Abstract
Aim
To compare intraocular pressure (IOP) measurements obtained with the Perkins applanation tonometer and Icare PRO (ICP) rebound tonometer in anesthetized aphakic or strabismus children. Furthermore, intra-operator correlation and inter-operator correlation have been evaluated, along with the effects of central corneal thickness (CCT) on IOP measurements.
Methods
Seventy children undergoing examination under anesthesia with sevoflurane for aphakic patients and for surgery for strabismus were included. IOP have been measured twice immediately after anesthesia induction with both Perkins applanation tonometer (PAT) and ICP in one eye and by two different operators with both devices in the fellow eye. Furthermore, CCT was measured with ultrasound pachymetry Pacline (Optikon). Agreement between the device measurements has been evaluated using Bland–Altman analyses. Repeatability and reproducibility of the device have been evaluated with intraclass correlation coefficient (ICC) with a value > 0.75 associated with excellent reliability. The relationship between IOP and CCT has been evaluated with Spearman’s correlation coefficient r and determination coefficient r2.
Results
Mean difference in IOP measurements between ICP and PAT was 1.97 mmHg ± 1.23 mmHg (p < 0.05). This difference appeared to be higher in aphakic patients (mean difference 2.15 ± 1.35) than in patients undergoing strabismus surgery (mean difference 1.83 mmHg ± 1.12). Intraclass correlation coefficient (ICC) is used to evaluate repeatability and reproducibility, which are both high for PAT (repeatability 0.96, reproducibility 0.76) compared with ICP (repeatability 0.81, reproducibility 0.70). Correlation coefficient between CCT and IOP is 0.66 for both ICP and PAT.
Conclusion
ICP tends to overestimate IOP compared to PAT. Repeatability and reproducibility are both high for PAT as compared to ICP. A significant correlation between IOP and CCT for both instruments has been demonstrated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intraocular pressure (IOP) measurement is fundamental in the diagnosis of aphakic glaucoma, occurring in up to 45% of children after surgery for congenital cataract [1, 2]. Goldmann applanation tonometer (Haag-Streit, Switzerland—GAT) is the gold standard in IOP measurement, yet its application is not always feasible in children due to lack of cooperation associated with the discomfort from the contact of the probe with the corneal surface and the need of using it in sitting position. Perkins applanation tonometer (Kowa Company, Japan—PAT) is a portable device that shares the same applanation principle used in GAT; it requires topical anesthesia and can be used both in sitting and in supine positions. It is the portable device providing the most accurate IOP measurement (also if compared to GAT) [3, 4].
Icare PRO (ICP) is a tonometer based on the rebound principle, as a small probe ejected onto the corneal surface, after an instant impact, undergoes a deceleration whose value is used by a software to calculate the IOP. ICP has been shown to provide IOP measurements generally higher than those obtained with GAT [5].
In clinical practice, various tonometers can be used, and we have to switch the tonometer depending on the situation (e.g., in children, bed-ridden patients, and poorly compliant patients). Agreement and repeatability among devices have been reported previously, but direct comparison between ICP and PAT is poor in the literature, especially in pediatric patients.
The aim of the present study is to compare IOP measurements obtained with ICP and PAT.
According to our opinion, this comparison can be useful because of the lack of standardization in IOP measurement in children under anesthesia. The IOP measurement in some clinical situation (for example, in aphakic children) is very critical, and few variations of IOP value could influence the clinical decision.
In addition, the correlation between central corneal thickness (CCT) and IOP measurements obtained with both devices has been analyzed.
Materials and methods
This prospective observational study has been carried out between December 2016 and June 2017 at the University Eye Clinic of the San Giuseppe Hospital (Milan, Italy). Patients were recruited from those referred to our Clinic for scheduled surgery for strabismus and for examination under anesthesia after phacoaspiration for congenital cataract. All patients enrolled were aged under 10 years of age. The youngest child is 2 months old. Exclusion criteria were: corneal astigmatism ≥ 2 D (to avoid any cases of corneal ectasia) and infectious inflammatory diseases evaluated during pre-operatory examination. Participation to the study has been proposed to parents/tutors during pre-operatory examination. Our study has been approved from the local ethic committee and abides by the tenets laid down in the Declaration of Helsinki.
IOP measurements were obtained immediately after anesthesia induction with sevoflurane. The measurement was taken by, P.N. and M.S., two pediatric ophthalmologists with more than 30-year experience. In the first eye, a single operator took measurements using both PAT and ICP to evaluate intra-operator repeatability. In the second eye, two different operators took independent measurements using PAT and ICP, respectively, to evaluate inter-operator reproducibility. In order to avoid confounding factors, the order of devices, the operators and the eyes were randomized.
PAT and ICP were calibrated according to the manufacturer’s instruction. For PAT, one IOP measurement was recorded. For ICP, only measurements resulting as “deviation: ok” in the device’s display were recorded, in order to evaluate just the measurements whose deviation was < 15%, as resulting from the manufacturer’s instructions. Ultimately, before surgery, CCT has been measured with ultrasound pachymeter Pacline (Optikon); three different measurements have been recorded, along with their mean.
The main variable of our measurements is the difference between the measurements with both PAT and ICP. Agreement between the devices has been evaluated using Bland–Altman analyses, with 95% limits of agreement [6]. Repeatability and reproducibility have been evaluated with intraclass correlation coefficient (ICC) in a causal-effect regression model [7]. ICC < 0.40 is conventionally considered as poor reliability, while ICC > 0.75 is associated with excellent reliability of the device. The relationship between IOP and CCT has been evaluated with Spearman’s correlation coefficient r and determination coefficient r2.
All statistical analyses were performed using Microsoft Excel 14.0.0 and GraphPad Prism 7. A p < 0.005 has been considered statistically significant.
Results
A total of 70 patients aged from 2 months to 10 years were recruited, 41 (58.57%) of them undergoing strabismus surgery (S) and 29 (41.43%) of them undergoing examination under sedation after phacoaspiration for congenital cataract (A). Mean age of enrolled patients was 4.30 ± 4.41 (range 0–10) years. Mean IOP was 13.40 ± 1.74 mmHg (range 9.8–22.1) using ICP and 11.43 ± 1.72 mmHg [7,8,9,10,11,12,13,14,15] using PAT. Results of patients suffering from strabismus and from congenital cataract are shown in Table 1.
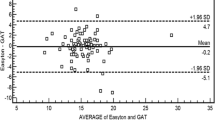
Difference between measurements carried out with ICP and PAT is 1.97 (SD ± 1.23 mmHg, upper LoA 4.38, lower LoA − 0.44). The difference is slightly lower in patients undergoing strabismus surgery (1.83 ± 1.12 mmHg, upper LoA 4.03, lower LoA − 0.37) and is higher in aphakic patients undergoing examination under sedation (2.16 ± 1.35 mmHg, upper LoA 4.80, lower LoA − 0.49) (Table 2).
There is a mean difference between measurements, along with 95% confidence interval. Limits of Agreement (LoA) was evaluated using Bland–Altman plot (Figs. 1, 2, 3).
Linear regression analysis of the difference between IOP measurements of both devices shows a non-statistically significant (p = 0.8273) tendency to have an increase in measurements’ difference with the increase in mean value of IOP obtained with both devices, with regression line y = 0.0098x + 1,8443, and r2 = 0.0002. Results are shown in Fig. 4.
Intra-operator repeatability of measurements obtained with ICP is characterized by ICC = 0.81 (Fig. 5), while using PAT ICC = 0.96 (Fig. 6). For what concerns inter-operator reproducibility, ICC = 0.70 (Fig. 7) with ICP and ICC = 0.76 with PAT (Fig. 8).
Table 3 shows the difference of ICC for both devices in patients suffering from strabismus and aphakic patients.
Spearman correlation coefficient r between measurements obtained with ICP and CCT is r = 0.66; the same value has been observed in measurements obtained with PAT (r = 0.66). Data concerning r in patients’ subgroups are shown in Table 4, along with determination coefficient r2.
Correlation between measurements obtained with both devices and CCT is graphically shown in Figs. 9, 10.
Discussion
There are few studies on the direct comparison between different portable tonometers, since the performance of portable tonometers was more frequently compared to a non-portable Goldmann (GAT) tonometer, which is nowadays the gold standard for measuring the IOP. Shortly after its development, during the 1970s and 1990s, the tonometric values detected with PAT were compared with those obtained with GAT in numerous studies [3, 6]. All these studies have established a good correlation between the pressure values detected with these two instruments, with a coefficient of correlation r which is near 0.91. In 2014, Arora et al. have established that the mean difference between the tonometric values measured with GAT and PAT is near 0.22 ± 0.44 mmHg [7]. This good correlation has also been demonstrated in patients with edematous cornea [8].
Reports that compare the tonometric values obtained with ICP and those obtained with GAT are also numerous. These studies have been carried out mainly on the adult population, and they are quite consistent in underlining the tendency of ICP to overestimate the IOP compared to GAT [9, 10]. In general, the mean difference between the two instruments is around 1.0 ± 2.5 mmHg. On the other hand, it has been shown that ICP tends to underestimate the values of IOP compared to GAT in some cases of high-pressure value [11, 12].
Furthermore, Icare TA01i has been shown to be less reliable than Icare PRO in comparison with GAT. Moreno-Montanes et al. showed that 79% of patients whose IOP had been evaluated with ICP had values with a difference less than 3 mmHg compared to GAT, while only 67% of patients whose IOP had been evaluated with Icare TA01i had values less than 3 mmHg [13].
In evaluation of these data, PAT is a closer tool to GAT precision, if compared to ICP, but is more difficult to use as a portable tonometer in children who were awake. In fact, the use of PAT requires supplements such as fluorescein and local anesthetic, because of the contact between the measuring cone and the cornea. These aspects make PAT an instrument that can create discomfort in pediatric patients. All in all, ICP is the easiest tonometer because it is easy to use in pediatric patient. For these reasons, a comparison between the two devices is very useful.
In our patients’ group, mean IOP values of 13.40 ± 1.74 mmHg and 11.43 ± 1.72 mmHg were established with ICP and PAT.
The mean difference between the tonometric values measured with ICP and PAT is statistically significant (p < 0.05) and is equal to 1.97 ± 1.23 mmHg. This is in agreement with the known literature about the comparison between applanation tonometry and rebound tonometry, even if there are few works about this. The first study comparing the portable tonometers was written in 2006 by Garcia-Resua et al.: They measured the tonometric values in a population of 65 subjects of young adult with PAT and with Icare TA01i, a device that cannot be used in a supine position. In these subjects, a tendency of Icare TA01i to overestimate the IOP values detected with PAT [8] was observed.
In 2013, Li et al. observed an average difference of 2.0 ± 1.8 mmHg in the tonometric values measured with Icare TA01i and PAT. They found that 95% limits of agreement between the two methods distributed between − 1.6 and 5.6 mm Hg [4]. The first comparative evaluation between ICP and PAT was carried out by Jablonski et al. in 2013: an average difference between the pressure values measured in the supine with ICP and PAT of 0.1 with 95% limits of agreement of − 3.6 to 3.8 mm Hg [15]. In 2015, Nakakura et al. confirmed these results, demonstrating a mean difference between these two instruments of 0.43 ± 2.28 mm Hg with 95% limits of agreement − 4.04 to 4.90 mm Hg [3]. More recently, Borrego-Sanz et al. showed a difference near to 0.42 ± 3.69 mmHg with 95% limits of agreement 7.7 to − 6.8 mm Hg between the pressure values measured with ICP and PAT in subjects with congenital glaucoma [5].
Clinical evaluation in our patients shows that the difference between tonometric values measured with ICP and PAT is significantly higher in aphakic patients (2.16 ± 1.35 mmHg) than in patients with strabismus (1.83 ± 1.12 mmHg). This indicates a tendency of ICP to provide significantly higher tonometric values in aphakic patients than in patients with strabismus.
Determination of IOP is influenced by several corneal properties including elasticity, rigidity and central thickness [16]. Surgical intervention on corneal tissue induces tissue structural changes and alters the corneal biomechanical properties. It is well known that central corneal thickness (CCT) increased after congenital cataract surgery [17,18,19]. In contrast, limited information is available on corneal biomechanical properties. According to Faramarzi et al. [20], corneal hysteresis (CH) decreased permanently after lensectomy. Simsek et al. reported that CH was lower in aphakic eyes, but there is no difference in corneal resistance factor (CRF) among normal and aphakic eyes [18].
To our knowledge, there are studies that analyze the difference in terms of agreement between ICP and PAT in postsurgical aphakia. Probably, the difference that we found is due to the different response modalities of the rebound tonometer on aphakic eye, in which the cornea has surgical alterations (change in CCT, CH and CRF), compared to a patient suffering from strabismus, in which the cornea has no postsurgical changes.
Jorge et al. [21] found that CH was correlated with rebound tonometer IOP value. Also, Chui and colleagues [22] found that rebound tonometry measurement was affected by CH and CRF; the same results were reported by Shin et al. [23] in a study including patients with glaucoma. To our knowledge, the only study that compares the effect of CH and CCT on IOP value obtained with rebound tonometry and applanation tonometry was conducted by Brown et al. [24].
According to their result, thinner CCT was significantly associated with lower value of IOP using both Icare and GAT, but GAT measurement is affected greater. Moreover, lower CH was associated with higher IOP using Icare and GAT, but GAT was more affected by CH than Icare. Then, the difference between GAT and Icare was greatest with higher CCT and lower CH.
Despite few studies and sometimes controversial results, these data could explain the greater difference between ICP and PAT in our study and the tendency to have higher IOP value with ICP in aphakic eye.
Our study shows the repeatability and reproducibility of ICP and PAT, with ICC values ranging from 0.63 to 0.97. These results confirm the previously reported good repeatability and reproducibility data of the Icare systems [25, 26].
However, most of the published studies report IOP values obtained in a sitting position.
In 2015, Nakakura et al. [3] showed that correlation values tend to be lower in the supine position. Finally, there is a statistically significant positive correlation between the tonometric values measured with both the ICP and PAT methods, and the central corneal thickness values, with a variable of coefficient of correlation r in a range from 0.62 to 0.70. This indicates that the measured tonometric values tend to increase as the CCT increases.
Many papers analyzed the correlation between the corneal characteristics and the IOP values measured by the various instruments, reporting very heterogeneous results. Nakakura et al. [3] and Jablonski et al. [15] did not demonstrate a correlation between CCT and IOP values measured with PAT and ICP, either in a supine or in a sitting position. Also, Borrego-Sanz et al. [5], when comparing between PAT and ICP in a pediatric population with congenital glaucoma, did not report a significant correlation between tonometric values measured with the two instruments and the CCT. Li et al. [4] have established that both instruments can give higher IOP values with increasing corneal thickness, which tends to be higher for Icare TA01i compared to PAT. In the patients of our study, there are no statistically significant differences related to the correlation between CCT and IOP using ICP rather than PAT.
The results of our study cannot be generalized to clinic sitting tonometry because the IOP is measured in supine position and under gas anesthesia; both these conditions affect the IOP value. It is accepted that IOP increases in supine versus sitting position [27]. It would have been interesting when compared between supine and sitting IOP, but patient in this study was under sedation because ophthalmic examination could not be conducted while they were awake. A limit of this study is the influence of sevoflurane on IOP values. It is known that sevoflurane affects IOP value with a reduction up to 15% in 8 min following induction of anesthesia [28]. We cannot rule out IOP change because of anesthetic, although the measurements were taken immediately after induction in order to limit as much as possible the effects of sevoflurane on the IOP.
Conclusion
The results obtained demonstrate that ICP can overestimate IOP values, with a statistically significant difference compared to PAT. This higher measurement was already known in previous works and tends to be higher with higher IOP values and in patients with postsurgical aphakia after congenital cataract aspiration. Both devices show good repeatability and reproducibility of measurements, ensuring a high reliability of the measured values. It should be considered that IOP values obtained tend to be on average 1.97 mmHg which is higher than PAT, which is known to be similar to GAT, the current gold standard for measuring IOP.
We also demonstrated a statistically significant correlation between the CCT values and IOP value, with a direct proportionality between the two parameters. Nowadays, in our knowledge, some data about this are extremely heterogeneous, probably due to the various viscoelastic properties of the cornea, which may influence IOP value. Further analyses are necessary in order to be able to correctly interpret the various corneal parameters and their influence on tonometry.
References
Egbert JE, Christiansen SP, Wright MM et al (2006) The natural history of glaucoma and ocular hypertension after pediatric cataract surgery. J AAPOS 10:54–57
Chen TC, Walton DS, Bhatia LS (2004) Aphakic glaucoma after congenital cataract surgery. Arch Ophthalmol 122:1819–1825
Nakakura S, Mori E, Yamamoto M et al (2015) Intradevice and interdevice agreement between a rebound tonometer, Icare PRO, and the Tonopen XL and Kowa Hand-Held applanation tonometer when used in sitting and supine position. J Glaucoma 24:515–521
Li Y, Tang L, Xiao M, Jia S, Liu P et al (2013) Comparison of the Icare tonometer and the hand-held Goldmann applanation tonometer in pediatric aphakia. J Glaucoma 22:550–554
Borrego-Sanz L, Morales-Fernandez L, Martinez-de-la-Casa J et al (2016) The Icare PRO rebound tonometer versus the hand-held applanation tonometer in congenital glaucoma. J Glaucoma 25:149–154
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160
McGraw K, Wong SP (1996) Forming inferences about some intraclass correlation coefficients. Psychol Methods 1:30–46
Garcia-Resua C, González-Meijome JM, Gilino J et al (2006) Accuracy of the new Icare rebound tonometer vs other portable tonometers in healthy eyes. Optom Vis Sci 83:102–107
Fernandes P, Diaz-Rey JA, Queiros A et al (2005) Comparison of the ICare rebound tonometer with the Goldmann tonometer in a normal population. Ophthalmic Physiol Opt 25:436–440
Brusini P, Salvetat ML, Zeppieri M et al (2006) Comparison of ICare tonometer with Goldmann applanation tonometer in glaucoma patients. J Glaucoma 15:213–217
Gao F, Liu X, Zhao Q, Pan Y et al (2017) Comparison of the iCare rebound tonometer and the Goldmann applanation tonometer. Exp Ther Med 13(5):1912–1916
Iliev ME, Goldblum D, Katsoulis K et al (2006) Comparison of rebound tonometry with Goldmann applanation tonometry and correlation with central corneal thickness. B J Ophthalmol 90:833–835
Moreno-Montañés J, Martínez-de-la-Casa JM, Sabater AL et al (2015) Clinical evaluation of the new rebound tonometers Icare PRO and Icare ONE compared with the Goldmann tonometer. J Glaucoma 24:527–532
McMillan F, Forster RK (1975) Comparison of MacKay-Marg, Goldmann, and Perkins tonometers in abnormal corneas. Arch Ophthalmol 93:420–424
Jablonski KS, Rosentreter A, Gaki S et al (2013) Clinical use of a new position-independent rebound tonometer. J Glaucoma 22:763–767
Kniestedt C, Punjabi O, Lin S et al (2008) Tonometry through the ages. Surv Ophthalmol 53:568–591
Simon JW, O’Malley MR, Gandham SB, Ghaiy R, Zobal-Ratner J, Simmons ST (2005) Central corneal thickness and glaucoma in aphakic and pseudophakic children. J AAPOS 9:326–329
Simsek T, Mutluay AH, Elgin U, Gursel R, Batman A (2006) Glaucoma and increased central corneal thickness in aphakic and pseudophakic patients after congenital cataract surgery. Br J Ophthalmol 90:1103–1106
Faramarzi A, Javadi MA, Bonyadi MHJ, Yaseri M (2010) Changes in central corneal thickness after congenital cataract surgery. J Cataract Refract Surg 36:2041–2047
Faramarzi A, Feizi S, Maghsoodlou A (2017) Factors influencing intraocular pressure, corneal thickness and corneal biomechanics after congenital cataract surgery. Br J Ophthalmol 101(11):1493–1499
Jorge JMM, González-Méijome JM, Queirós A, Fernandes P, Parafita MA (2008) Correlations between corneal biomechanical properties measured with the ocular response analyzer and ICare rebound tonometry. J Glaucoma 17(6):442–448
Chui W, Lam A, Chen D, Chiu R (2008) The influence of corneal properties on rebound tonometry. Ophthalmology 115(1):80–84
Shin J, Lee J-W, Kim E-A, Caprioli J (2015) The effect of corneal biomechanical properties on rebound tonometer in patients with normal-tension glaucoma. Am J Ophthalmol 159(1):144–154
Brown L, Foulsham W, Pronin S, Tatham AJ (2018) The influence of corneal biomechanical properties on intraocular pressure measurements using a rebound self-tonometer. J Glaucoma 27(6):511–518
Sahin A, Basmak H, Niyaz L et al (2007) Reproducibility and tolerability of the Icare rebound tonometer in school children. J Glaucoma 16:185–188
Asrani S, Chatterjee A, Wallace DK et al (2011) Evaluation of the Icare rebound tonometer as a home intraocular pressure monitoring device. J Glaucoma 20:74–79
Lee T-E, Yoo C, Kim YY (2013) Effects of different sleeping postures on intraocular pressure and ocular perfusion pressure in healthy young subjects. Ophthalmology 120(8):1565–1570
Blumberg D, Congdon N, Jampel H et al (2007) The effects of sevofluorane and ketamine on intraocular pressure in children during examination under anaesthesia. Am J Ophthalmol 143:494–499
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Serafino, M., Villani, E., Lembo, A. et al. A comparison of Icare PRO and Perkins tonometers in anesthetized children. Int Ophthalmol 40, 19–29 (2020). https://doi.org/10.1007/s10792-019-01143-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01143-3