Abstract
Objective
To compare intraocular pressure (IOP) measurements obtained using the new transpalpebral Easyton® tonometer and Perkins applanation tonometer (PAT) in three different clinical populations.
Methods
The participants of this prospective study were 84 subjects divided into the groups: 22 healthy children (G1), 42 healthy adults (G2), and 20 adult patients with primary open angle glaucoma (G3). The data recorded in 84 eyes of these subjects were age, sex, gender, central corneal thickness (CCT), and axial length (AL). In all eyes, IOP was determined in the same examination room by the same experienced examiner using Easyton® and PAT in random order.
Results
Mean differences in IOP readings between Easyton® and PAT were 0.45 ± 1.97 (p = 0.295), − 0.15 ± 2.13 (p = 0.654), − 1.65 ± 3.22 (p = 0.033), and − 0.018 ± 2.50 mmHg (p = 0.500) in the groups G1, G2, G3, and whole sample (G4), respectively. Correlations between Easyton® and PAT IOP values were 0.668 (p = 0.001) for G1, 0.463 (p = 0.002) for G2, 0.680 (p < 0.001) for G3, and 0.605 (p < 0.001) for G4. Moderate to good agreement between the two tonometers was found in all groups according to intraclass correlation coefficients, which were 0.794 (p < 0.001) for G1, 0.632 (p < 0.001) for G2, 0.809 (p < 0.001) for G3, and 0.740 (p < 0.001) for G4. The lower and upper limits of agreement between the devices were − 5.1 and 4.7 mmHg, respectively, in the complete group. No correlation was noted between CCT or AL and the Easyton® IOP measurements.
Conclusion
IOP measurements obtained with Easyton® and PAT show an acceptable level of agreement mainly in healthy individuals, recommending it for IOP screening in children and in patients in which PAT measurement may be impared as patients with hemifacial spasms, corneal irregularities, or reduced mobility. It is not recommended for glaucoma patients follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Glaucoma is a leading cause of blindness worldwide and thus a significant public health concern [1]. While its origin is multifactorial, elevated intraocular pressure (IOP) has been identified as the main risk factor and has been also related to glaucoma progression. Accordingly, both before and after a diagnosis of glaucoma, this factor is a major therapeutic target.
There are several devices available to measure IOP. Many studies examining devices based on different principals including rebound, transpalpebral, and noncontact air pump tonometers [2], among others, have compared the reproducibility and precision of their measurements [3,4,5,6,7,8,9,10]. Besides these parameters, each device offers its own benefits for use in specific populations or situations. Transpalpebral tonometry has the main advantage that corneal contact is avoided, which might be necessary when this is not possible [11] or not advisable due to a compromised corneal surface [7, 12, 13]. Today, Goldmann applanation tonometry (GAT) is considered the gold standard so most studies have focused on confirming the clinical interchangeability of GAT with each different device [4,5,6,7,8,9,10]. The Perkins applanation tonometer (PAT) is a handheld device that offers IOP measurements that are closely comparable with GAT [14].
Previous transpalpebral tonometers have proved that the reading is not influenced by corneal thickness [15] or the presence of corneal disease or any corneal irregularity [7, 12, 13] as occurs with GAT measurements.
To the best of our knowledge, however, no study has compared IOP measurements made with this transpalpebral tonometer and PAT. The aim of the present study was therefore to compare pressure readings offered by Easyton® and PAT in three clinical settings: healthy children, and adults with and without glaucoma.
Methods
Participants
The subjects recruited for this comparative prospective study were 22 healthy children, 42 healthy adults, and 20 adults with primary open angle glaucoma (POAG). All measurements were made in the same examination room at the Hospital Clínico San Carlos, Madrid, Spain. The study protocol adhered to the principles of the Declaration of Helsinki and was approved by the clinical review board of this hospital. Informed consent was obtained from every patient, in the case of children, informed consent was obtained from their parents.
Exclusion criteria were the presence of any corneal, eyelid, or scleral pathology that could hinder measurements. Candidates were also excluded if they were noncooperative. If both eyes did not meet any of the exclusion criteria, the eye to be examined was selected randomly using a web application (www.randomization.com).
Inclusion criteria for the glaucoma group were a clinical diagnosis of POAG (open angle detected on gonioscopy, IOP over 21 mm Hg on at least 3 different days, typical changes at the optic nerve head and visual field defects consistent with POAG). The healthy adult group included subjects with an IOP of 21 mm Hg or lower, no visual field defects, no other ocular diseases, and no family history of glaucoma. These subjects were consecutively recruited among the hospital staff including nurses, relatives of patients, and persons visiting our clinic for a routine ophthalmological examination. The Children group included patients under 18 years old who came for routine ophthalmological examination with no other ocular diseases, no family history of glaucoma and who were cooperative to perform both PAT IOP and transpalpebral IOP measurement.
Clinical measures
A comprehensive ophthalmologic examination was performed in all subjects including, slit lamp biomicroscopy, fundus evaluation, central corneal thickness (CCT), axial length (AL), and IOP. Fundus examination was performed on slit lamp with 90D lens. CCT was measured by ultrasound pachymetry using double anesthetic composed of oxybuprocain and tetracaine (Dicon P55; Paradigm Medical Industries Inc., Salt Lake City, UT) and AL was measured using an optical biometer (IOL Master 700, Carl Zeiss Meditec, Jena, Germany). For each participant, data were recorded including age, gender, and the eye randomly selected for the study. For the patients with POAG, additional data compiled were their hypotensive treatment regimen (number of intraocular pressure-lowering drugs taken) and their latest visual field data square root of loss variance (sLV) and mean deviation (MD).
The same examiner performed all IOP measurements consecutively in a single session using the PAT (Perkins®; Clement-Clarke, Columbus, OH, USA) and Easyton® tonometers. Measurements of IOP with the recently introduced TVGD-02 Easyton® (Yelatma Instrument Making Enterprise, JSC, Yelatma, Russia) were made through the upper eyelid using a hydraulic system. In the examination room, the subject is instructed to tilt the head backwards and the glance line is oriented at an angle of around 45º to the horizontal. The examiner stands behind the subject and presses the instrument against the upper eyelid approximately 1 mm away from the limbus and the measurement is automatically recorded. The order of use of both devices was randomized using a web application (www.randomization.com). For the applanation tonometry, we used Fluotest Multidose composed of topical fluorescein and an anesthetic (oxybuprocain), three measurements were taken with each device and the mean of these three measures entered in the statistical analysis. All measurements were taking in the morning between 9:00am and 13:00am. In children, measurements were performed by a pediatric ophthalmology specialist, for PAT measurements Fluotest drops were used and measurements were only made in cooperative children asking them to sit on chair and resting the back of their head against the wall to make the measurement easier for the specialist.
Demographic and clinical data are provided in Table 1 for each participant group: group 1 (G1) including 22 eyes of 22 healthy children of mean age of 9.7 ± 2.5 years, group 2 (G2) including 42 eyes of 42 healthy adults of mean age of 77.6 ± 10.0 years, and group 3 (G3) including 20 eyes of 20 patients with POAG of mean age 73.3 ± 9.3 years. Data for the whole group of 84 participants (G4) are also provided.
Statistical analysis
All statistical tests were performed using SPSS software version 22.0 for Windows (SPSS Inc., Chicago, IL, USA) and MedCalc 7.3. The Kolmogorov–Smirnov test was used to check the normality of the distribution of quantitative data. Normally distributed data were compared using the Student’s t-test and Pearson’s r coefficient of correlation and non-normally distributed data with the Mann–Whitney nonparametric test and Spearman’s r coefficient. Individual groups were compared through one-way analysis of variance (ANOVA) and the Kruskal–Wallis test for normally and non-normally distributed data variables, respectively. Post-hoc Bonferroni adjustment was used to correct for the effect of multiple comparisons. To assess agreement between the two tonometers, we calculated intraclass correlation coefficients (ICC). The Bland–Altman method was used to graphically depict the level of agreement between the Easyton© and Perkins© IOP measurements. Significance was set at p < 0.05.
Results
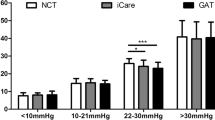
The mean IOP values obtained through applanation and transpalpebral tonometry. The mean differences between the two devices may be seen in Table 2. No significant differences were found between transpalpebral and PAT measurements in the participant groups G1, G2, and G4. Mean IOP differences were 0.45 ± 1.97 (p = 0.295) for G1, − 0.15 ± 2.13 (p = 0.654) for G2, and − 0.02 ± 2.50 (p = 0.500) for G4. In G3, PAT readings were significantly higher than those obtained with the transpalpebral tonometer with a mean difference of − 1.65 ± 3.22 (p = 0.033). Positive significant correlation was found between the PAT and Easyton® IOP measurements in all groups (G1: r = 0.668, G2: r = 0.463, G3: r = 0.680, G4: r = 0.605, all p < 0.002) (Table 3). Strongest correlation was found for G3 (r = 0.680, p < 0.001) (Table 3).
Moderate to good agreement was found between the IOP measurements made with both devices in all groups (Table 3); ICC values were always over 0.6 (mean ICC's G1 = 0.794, G2 = 0.632, G3 = 0.809, G4 = 0.740). According to the Bland–Altman plot in Fig. 1, there was agreement between the PAT and Easyton® measurements in the whole sample (n = 84). As shown, the mean difference between the tonometers was − 0.2 mm Hg (p = 0.500), and the lower and upper limits of agreement were − 5.1 and 4.7 mm Hg, respectively. In the plot, only two readings were above and another two below the limits of agreement (5.9% of the readings), whereas the rest of the readings (79/84) was within such limits. Bland–Altman plot was also calculated for each subgroup finding a lower and upper limits of agreement of -8,0 and 4,7 mm Hg, respectively, with a mean difference of 1,65 in G3. A lower and upper limits of agreement of − 4,0 and 4,3 mm Hg, respectively, with a mean difference of 0,15 in G2. A lower and upper limits of agreement of − 3,4 and 4,3 mm Hg, respectively, with a mean difference of 0,45 in G1.
Finally, we also looked for correlations between CCT or AL and the IOP readings obtained with both tonometers in all groups (Table 4). No significant correlations emerged between both measurements (CCT or AL) and Easyton® IOP in any of the four groups G1: IOP-CCT: r = − 0.23 (p = 0.913), IOP-AL: r = -0.137 (p = 0.505). G2: IOP-CCT: r = 0.342 (p = 0.059), IOP-AL: r = -0.308 (p = 0.057). G3: IOP-CCT: r = − 0.093 (p = 0.696), IOP-AL: r = -0.008 (p = 0.972). G4: IOP-CCT: r = 0.086 (p = 0.424), IOP-AL: r = − 0.081 (p = 0.456). As expected, PAT IOP measurements showed significant correlation with CCT (r = 0.314; p = 0.013).
Discussion
This study sought to assess IOP readings made with the new transpalpebral Easyton® tonometer using the Perkins applanation tonometer as reference in healthy children and adults and in adult patients with glaucoma. Our results indicate no significant differences between IOP measurements made using the two devices except in the group of glaucoma patients (− 1.65 ± 3.22, p = 0.033). In this group, Easyton® readings were usually slightly lower than those recorded using PAT.
Other authors have also reported lower transpalpebral tonometry measurements in glaucoma patients [8, 16]. Schlote and Landerberger [16] found that the transpalpebral tonometer TGDc-01"PRA" significantly underestimated IOP compared to GAT in eyes with elevated IOP. Using the same transpalpebral tonometer, Troost et al. [8] noted increasing underestimation of IOP with increasing IOP levels when compared to GAT. Our finding of this underestimation by Easyton® in our glaucoma group compared to the groups of healthy individuals is in line with previous reports make it a device only advisable for screening purposes and not glaucoma patients follow-up. Further investigation is warrented to devise a correction factor for Easyton® when used in subjects with elevated intraocular pressures.
Despite the lower Easyton® IOP values obtained in our G3 compared to PAT, agreement between the devices was moderate in all groups and ICC's were over 0.60 [17]. Although the mean values of ICC were all above 0.60, the IC 95% was wide mainly in G2 composed of healthy adults in which a bad to good agreement could be found.
To examine the clinical interchangeability of the two devices we included data for the whole population of both healthy individuals and glaucoma patients and we also made an analyses of every subgroup. The mean difference detected between the Easyton® and PAT readings was − 0.018 ± 2.5 mm Hg and lacked significance (p = 0.500). Although most of the differences detected were small, the Bland–Altman plot revealed wide 95% limits of agreement, ranging from 4.7 to 5.1 mmHg. While this suggests a moderate level of interchangeability between devices, this range of agreement was narrower than those reported in studies that have compared other transpalpebral tonometers with GAT: lower and upper limits of agreement, respectively, of + 4.4 mmHg and − 11.8 mmHg reported by Lösch et al. [9] for TGDc-01, + 8.4 mm Hg and − 9.6 mm Hg by Doherty et al. [4] for the transpalpebral tonometer Diaton®, and − 6 mmHg and + 6 mmHg by Sandner et al. [18] also for TGDc-01, the latter being closer to our results. The best results were found in the healthy children group with a lower and upper limit of agreement, respectively, -3,4 and 4,3 mm Hg and the worst results were found in the glaucoma group with a lower and upper limit of agreement, respectively, − 8,0 and 4,7 mm, respectively. These results showed an improvement in transpalpebral measurements compared with previous devices, as IOP is lower in children, it can be the reason why the best agreement has been found in this group apart from an improvement of the measuring system. Easyton may be only advisable in patients in which measurements are difficult or children in which IOP values are lower and it seems to be accurate enough.
Finally, we also examined correlations between IOP values obtained with both devices and CCT or AL as older models of transpalpebral tonometers are affected by corneal thickness, especially in subjects with thin corneas [19]. Here, no correlation was detected between CCT or AL and IOP measurements in any of our study groups. This independence from CCT is useful as it is one of the main limitations of GAT [20]. This means that an eye's AL and CCT are not confounding factors for Easyton® IOP measurements.
As limitations of our study, we should mention that IOP readings were taken consecutively with no pauses and we did not examine lid biomechanics, corneal biomechanics, or the impacts of lid thickness on measurements. Further, a subgroup analysis of different IOP ranges was not performed.
In conclusion, our findings indicate an acceptable level of agreement between the transpalpebral tonometer Easyton© and the Perkin's applanation tonometer in healthy individuals, recommending it for IOP screening in children and in patients in which PAT measurement may be impaired as patients with hemifacial spasms, corneal irregularities, or reduced mobility. The transpalpebral device, however, tended to underestimate IOP in the glaucoma patients which make it a not recommended device for glaucoma patients follow-up. The readings obtained with this new tonometer were also highly independent from corneal thickness. As this device avoids direct contact with the eye, there is no need for topical fluorescein and it can be easily used in subjects with corneal infection or corneal irregularities, noncooperative subjects, or those with reduced mobility [3,4,5,6,7,8,9]. If our findings are confirmed in further work, these benefits make this transpalpebral tonometer especially useful for IOP screening and for use in children and individuals with corneal disease.
References
Weinreb RN, Aung T, Medeiros FA (2014) The pathophysiology and treatment of glaucoma: a review. JAMA 311:1901–1911. https://doi.org/10.1001/jama.2014.3192
Brusini P, Salvetat ML, Zeppieri M (2021) How to measure intraocular pressure: an updated review of various tonometers. J Clin Med. https://doi.org/10.3390/jcm10173860
Gao F, Liu X, Zhao Q, Pan Y (2017) Comparison of the iCare rebound tonometer and the Goldmann applanation tonometer. Exp Ther Med 13:1912–1916. https://doi.org/10.3892/etm.2017.4164
Doherty MD, Carrim ZI, O’Neill DP (2012) Diaton tonometry: an assessment of validity and preference against Goldmann tonometry. Clin Exp Ophthalmol 40(4):e171–e175. https://doi.org/10.1111/j.1442-9071.2011.02636.x
Li Y, Shi J, Duan X, Fan F (2010) Transpalpebral measurement of intraocular pressure using the Diaton tonometer versus standard Goldmann applanation tonometry. Graefes Arch Clin Exp Ophthalmol 248:1765–1770. https://doi.org/10.1007/s00417-009-1243-y
Waisbourd M, Shemesh G, Top LB et al (2010) Comparison of the transpalpebral tonometer TGDc-01 with Goldmann applanation tonometry. Eur J Ophthalmol 20:902–906. https://doi.org/10.1177/112067211002000514
Shemesh G, Waisbourd M, Varssano D et al (2009) Measurements of intraocular pressure by Goldmann tonometry, Tonopen XL, and the transpalpebral tonometer, TGDc-01, after penetrating keratoplasty: a comparativye study. Cornea 28:724–727. https://doi.org/10.1097/ICO.0b013e3181930be8
Troost A, Specht K, Krummenauer F et al (2005) Deviations between transpalpebral tonometry using TGDc-01 and Goldmann applanation tonometry depending on the IOP level. Graefes Arch Clin Exp Ophthalmol 243:853–858. https://doi.org/10.1007/s00417-005-1142-9
Lösch A, Scheuerle A, Rupp V et al (2005) Transpalpebral measurement of intraocular pressure using the TGDc-01 tonometer versus standard Goldmann applanation tonometry. Graefes Arch Clin Exp Ophthalmol 243:313–316. https://doi.org/10.1007/s00417-004-0971-2
Fogt JS, Nau CB, Schornack M et al (2020) Comparison of pneumatonometry and transpalpebral tonometry measurements of intraocular pressure during scleral lens wear. Optom Vis Sci 97:711–719. https://doi.org/10.1097/OPX.0000000000001574
Müller A, Godenschweger L, Lang GE, Kampmeier J (2004) Prospective comparison of the new indentation tonometer TGdC-01, the non-contact tonometer PT100 and the conventional Goldmann applanation tonometer. Klin Monbl Augenheilkd 221:762–768. https://doi.org/10.1055/s-2004-813566
Risma JM, Tehrani S, Wang K et al (2016) The utility of diaton tonometer measurements in patients with ocular hypertension, glaucoma, and glaucoma tube shunts: a preliminary study for its potential use in keratoprosthesis patients. J Glaucoma 25:643–647. https://doi.org/10.1097/IJG.0000000000000394
Arora R, Bellamy H, Austin M (2014) Applanation tonometry: a comparison of the Perkins handheld and Goldmann slit lamp-mounted methods. Clin Ophthalmol 8:605–610. https://doi.org/10.2147/OPTH.S53544
Wisse RP, Peeters N, Imhof SM, van der Lelij A (2016) Comparison of Diaton transpalpebral tonometer with applanation tonometry in keratoconus. Int J Ophthalmol 9:395–398. https://doi.org/10.18240/ijo.2016.03.12
Cacho I, Sanchez-Naves J, Batres L et al (2015) Comparison of intraocular pressure before and after laser in situ keratomileusis refractive surgery measured with perkins tonometry, noncontact tonometry, and transpalpebral tonometry. J Ophthalmol 2015:683895. https://doi.org/10.1155/2015/683895
Schlote T, Landenberger H (2005) Intraocular pressure difference in Goldmann applanation tonometry versus a transpalpebral tonometer TGDc-01"PRA" in glaucoma patients. Klin Monbl Augenheilkd 222:123–131. https://doi.org/10.1055/s-2005-857881
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Sandner D, Böhm A, Kostov S, Pillunat L (2005) Measurement of the intraocular pressure with the “transpalpebral tonometer” TGDc-01 in comparison with applanation tonometry. Graefes Arch Clin Exp Ophthalmol 243:563–569. https://doi.org/10.1007/s00417-004-1037-1
Toker MI, Vural A, Erdogan H et al (2008) Central corneal thickness and Diaton transpalpebral tonometry. Graefes Arch Clin Exp Ophthalmol 246:881–889. https://doi.org/10.1007/s00417-008-0769-8
Ehlers N, Bramsen T, Sperling S (1975) Applanation tonometry and central corneal thickness. Acta Ophthalmol 53:34–43. https://doi.org/10.1111/j.1755-3768.1975.tb01135.x
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Elena Montolío-Marzo, Laura Morales-Fernández and Jose María Martínez-de-la-Casa. The first draft of the manuscript was written by Elena Montolío-Marzo and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Montolío-Marzo, E., Morales-Fernández, L., Saenz-Frances San Baldomero, F. et al. Easyton® transpalpebral versus Perkins applanation tonometry in different populations. Int Ophthalmol 43, 3491–3497 (2023). https://doi.org/10.1007/s10792-023-02754-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02754-7