Abstract
The nature of the co-occurrence of chronic tic disorders (CTD) and attention deficit hyperactivity disorder (ADHD) is unclear. Especially in the field of psychopathology, the relationship of CTD and ADHD remains to be clarified. Thus, the aim of the present chart review study was to specify the contribution of CTD and/or ADHD to the psychopathological profile of the comorbid group (CTD+ADHD). The psychopathological profiles of four large groups (CTD-only (n=112), CTD+ADHD (n=82), ADHD-only (n=129), controls (n=144)) were measured by the eight subscales of the Child Behavior Checklist (CBCL) and analyzed by a 2×2 factorial design followed by contrasts. There were main effects of ADHD diagnosis on all but one subscale of the CBCL (Somatic Complaints). For CTD diagnosis, main effects were found for Attention Problems, Anxious/Depressed, Thought Problems, Social Problems and Somatic Complaints. The only interaction effect was seen for Somatic Complaints. While CTD and ADHD were both related to internalizing psychopathology of children in the CTD+ADHD group, ADHD had the largest effect on externalizing psychopathology in the comorbid group. At the level of psychopathology, an additive model for the co-occurrence of CTD and ADHD is strongly supported. In the comorbid group (CTD+ADHD), the ADHD diagnosis shows the strongest relation to externalizing psychopathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Addictive effects
Chronic tic disorders (CTD) and attention deficit hyperactivity disorder (ADHD) are common disabling chronic disorders of childhood onset. ADHD is usually a precursor of CTD and both disorders often co-occur. About half of the cases with CTD also meet criteria for ADHD, whereas about 20% of children with ADHD are also affected by tics (Gillberg et al., 2004; Kadesjo & Gillberg, 2000; Spencer et al., 2001a). Therefore, evidence-based information about similarities and differences in broadband psychopathology as well as the relationship of CTD and ADHD is clinically important.
However, research focusing on the background of this comorbidity is scarce, although several hypotheses have been formulated to elucidate the nature of the co-occurrence of CTD and ADHD (Robertson, 2000; Yordanova, Dumais-Huber, & Rothenberger, 1996; Yordanova, Heinrich, Kolev, & Rothenberger, 2006). Hence, more evidence in this field is of both heuristic and practical value. The most common approach to specify psychopathology in the comorbid group (CTD+ADHD) is its comparison with ‘pure’ groups (CTD, ADHD, controls). Differences in the number and criteria of groups included (e.g. inclusion of confounding additional comorbid diagnoses like OCD), as well as in the psychopathological aspects under investigation have limited the comparability of findings so far. Unfortunately, studies using the optimal design of including all four groups (CTD, CTD+ADHD, ADHD, controls) are few (Gadow, Nolan, Sprafkin, & Schwartz, 2002; Shin, Chung, & Hong, 2001; Spencer et al., 1998; Sukhodolsky et al., 2003), Moreover, in these as well as in other studies, methodological shortcomings reduce the validity of the conclusions drawn about the overlap of CTD and ADHD.
Nevertheless, there is increasing evidence that patients of the comorbid group consistently show the most severe psychopathology and psychosocial impairment (Carter et al., 2000; Gadow et al., 2002; Kurlan et al., 2002; Pierre, Nolan, Gadow, Sverd, & Sprafkin, 1999; Spencer et al., 1998; Sukhodolsky et al., 2003). However, psychopathological similarities and differences of the groups in question are still a matter of debate: ADHD (without CTD) has sometimes been found to be more similar to CTD+ADHD, and sometimes to be closer to CTD (without ADHD). Similarly, it is not clear whether the psychopathology of patients with CTD (without ADHD) is more similar to that of controls than to that of ADHD (without CTD) (Carter et al., 2000; Hoekstra et al., 2004; Pierre et al., 1999; Spencer et al., 1998; Stephens & Sandor, 1999; Sukhodolsky et al., 2003; for a review see Robertson, 2006). Therefore, the first aim of the present study was to overcome the existing methodological shortcomings and gain clarity by analyzing group differences of a broad psychopathological profile among four large, age- and sex-similar groups (CTD-only, CTD+ADHD, ADHD-only, controls) of comparable size. To minimize confounding influences, further psychiatric diagnoses (axis I according to ICD-10 multiaxial classification system (World Health Organisation, 1996)) were excluded in accordance to Sukhodolsky et al. (2003). The Child Behavior Checklist (CBCL) (Achenbach, 1991) was used to evaluate similarities and differences in dimensional psychopathology in children with CTD and/or ADHD.
Thus far, most authors have concluded that ADHD compared to CTD makes a major contribution to psychopathology and psychosocial impairment in the comorbid group (CTD+ADHD) (Carter et al., 2000; Kurlan et al., 2002; Pierre et al., 1999; Spencer et al., 1998; Sukhodolsky et al., 2003). These conclusions were more deductive rather than evidence-based, since a 2×2 factorial design (ADHD (yes, no) x tics (yes, no)) including all four groups was used only in one study (Gadow et al., 2002). Gadow et al. (2002) reported age-specific interactive patterns, but statistics or more details as well as interpretation of their findings are lacking. Therefore, the second aim of the present study was to use a 2×2 factorial design with the factors CTD and ADHD. This allows for clarification of (a) whether the comorbid group represents the additive or interactive co-occurrence of the features of both ‘pure’ disorders and if an additive model is supported, and (b) whether or not each factor is related to the psychopathology scores on the CBCL.
However, the detailed relationship between factors (CTD vs. ADHD) remains unclear in a 2×2 design. Therefore, the third aim of this study was to specify the contribution of each factor to the psychopathology of the comorbid group in more detail than indicated by the main effects. The direct statistical comparison of effects of the two factors is the only way to obtain information on the hypothesized importance of ADHD compared to CTD. Thus, contrasts of the relationship of both CTD and ADHD to the psychopathology scores will be computed if support for additive effects is found in the 2×2 ANOVA.
Method
Participants
All participants (more than 99% Caucasians) of this chart review study had been referred to the outpatient clinic of the Department of Child and Adolescent Psychiatry at the University of Goettingen between January 1997 and January 2005 for routine clinical assessment. For more than a decade, this clinic has been closely associated with ongoing research and also includes a center of excellence for CTD, ADHD and OCD with a specialized outpatient clinic for these disorders.
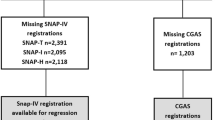
The three patient groups were screened from 1,373 patients referred to the specialized clinic during this period. Sixty-nine patients had to be excluded due to missing values (>20) on the CBCL. Out of the remaining 1,304 cases, a further 343 children had to be excluded because they showed neither CTD nor ADHD. To obtain results of high quality concerning the complex co-occurrence of CTD and ADHD, confounding variables present in other studies in this field (age, sex, other psychiatric diagnoses than CTD and ADHD) were controlled by excluding children with other diagnoses (axis I according to ICD-10 multiaxial classification system (World Health Organisation, 1996)) and by selecting children to form groups that did not differ in age or gender composition. Hence, 593 children with any additional psychiatric diagnosis (axis I according to ICD-10 multiaxial classification system (World Health Organisation, 1996)) other than CTD and/or ADHD were excluded. Thereafter, in the CTD-only group 13 children, in the CTD+ADHD group 10 children and in the ADHD-only group 22 children were excluded from the study to eliminate significant age and gender differences between the three groups. The final group size and mean ages were: CTD-only n=112, mean age=11.1, SD=2.6 years; CTD+ADHD n=82, mean age=10.7, SD=2.3 years and ADHD-only n=129, mean age=10.5, SD=2.5 years.
As controls, 354 subjects from the general outpatient clinic not suffering from an axis I diagnosis according to ICD-10 multiaxial classification system (World Health Organisation, 1996) were included (43% learning disorder, 57% no diagnosis). These children had been referred by their families for assessment of supposed psychiatric problems, but showed no or only subcategorical psychiatric problems or learning disorders. Sixteen of the control patients were excluded due to missing values (>20) in the CBCL. Out of the remaining 338 children, 144 were selected (mean age=10.4, SD=2.4 years) to obtain a group that did not differ statistically from the other three groups in child age or gender.
Patients with CTD and/or ADHD fulfilled the diagnostic criteria for these disorders according to the Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (American Psychiatric Association, 2000) as well as the International Classification of Diseases ICD-10 (Dilling, Mombour, & Schmidt, 2000) (CTD including Tourette Syndrome and ADHD combined type or hyperkinetic disorder (HD)). All children (cases and controls) were clinically assessed and best-estimate diagnoses were assigned on the basis of clinical observation, semi-structured interviews with parents and children (BADO; Englert et al., 1996) and various clinical ratings (parents, teachers, experts) (e.g. Conners Rating Scale (Goyette, Conners, & Ulrich, 1978); Tourette Syndrome Severity Scale (TSSS, Walkup, Rosenberg, Brown, & Singer, 1992); Yale Global Tic Severity Scale (YGTSS, Leckman et al., 1989)). All diagnoses were verified in a case conference by senior board-certified child psychiatrists. These experts have been working in clinical and research settings for CTD and ADHD for many years. This chart review was considered by the local Ethics Committee to be exempt from review, and written informed consent was not required.
Psychopathology measure
The Child Behavior Checklist (CBCL) is one of the most established inventories for the evaluation of dimensional psychopathology in children and adolescents (Achenbach, 1991; Bird, 1996). The 112 behavioral items are rated by a parent on a three-point scale. After generating T scores on subscales that assess empirically derived dimensions of psychopathology and social competence, a profile of childhood psychological problems can be described with scores on eight subscales as well as on composite Internalizing, Externalizing and Total Problem scales. We used only the eight subscales. Numerous studies have confirmed the instrument’s stability of psychometric properties, showing good reliability and validity in both clinical and non-clinical populations (Jensen et al., 1996; Schmeck et al., 2004). The stability of the subscales over a 4-year period in a clinical sample of youth with ADHD has been observed (Biederman et al., 2001). In addition, CBCL scores demonstrate good convergence with structured interviews for psychiatric diagnosis in children with ADHD (Biederman et al., 1993) and its subscale Attention Problems has a highly discriminative power for ADHD (Chen, Faraone, Biederman, & Tsuang, 1994). Furthermore, the CBCL has shown particular usefulness in psychopathological studies on CTD (Cardona, Romano, Bollea, & Chiarotti, 2004; Termine et al., 2006).
Statistics
Two-way analyses of variance (ANOVA) for the factors CTD (yes, no) x ADHD (yes, no) were conducted to better understand the nature of co-occurrence. The lack of a significant CTD x ADHD interaction would support an additive model. Because there are differences in the rate of comorbid learning disorders (extraordinary high rate in the control group), additional ANCOVAs were conducted to test for the role of comorbid learning disorders.
If the additive model was supported, contrasts were computed to compare the relative contribution of each factor (CTD vs. ADHD) to the psychopathology in the comorbid group. The calculation was performed on the assumption that the difference in the sum of mean values from the CBCL subscales between children with or without a tic disorder does not deviate from the difference in the sum of mean values in children with or without ADHD ((ADHD/CTD + CTD) - (ADHD + controls) = (ADHD/CTD + ADHD) - (CTD + controls)). After solving the equations the following contrast weights resulted: controls = 0; CTD = 1; ADHD = −1 and CTD/ADHD = 0.
Results
There were no significant group differences based on age, F(3, 463)=2.51, p=.06 or gender, χ 2 (df=1, N=467)=1.09, p=.21; the percentage of learning disorders differed between the groups, χ 2(df=1, N=467)=7.56, p<.01 (CTD-only 4%; CTD+ADHD 16%; ADHD-only 29%; controls 43%).
Performing a 2×2 factorial ANOVA revealed main effects for the factor ADHD on all CBCL subscales except the subscale Somatic Complaints. For the factor CTD there were significant main effects on the subscales Attention Problems, Anxious/Depressed, Thought Problems, Somatic Complaints and Social Problems. No interaction effect could be seen except on the subscale Somatic Complaints (see Table 1).
Additional 2×2 factorial ANCOVAS revealed no effects of the dichotomous (present or not) covariate ‘learning disorder’ on any CBCL subscale: Aggressive Behavior, F(1, 463)=1.25, p=.263; Delinquent Behavior, F(1, 463)=0.02, p=.899; Attention Problems, F(1, 463)=0.30, p=.583; Anxious/Depressed, F(1, 463)=0.01, p=.922; Thought Problems, F(1, 463)=0.13, p=.715; Withdrawn, F(1, 463)=2.18, p=.140; Somatic Complaints, F(1, 463)=0.12, p=.734; or Social Problems, F(1, 463)=54, p =.111.
The contrasts, calculated to specify the relationships of the factors CTD and ADHD to each CBCL subscale, showed that CTD was not stronger related than ADHD for any subscale (see Table 2). A stronger relationship of the ADHD diagnosis compared to CTD was observed on the subscales Aggressive Behavior, Delinquent Behavior, Attention Problems and Social Problems. No differences have been found on the other subscales. On the subscale Somatic Complaints the lack of an additive model prohibited the calculation of contrasts.
Discussion
The main objective of the present study was to investigate how CTD or ADHD relate to the psychopathology of CTD+ADHD. For the first time, groups of large size without any further confounding psychiatric conditions and comparable in age and sex were studied. The comparison of the four clinically diagnosed groups (CTD-only, CTD+ADHD, ADHD-only, controls) using CBCL subscales revealed the highest levels of psychopathology in patients with CTD+ADHD, except on the subscale Somatic Complaints. Furthermore, no interaction effects between the factors CTD and ADHD were found on any subscales, except Somatic Complaints. This strongly supported the existence of an additive model. Moreover, the calculated contrasts revealed the greater importance of ADHD, compared to CTD in the psychopathology of the comorbid group.
The higher scores of psychopathology in the comorbid group (CTD+ADHD) compared to both ‘pure’ groups (CTD-only, ADHD-only) are consistent with other studies of epidemiological (Gadow et al., 2002; Kurlan et al., 2002) and clinical samples of children (Pierre et al., 1999; Shin et al., 2001; Spencer et al., 1998), children and adults combined (B. G. Comings & D. E. Comings, 1987; D. E. Comings & B. G. Comings, 1987) and older adolescents/adults with CTD (Comings, 1995a, 1995b). Furthermore, the main effect of ADHD on the subscales Aggressive Behavior and Delinquent Behavior is in agreement with the literature (Pierre et al., 1999; Sukhodolsky et al., 2003) and underlines the strong relationship of ADHD to externalizing psychopathology measured by the CBCL. For internalizing behaviors, the highest scores in both groups with CTD (CTD+ADHD and CTD-only) on the subscale Somatic Complaints is also consistent with other results (Carter et al., 2000; Hoekstra et al., 2004; Shin et al., 2001; Termine et al., 2006). In conclusion, our data based on larger samples of higher quality confirm most previous findings.
The present results of a 2×2 factorial design strongly support an additive model of the factors CTD and ADHD from a psychopathological point of view. This is in accordance with neurophysiological data of basic brain functions (Kirov, Kinkelbur, Banaschewski, & Rothenberger, submitted; Moll et al., 2001). On the other hand, an interactive model may come into play if more complex psychopathological conditions (e.g. CTD+ADHD+OCD; see Peterson, Pine, Cohen, & Brook, 2001) or cognitive tasks (Yordanova et al., 1996; Yordanova, Dumais-Huber, Rothenberger, & Woerner, 1997; Yordanova et al., 2006) had been considered.
For the first time, in this study, the relationships of CTD and/or ADHD to different aspects of psychopathology have been specified in detail by computing contrasts of both factors. The found predominance of the ADHD diagnosis on CBCL subscales for Aggressive Behavior, Delinquent Behavior, Attention Problems and Social Problems compared to the CTD diagnosis is in agreement with several previous studies which indicated that disruptive behavior and impairment of psychosocial functioning is associated with ADHD and not with the existence or severity of tics per se (Bawden, Stokes, Camfield, Camfield, & Salisbury, 1998; Carter et al., 2000; Hoekstra et al., 2004; Shin et al., 2001; Spencer, Biederman, Faraone et al., 2001b; Stephens & Sandor, 1999; Sukhodolsky et al., 2003).
Thus, the present data strongly support the recommendation that successful treatment of ADHD has to be the main focus of therapy in most patients comorbid for CTD and ADHD (Banaschewski et al., 2006; Peterson & Cohen, 1998). This is in accordance with the fact that ADHD symptoms, compared to tics, generally impair cognitive, emotional and social skills more severely than tics (Como, 2005; Roessner, Becker, Banaschewski, & Rothenberger, in press; Sukhodolsky et al., 2003). In addition, CTD follow a largely remitting course and have a limited impact on the course and outcome of individuals with ADHD across the life cycle (Spencer, Biederman, Faraone et al., 2001b). Furthermore, the mental effort required to suppress tics may accentuate inattention in ADHD (Brown & Dure, 2005) and attentional problems are negatively correlated with the ability to suppress tics (Himle & Woods, 2005) and positively with the severity of CTD (Cardona et al., 2004). Nevertheless, it was shown that the CTD diagnosis contributed to internalizing psychopathology in a similar way as ADHD. This should be considered for treatment planning when internalizing psychopathology contributes substantially to individual impairment, and implised that both tics and ADHD symptoms should be target of therapy for such cases, e.g. atomoxetine would be superior to stimulants (Allen et al., 2005; Van Brunt et al., 2005).
Limitations
The previous argument that the association between CTD and ADHD may be mainly an artifact of ascertainment bias has been questioned by findings of epidemiological studies (Gadow et al., 2002; Kadesjo & Gillberg, 2000; Kurlan et al., 2002), which are comparable to that of clinical samples (Pauls, Cohen, Kidd, & Leckman, 1988; Pauls, Leckman, & Cohen, 1994). Thus, the present findings (which agree with the results of several previous studies) should also be replicable in an epidemiological sample. The possible objection that there might be a problem of circularity between diagnoses and CBCL scores is refuted on the basis of the limited contribution of CBCL data to our diagnostic process, as well as the findings of group differences even on subscales that are quite independent of the core symptoms of the disorders under investigation. Although the diagnoses were based on routine clinical assessment at a center of excellence for CTD and ADHD, including a wealth of structured multi-informant data with case conferences and best estimate diagnoses under the guidance of experienced board-certified child and adolescent psychiatrist, an internationally accepted, psychometrically reliable and valid semi-structured interview such as the Kiddie-SADS (Kaufman et al., 1997 might have further strengthened the diagnostic classification. While the rate of learning disorders in the three patient groups reflects clinical reality, the rate in the control group is much higher than in other studies. However, ANCOVA results suggested that these group differences in learning disorders had no influence on the results.
Although severity ratings of CTD and ADHD symptoms are an important clinical marker for psychopathology (Cardona et al., 2004), we did not include detailed information from such rating scales (e.g. Conners Rating Scale (Goyette et al., 1978); Tourette Syndrome Severity Scale (TSSS, Walkup et al., 1992); Yale Global Tic Severity Scale (YGTSS, Leckman et al., 1989)) due to missing values in our data set. Similarly, missing information prohibited consideration of the children’s medication status. In light of the clear advantage of investigating large groups of patients without statistical differences in size, age and gender and lacking further comorbid conditions, these limitations seem of minor importance.
Conclusions
In summary, ADHD was found to be strong related to externalizing as well as internalizing psychopathology, and CTD was related to internalizing psychopathology in patients comorbid for CTD and ADHD. This was quantified by calculated contrasts. Our evidence supports an additive model of the co-existence of CTD and ADHD from a psychopathological point of view. Further research using the 2×2 factorial design is necessary to disentangle the overlap between CTD and ADHD and its pathophysiological background.
References
Achenbach, T. M. (1991). Manual for the child behavior checklist 14–18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry.
Allen, A. J., Kurlan, R. M., Gilbert, D. L., Coffey, B. J., Linder, S. L., Lewis, D. W., et al. (2005). Atomoxetine treatment in children and adolescents with ADHD and comorbid tic disorders. Neurology, 65, 1941–1949.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders DSM-IV-TR (Text Revision) (4th ed.). Washington: American Psychiatric Association.
Banaschewski, T., Coghill, D., Santosh, P., Zuddas, A., Asherson, P., Buitelaar, J., et al. (2006). Long-acting medications for the hyperkinetic disorders: A systematic review and European treatment guideline. European Child & Adolescent Psychiatry. [Epub ahead of print].
Bawden, H. N., Stokes, A., Camfield, C. S., Camfield, P. R., & Salisbury, S. (1998). Peer relationship problems in children with Tourette’s disorder or diabetes mellitus. Journal of Child Psychology & Psychiatry, 39, 663–668.
Biederman, J., Monuteaux, M. C., Greene, R. W., Braaten, E., Doyle, A. E., & Faraone, S. V. (2001). Long-term stability of the Child Behavior Checklist in a clinical sample of youth with attention deficit hyperactivity disorder. Journal of Clinical Child Psychology, 30, 492–502.
Bird, H. R. (1996). Epidemiology of childhood disorders in a cross-cultural context. Journal of Clinical Child Psychology, 37, 35–49.
Brown, L., & Dure, L. S. (2005). The treatment of comorbid attention-deficit disorder and Tourette’s syndrome. In R. Kurlan (Ed.), Handbook of Tourette’s syndrome and related tic and behavioral disorders (2 ed., pp. 455–465). New York: Marcel Dekker.
Cardona, F., Romano, A., Bollea, L., & Chiarotti, F. (2004). Psychopathological problems in children affected by tic disorders - study on a large Italian population. European Child & Adolescent Ppsychiatry, 13, 166–171.
Carter, A. S., O’Donnell, D. A., Schultz, R. T., Scahill, L., Leckman, J. F., & Pauls, D. L. (2000). Social and emotional adjustment in children affected with Gilles de la Tourette’s syndrome: associations with ADHD and family functioning. Attention Deficit Hyperactivity Disorder. Journal of Child Psychology & Psychiatry, 41, 215–223.
Chen, W. J., Faraone, S. V., Biederman, J., & Tsuang, M. T. (1994). Diagnostic accuracy of the Child Behavior Checklist scales for attention-deficit hyperactivity disorder: a receiver-operating characteristic analysis. Journal of Consulting and Clinical Psychology, 62, 1017–1025.
Comings, B. G., & Comings, D. E. (1987). A controlled study of Tourette syndrome. V. Depression and mania. American Journal of Human Genetics, 41, 804–821.
Comings, D. E. (1995a). The role of genetic factors in conduct disorder based on studies of Tourette syndrome and attention-deficit hyperactivity disorder probands and their relatives. Journal of Developmental and Behavioral Pediatrics, 16, 142–157.
Comings, D. E. (1995b). Role of genetic factors in depression based on studies of Tourette syndrome and ADHD probands and their relatives. American Journal of Medical Genetics, 60, 111–121.
Comings, D. E., & Comings, B. G. (1987). A controlled study of Tourette syndrome. II. Conduct. American Journal of Human Genetics, 41, 742–760.
Como, P. G. (2005). Neuropsychological function in Tourette’s Syndrome. In R. Kurlan (Ed.), Handbook of Tourette’s syndrome and related tic and behavioral disorders (2 ed., pp. 237–252). New York: Marcel Dekker.
Dilling, H., Mombour, W., & Schmidt, M. H. (2000). Internationale Klassifikation psychischer Störungen, ICD-10, Kapitel V (F). Bern: Huber.
Englert, E., Jungmann, J., Rotthaus, W., Wienand, F., Lam, L., & Poustka, F. (1996). Glossar zur Basisdokumentation Kinder- und Jugendpsychiatrie. Forum der Kinder- und Jugendpsychiatrie und Psychotherapie, III, 38–51.
Gadow, K. D., Nolan, E. E., Sprafkin, J., & Schwartz, J. (2002). Tics and psychiatric comorbidity in children and adolescents. Developmental Medicine and Child Neurology, 44, 330–338.
Gillberg, C., Gillberg, I. C., Rasmussen, P., Kadesjo, B., Soderstrom, H., Rastam, M., et al. (2004). Co-existing disorders in ADHD – implications for diagnosis and intervention. European Child & Adolescent Psychiatry, 13 Suppl 1, I80–92.
Goyette, C. H., Conners, C. K., & Ulrich, R. F. (1978). Normative data on revised Conners Parent and Teacher Rating Scales. Journal of Abnormal Child Psychology, 6, 221–236.
Himle, M. B., & Woods, D. W. (2005). An experimental evaluation of tic suppression and the tic rebound effect. Behaviour Research and Therapy, 43, 1443–1451.
Hoekstra, P. J., Steenhuis, M. P., Troost, P. W., Korf, J., Kallenberg, C. G., & Minderaa, R. B. (2004). Relative contribution of attention-deficit hyperactivity disorder, obsessive-compulsive disorder, and tic severity to social and behavioral problems in tic disorders. Journal of Developmental and Behavioral Pediatrics, 25, 272–279.
Jensen, P. S., Watanabe, H. K., Richters, J. E., Roper, M., Hibbs, E. D., Salzberg, A. D., et al. (1996). Scales, diagnoses, and child psychopathology: II. Comparing the CBCL and the DISC against external validators. Journal of Abnormal Child Psychology. 24, 151–168.
Kadesjo, B., & Gillberg, C. (2000). Tourette’s disorder: epidemiology and comorbidity in primary school children. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 548–555.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1065–1069.
Kirov, R., Kinkelbur, J., Banaschewski, T., & Rothenberger, A. (submitted). Sleep patterns in children with hyperkinetic disorders.
Kurlan, R., Como, P. G., Miller, B., Palumbo, D., Deeley, C., Andresen, E. M., et al. (2002). The behavioral spectrum of tic disorders: a community-based study. Neurology, 59, 414–420.
Leckman, J. F., Riddle, M. A., Hardin, M. T., Ort, S. I., Swartz, K. L., Stevenson, J., et al. (1989). The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. Journal of the American Academy of Child and Adolescent Psychiatry, 28, 566–573.
Moll, G. H., Heinrich, H., Trott, G. E., Wirth, S., Bock, N., & Rothenberger, A. (2001). Children with comorbid attention-deficit-hyperactivity disorder and tic disorder: evidence for additive inhibitory deficits within the motor system. Annals of Neurology, 49, 393–396.
Pauls, D. L., Cohen, D. J., Kidd, K. K., & Leckman, J. F. (1988). Tourette syndrome and neuropsychiatric disorders: is there a genetic relationship? American Journal of Human Genetics, 43, 206–217.
Pauls, D. L., Leckman, J. F., & Cohen, D. J. (1994). Evidence against a genetic relationship between Tourette’s syndrome and anxiety, depression, panic and phobic disorders. The British Journal of Psychiatry, 164, 215–221.
Peterson, B. S., & Cohen, D. J. (1998). The treatment of Tourette’s syndrome: multimodal, developmental intervention. The Journal of Clinical Psychiatry, 59 Suppl 1, 62–72.
Peterson, B. S., Pine, D. S., Cohen, P., & Brook, J. S. (2001). Prospective, longitudinal study of tic, obsessive-compulsive, and attention-deficit/hyperactivity disorders in an epidemiological sample. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 685–695.
Pierre, C. B., Nolan, E. E., Gadow, K. D., Sverd, J., & Sprafkin, J. (1999). Comparison of internalizing and externalizing symptoms in children with attention-deficit hyperactivity disorder with and without comorbid tic disorder. Journal of Developmental and Behavioral Pediatrics, 20, 170–176.
Robertson, M. M. (2000). Tourette syndrome, associated conditions and the complexities of treatment. Brain, 123 Pt 3, 425–462.
Robertson, M. M. (2006). Attention deficit hyperactivity disorder, tics and Tourette’s syndrome: the relationship and treatment implications. A commentary. European Child & Adolescent Psychiatry, 15, 1–11.
Roessner, V., Becker, A., Banaschewski, T., & Rothenberger, A. (in press). Executive functions in children with chronic tic disorders with/without ADHD - new insights. European Child & Adolescent Psychiatry.
Schmeck, K., Poustka, F., Dopfner, M., Pluck, J., Berner, W., Lehmkuhl, G., et al. (2004). Discriminant validity of the child behaviour checklist CBCL-4/18 in German samples. European Child & Adolescent Psychiatry. 10, 240–247.
Shin, M. S., Chung, S. J., & Hong, K. E. (2001). Comparative study of the behavioral and neuropsychologic characteristics of tic disorder with or without attention-deficit hyperactivity disorder (ADHD). Journal of Child Neurology, 16, 719–726.
Spencer, T., Biederman, J., Coffey, B., Geller, D., Faraone, S., & Wilens, T. (2001a). Tourette disorder and ADHD. Advances in Neurology, 85, 57–77.
Spencer, T., Biederman, J., Faraone, S., Mick, E., Coffey, B., Geller, D., et al. (2001b). Impact of tic disorders on ADHD outcome across the life cycle: findings from a large group of adults with and without ADHD. The American Journal of Psychiatry, 158, 611–617.
Spencer, T., Biederman, J., Harding, M., O’Donnell, D., Wilens, T., Faraone, S., et al. (1998). Disentangling the overlap between Tourette’s disorder and ADHD. Journal of Child Psychology and Psychiatry, 39, 1037–1044.
Stephens, R. J., & Sandor, P. (1999). Aggressive behaviour in children with Tourette syndrome and comorbid attention-deficit hyperactivity disorder and obsessive-compulsive disorder. Canadian Journal of Psychiatry, 44, 1036–1042.
Sukhodolsky, D. G., Scahill, L., Zhang, H., Peterson, B. S., King, R. A., Lombroso, P. J., et al. (2003). Disruptive behavior in children with Tourette’s syndrome: association with ADHD comorbidity, tic severity, and functional impairment. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 98-105.
Termine, C., Balottin, U., Rossi, G., Maisano, F., Salini, S., Di Nardo, R., et al. (2006). Psychopathology in children and adolescents with Tourette’s syndrome: A controlled study. Brain & Development, 28, 69–75.
Van Brunt, D. L., Johnston, J. A., Ye, W., Pohl, G. M., Sun, P. J., Sterling, K. L., et al. (2005). Predictors of selecting atomoxetine therapy for children with attention-deficit-hyperactivity disorder. Pharmacotherapy, 25, 1541–1549.
Walkup, J. T., Rosenberg, L. A., Brown, J., & Singer, H. S. (1992). The validity of instruments measuring tic severity in Tourette’s syndrome. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 472–477.
World Health Organisation. (1996). Multiaxial Classification of Child and Adolescent Psychiatric Disorders: The ICD-10 Classification of Mental and Behavioural Disorders in Children and Adolescents. Cambridge: Cambridge University Press.
Yordanova, J., Dumais-Huber, C., & Rothenberger, A. (1996). Coexistence of tics and hyperactivity in children: no additive effect at the psychophysiological level. International Journal of Psychophysiology, 21, 121–133.
Yordanova, J., Dumais-Huber, C., Rothenberger, A., & Woerner, W. (1997). Frontocortical activity in children with comorbidity of tic disorder and attention-deficit hyperactivity disorder. Biological Psychiatry, 41, 585–594.
Yordanova, J., Heinrich, H., Kolev, V., & Rothenberger, A. (2006). Increased event-related theta activity as a psychophysiological marker of comorbidity in children with tics and attention-deficit/hyperactivity disorders. Neuroimage, 15, 940–55.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roessner, V., Becker, A., Banaschewski, T. et al. Psychopathological Profile in Children with Chronic Tic Disorder and Co-existing ADHD: Additive Effects. J Abnorm Child Psychol 35, 79–85 (2007). https://doi.org/10.1007/s10802-006-9086-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-006-9086-z