results
Preliminary Analysis
A one-way ANOVA revealed that the duration of the ESCS testing did not differ across the four groups (F(3, 86) = .31, p > .05). The mean duration of ESCS testing was 20.3 min (SD = 2.82) for the group with autism, 19.9 min (SD = 3.87) for DD, 20.2 min (SD = 2.42) for TD2, and 20.0 min (SD = 2.36) for TD1. There was a significant difference in the average number of nonverbal communicative acts in four groups in ESCS (F(3, 86) = 22.46, p < .001). The mean number of nonverbal communicative acts was 28.09 (SD = 12.00, range = 5–50) for autism group, 59.96 (SD = 19.42, range = 18–96) for DD, 61.86 (SD = 14.12, range = 36–94) for TD2 and 62.41 (SD = 18.73, range = 39–105) for TD1. Post hoc analysis (Tukey HSD) revealed that children with autism had significantly fewer nonverbal communication than the children in other three groups (p < .001), while the latter three groups did not differ.
In the following, we provide two types of analyses. The first focused on frequency of three types of nonverbal communication among four groups, as most studies had done. Second, we compared the proportion of three types of initiating nonverbal communication among the four groups. The major reason for the proportional analysis is to examine whether communicative patterns are similar or different in children with autism, independent of the frequency of their communications.
Comparison of Group Frequency Data
To examine group differences, Multivariate Analysis of Variance (MANOVA) was computed using the behavioral frequency scores from each level of categories of nonverbal communication. There were significant effects of group difference (Wilk’s Lamda = .44, p < .001). These were followed by group comparisons in each level of nonverbal communication categories.
Table 2 shows the frequency of High/Low level of three categories of nonverbal communication in four groups. Analyses revealed significant group effect for Low Level of initiating joint attention (F(3, 86) = 6.61, p < .001) and High Level of initiating joint attention (F(3, 86) = 6.29, p < .001). Pairwise group contrasts revealed that the young children with autism displayed deficits on Low Level initiating joint attention compared to other three groups (p < .01), as well as impairments on High Level initiating joint attention compared to DD and TD2 groups (p < .01). In addition, TD2 group displayed significantly more High Level initiating joint attention acts (p < .05) than the TD1 group.
Analyses of the High- and Low-Level responding joint attention revealed similar significant group effects (F(3, 86) = 10.73, p < .001; F(3, 86) = 11.86, p < .001). Post hoc analysis revealed that young children with autism displayed significantly fewer proximal points than children of other three groups (for TD2 and DD, p < .01; for TD1, p < .05), and also a significant deficit in the capacity to follow others’ pointing relative to all three other groups (p < .01). In addition, TD2 group also demonstrated more number of proximal pointing than TD1 group (p < .05).
Analyses of the initiating requests revealed significant group differences on Low Level requesting (F(3, 86) = 9.27, p < .001) and High Level requesting (F(3, 86) = 5.64, p < .01). Pairwise contrasts revealed that young children with autism displayed fewer Low and High level requests than TD2 (for low level, p < .01; for high level, p < .05) and TD1 (for Low and High levels, p < .01) groups.
Analyses of the social interaction data revealed significant group effects for both of initiating social interaction (F(3, 86) = 14.04, p < .001) and Low Level responding social interaction (F(3, 86) = 6.54, p < .01) as well as High Level social interaction (F(3, 86) = 4.63, p < .01). Pairwise contrasts revealed that children with DD group displayed more initiating social interaction than children with autism group and both of typically developing groups (p < .05). Within the data on the two level of responding behaviors, post hoc analyses indicated that young children with autism were significantly impaired on Low Level social interaction compared to all three other groups (p < .05) and impaired on High Level social interaction when compared to the group with DDs (p < .05).
Profile Analysis of Group Comparison for Frequency Data
A MANOVA with different groups (autism, DD, TD1, and TD2) as the between-subjects factor, and nonverbal communication categories as the within-subjects factor for tests of parallelism, equality, and levels of profile revealed main effect of the groups (Wlik’s Lambda = .35, p < .0001; F(3, 86) = 24.09, p < 0.001; Greenhouse-Geisseer = 69.19, p < .0001) (Johnson and Wichern 1998). Pairwise comparisons for equality found that young children with autism manifested significantly different patterns than those with DD, TD1 and TD2 (p < .0001, multiple comparisons were adjusted by the Bonferroni method), and the latter groups did not differ from each other.
Comparison of Group Proportion Data
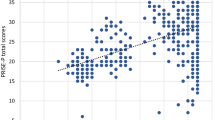
In order to examine the ways in which young children with autism used nonverbal communication in comparison to the other three groups; proportions were calculated for each area of interest from the total corpus of their initiating communication acts. Figures 1 and 2 show the proportion of Low- and High-level of initiating nonverbal communication in four groups. Analyses revealed a significant group effect on High Level joint attention (F(3, 86) = 5.489, p < .01), but not on Low Level joint attention (F(3, 86) = .507, p > .05). Pairwise group contrasts revealed that young children with autism displayed proportionately fewer High Level of initiating joint attention behaviors compared to DD and TD2 groups (p < .05). TD2 group had higher proportion of High Level of initiating joint attention skills than TD1 group (p < .05).
High and Low Level of nonverbal communication (frequency). AC, autistic children (N = 23); DD, developmental delay (N = 23); TD1, 13–15 months typical (N = 22); TD2, 18–20 months typical (N = 22); IJA-L, initiating joint attention—low; IJA-H, initiating joint attention—high; RJA-L, responding joint attention—low; RJA-H, responding joint attention—high; IR-L, initiating requesting—low; IR-H, initiating requesting—high; ISI, initiating social interaction; RSI-L, responding social interaction—low; RSI-H, responding social interaction—high. Equality of profiles test showed that there was a main effect of the between group (F(3, 86) = 24.09, p < .001). There were significant difference in the frequency of nonverbal communication between AC and DD (p < .001), TD1 (p < .001), and TD2 (p < .001) (multiple comparisons were adjusted by the Bonferroni method)
High and Low Level of initiating nonverbal communication (proportion). Note. AC, autistic children (N = 23); DD, developmental delay (N = 23); TD2, 18–20 months normal (N = 22); TD1, 13–15 months normal (N = 22); IJA-L, initiating joint attention—low; IJA-H, initiating joint attention—high; IR-L, initiating requesting—low; IR-H, initiating requesting—high; ISI, initiating social interaction. * p < .05; ** p < .01
Analyses of the requesting data revealed no significant group differences on proportions of Low- and High-level requests (for low level, F(3, 86) = 1.656, p > .05; for high level, F(3,86) = .939, p > .05). However, since we were interested in comparing the two main groups, pairwise group contrasts were carried out and revealed that young children with autism displayed significant higher proportion of Low Level requests than the DD group (p < .05).
Analysis of initiating social interaction revealed significant group differences (F(3, 86) = 7.32, p < .01). Pairwise comparisons found children with DD group had significant higher proportion than children with autism, and other two typically developing groups (p < .05).
Discussion
This study examined the nonverbal communicative skills in young children with autism, relative to two MA-matched children with DD and 18–20 months typically developing toddlers (TD2), and one lower-MA typically developing infants aged 13–15 months (TD1). The results demonstrated that, in both frequency and proportion of communicative acts used, young children with autism revealed deficits on initiating joint attention, especially on high-level skills. However, compared to lower-MA typically developing infants, young autistic children displayed fewer number in most categories of nonverbal communication. In addition, profile analysis found that young children with autism displayed unequal pattern in nonverbal communication comparing with two MA-matched groups and even lower MA infants with typical development. Thus, these results demonstrated that young children with autism demonstrated a pattern of deviant development in their use of different types of nonverbal communications, and a decreased frequency, above and beyond what could be explained by their general mental age.
The frequency data revealed that these 2- and 3-year-old children with autism revealed deficits in both of initiating and responding joint attention compared to MA-matched comparison groups of both typically developing and developmentally delayed children. This finding replicates earlier findings that demonstrated that the nonverbal communication difficulties in young children with autism seemed only limit to joint attention, or a kind of triadic behaviors for sharing (McDonald et al. 2006; Mundy et al. 1986, 1994). Mundy et al. (1994) indicated that when MA lower than 20 months, both low and high levels of initiating joint attention and high level of responding joint attention were impaired comparing with controls. In our study, the mean MA was 22 months in children with autism, most participants with autism were lower than 20 months in MA (16/23). Thereby, it was not surprised to find the similar results. Young children with autism around 2–3 years of age, not only impaired on high level of initiating joint attention, but also have deficiency in low level of responding joint attention, i.e., responding to proximal point by an adult.
In addition, we also found that young children with autism manifested lower frequency in low level of responding social interaction. This result was similar with earlier study (Mundy et al. 1986) but not others (Sigman and Ruskin 1999). However, the developmental issue was needed to highlight. Regarding the low level of responding social interaction, which recorded eye contact, vocalization, and combining both responded by the child when tester involved tickle game. The behaviors are dyadic-based, or person-to-person interaction and not involve object between them and developed before 6 months in typical development (for a review, Hobson 2002). Although we understand that ESCS is not good tool to measure dyadic interaction and most of the items, even in social interaction were designed for triadic interaction, i.e., person-object-person interaction. We argued that when young children with autism aged 2–3 years, the deficit of dyadic interaction, like turn-taking skills should be underscored.
By examining the proportion of each type of nonverbal communications, young children with autism displayed lower proportion on high level joint attention compared with two MA-matched children with clinical and typically developmental groups. In addition, comparing with clinical comparison group (DD group), the data revealed that young children with autism used a higher proportion on low level of initiating requests and social interactions, replicating Stone et al. (1997). The proportions of their various types of communications in the group with autism resembled the proportions seen in our group of 13–15 month olds typically developing children, though their frequencies were lower.
These findings contribute to our understanding of the unique impairment of social engagement seen in early autism. Mundy (1995) suggested a model that contrasted children’s social-emotional approaches with their object approaches in early cognitive development. He suggested that initiating joint attention bids is prototypical of social-emotional approach behavior, while initiating requests is prototypic of object approach behavior. Children with autism reveal abnormalities in the development of the former, but not the latter. We agree with his suggestion, but we wish to extend it somewhat. Theories of typical development of joint attention behavior suggest that dyadic interactions, both with a social partner, and with objects, provide a foundation for later triadic communications, in which self, partner, and object come together (Adamson and Bakeman 1991; Hobson 1993, 2002). We suggest that in autism, difficulties in joint attention behavior reflect earlier developing problems in dyadic engagement, which are present in infants and toddlers with autism but mature somewhat in the preschool years. Thus, depending on the age of the sample, one may or may not detect deficits in dyadic communications in the ESCS. The present data mirror such findings reported by others studying very young samples. For instance, Wimpory et al. (2000) reported similar deficits in dyadic engagement using a semistructured interview for parents, the Detection of Autism by Infant Sociability Interview. They found infants with autism (during first 24 months) differed from those of the control group on 16/19 items. Some of the items, like “greeted parents,” “enjoyed lap games,” “preverbal turn-taking,” are typical dyadic socially interactive behaviors, which the parents believed were abnormal during their infants’ first 2 years of life, as were the children’s responses to joint attention. Wimpory et al. (2000) suggested that the infants with autism have marked limitations in both person-to-person and person-person-object social engagement. Our current findings support this suggestion.
The final point to be discussed concerns the theoretical perspective involving another aspect of dyadic interaction, that of social orienting. Dawson and colleagues (Dawson et al. 1998, 2004) used two kinds of stimuli to elicit visual orienting, one that involved social stimuli (name called, hand clapping, etc.), and the other involving nonsocial stimuli (a time beeping, a whistle, etc.). They reported repeatedly that, compared to children with DD or Down syndrome and typical development, children with autism more frequently failed to orient to all stimuli, and that this failure was much more extreme for social stimuli. Leekam et al. (2000, 2006) found children with autism were less responsive than developmentally delayed controls in orienting to attention bids (vocal and non-vocal) and in following a human head-turn cue. These studies demonstrated additional aspects of social dyadic deficits in young children with autism. We suggest that the social impairment in autism possibly begins at the level of dyadic engagement, rather than difficulties with joint attention and coordination of mental states. Current work focused on studies of infant development of autism should help us clarify the developmental profile of the social and communicative impairments in autism.
It is important to consider the limitations of this study. First, while both groups of clinical subjects were diagnosed and referred by the most expert clinicians in Taiwan, we could not obtain standardized autism assessment data from instruments (like the ADOS, or ADI-R) since these had not yet been translated at the time of this study. The clinicians followed current diagnostic practices including the official criteria of DSM-IV (APA 1994) and ICD-10 (WHO 1992). While we feel confident about the diagnoses of these subjects (and expert diagnosis is considered the gold standard), having multiple measures of diagnosis would be helpful. Second, the Bayley Scales of Infant Development have not yet been standardized on a Taiwanese sample or translated in Taiwanese, so that children’s scores were derived from the US norms. While we do not yet have any research on of the effects of cultural differences between Mandarin language versus English language on this scale, we do not know how this would affect scores. However, since all the groups were tested, scored, and matched in the same way, this should not affect the general findings of this study. Third, only using a semi-structured scale, ESCS paradigm for measuring children’s social communication cannot stand for their comprehensive abilities. Further studies are required to include unstructured measures, like parent–child interaction observation and other measures focused on dyadic interaction for strengthening the methodology.
In summary, in this study we demonstrated that 2- and 3-year-old with autism displayed deficits mainly in initiating joint attention, especially in high level skills compared to both typically developing and delayed comparison groups. The deficit in terms of frequency of communication acts was marked even compared with typically developing infants with younger mental age. In addition, the study also showed one type of dyadic interaction, like turn-taking skill was possibly impaired in autism before ages of 3. The observation of very young children with autism and their specific patterns of nonverbal communication have important implications in early diagnosis and intervention. Concerning the early diagnosis of autism, both deficits in the quantity and patterns of the initiating of high joint attention, like pointing and showing, and turn-taking behaviors in social interactions may be key indicators for further screening the diagnosis of autism. In terms of early intervention, we agree with Stone et al. (1997) that interventions should place an emphasis on teaching children to monitor the adult’s attention within the context of requesting situations. In addition, focus on basic dyadic play like turn-taking routines, will facilitate the early sociocommunicative ability in autism. One recent program, the Denver Model (Rogers et al. 2000), emphasizes just this kind of activity, referred to as sensory-social routines, for young children with autism beginning treatment, and this provides a good example of this kind of dyadic engagement.
References
Adamson, L. B., & Bakeman, R. (1991). The development of shared attention during infancy. In R. Vasta (Ed.), Annals of child development (Vol. 8, pp. 1–41). London: Kingsley.
Adamson, L. B., & McArthur, D. (1995). Joint attention, affect, and culture. In C. Moore & P. J. Dunham (Eds.), Joint attention: Its origins and role in development (pp. 205–222). NJ: Lawrence Erlbaum.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th edn.). Washington, DC: Author.
Attwood, A., Frith, U., & Hermelin, B. (1988). The understanding and use of interpersonal gestures by autistic and Downs Syndrome children. Journal of Autism and Pervasive Disorders, 18, 241–257.
Baron-Cohen, S. (1989). Perceptual role taking and protodeclarative pointing in autism. British Journal of developmental Psychology, 7, 113–127.
Bayley, N. (1993). Bayley scales of infant development (2nd edn.). Orlando: The Psychological Corporation.
Charman, T., Swettenham, J., Baron-Cohen, S., Cox, A., Baird, G., & Drew, A. (1997). Infants with autism: an investigation of empathy, pretend play, joint attention, and imitation. Developmental Psychology, 33, 781–789. doi:10.1037/0012-1649.33.5.781.
Curcio, F. (1978). Sensorimotor functioning and communication in mute autistic children. Journal of Autism and Developmental Disorders, 8, 281–292. doi:10.1007/BF01539631.
Dawson, G., Meltzoff, A. N., Osterling, J., Rinaldi, J., & Brown, E. (1998). Children with autism fail to orient to naturally occurring social stimuli. Journal of Autism and Developmental Disorders, 28, 479–485. doi:10.1023/A:1026043926488.
Dawson, G., Toth, K., Abbott, R., Osterling, J., Munson, J., Estes, A., & Liaw, J. (2004). Early social attention impairments in autism: Social orienting, joint attention, and attention to distress. Developmental Psychology, 40, 271–283. doi:10.1037/0012-1649.40.2.271.
DiLavore, P. & Lord, C. (1995). Do you see what I see? Requesting and joint attention in young autistic children. Paper presented in SRCD conference.
DiLavore, P., Lord, C., & Rutter, M. (1995). The pre-linguistic autism diagnostic observation schedule. Journal of Autism and Developmental Disorders, 25, 355–379. doi:10.1007/BF02179373.
Hobson, P. (1993). Autism and the development of mind. Hove, Sussex: Erlbaum.
Hobson, P. (2002). The cradle of thought: Exploring the origins of thinking. NY: Oxford University Press.
Johnson, R. A., & Wichern, D. W. (1998). Applied multivariate statistical analysis. NJ: Prentice-Hall International, Inc.
Leekam, S. R., Lopez, B., & Moore, C. (2000). Attention and joint attention in preschool children with autism. Developmental Psychology, 36, 261–273. doi:10.1037/0012-1649.36.2.261.
Leekam, S. R., & Ramsden, A. H. (2006). Dyadic orienting and joint attention in preschool children with autism. Journal of Autism and Developmental Disorders, 36, 185–197. doi:10.1007/s10803-005-0054-1.
Lord, C., & Bailey, A. (2002). Autism spectrum disorders. In M. Rutter & E. Taylor (Eds.), Child and adolescent psychiatry (4th edn., pp. 636–663). London: Blackwell Scientific Publication.
MacDonald, R., Anderson, J., Dube, W., Geckeler, A., Green, G., Holcomb, W., Mansfield, R., & Sanchez, J. (2006). Behavioral assessment of joint attention: A methodological report. Research in Developmental Disabilities, 27, 138–150. doi:10.1016/j.ridd.2004.09.006.
Mitchell, F. (1979). Interobserver agreement, reliability, and generalizability of data collected in observational studies. Psychological Bulletin, 86, 376–390. doi:10.1037/0033-2909.86.2.376.
Mundy, P., Hogan, A., & Doehring, P. (1996). Early social communication scales (ESCS) (A preliminary manual for the abridged).
Mundy, P. (1995). Joint attention and social-emotional approach behavior in children with autism. Development and Psychopathology, 7, 63–82.
Mundy, P., Sigman, M., & Kasari, C. (1994). Joint attention, developmental level, and symptom presentation in autism. Development and Psychopathology, 6, 389–401.
Mundy, P., Sigman, M., Ungerer, J. A., & Sherman, T. (1986). Defining the social deficits in autism: The contribution of non-verbal communication measures. Journal of Child Psychology and Psychiatry, 27, 657–669. doi:10.1111/j.1469-7610.1986.tb00190.x.
Naber, F. B. A., Bakermans-Kranenburg, M. J., van IJzendoorn, M. H., Dietz, C., van Daalen, E., Swinkels, S. H. M., Buitelaar, J. K., & van Engeland, H. (2008). Joint attention development in toddlers with autism. European Journal of Child and Adolescent Psychiatry, 17, 143–152.
Osterling, J., Dawson, G., & Munson, J. (2002). Early recognition of 1-year-old infants with autism spectrum disorder versus mental retardation. Development and Psychopathology, 14, 239–251. doi:10.1017/S0954579402002031.
Rogers, S. J., Hall, T., Osaki, D., Reaven, J., & Herbison, J. (2000). The Denver model: A comprehensive, integrated educational approach to young children with autism and their families. In J. S. Handleman & S. L. Harris (Eds.), Preschool education programs for children with autism (pp. 95–134). Austin, TX: Pro-Ed.
Rutherford, M. D., & Rogers, S. J. (2003). Cognitive underpinning of pretend play in autism. Journal of Autism and Developmental Disorders, 33, 289–302. doi:10.1023/A:1024406601334.
Shavelson, R. J., & Webb, N. M. (1991) Generalizability theory: A primer. Newbury Park: SAGE Publications, Inc.
Sigman, M., Mundy, P., Sherman, T., & Ungerer, J. A. (1986). Social interactions of autistic, mentally retarded and normal children with the caregivers. Journal of Child Psychology and Psychiatry, 27, 647–669. doi:10.1111/j.1469-7610.1986.tb00189.x.
Sigman, M., & McGovern, C. W. (2005). Improvement in cognitive and language skills from preschool to adolescence in autism. Journal of Autism and Developmental Disorders, 35, 15–23.
Sigman, M., & Ruskin, E. (1999). Social competence in children with autism, down syndome, and other developmental delays. In Monograph of the Society for Research in Child Development (Serial No. 256, Vol. 64, No. 1). Chicago, IL: University of Chicago Press.
Stone, W. L., Ousley, O. Y., Yodar, P. J., Hogan, K. L., & Hepburn, S. L. (1997). Nonverbal communication in two- and three-year-old children with autism. Journal of Autism and Developmental Disorders, 27, 677–696. doi:10.1023/A:1025854816091.
Sullivan, M., Finelli, J., Marvin, A., Garrett-Mayer, E., Bauman, M., & Landa, R. (2007). Response to joint attention in toddlers at risk for autism spectrum disorders: A prospective study. Journal of Autism and Developmental Disorders, 37, 37–48. doi:10.1007/s10803-006-0335-3.
Toth, K., Munson, J., Meltzoff, X., & Dawson, G. (2006). Early predictors of communication development in young children with autism spectrum disorders: joint attention, imitation, and toy play. Journal of Autism and Developmental Disorders, 36, 993–1005. doi:10.1007/s10803-006-0137-7.
Wetherby, A., & Prutting, C. (1984). Profile of communicative and cognitive-social abilities in autistic children. Journal of Speech and Hearing Research, 27, 364–377.
Wimpory, D. C., Hobson, R. P., Williams, J. M., & Nash, S. (2000). Are infants with autism socially engaged? A study of recent retrospective parental reports. Journal of Autism and Developmental Disorders, 30, 525–536. doi:10.1023/A:1005683209438.
World health Organization (WHO). (1992). The ICD-10 classification of mental and behavioral disorders: Clinical descriptions and diagnostic guidelines. Geneva: Author.
Acknowledgments
This research was part of dissertation by the first author, and part of the autism projects by the first two authors. The studies were supported by National Science Council in Taiwan (NSC-88-2413-H002-008, NSC-89-2413-H002-53 and NSC-92-2413-194-031). Dr. Rogers was supported in part by the National Institute of Child and Human Development award #HD35468 in USA. We thank Chi-Lin Huang for help data collection, and the children and their parents whose participation made the study possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chiang, CH., Soong, WT., Lin, TL. et al. Nonverbal Communication Skills in Young Children with Autism. J Autism Dev Disord 38, 1898–1906 (2008). https://doi.org/10.1007/s10803-008-0586-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-008-0586-2