Abstract
Early communication impairment is among the most-reported first concerns in parents of young children with autism spectrum disorder (ASD). Using a parent-report questionnaire, we derived trajectory groups for early language and gesture acquisition in siblings at high risk for ASD and in children at low risk, during their first 2 years of life. Developmental skills at 6 months were associated with trajectory group membership representing growth in receptive language and gestures. Behavioral symptoms also predicted gesture development. All communication measures were strongly related to clinical and developmental outcomes. Trajectory groups further indicated slowest language/gesture acquisition in infants with later ASD diagnoses, in particular when associated with language delay. Overall, our results confirm considerable variability in communication development in high-risk infants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reduced verbal and nonverbal communication skills, together with differences in social interaction and the presence of restricted and repetitive behaviors represent core features of autism spectrum disorder (ASD) (American Psychiatric Association 2013). The clinical manifestations and onset of ASD symptoms during infancy show significant variability (Bryson et al. 2007; Estes et al. 2015; Ozonoff et al. 2008; Piven et al. 2017; for a review, see, Rogers 2009). Prospective studies including high-risk siblings (HR-Sibs) of children with ASD compared to low-risk infants (LR) represent a widely recognized method allowing observation of the early emergence of ASD symptomatology and other communication-related differences. In fact, the rate of ASD diagnoses in HR-Sibs rises to 18.7% and an additional 28% of HR infants show sub-clinical manifestations of ASD or developmental impairments (e.g., language delays, LangD; Messinger et al. 2013; Ozonoff et al. 2011, 2014).
Prospective studies involving comparison of HR-Sibs to LR infants have evidenced atypicalities since the first year of life in various developmental domains, including reduced interest in social stimuli (Chawarska et al. 2013; Jones and Klin 2013), reduced activity level (Zwaigenbaum et al. 2005), atypical verbal expression (Paul et al. 2011), motor delays (Flanagan et al. 2012), and increased parental concerns (Sacrey et al. 2015). However, diagnostic predictability and specificity of signs for ASD become consistent only from the first birthday (Zwaigenbaum et al. 2005; for a review see, Jones et al. 2014).
Language and communication concerns (e.g., delayed language onset) are the most common reasons for clinical consultation by parents of children with ASD (Bolton et al. 2012; DeGiacomo and Fombonne 1998; Richards et al. 2016). Moreover, consistent evidence indicates language impairment in most young children with ASD (e.g., Charman et al. 2003b, c; Volden et al. 2011). Therefore, many studies on HR-Sibs have focused on verbal and nonverbal communication development (Iverson et al. 2017; Landa et al. 2007; Mitchell et al. 2006; Parlade and Iverson 2015; Stone et al. 2007; Yirmiya et al. 2006). Overall, these studies have demonstrated that HR-Sibs show reduced language and communicative development compared to LR infants from the first year. Beyond the second year of life, language and communication development further differentiate HR-sibs who will develop ASD (HR-ASD) from HR-Sibs who will not (HR-Non-ASD) (Iverson et al. 2017; Landa et al. 2007; Mitchell et al. 2006; Stone et al. 2007).
Several studies have looked at communication trajectories in HR-Sibs and specifically compared HR-ASD to HR-Non-ASD infants, showing developmental differences between these two groups (Iverson et al. 2017; Landa et al. 2007; Parlade and Iverson 2015; Leonard et al. 2015). In particular, Iverson et al. (2017) demonstrated reduced growth rate of gesture production in HR-ASD, compared to LR infants from the first year. They found a similar reduction in HR-Non-ASD infants with LangD compared to LR infants. From the second year, children’s gains in verbal skill also differentiated HR-ASD, HR-Non-ASD, HR-Non-ASD with LangD, and LR infants (Iverson et al. 2017; Landa et al. 2007; Parlade and Iverson 2015). In sum, these results indicate the importance of exploring variability in language development in HR-Sibs. Existing research highlights the importance of taking into account the potential impact of early communication impairment on ASD symptomatology, as well as on later language impairments. However, whereas previous studies have compared communication development in HR-ASD and HR-Non-ASD infants with LangD, comparisons between HR-ASD infants with or without LangD have been lacking. A better understanding of early communication development among infants later diagnosed with ASD has the potential to inform us about early markers of further language impairments within the disorder, while also contributing to the identification of critical early intervention targets.
Existing longitudinal research has pointed out that both verbal and nonverbal skills (including joint attention, play development, imitation and motor skills) predict verbal development in young children with ASD (Paul et al. 2008; Thurm et al. 2007; Charman et al. 2003b, 2005; Ellis Weismer et al. 2010; Manwaring et al. 2017; Stone and Yoder 2001). Studies in HR-Sibs have further demonstrated the role of motor skills and gaze behavior (more gazing at mouth) from 6 months in predicting language development (Bhat et al. 2012; LeBarton and Iverson 2013; Leonard et al. 2015; West et al. 2017; Young et al. 2009). In turn, language skills also have a critical role in children’s outcomes, predicting cognitive development (Brady et al. 2004; Ray-Subramanian and Ellis Weismer 2012; Szatmari et al. 2003). Taken together, research shows that communication development in ASD can be predicted from the first year, confirming the importance of exploring language development in HR-Sibs as an early marker for general developmental difficulties.
One way of analyzing developmental heterogeneity in clinical samples involves data-driven analytic approaches such as group-based modeling (GBM) in large samples (Jones et al. 2001; Jones and Nagin 2007). This method has been used to examine atypical pathways in cognitive and communication development among ASD-HR and ASD-Non-HR siblings (e.g., Brian et al. 2014; Longard et al. 2017). In this paper, we first aim to explore variability in growth of verbal language (i.e., expressive and receptive) and non-verbal communication (i.e., gestures) from 9 to 24 months, in the most substantial sample to date of HR-Sibs and LR infants. Second, we aim to explore how early clinical and developmental predictors are related to this variability, and to later functioning and ASD symptomatology. We expect to show differences in our communication variables between HR-sibs and LR infants, and predict that this variability will be related to both clinical (ASD symptom) and developmental scores, and to ASD diagnoses. Finally, we also expect that trajectories of communication development will be informative regarding later language difficulties specifically in the children with ASD.
Method
Participants
The sample consisted of 660 participants (361 boys). Among the participants, 482 (266 boys) were infant siblings of children with ASD, and 178 (95 boys) were LR control infants. The sex distribution difference was similar between the two groups (see Table 1). All participants were part of a longitudinal prospective study specifically dedicated to the assessment of infants at HR for ASD (Zwaigenbaum et al. 2005). Participants were recruited at four sites in Canada: IWK Health Centre/Dalhousie University (Halifax), University of Alberta (Edmonton), Bloorview Research Institute (Toronto), and McMaster Children’s Hospital (Hamilton). Participants were all born at 36–42 weeks gestation with a birth weight > 2500 g, and had no specific neurological or genetic conditions or severe sensory/motor impairments. HR infants had an older sibling with a clinical diagnosis of ASD. LR infants were recruited from community sources and had no first- or second-degree relatives with ASD. All participants with relevant data were included in the study. However, participants were pre-selected according to a defined age range for each collection of data on the MacArthur Communicative Development Inventory (M-CDI; Fenson et al. 1993) at 9, 12, 15, 18, 21 and 24 months of age (i.e., from 8.9 to 10.1 for the 9-month visit, from 11.9 to 13.1 for the 1- month visit, etc.) (see Supplementary Table 1 for exact age means). Research Ethics Boards at each of the four sites approved the study protocol, and participants’ parents gave their informed consent before inclusion in the study.
Measures
Vocabulary and Development
MacArthur Communicative Development Inventory, Infant Form (M-CDI; Fenson et al. 1993)
Data on language development were collected at 9, 12, 15, 18, 21 and 24 months of age using the M-CDI, Words and Gestures form. The M-CDI Part I concerns vocabulary production and vocabulary reception (comprehension). Parents mark each word that the child understands or produces, from among a list of 396 words. Part II includes an inventory of 63 gestures composed of early gestures (i.e., first communicative gestures and games and routines) and late gestures (i.e., actions with objects, pretending to be a parent, and imitating other adult actions.) The M-CDI inventory is based on the relative onset of language and gestures in typical development. It is designed for and includes percentiles for 8- to 18-month-olds but has been shown to be effective in exploring language onset in preschoolers with ASD (mean age = 3.2 years, SD = 1.2; Charman et al. 2003c). To account for infants’ vocabulary sizes, we analyzed absolute raw scores as per Charman et al. (2003c), Mitchell et al. (2006) and Iverson et al. (2017). 2 or 3 weeks before each study visit, the M-CDI was mailed to parents. Parents returned the forms by mail or in person on the day of the assessment to ensure chronological proximity to other evaluations.
Predictors and Outcome: Clinical and Developmental Assessments
Data on predictors were collected at 6 months and data on outcomes, which included a diagnostic evaluation, were collected at 36 months of age.
Autism Observation Scale for Infants (AOSI; Bryson et al. 2008)
Data on early clinical concerns were collected using the AOSI at 6 months of age. The AOSI, a semi-structured play-based assessment requiring about 20 min, was developed for research purposes to detect and monitor early signs of ASD in 6- to 18-month-olds. The AOSI provides reliable data for assessing the early emergence of ASD among HR infant siblings (Bryson et al. 2008).
The Mullen Scales of Early Learning (MSEL; Mullen 1995)
Data on developmental skills were collected at 6 and 36 months of age with the MSEL. The MSEL is a standardized assessment of early development from 0 to 68 months, providing an early learning composite (ELC, mean = 100, SD = 15). It covers 5 subdomains: gross motor (GM), fine motor (FM), visual reception (VR), receptive (RL) and expressive language (EL). Standard scores from the MSEL subscales were derived from t scores and used for our primary analyses. The MSEL has shown good internal consistency and test–retest stability (Mullen 1995).
The Autism Diagnostic Observation Schedule-Generic (ADOS; Lord et al. 2000)
Data on severity of ASD symptoms at 36 months were collected using the ADOS. The ADOS represents the gold standard observational measure for ASD symptoms. This assessment is a play-based and semi-structured evaluation of communication, social interaction, and repetitive and restricted behaviors as diagnostic symptoms for ASD. The instrument consists of four modules according to the age and verbal expression level of each child, and shows excellent inter-rater reliability (Lord et al. 2000). Symptom severity scores were obtained using the algorithm by Gotham et al. (2009), allowing for comparison across modules.
Diagnostic Assessment at 36 Months
Autism Spectrum Disorder
Diagnosis at 36 months was based on diagnostic tools (ADOS and Autism Diagnostic Interview-Revised, ADI-R; Rutter et al. 2003) and clinical judgment of an expert clinician blind to previous assessments, using DSM-IV-TR criteria (American Psychiatric Association 2000). See Zwaigenbaum et al. (2012) for a detailed description of the diagnostic procedure.
Language Delay
Language delay (LangD) was defined by receptive and/or expressive standard scores that were at least 1.5 S.D. below the mean, as measured by the MSEL at 36 months of age (also see Mitchell et al. 2006), regardless of other developmental impairments.
Analytic Strategy
Trajectory groups for vocabulary and gesture development (collected with the M-CDI, from 9 to 24 months) were derived using a semi-parametric group-based modeling approach (GBM, SAS PROC TRAJ) (Jones et al. 2001; Jones and Nagin 2007). SAS PROC TRAJ establishes sub-populations of participants from the entire sample based on shared characteristics on longitudinal observations. All the participants with a valid M-CDI assessment were included in the analyses (Nagin 1999; see also; Brian et al. 2014). For each variable (verbal expression, verbal reception, and gestures as measured by raw scores/counts from the M-CDI), the number of trajectories was decided according to the best model fitting the variation in the data (Nagin 1999). An average posterior probability (APP) was further obtained for each group resulting from GMB analyses to verify the accuracy of participants’ allocation in the correct trajectory group. An APP > 0.70 indicates that participants are well assigned to their groups (Nagin 2005). After the establishment of the derived trajectory groups, PROC TRAJ allows the examination of the association of risk factors (predictors) and outcome measures with the derived trajectory groups (Nagin 1999; Jones et al. 2001; Jones and Nagin 2007). According to the PROC TRAJ procedure, coefficient estimates, which represent odds ratios, define the impact that risk factors have on the probability of membership in a specific trajectory group. The dependency between trajectory group membership and outcome measure is further modeled through a linear predictor (see Jones and Nagin 2007). The association of trajectory group membership with the diagnostic outcome at 36 months was evaluated using a Pearson Chi-Square test.
Results
Vocabulary and Gesture Trajectories
Verbal Expression
A 2-group solution was obtained for Verbal Expression (see Fig. 1, also see Supplementary Table 1 for details on point estimates). Trajectory group 1 (“Low”, n = 450, 68.2%; 94 LR and 356 HR) was characterized by slower acquisition of vocabulary production than in Trajectory group 2 (“High”, n = 210, 31.8%; 84 LR and 126 HR). APP for “Low” trajectory group was 0.92 and for the “High” trajectory group was 0.93, indicating high accuracy of group assignment. Comparisons of the estimates of quadratic slopes between the two groups revealed a statistically significant difference. However, estimated intercepts did not differ significantly between the two trajectory groups (see Table 2). Sex distribution within trajectory groups differed significantly between groups (p < 0.001) (74.79% of boys in the “Low” Trajectory group vs. 60.20% of girls).
Verbal Reception
A 3-group solution was obtained for Verbal reception (see Fig. 2, also see Supplementary Table 1 for details on point estimates). Trajectory group 1 indicated slower acquisition (“Low”, n = 215, 32.6%; 26 LR and 189 HR), Trajectory group 2 indicated an intermediate rate of acquisition (“Intermediate”, n = 327, 49.5%; 92 LR and 235 HR) and Trajectory group 3 indicated most rapid acquisition (“High”, n = 118, 17.9%; 60 LR and 58 HR) of receptive vocabulary. APP for “Low” trajectory group was 0.88, for “Intermediate” trajectory group was 0.89 and for “High” trajectory group was 0.90, indicating very good to excellent group assignment. Pairwise comparisons of estimates of quadratic slopes and intercepts between trajectory groups were all statistically significant (see Table 2). Sex distribution differed within trajectories (p < 0.001) (“Low” Trajectory group: 37.67% of boys vs. 26.42% of girls/“High” trajectory group: 11.91% of boys vs. 25.08% of girls).
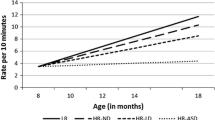
Gesture Production
A 3-group solution was obtained for gesture production (see Fig. 3, also see Supplementary Table 1 for details on point estimates). Trajectory group 1 indicated slower acquisition (“Low”, n = 86, 13.0%; 3 LR and 83 HR), Trajectory group 2 indicated intermediate acquisition (“Intermediate”, n = 339, 51.4%; 73 LR and 266 HR), and Trajectory group 3 indicated most rapid acquisition (“High”, n = 235, 35.6%; 102 LR and 133 HR) of gesture production. APP for the “Low” trajectory group was 0.85, for the “Intermediate” trajectory group was 0.88, and for the “High” trajectory group was 0.88, indicating very good accuracy of group assignment. All pairwise comparisons of the estimates of quadratic slopes between trajectory groups were statistically significantly different, except for the comparison of “Low” and “High” trajectory groups. Estimates of intercepts did not differ between groups (see Table 2). Sex distribution differed within trajectories (p < 0.001) (“Low” trajectory group: 18.00% of boys vs. 7.02% of girls/“High” trajectory group: 26.04% of boys vs. 47.16% of girls).
Predictors and Outcomes
Predictors
We investigated whether predictors (6-month MSEL and AOSI scores) were risk factors for trajectory group membership related to verbal or gesture skills on the M-CDI. Table 3 shows log-odds estimates for each risk factor for each trajectory group relative to the “Low” trajectory group (Nagin 1999, 2005). Concerning verbal reception, our results show that as the MSEL ELC increases, the likelihood of belonging to the verbal reception “High” trajectory group increases as well; this was also true for gross motor and receptive language MSEL subscales (see Table 3). Concerning gesture development, increasing ELC on the MSEL was similarly related to increased probability of belonging to the “High” trajectory group, which also applied to all MSEL subscales except expressive language (i.e., visual reception, receptive language, gross motor and fine motor). Higher AOSI scores were related to a lower probability of belonging to the “High” gesture development trajectory group (see Table 3). No predictors were associated with trajectory group membership for verbal expression (see Table 3).
Outcomes
Table 4 illustrates the mean scores for both MSEL and ADOS scores with 95% confidence intervals (CI) for each trajectory group and each variable, calculated from the φk coefficient estimates and standard errors (Jones and Nagin 2007). Membership in each of our M-CDI trajectory groups (verbal expression, verbal reception, and gestures) was related to both MSEL and ADOS outcomes at 36 months: as the trajectory group represented more rapid communication growth, MSEL scores increased and ADOS scores deceased, indicating better developmental skills and reduced ASD symptom severity. However, the 95% CI overlapped between the “Intermediate” and the “High” verbal reception trajectory groups for ADOS symptom severity and MSEL visual reception, showing no significant differences.
Association Between Trajectories and Diagnostic Classification
Autism Spectrum Disorder
At the 36-month visit, 405 HR and 165 LR children underwent a diagnostic assessment as described above. Of these, 114 participants (all HR; 78 boys) met criteria for an ASD diagnosis (HR-ASD infants). We found a significant association between verbal expression, verbal reception, gesture trajectory group membership and ASD diagnosis, compared to HR-Non-ASD and LR infants. Most children with ASD were in the “Low” trajectory groups for verbal expression and verbal reception, and in the “Intermediate” trajectory group for gesture development (see Table 5; also see Supplementary Table 2 for mean M-CDI scores at each visit for diagnostic group). The same pattern was observed in boys and girls separately (boys: verbal expression, X2 = 14.31, p < 0.001, verbal reception, X2 = 45.54, p < 0.001, gestures, X2 = 41.92, p < 0.001; girls: verbal expression, X2 = 25.05, p < 0.001, verbal reception, X2 = 38.83, p < 0.001, gestures, X2 = 58.17, p < 0.001).
Language Delay in HR-ASD Siblings
At the 36-month visit, 390 HR-Sibs underwent a diagnostic assessment for both ASD and LangD as described above. Of these, 110 participants met criteria for an ASD diagnosis, and 58 participants met criteria for LangD. Among the HR-ASD siblings, 37 (33.6%) also met criteria for LangD (HR-ASD-LangD), and 73 (66.4%) did not meet criteria for LangD (HR-ASD-Non-LangD). When we compared these two groups and their association with communication trajectory groups, a significant association was seen for verbal expression and verbal reception but not Gesture development (see Table 6, also see Supplementary Table 2 for mean M-CDI scores at each visit for diagnostic group). Further analyses observing boys and girls separately revealed the same pattern for boys, with a tendency for girls (boys, n = 23; girls, n = 11) (boys: verbal expression, X2 = 5.51, p = 0.02, verbal reception, X2 = 5.58, p = 0.04, gestures, X2 = 8.84, p = 0.12; girls: verbal expression, X2 = 3.48, p < 0.06, verbal reception, X2 = 5.82, p = 0.05, gestures, X2 = 4.35, p = 0.11). Finally, we verified the distribution among trajectory groups of HR-Non-ASD infants with or without language delay, and found a significant difference only in the distribution of verbal expression (X2 = 10.12, p = 0.001; see Supplementary Table 3).
Discussion
In this study, we examined the variability in growth of communication skills in a large sample of infant siblings at high-risk (HR) for ASD and in low-risk infants from 9 to 24 months of age. Communication, including verbal expression and reception, and gesture production, was measured with an extensive parent-report questionnaire, the MacArthur Communicative Development Inventory (M-CDI; Fenson et al. 1993). Trajectory groups were derived using a group-based trajectory model (GBM) approach, designed to identify groups of participants following a similar developmental pathway.
With this study, we brought evidence of developmental variability in the growth of language and gestures during the first 2 years lives of HR and LR infants. In particular, we evidenced distinct trajectory groups for verbal expression, verbal reception and gesture development. Two groups showing “Low” and “High” language acquisition were derived for verbal expression. In contrast, we derived three trajectory groups each for verbal reception and gesture development, indicating “Low,” “Intermediate” and “High” rates of communication development. At 9 months of age gestures and verbal reception development already showed heterogeneity (see Figs. 2, 3), as most children had already acquired some of these skills. This was not the case for verbal expression. This difference could explain the reduced number of trajectories for verbal expression, where we capitalized on parents’ reporting of the emergence of early words (see Fig. 1) (also see Charman et al. 2003c; Iverson et al. 2017; Mitchell et al. 2006). The observations we have provided for language expression include acquisition of first words, which is of interest because delayed language onset is among the most common reasons for clinical consultation by parents of children with ASD (e.g., DeGiacomo and Fombonne 1998).
Similarly, a previous study from Longard et al. (2017) analyzed the same sample of HR and LR infants from 6 to 36 months on MSEL expressive and receptive language standard scores using a GBM approach. The authors derived three trajectory groups on each measure, displaying increasing, stable, or decreasing developmental patterns. In contrast, in our study the measure of verbal expression yielded only two trajectory groups. Longard et al. (2017) used MSEL standard scores, hence exploring the developmental course of language abilities in reference to typical development (also see Brian et al. 2014). This may suggest a difference between observations of standardized measures for language expression, compared to growth in infants’ vocabulary size in HR infants.
Overall, our findings confirm the variability of communication acquisition in children at risk for ASD, in the most substantial sample reported to date. All the trajectory groups provided by our analyses show growth of language and gesture skills, ranging with respect to acquisition rate. In the following sections, we will discuss the clinical and developmental predictors and outcome related to this variability for each measure.
Predictors of Communicative Development
Our study demonstrated that clinical and developmental skill predictors at 6-months were significantly associated with verbal reception and gesture trajectory groups. We did not find significant predictors for the verbal expression trajectory groups. As previously discussed, this difference may be explained by the reduced variability observed in our verbal expression measure especially in the earliest months, which led to a two-trajectory, rather than the three-trajectory group solution observed for verbal reception and gestures.
We evidenced a positive relationship between motor skills and verbal reception and gesture trajectory groups, as observed in previous studies including HR-Sibs (Bhat et al. 2012; LeBarton and Iverson 2013; Leonard et al. 2015). More specifically, we found that gross motor skills (with a trend for fine motor) were positively associated with verbal reception development, whereas both fine and gross motor skills were positively related to gesture development. In contrast, Leonard et al. (2015) found using MSEL standard scores that the relationship between motor development and language skills was specific to gross motor skills (with a trend for fine motor skills) and expressive (and not receptive) language. As previously discussed, use of MSEL standard scores can lead to substantially different results than M-CDI vocabulary raw scores. In particular, for language expression in younger children, the MSEL includes use of some gestures (e.g., play gestures) as part of the communicative repertoire. Interestingly, we also found that gesture development was associated with both fine and motor skills at 6 months. This finding could suggest that gesture development, a precursor of vocabulary acquisition, could play a significant role in the relation between motor skills and language development. In sum, our results confirm that motor skills play a critical role in the early communication development of HR infants, from the first year of life. It is important to note that MSEL communication skills at 6 months did not differ between LR and HR infants (See Table 1), whereas motor skills did differentiate the two groups (despite standard scores that are situated within the average range for both groups). As suggested by previous evidence (LeBarton and Iverson 2013; Iverson 2010), this may indicate that motor skills should be assessed closely in the first year of life of HR infants, and potentially taken into account in early intervention plans.
Beyond motor skills, behavioral symptoms observed during the AOSI at 6 months of age were also related to gesture development; infants with more behavioral symptoms of ASD had a higher probability of being in the group with slower gesture growth. To date, existing findings have not shown a clear association between AOSI scores at 6 months and subsequent ASD diagnosis (Estes et al. 2015; Zwaigenbaum et al. 2005). Here, we have demonstrated that behavioral symptoms may be related to later gesture development, which as we will see in the following section is in turn related to ASD outcome.
Our results bolster the importance of assessing HR-Sibs very carefully in the first years. Early developmental skills, as well as behavioral symptoms can be informative about future communication development. Advances in research on HR-Sibs has led to the development of intervention approaches adapted for children at risk under 2 years of age, which have been shown to significantly improve nonverbal and verbal communication skills (Drew et al. 2002; Rogers et al. 2012; Schertz and Odom 2007; for a review, see Bradshaw et al. 2015). Our results suggest that motor skills could also affect the development of language and gesture acquisitions. Early intervention plans should hence consider motor skills as a potential contributor to the development of communication abilities (for a discussion see, LeBarton and Iverson 2013; Iverson 2010). In addition, future studies should clarify the impact that early motor skill interventions may have on communication abilities in children at heightened risk for ASD. Refining early intervention targets to promote language development appears of particular importance, considering the high rate of language delays in HR-Sibs, those with both ASD and Non-ASD diagnostic outcomes (Messinger et al. 2013; Ozonoff et al. 2014; Yirmiya et al. 2006).
Communicative Development and Related Outcome
Verbal expression, verbal reception, and gesture trajectory group memberships were all strongly related to 36-month outcomes on both developmental and ASD symptom measures. These results suggest that slower early communication growth is associated with additional atypical aspects of development in individuals with or at risk for ASD. Szatmari et al. (2003) previously showed that language skills at 6 years predicted later developmental outcome in children with ASD with an IQ > 70. More recently, Ray-Subramanian et al. (2012) also found a relationship between language growth from age 2 to 3 years and reduced restricted and repetitive behaviors as well as improved nonverbal skills at 3 years in young children with ASD. Our results extend these findings by providing evidence that communication development in the first 2 years is critical for global development in HR-Sibs, beyond communication. This observation strengthens the suggestion that communication growth rate in HR-Sibs should be monitored, as suggested previously (see Zwaigenbaum et al. 2009).
Communication trajectory group membership was also associated with ASD diagnosis at 36 months. Iverson et al. (2017) similarly showed that M-CDI communication trajectories in HR-ASD children were reduced compared to LR, HR-non-ASD and HR-non-ASD infants with LangD. We confirmed a similar pattern in a much larger sample using a different statistical approach (GBM). Whereas the vast majority of children with ASD was in the lowest trajectory group for both verbal expression and reception, the majority of children with ASD fell in the intermediate trajectory group for gesture development. Nonetheless, the percentage of HR-ASD children in the lowest gesture trajectory group was still higher than that for HR-Non-ASD or LR infants. Our large sample allowed us to examine further the specificity of language delays (LangD) within HR-ASD siblings. Interestingly, we found a different distribution of LangD among trajectory groups for verbal expression and reception. HR-ASD infants with LangD were more represented in the lower M-CDI communication trajectories than HR-ASD infants without LangD. This observation suggests for the first time that early communication growth in individuals with ASD predicts their future language impairments. However, early gesture development was not differentially represented in communication trajectories between HR-ASD with or without LangD, suggesting that gesture development is less associated with later language impairments than growth in verbal skills in infants with ASD. In sum, the growth rate of verbal skills in two first years in children with ASD is related to later language deficits. From a clinical point of view, this suggests that vocabulary acquisition in infants for whom there are strong clinical concerns regarding ASD may predict not only an ASD diagnosis but also specific language impairment.
Our supplementary results additionally showed that gesture scores appear to differentiate outcome groups earlier than do verbal scores (see Supplementary Table 2). Specifically, M-CDI gesture scores distinguished HR-ASD, HR-Non-ASD and LR infants from 12 months of age, whereas verbal expression and reception scores differentiated the three groups from 15 months of age. Iverson et al. (2017) reported a positive relationship between gesture production and later expressive verbal development, which similarly suggests earlier impairments of nonverbal communication over verbal communication (also see Charman 2003a). The gestures included in the M-CDI largely reflect deictic joint attention skills (e.g., giving, requesting pointing, showing) and pretend play actions (e.g., pretending to be a parent, and imitating other adult actions). Joint attention skills and pretend play are both known to be impaired in young children with ASD (Ibanez et al. 2013; Parlade and Iverson 2015; Winder et al. 2013) and predictive of language development in young children with ASD. Numerous studies have also shown that joint attention and pretend play are related to language development in both typical and atypical development (Ingersoll and Dvortcsak 2010; Jones et al. 2006; Murray et al. 2008; Rowe and Goldin-Meadow 2009; Toth et al. 2006). We have confirmed that these atypicalities may emerge as early as the first birthday in children at risk for ASD, suggesting that poor gesture development could be a critical early marker for ASD. Future studies should specifically address the relationship between gesture and language measured on the M-CDI and through direct assessment. However, this finding supports the need to intervene on nonverbal communication as part of the effort to promote language development in high-risk infants.
Limitations
Our study presents several limitations. First, the M-CDI is a parent-report measure. Parental measures collected within HR studies are subject to bias (Iverson et al. 2017; Szatmari et al. 2016). In fact, parents of children with ASD tend to be more alert to their children’s development than parents of children with typical development. The M-CDI has the advantage of showing excellent reliability (Fenson et al. 1993). Moreover, the M-CDI allows for extensive collection of the vocabulary and gesture repertoire in a child’s everyday life. Second, our dataset was unstructured in term of the number of participants per visit. More specifically, fewer data have been collected at 9, 15 and 21 months of age. For this reason, we applied a GBM approach, which aims to generalize the derived trajectories for a whole sample. This statistical method has been used successfully with the same sample (Brian et al. 2014; Longard et al. 2017). Finally, the M-CDI is intended for children up to 18 months of age. Previous research has demonstrated the relevance of using the M-CDI in children with ASD older than 18 months (Charman et al. 2003c). Furthermore, we didn’t observe evidence for ceiling effects on the data collected with the M-CDI at 24 months (see Supplementary Table 2). Finally, we were unable to take into account the interventions that children may have received during study participation. Future studies should evaluate the impact of early interventions on the developmental trajectories of language and gesture development.
Conclusions and Clinical Implications
Early variability in gesture and vocabulary growth is a critical aspect of the early development of infants at high risk for ASD. Slower communication growth early in life appears characteristic of HR-ASD infants, and even more so of HR-ASD children with language delay. Developmental surveillance and specific assessment of communication abilities, evaluating growth in the gesture and vocabulary repertoires of HR infants, should be part of clinical practice. Atypical communication growth rates in HR infants can inform about increased risk for both ASD and LangD outcomes, indicating the necessity of intervening as soon as possible. In particular, a lower rate of gesture use by the first birthday can be associated with a later ASD diagnosis. Early interventions have shown to be feasible and effective as clinical concerns are raised; even before a formal ASD diagnosis is confirmed (e.g., Brian et al. 2016, 2017; Rogers et al. 2012, 2014). Our results further suggest that motor skills may represent an essential target, beyond more obvious language-related abilities, in early intervention plans for children at risk. Monitoring the growth of gesture and language development could indicate developmental disabilities in children with a heightened risk for ASD.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th edn. text rev; DSM-IV-TR). Washington, DC: American Psychiatric Association.
American Psychiatric Association. (2013). Cautionary statement for forensic use of DSM-5. In Diagnostic and statistical manual of mental disorders (5th edn.). https://doi.org/10.1176/appi.books.9780890425596.744053.
Bhat, A. N., Galloway, J. C., & Landa, R. J. (2012). Relation between early motor delay and later communication delay in infants at risk for autism. Infant Behavior and Development, 35(4), 838–846. https://doi.org/10.1016/j.infbeh.2012.07.019.
Bolton, P. F., Golding, J., Emond, A., & Steer, C. D. (2012). Autism spectrum disorder and autistic traits in the Avon longitudinal study of parents and children: Precursors and early signs. Journal of the American Academy of Child and Adolescent Psychiatry, 51(3), 249–260.
Bradshaw, J., Steiner, A. M., Gengoux, G., & Koegel, L. K. (2015). Feasibility and effectiveness of very early intervention for infants at-risk for autism spectrum disorder: A systematic review. Journal of Autism and Developmental Disorders, 45(3), 778–794. https://doi.org/10.1007/s10803-014-2235-2.
Brady, N. C., Marquis, J., Fleming, K., & McLean, L. (2004). Prelinguistic predictors of language growth in children with developmental disabilities. Journal of Speech, Language, and Hearing Research, 47(3), 663–677. https://doi.org/10.1044/1092-4388(2004/051).
Brian, A. J., Roncadin, C., Duku, E., Bryson, S. E., Smith, I. M., Roberts, W., et al. (2014). Emerging cognitive profiles in high-risk infants with and without autism spectrum disorder. Research in Autism Spectrum Disorders, 8(11), 1557–1566. https://doi.org/10.1016/j.rasd.2014.07.021.
Brian, J. A., Smith, I. M., Zwaigenbaum, L., & Bryson, S. E. (2017). Cross-site randomized control trial of the Social ABCs caregiver-mediated intervention for toddlers with autism spectrum disorder. Autism Research: Official Journal of the International Society for Autism Research, 10(10), 1700–1711. https://doi.org/10.1002/aur.1818.
Brian, J. A., Smith, I. M., Zwaigenbaum, L., Roberts, W., & Bryson, S. E. (2016). The Social ABCs caregiver-mediated intervention for toddlers with autism spectrum disorder: Feasibility, acceptability, and evidence of promise from a multisite study. Autism Research: Official Journal of the International Society for Autism Research, 9(8), 899–912. https://doi.org/10.1002/aur.1582.
Bryson, S. E., Zwaigenbaum, L., Brian, J., Roberts, W., Szatmari, P., Rombough, V., et al. (2007). A prospective case series of high-risk infants who developed autism. Journal of Autism and Developmental Disorders, 37(1), 12–24. https://doi.org/10.1007/s10803-006-0328-2.
Bryson, S. E., Zwaigenbaum, L., McDermott, C., Rombough, V., & Brian, J. (2008). The autism observation scale for infants: Scale development and reliability data. Journal of Autism and Developmental Disorders, 38(4), 731–738. https://doi.org/10.1007/s10803-007-0440-y.
Charman, T. (2003a). Why is joint attention a pivotal skill in autism? Philosophical Transactions of the Royal Society of London: Biological Sciences, 358(1430), 315–324. https://doi.org/10.1098/rstb.2002.1199.
Charman, T., Baron-Cohen, S., Swettenham, J., Baird, G., Drew, A., & Cox, A. (2003b). Predicting language outcome in infants with autism and pervasive developmental disorder. International Journal of Language & Communication Disorders, 38(3), 265–285. https://doi.org/10.1080/136820310000104830.
Charman, T., Drew, A., Baird, C., & Baird, G. (2003c). Measuring early language development in preschool children with autism spectrum disorder using the MacArthur communicative development inventory (Infant Form). Journal of Child Language, 30(1), 213–236.
Charman, T., Taylor, E., Drew, A., Cockerill, H., Brown, J.-A., & Baird, G. (2005). Outcome at 7 years of children diagnosed with autism at age 2: Predictive validity of assessments conducted at 2 and 3 years of age and pattern of symptom change over time. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 46(5), 500–513. https://doi.org/10.1111/j.1469-7610.2004.00377.x.
Chawarska, K., Macari, S., & Shic, F. (2013). Decreased spontaneous attention to social scenes in 6-month-old infants later diagnosed with autism spectrum disorders. Biological Psychiatry, 74(3), 195–203. https://doi.org/10.1016/j.biopsych.2012.11.022.
DeGiacomo, A., & Fombonne, E. (1998). Parental recognition of developmental abnormalities in autism. European Child & Adolescent Psychiatry, 7(3), 131–136.
Drew, A., Baird, G., Baron-Cohen, S., Cox, A., Slonims, V., Wheelwright, S., et al. (2002). A pilot randomised control trial of a parent training intervention for pre-school children with autism. European Child & Adolescent Psychiatry, 11(6), 266–272. https://doi.org/10.1007/s00787-002-0299-6.
Ellis Weismer, S., Lord, C., & Esler, A. (2010). Early language patterns of toddlers on the autism spectrum compared to toddlers with developmental delay. Journal of Autism and Developmental Disorders, 40(10), 1259–1273. https://doi.org/10.1007/s10803-010-0983-1.
Estes, A., Zwaigenbaum, L., Gu, H., John, T. S., Paterson, S., Elison, J. T., et al. (2015). Behavioral, cognitive, and adaptive development in infants with autism spectrum disorder in the first 2 years of life. Journal of Neurodevelopmental Disorders, 7(1), e1–e10. https://doi.org/10.1186/s11689-015-9117-6.
Fenson, L., Dale, J., Reznick, S., Thal, D., Bates, E., Hartung, J. P., et al. (1993). MacArthur communicative development inventories: User’s guide and manual. San Diego, CA: Singular Publishing Group.
Flanagan, J. E., Landa, R., Bhat, A., & Bauman, M. (2012). Head lag in infants at risk for autism: A preliminary study. The American Journal of Occupational Therapy, 66(5), 577–585. https://doi.org/10.5014/ajot.2012.004192.
Gotham, K., Pickles, A., & Lord, C. (2009). Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(5), 693–705.
Ibanez, L. V., Grantz, C. J., & Messinger, D. S. (2013). The development of referential communication and autism symptomatology in high-risk infants. Infancy, 18(5), 687–707. https://doi.org/10.1111/j.1532-7078.2012.00142.x.
Ingersoll, B., & Dvortcsak, A. (2010). Teaching social communication to children with autism. New York: The Guilford Press.
Iverson, J. M. (2010). Developing language in a developing body: The relationship between motor development and language development. Journal of Child Language, 37(2), 229–261. https://doi.org/10.1017/S0305000909990432.
Iverson, J. M., Northrup, J. B., Leezenbaum, N. B., Parlade, M. V., Koterba, E. A., & West, K. L. (2017). Early gesture and vocabulary development in infant siblings of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 115(3), 517–527. https://doi.org/10.1007/s10803-017-3297-8.
Jones, B. L., Nagin, D., & Roeder, K. (2001). A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research, 29, 374–393.
Jones, B. L., & Nagin, D. S. (2007). Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological & Research, 35(4), 542–571. https://doi.org/10.1177/0049124106292364.
Jones, E. A., Carr, E. G., & Feeley, K. M. (2006). Multiple effects of joint attention intervention for children with autism. Behavior Modification, 30(6), 782–834. https://doi.org/10.1177/0145445506289392.
Jones, E. J. H., Gliga, T., Bedford, R., Charman, T., & Johnson, M. H. (2014). Developmental pathways to autism: A review of prospective studies of infants at risk. Neuroscience & Biobehavioral Reviews, 39, 1–33. https://doi.org/10.1016/j.neubiorev.2013.12.001.
Jones, W., & Klin, A. (2013). Attention to eyes is present but in decline in 2–6-month-old infants later diagnosed with autism. Nature, 504(7480), 427–431. https://doi.org/10.1038/nature12715.
Landa, R. J., Holman, K. C., & Garrett-Mayer, E. (2007). Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry, 64(7), 853–864. https://doi.org/10.1001/archpsyc.64.7.853.
LeBarton, E. S., & Iverson, J. M. (2013). Fine motor skill predicts expressive language in infant siblings of children with autism. Developmental Science, 16(6), 815–827. https://doi.org/10.1111/desc.12069.
Leonard, H. C., Bedford, R., Pickles, A., Hill, E. L., & BASIS Team. (2015). Predicting the rate of language development from early motor skills in at-risk infants who develop autism spectrum disorder. Research in Autism Spectrum Disorders, 13–14, 15–24. https://doi.org/10.1016/j.rasd.2014.12.012.
Longard, J., Brian, J., Zwaigenbaum, L., Duku, E., Moore, C., Smith, I. M., et al. (2017). Early expressive and receptive language trajectories in high-risk infant siblings of children with autism spectrum disorder. Autism & Developmental Language Impairments, 2(3), 239694151773741. https://doi.org/10.1177/2396941517737418.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Leventhal, B. L., DiLavore, P. C., et al. (2000). The autism diagnostic observation schedule–generic: A standard measure of social and communicative deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30, 205–223.
Manwaring, S. S., Mead, D. L., Swineford, L., & Thurm, A. (2017). Modelling gesture use and early language development in autism spectrum disorder. International Journal of Language & Communication Disorders, 52(5), 637–651. https://doi.org/10.1111/1460-6984.12308.
Messinger, D., Young, G. S., Ozonoff, S., Dobkins, K., Carter, A., Zwaigenbaum, L., et al. (2013). Beyond autism: A baby siblings research consortium study of high-risk children at three years of age. Journal of the American Academy of Child and Adolescent Psychiatry, 52(3), 300–308. https://doi.org/10.1016/j.jaac.2012.12.011.
Mitchell, S. M., Brian, J., Zwaigenbaum, L., Roberts, W., Szatmari, P., Smith, I., et al. (2006). Early language and communication development of infants later diagnosed with autism spectrum disorder. Journal of Developmental and Behavioral Pediatrics, 27(2), 68–78.
Mullen, E. M. (1995). Mullen scales of early learning. Circle Pines, MN: American Guidance.
Murray, D. S., Creaghead, N. A., Manning-Courtney, P., Shear, P. K., Bean, J., & Prendeville, J.-A. (2008). The relationship between joint attention and language in children with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 23(1), 5–14. https://doi.org/10.1177/1088357607311443.
Nagin, D. S. (1999). Analyzing developmental trajectories: A semi-parametric, group based approach. Psychological Methods, 4, 139–177.
Nagin, D. S. (2005). Group-based modeling of development. Cambridge, MA: Harvard University Press.
Ozonoff, S., Heung, K., Byrd, R., Hansen, R., & Hertz-Picciotto, I. (2008). The onset of autism: Patterns of symptom emergence in the first years of life. Autism Research, 1(6), 320–328. https://doi.org/10.1002/aur.53.
Ozonoff, S., Young, G. S., Belding, A., Hill, M., Hill, A., Hutman, T., et al. (2014). The broader autism phenotype in infancy: When does it emerge? Journal of the American Academy of Child and Adolescent Psychiatry, 53(4), 398–407. https://doi.org/10.1016/j.jaac.2013.12.020.
Ozonoff, S., Young, G. S., Carter, A., Messinger, D., Yirmiya, N., Zwaigenbaum, L., et al. (2011). Recurrence risk for autism spectrum disorders: A baby siblings research consortium study. Pediatrics, 128(3), e488–e495. https://doi.org/10.1542/peds.2010-2825.
Parlade, M. V., & Iverson, J. M. (2015). The development of coordinated communication in infants at heightened risk for autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(7), 2218–2234. https://doi.org/10.1007/s10803-015-2391-z.
Paul, R., Chawarska, K., Cicchetti, D., & Volkmar, F. (2008). Language outcomes of toddlers with autism spectrum disorders: A two year follow-up. Autism Research, 1(2), 97–107. https://doi.org/10.1002/aur.12.
Paul, R., Fuerst, Y., Ramsay, G., Chawarska, K., & Klin, A. (2011). Out of the mouths of babes: Vocal production in infant siblings of children with ASD. Journal of Child Psychology and Psychiatry, 52(5), 588–598. https://doi.org/10.1111/j.1469-7610.2010.02332.x.
Piven, J., Elison, J. T., & Zylka, M. J. (2017). Toward a conceptual framework for early brain and behavior development in autism. Molecular Psychiatry, 22(10), 1385–1394. https://doi.org/10.1038/mp.2017.131.
Ray-Subramanian, C. E., & Ellis Weismer, S. (2012). Receptive and expressive language as predictors of restricted and repetitive behaviors in young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(10), 2113–2120. https://doi.org/10.1007/s10803-012-1463-6.
Richards, M., Mossey, J., & Robins, D. L. (2016). Parentsʼ concerns as they relate to their childʼs development and later diagnosis of autism spectrum disorder. Journal of Developmental & Behavioral Pediatrics, 37(7), 532–540. https://doi.org/10.1097/DBP.0000000000000339.
Rogers, S. J. (2009). What are infant siblings teaching us about autism in infancy? Autism research. Official Journal of the International Society for Autism Research, 2(3), 125–137. https://doi.org/10.1002/aur.81.
Rogers, S. J., Estes, A., Lord, C., Vismara, L., Winter, J., Fitzpatrick, A., et al. (2012). Effects of a brief early start Denver model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 51(10), 1052–1065. https://doi.org/10.1016/j.jaac.2012.08.003.
Rogers, S. J., Vismara, L., Wagner, A. L., McCormick, C., Young, G., & Ozonoff, S. (2014). Autism treatment in the first year of life: A pilot study of infant start, a parent-implemented intervention for symptomatic infants. Journal of Autism and Developmental Disorders, 44(12), 2981–2995. https://doi.org/10.1007/s10803-014-2202-y.
Rowe, M. L., & Goldin-Meadow, S. (2009). Early gesture selectively predicts later language learning. Developmental Science, 12(1), 182–187. https://doi.org/10.1111/j.1467-7687.2008.00764.x.
Rutter, M., Le Couteur, A., & Lord, C. (2003). ADI-R: Autism diagnostic Interview revised manual. Los Angeles: Western Psychological Services.
Sacrey, L.-A. R., Zwaigenbaum, L., Bryson, S., Brian, J., Smith, I. M., Roberts, W., et al. (2015). Can parents’ concerns predict autism spectrum disorder? A prospective study of high-risk siblings from 6 to 36 months of age. Journal of the American Academy of Child and Adolescent Psychiatry, 54(6), 470–478. https://doi.org/10.1016/j.jaac.2015.03.014.
Schertz, H. H., & Odom, S. L. (2007). Promoting joint attention in toddlers with autism: A parent-mediated developmental model. Journal of Autism and Developmental Disorders, 37(8), 1562–1575. https://doi.org/10.1007/s10803-006-0290-z.
Stone, W. L., McMahon, C. R., Yoder, P. J., & Walden, T. A. (2007). Early social-communicative and cognitive development of younger siblings of children with autism spectrum disorders. Archives of Pediatrics & Adolescent Medicine, 161(4), 384–390. https://doi.org/10.1001/archpedi.161.4.384.
Stone, W. L., & Yoder, P. J. (2001). Predicting spoken language level in children with autism spectrum disorders. Autism, 5(4), 341–361. https://doi.org/10.1177/1362361301005004002.
Szatmari, P., Bryson, S. E., Boyle, M. H., Streiner, D. L., & Duku, E. (2003). Predictors of outcome among high functioning children with autism and Asperger syndrome. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 44(4), 520–528.
Szatmari, P., Chawarska, K., Dawson, G., Georgiades, S., Landa, R., Lord, C., et al. (2016). Prospective longitudinal studies of infant siblings of children with autism: Lessons learned and future directions. Journal of the American Academy of Child and Adolescent Psychiatry, 55(3), 179–187. https://doi.org/10.1016/j.jaac.2015.12.014.
Thurm, A., Lord, C., Lee, L.-C., & Newschaffer, C. (2007). Predictors of language acquisition in preschool children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 37(9), 1721–1734. https://doi.org/10.1007/s10803-006-0300-1.
Toth, K., Munson, J., Meltzoff, A. N., & Dawson, G. (2006). Early predictors of communication development in young children with autism spectrum disorder: Joint attention, imitation, and toy play. Journal of Autism and Developmental Disorders, 36(8), 993–1005. https://doi.org/10.1007/s10803-006-0137-7.
Volden, J., Smith, I. M., Szatmari, P., Bryson, S., Fombonne, E., Mirenda, P., et al. (2011). Using the preschool language scale, fourth edition to characterize language in preschoolers with autism spectrum disorders. American Journal of Speech-Language Pathology, 20(3), 200–210. https://doi.org/10.1044/1058-0360(2011/10-0035).
West, K. L., Leezenbaum, N. B., Northrup, J. B., & Iverson, J. M. (2017). The relation between walking and language in infant siblings of children with autism spectrum disorder. Child Development, 17(1), 213. https://doi.org/10.1111/cdev.12980.
Winder, B. M., Wozniak, R. H., Parlade, M. V., & Iverson, J. M. (2013). Spontaneous initiation of communication in infants at low and heightened risk for autism spectrum disorders. Developmental Psychology, 49(10), 1931–1942. https://doi.org/10.1037/a0031061.
Yirmiya, N., Gamliel, I., Pilowsky, T., Feldman, R., Baron-Cohen, S., & Sigman, M. (2006). The development of siblings of children with autism at 4 and 14 months: Social engagement, communication, and cognition. Journal of Child Psychology and Psychiatry, 47(5), 511–523. https://doi.org/10.1111/j.1469-7610.2005.01528.x.
Young, G. S., Merin, N., Rogers, S. J., & Ozonoff, S. (2009). Gaze behavior and affect at 6 months: Predicting clinical outcomes and language development in typically developing infants and infants at risk for autism. Developmental Science, 12(5), 798–814. https://doi.org/10.1111/j.1467-7687.2009.00833.x.
Zwaigenbaum, L., Bryson, S., Lord, C., Rogers, S., Carter, A., Carver, L., et al. (2009). Clinical assessment and management of toddlers with suspected autism spectrum disorder: Insights from studies of high-risk infants. Pediatrics, 123(5), 1383–1391. https://doi.org/10.1542/peds.2008-1606.
Zwaigenbaum, L., Bryson, S., Rogers, T., Roberts, W., Brian, J., & Szatmari, P. (2005). Behavioral manifestations of autism in the first year of life. International Journal of Developmental Neuroscience, 23(2–3), 143–152. https://doi.org/10.1016/j.ijdevneu.2004.05.001.
Zwaigenbaum, L., Bryson, S. E., Szatmari, P., Brian, J., Smith, I. M., Roberts, W., et al. (2012). Sex differences in children with autism spectrum disorder identified within a high-risk infant cohort. Journal of Autism and Developmental Disorders, 42(12), 2585–2596. https://doi.org/10.1007/s10803-012-1515-y.
Acknowledgments
The authors would like to thank all the families who kindly volunteered to participate as well as all the person involved in data collection. This work was supported by the Canadian Institutes of Health Research [Grant Number MOP102655] and Autism Speaks Canada [Grant Number ASCanada-2010-01]. MF was further supported by an individual grant from the Swiss National Science Foundation (Grant Number P2GEP1_171686).
Author information
Authors and Affiliations
Contributions
SEB, LZ, and JB designed and planned the cohort study. MF and IMS conceived the current study. JB, SEB, LZ, IMS, WR, and CR participated in data collection. MF performed the analyses. ED provided support in the statistical analyses. ED, IMS, VA, and MF contributed to the interpretation of the results. MF took the lead in writing the manuscript, and IMS supervised the writing. All authors provided critical feedback and helped shape the research, analysis, and manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Franchini, M., Duku, E., Armstrong, V. et al. Variability in Verbal and Nonverbal Communication in Infants at Risk for Autism Spectrum Disorder: Predictors and Outcomes. J Autism Dev Disord 48, 3417–3431 (2018). https://doi.org/10.1007/s10803-018-3607-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-018-3607-9