Abstract
While attention deficit hyperactivity disorder (ADHD) and obsessive compulsive disorder have been shown to have major impacts on quality of life in individuals with Tourette syndrome, there is comparatively little data on how the presence of these comorbidities influence tic severity and treatment. 114 children (mean age 10.25 years) were extensively clinically phenotyped at a single specialty clinic. While there was no difference in Yale Global Tic Severity Scale (YGTSS) scores in children with versus without ADHD, children with obsessive compulsive behaviors had significantly higher YGTSS scores (p = 0.008). There was a significant correlation between YGTSS scores and age (r = 0.344, p < 0.001). Children with ADHD were more likely to be treated for their tics within the first two years of diagnosis (OR 3.51, p = 0.009). As tic severity does not appear to be greater in children with ADHD, this association may relate to greater overall psychosocial impairment in children with this comorbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tourette syndrome (TS) is a childhood onset neuropsychiatric disorder characterized by the presence of multiple motor and at least one vocal tic. TS is common in school age children, with a prevalence close to 1%, affecting boys more frequently than girls [1]. Symptom severity usually peaks in early adolescence, with many individuals reporting an improvement or remission of tics in late adolescence [2, 3]. By adulthood, the prevalence of diagnosed TS falls to less than 0.1% [4].
Many individuals with TS are affected by comorbid conditions; of which the two most commonly reported and studied are Attention Deficit Hyperactivity Disorder (ADHD), and Obsessive Compulsive Disorder (OCD). The proportion of individuals affected by these comorbidities varies depending on sample characteristics, with studies of clinically referred populations reporting higher rates than community based samples [5]. A recent study of lifetime prevalence of comorbid psychiatric disorders in 1374 individuals with TS participating in genetic studies found that 50.0% of their sample met diagnostic criteria for OCD, 54.3% for ADHD, and 29.5% met criteria for all three disorders [6].
Although the pathophysiology of tic generation is incompletely understood, it is postulated that aberrant activity within the basal ganglia and cortico-striato-thalamocortical loops are central to the production of tics [7]. Similarly, models of OCD pathophysiology have focused on cortico-striatal circuitry, as well as involvement of the orbitofrontal cortex, anterior cingulate cortex and amygdala [8]. Both TS and OCD are highly heritable, with multiple studies demonstrating familial clustering of both disorders and significant cross disorder risk. A recent population based study using the Danish national health registries found that in individuals whose oldest sibling was diagnosed with TS or a chronic tic disorder, the relative recurrence risk for TS/chronic tic disorder was 18.63 (95% CI 15.34–22.63) and the relative recurrence risk for OCD was 3.98 (95% CI 2.58–6.12) [9]. This cross disorder risk and the overlapping phenomenological features of TS and OCD suggest that the two disorders may be alternate phenotypes with a shared underlying genetic cause.
The comorbidity between ADHD and TS appears to relate to shared underlying neurobiological and pathophysiological mechanisms rather than a common genetic cause. A family study of individuals with TS only, ADHD only, comorbid TS and ADHD, and controls found that the presence of TS only did not increase the risk of ADHD only in relatives, and conversely that the presence of ADHD only did not increase the risk of TS only in relatives [10]. Some investigators have hypothesized that the overlap in ADHD and TS symptoms and common comorbidity suggest that these disorders are part of a broader neurodevelopmental illness spectrum, which results from processes that cause neural long-range underconnectivity and short-range overconnectivity that may share a similar environmental, or epigenetic etiology [11]. Reduced intracortical inhibition has been described in both disorders, which are significantly and inversely associated with symptom severity [12, 13].
Both ADHD and OCD comorbidity in individuals with TS have been shown in numerous studies to have major impacts on psychosocial function and health related quality of life [14–16]. Negative correlations between clinician rated tic severity scores on the Yale Global Tic Severity Scale and children’s self reported quality of life have also been reported. Interestingly, tic severity was only significantly related to parent rated quality of life in children with low externalizing symptoms, suggesting that parents experience externalizing symptoms as more problematic and disruptive than tics [17].
There is comparatively little data on how the presence and severity of ADHD and OCD comorbidity influence tic severity and the need for treatment of tics. This study sought to understand how the presence, severity and treatment of these two common comorbidities influences tic severity and the need for treatment of tics early in the course of the disorder. Given the shared underlying genetic, neurobiological and pathophysiological mechanisms between TS, OCD and ADHD, comorbidity may be a marker of phenotypic severity, resulting in greater overall symptom severity. Based on previous research, it was hypothesized that comorbid OCD and possibly ADHD would be associated with higher tic severity and influence the need for treatment of tics.
Methods
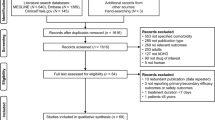
This study was approved by the Conjoint Health Regional Ethics Board of the University of Calgary. This study examined the relationship between the presence of a comorbid ADHD diagnosis, ADHD symptom severity, medical treatment for ADHD, comorbid obsessive compulsive behaviors (OCBs), comorbid OCD diagnosis, OCD symptom severity, treatment for OCD, and (1) tic severity, (2) treatment for tics within the first two years of diagnosis.
Participants in the study were children and youth seen at a single specialty TS clinic over an 18-month period. To be eligible for the study, participants had to be less than 18 years of age and had a legal guardian able to provide informed consent and historical information for the child. Participants had to have a tic diagnosis. The children were extensively clinically phenotyped for the study. All children and their parents underwent a structured clinical interview with a specialist physician to confirm the diagnosis of a tic disorder, assess for common comorbidities and rate symptom severity. The Yale Global Tic Severity Scale (YGTSS) and the Children’s Yale Brown Obsessive Compulsive Symptom Scale (CYBOCS) were completed with the patient and their parent(s) by the specialist physician or nurse to measure the severity of tics and obsessive compulsive behaviors. Both the specialist physician and nurse have used these instruments extensively in clinical practice and for research. Inter-rater reliability was not formally assessed for the purposes of this study. Parents completed the Conner’s 3 Parent Short as a measure of ADHD symptom severity.
Children were classified as having one of four possible tic disorder diagnoses: Tourette Syndrome, Chronic Motor Tic Disorder, Chronic Vocal Tic Disorder, and Provisional Tic Disorder if symptoms had not yet been present for at least one year. Children were classified as having obsessive compulsive behaviors if they endorsed obsessions or compulsions on the CYBOCS symptom checklist. Only children having at least mild impairment or disability related to obsessive compulsive behaviors were classified as having OCD (CYBOCS score 8 or greater). Children were classified as having ADHD if they met DSM criteria for the inattentive, hyperactive or combined subtype.
The YGTSS has a total tic score with a maximum score of 50 points, made up of a motor tic subscore and a vocal tic subscore (25 points each). Tic related impairment is rated on a scale of 0 to 50 points. The YGTSS total score therefore has a maximum score of 100 points, 50 points from the total tic score and 50 points from the tic related impairment score. The Children’s Yale Brown Obsessive Compulsive Symptom Scale has a maximum score of 40 points, with 20 points pertaining to obsessions and 20 points pertaining to compulsions. The Conner’s 3 Parent Short yields age and sex specific T-scores in six different domains- Inattention, Hyperactivity, Executive Function, Learning Problems, Peer Relations, and Aggression. For the purpose of this research, only the Inattention and Hyperactivity domains were evaluated.
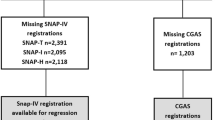
All continuous variables were assessed for normality. It was determined that age and YGTSS scores were normally distributed while CYBOCS and Conner’s Parent Short T scores were not. Two sample t tests were performed to evaluate for differences in the YGTSS total tic score in individuals with and without treatment for tics within the first two years of symptom onset, sex, an ADHD diagnosis, medical treatment for ADHD, the presence of OCBs, OCD diagnosis, and the treatment of OCD. Correlations between YGTSS total tic scores and CYBOCS scores or Conner’s Parent Short Inattention and Hyperactivity T scores were measured using Spearman’s rho. Correlations between the YGTSS total tic scores and age were measured using the Pearson correlation. Analysis of covariance was used to assess the relationship between the YGTSS total tic score and age, sex, treatment for tics, ADHD diagnosis, ADHD treatment, the presence of OCBs, OCD diagnosis, and OCD treatment as independent variables. Non-significant variables were removed from the model and interactions between variables were tested to create a final model.
Odds ratios were measured for the association between treatment for tics within the first two years of symptom onset and ADHD diagnosis, medical treatment for ADHD, presence of OCBs, OCD diagnosis and treatment of OCD.
All statistical analyses were performed using STATA statistical software.
Results
There were 114 children in the sample, with a mean age of 10.25 years (SD 3.01, range 5–17) (Table 1). Males accounted for 79% of the sample. A diagnosis of Tourette syndrome was present in 73%, Chronic Motor Tic Disorder in 13%, Chronic Vocal Tic Disorder in 3% and Provisional Tic Disorder in 11%.
A diagnosis of comorbid ADHD was present in 39% of children; OCBs in 35%; and OCD in 7%. The mean total tic severity score on the YGTSS was 17.10 points (SD 8.78, range 0–43), and the mean tic plus impairment score on the YGTSS was 30.78 (SD 18.56, range 0–74).
Treatment for tics was required in 24 children (21%) within the first two years of symptom onset. Mean YGTSS scores were higher by 5.89 points (95% CI 2.03–9.76, p = 0.002) in children requiring treatment for tics than in those who did not.
There was no difference in YGTSS total tic scores between children diagnosed with versus without ADHD (Table 2). Children treated with medication for ADHD (stimulants or non-stimulants) had borderline significant higher total tic scores by 3.37 points (95% CI −0.13 to 6.86, p = 0.029).
YGTSS total tic scores were significantly higher in children with OCBs by 4.13 points (95% CI 0.78–7.47, p = 0.008). There was no difference in YGTSS total tic scores between children diagnosed with versus without OCD, or between children treated versus untreated for OCD.
Evaluation of Spearman correlations revealed a borderline positive correlation between the YGTSS total tic score and the Conners’ Parent Report Hyperactivity T-score (Spearman’s rho 0.227, p = 0.016). There was no correlation between the YGTSS total tic score and the Conners’ Parent Report Inattention T-score or the Children’s Yale Brown Obsessions and Compulsions Scale score. Evaluation of Pearson’s correlation between the YGTSS and age revealed a significant correlation, with an r of 0.344 (p < 0.001).
Analysis of covariance examining the relationship between YGTSS total tic score and age, sex, treatment for tics, ADHD diagnosis, ADHD treatment, the presence of OCBs, OCD diagnosis, and OCD treatment revealed a significant relationship only with age and treatment for tics. The coefficient for age was 0.92 (95% CI 0.42–1.42, p < 0.001), and the coefficient for treatment of tics was 5.06 (95% 1.37–8.76, p = 0.008).
There was an association between treatment for tics within the first 2 years of symptom onset and the diagnosis of ADHD, and medical treatment for ADHD (Table 3). Children with a comorbid ADHD diagnosis were more likely to be treated for their tics, with an odds ratio of 3.51 (95% CI 1.37–8.95). Similarly, children treated medically for ADHD had an odds ratio of 4.60 (95% CI 1.78–11.86) for the treatment of tics. There was no association between treatment for tics within the first 2 years of symptoms onset and OCBs, OCD, or the treatment of OCD.
Discussion
This clinic based study found significantly greater current tic severity in individuals with obsessive compulsive behaviors, and borderline significantly greater tic severity in children receiving medical treatment for ADHD symptoms. Mean tic severity was also greater in individuals diagnosed with ADHD or OCD, and those requiring treatment for OCD, but the difference was not statistically significant. This may have been partly due to sample size, at least for the OCD variables, as there were very few children in the sample that met criteria for OCD and required treatment. Most of the children in the sample were less than 12 years of age, and previous research has shown that rates of comorbid OCD tend to increase in adolescence [3, 18]. Not surprisingly, individuals requiring treatment for tics within the first 2 years of symptom onset had significantly worse tic severity. In a model including all comorbidity variables, age and treatment for tics, only age and treatment for tics remained significant predictors of current tic severity. The association between age and tic severity is in keeping with previous research, as natural history studies have shown an increase in tic severity with age that peaks between the age of 10 and 12, followed by a gradual improvement in late adolescence [19].
Other studies evaluating the effect of comorbidity on tic severity have demonstrated similar findings. Using the Tourette syndrome International database Consortium (TIC) database, Roessner studied the impact of ADHD on developmental psychopathology in children and adolescents with TS [15]. In their sample, which includes 5060 children and adolescents from 27 countries, 61.2% suffered from TS with co-occurring ADHD. Peak tic severity was rated on a three step scale (mild, moderate or severe), and no difference was found in tic severity between individuals with or without ADHD. Comorbid ADHD was associated however with an earlier onset of tics, and a higher rate of other comorbid conditions. Similarly, Sukhodolsky studied the association of disruptive behavior with social, adaptive and family functioning in TS with and without comorbid ADHD [14]. They found no differences in the YGTSS total current or worse-ever tic severity scores between children with TS only and TS plus ADHD. However, children with TS plus ADHD had significantly greater ratings of aggression and delinquent behaviors than control children, while children with TS only did not. Based on the findings from these two studies and our own data, the effect of a comorbid ADHD diagnosis on tic severity appears to be minimal. In contrast, numerous studies have shown that comorbid ADHD has clear implications on psychosocial functioning in individuals with TS, though this does not appear to be related to any direct effect on tic severity.
Lebowitz studied the associations between the presence of comorbid ADHD and OCD and the severity of tics in 158 children with TS [20]. In this sample, 53.8% had comorbid OCD, and 38.6% had comorbid ADHD. Similar to our study, they found that youth with comorbid OCD had significantly greater tic severity on the YGTSS than those without OCD, while subjects with ADHD showed a non-significant trend to more severe tics compared to those without ADHD. The association between tic severity and comorbid OCBs or OCD likely relates to the overlapping phenomenology of these disorders, or may be a marker of overall greater phenotypic severity in individuals with this comorbidity. Previous work has shown that TS patients with co-morbid OCD are more likely to present with complex tics at onset than those without OCD [21]. Distinguishing between complex tics and compulsions can be challenging for both patients and clinicians, especially in children. While the presence of an obsessive thought connected to a repetitive act generally guides one to label it as compulsion rather than a complex tic, the ability to articulate obsessive thoughts or the aim of compulsions may be lacking. Current evidence suggests that first line treatment of OCD in individuals with tics should be cognitive behavioral therapy (CBT), as individuals with tics may not respond as well to SSRIs for OCD symptoms as individuals without tics [22, 23]. In contrast, children with OCD with tics appear to respond just as well to cognitive behavioral therapy as children with OCD only [24].
While tic severity was no greater in individuals with ADHD, our study found that those with an ADHD diagnosis or requiring medical treatment for ADHD were more likely to be treated for their tics. There are a few possible reasons for this association. While randomized controlled trials of both methylphenidate and dextroamphetamine in children with tics and ADHD have found overall improvements in mean tic severity, worsening of tics was demonstrated at higher doses of dextroamphetamine, and limited dosage increases of methylphenidate [25]. Some treatments, such as the alpha agonists, have been proven effective in treating tics, inattention, hyperactivity and oppositional behavior [26–28]. Parents may feel more comfortable using medication if it will help with several symptoms, which together add to a greater overall burden on psychosocial functioning. Children requiring treatment for ADHD symptoms are by definition more severely affected, and greater ADHD symptom severity is one of the most important predictors of psychosocial quality of life in children with TS [16]. The overall greater impairment in psychosocial quality of life in children with TS + ADHD is very likely to influence treatment decisions for tics. While individuals without an ADHD comorbidity may be prepared to tolerate their tics, the added difficulties associated with tics in a child with psychosocial impairment related to ADHD symptoms may be more overwhelming.
Limitations to this study include the use of a clinically ascertained sample, which by nature will include only those individuals with symptoms requiring medical attention, and is more likely to include individuals with comorbid disorders. As the focus of this study was on the influence of comorbid ADHD and OCD on tic severity and treatment, the sample was appropriate for the study question. The results however, may not be generalizable to individuals with tics in community-based populations. In addition, the contribution of other common comorbidities, such as Oppositional Defiant Disorder and Generalized Anxiety Disorder, were not assessed in this sample.
Implications of the current study include the need to ensure a holistic approach to assessment and treatment of children with tics. The American Academy of Child and Adolescent Psychiatry recommends assessment of all children with tics for comorbid disorders, and treatment of both tics and comorbidity based on the level of distress and impairment [29]. While children with ADHD did not have greater tic severity than those without this diagnosis, they were more likely to be treated for their tics. A comprehensive treatment approach, such as the “Living with Tics” cognitive behavioral intervention [30] which includes modules on problem solving, emotional regulation, and parent training for disruptive behaviors, may result in greater overall improvement in quality of life and function in these youth with multiple treatment needs. Future research such as longitudinal studies evaluating tic, OCD and ADHD severity from early childhood to the end of adolescence may be helpful in understanding if the presence and severity of these comorbid disorders affects long-term outcome and remission of tics.
Summary
The present study examined how the presence and severity of Attention Deficit Hyperactivity Disorder and Obsessive Compulsive Disorder influence tic severity and the need for treatment of tics in children with Tourette syndrome. Participants were 114 children aged 5–17 years seen at a single specialty clinic. Results showed that tic severity was significantly higher in children receiving treatment for their tics, and a significant positive correlation between tic severity and age. There was no difference in tic severity between children diagnosed with versus without ADHD, while tic severity was significantly higher in children with OCBs. Children diagnosed and treated for ADHD were more likely to be treated for their tics. As tic severity does not appear to be greater in the children with ADHD, the higher odds of tic treatment may relate to the greater overall psychosocial impairment associated with this comorbidity. The findings of this study reinforce recommendations that children with tics should be assessed for comorbid conditions, with treatment focused on those symptoms that cause the most impairment in daily life.
References
Knight T, Steeves T, Day L, Lowerison M, Jette N, Pringsheim T (2012) Prevalence of tic disorders: a systematic review and meta-analysis. Pediatr Neurol 47(2):77–90. doi:10.1016/j.pediatrneurol.2012.05.002
Bloch MH, Leckman JF (2009) Clinical course of Tourette syndrome. J Psychosom Res 67(6):497–501
Bloch MH, Peterson BS, Scahill L, Otka J, Katsovich L, Zhang H et al (2006) Adulthood outcome of tic and obsessive-compulsive symptom severity in children with Tourette syndrome. Arch Pediatr Adolesc Med 160(1):65–69. doi:10.1001/archpedi.160.1.65
Yang J, Hirsch L, Martino D, Jette N, Roberts J, Pringsheim T (2016) The prevalence of diagnosed tourette syndrome in Canada: a national population-based study. Mov Disord 31(11):1658–1663. doi:10.1002/mds.26766
Kurlan R, Como P, Miller B, Palumbo D, Deeley C, Andresen EM et al (2002) The behavioural spectrum of tic disorders. A community based study. Neurology 59:414–420
Hirschtritt ME, Lee PC, Pauls DL, Dion Y, Grados MA, Illmann C, et al. Lifetime prevalence, age of risk, and genetic relationships of comorbid psychiatric disorders in Tourette syndrome. JAMA Psychiatry. 2015;72(4):325–333. doi:10.1001/jamapsychiatry.2014.2650
Ganos C, Roessner V, Munchau A (2013) The functional anatomy of Gilles de la Tourette syndrome. Neurosci Biobehav Rev 37(6):1050–1062. doi:10.1016/j.neubiorev.2012.11.004
Milad MR, Rauch SL (2012) Obsessive-compulsive disorder: beyond segregated cortico-striatal pathways. Trends Cogn Sci 16(1):43–51. doi:10.1016/j.tics.2011.11.003
Browne HA, Hansen SN, Buxbaum JD, Gair SL, Nissen JB, Nikolajsen KH, et al. Familial clustering of tic disorders and obsessive-compulsive disorder. JAMA Psychiatry. 2015;72(4):359–366. doi:10.1001/jamapsychiatry.2014.2656
Stewart SE, Illmann C, Geller DA, Leckman JF, King R, Pauls DL (2006) A controlled family study of attention-deficit/hyperactivity disorder and Tourette’s disorder. J Am Acad Child Adolesc Psychiatry 45(11):1354–1362. doi:10.1097/01.chi.0000251211.36868.fe
Kern JK, Geier DA, King PG, Sykes LK, Mehta JA, Geier MR (2015) Shared brain connectivity issues, symptoms, and comorbidities in autism spectrum disorder, attention deficit/hyperactivity disorder, and Tourette syndrome. Brain Connect 5(6):321–335. doi:10.1089/brain.2014.0324
Gilbert DL, Bansal AS, Sethuraman G, Sallee FR, Zhang J, Lipps T et al (2004) Association of cortical disinhibition with tic, ADHD, and OCD severity in Tourette syndrome. Mov Disord 19(4):416–425. doi:10.1002/mds.20044
Orth M, Rothwell JC (2009) Motor cortex excitability and comorbidity in Gilles de la Tourette syndrome. J Neurol Neurosurg Psychiatry 80(1):29–34. doi:10.1136/jnnp.2008.149484
Sukhodolsky DG, Scahill L, Zhang H, Peterson BS, KIng R, Lombroso PJ et al (2003) Disruptive behaviour in children’s with Tourette’s syndrome: association with ADHD comorbidity, tic severity and functional impairment. J Am Acad Child Adolesc Psychiatry 42(1):98–105. doi:10.1097/01.CHI.0000024904.60748.3A
Roessner V, Becker A, Banaschewski T, Freeman RD, Rothenberger A, Tourette Syndrome International Database C (2007) Developmental psychopathology of children and adolescents with Tourette syndrome–impact of ADHD. Eur Child Adolesc Psychiatry 16(Suppl 1):24–35. doi:10.1007/s00787-007-1004-6
Pringsheim T, Lang A, Kurlan R, Pearce M, Sandor P (2009) Understanding disability in Tourette syndrome. Dev Med Child Neurol 51(6):468–472. doi:10.1111/j.1469-8749.2008.03168.x
Storch EA, Merlo LJ, Lack C, Milsom VA, Geffken GR, Goodman WK et al (2007) Quality of life in youth with Tourette’s syndrome and chronic tic disorder. J Clin Child Adolesc Psychol 36(2):217–227
Ford T, Goodman R, Meltzer H (2003). The British Child and Adolescent Mental Health Survey 1999: The prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry. 42(10):1203–1211.
Leckman JF, Zhang H, Vitale A, Lahnin F, Lynch K, Bondi C et al (1998) Course of tic severity in Tourette syndrome: the first two decades. Pediatrics 102(1 Pt 1):14–19
Lebowitz ER, Motlagh MG, Katsovich L, King RA, Lombroso PJ, Grantz H et al (2012) Tourette syndrome in youth with and without obsessive compulsive disorder and attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry 21(8):451–457. doi:10.1007/s00787-012-0278-5
Santangelo SL, Pauls DL, Goldstein JM, Faraone SV, Tsuang MT, Leckman JF (1994) Tourette’s Syndrome: what are the influences of gender and comorbid obsessive-compulsive disorder? J Am Acad Child Adolesc Psychiatry 33(6):795–804
March JS, Biederman J, Wolkow R, Safferman A, Mardekian J, Cook EH et al (1998) Sertraline in children and adolescents with obsessive-compulsive disorder: a multicenter randomized control trial. JAMA 280:1752–1756
March JS, Franklin ME, Leonard H, Garcia A, Moore P, Freeman J et al (2007) Tics moderate treatment outcome with sertraline but not cognitive-behavior therapy in pediatric obsessive-compulsive disorder. Biol Psychiatry 61(3):344–347. doi:10.1016/j.biopsych.2006.09.035
Hojgaard DR, Skarphedinsson G, Nissen JB, Hybel KA, Ivarsson T, Thomsen PH (2016) Pediatric obsessive-compulsive disorder with tic symptoms: clinical presentation and treatment outcome. Eur Child Adolesc Psychiatry. doi:10.1007/s00787-016-0936-0
Pringsheim T, Steeves T (2011) Pharmacological treatment for attention deficit hyperactivity disorder (ADHD) in children with comorbid tic disorders. Cochrane Database Syst Rev 4 (CD007990)
Kurlan R, Goetz CG, McDermott MP, Plumb S, Singer H, Dure L et al (2002) Treatment of ADHD in children with tics: A randomized controlled trial. Neurology 58(4):527–536
Pringsheim T, Hirsch L, Gardner D, Gorman DA (2015) The pharmacological management of oppositional behaviour, conduct problems, and aggression in children and adolescents with disruptive behaviour disorders: a systematic review and meta-analysis. Part 1: psychostimulants, alpha-2 agonists, and atomoxetine. Can J Psychiatry 60(2):42–51
Scahill L, Chappell PB, Kim YS, Schultz RT, Katsovich L, Shepherd E et al (2001) A placebo-controlled study of guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder. Am J Psychiatry 158(7):1067–1074
Murphy TK, Lewin AB, Storch EA, Stock S (2013) Practice parameter for the assessment and treatment of children and adolescents with tic disorders. J Am Acad Child Adolesc Psychiatry 52(12):1341–1359
McGuire JF, Arnold E, Park JM, Nadeau JM, Lewin AB, Murphy TK et al (2015) Living with tics: reduced impairment and improved quality of life for youth with chronic tic disorders. Psychiatry Res 225(3):571–579. doi:10.1016/j.psychres.2014.11.045
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Rights and permissions
About this article
Cite this article
Pringsheim, T. Tic Severity and Treatment in Children: The Effect of Comorbid Attention Deficit Hyperactivity Disorder and Obsessive Compulsive Behaviors. Child Psychiatry Hum Dev 48, 960–966 (2017). https://doi.org/10.1007/s10578-017-0718-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-017-0718-z