Abstract
Background
Many injuries cause pain and inflammation, which are one of the major challenges for physicians. In this study, the analgesic and the anti-inflammatory effects of milnacipran were investigated on carrageenan-induced nociception and inflammation in male rats.
Methods
Pain and inflammation were induced by injection of λ-carrageenan (1% v/v) into the hind paw. Indomethacin (10 mg/kg: ip) or milnacipran (10, 20 and 40 mg/kg: ip) were administered 30 min before carrageenan. Analgesia and inflammation were measured by hot plate and plethysmometer. Finally, lipid peroxidation, tumor necrosis factor alpha (TNF-α), Interleukin 1 beta (IL-1β), Interleukin 6 (IL-6), myeloperoxidase (MPO) activity, nitric oxide (NO) and total antioxidant capacity (TAC) status evaluated in the hind paw tissue.
Results
The results showed that carrageenan caused hyperalgesia and inflammation in the hind paw tissue. Milnacipran (20 and 40 mg/kg) significantly and dose-dependently attenuated (65 ± 3.2%; p ≤0.01 and 42 ± 6.2%; p ≤ 0.001, respectively) carrageenan-induced inflammation and significantly increased (p ≤ 0.001) nociception threshold. Also, milnacipran (20 and 40 mg/kg) significantly suppressed levels of malondialdehyde (MDA), NO (p ≤ 0.05), MPO activity, TNF-α, IL-1β and IL-6 (p ≤ 0.001) following carrageenan injection. Additionally, milnacipran (10, 20 and 40 mg/kg) significantly augmented (p ≤ 0.05) TAC status following carrageenan in the hind paw tissue.
Conclusion
In the present study, milnacipran showed anti-nociceptive and anti-inflammatory effects on carrageenan-induced hyperalgesia and inflammation in a dose-dependent manner. Milnacipran reduced inflammatory edema and increased the paw withdrawal threshold probably through suppression of MDA, NO, TNF-α, IL-1β, IL-6 and MPO activity, and increase of TAC status in the hind paw tissue. Therefore, milnacipran holds important potential as an anti-inflammatory and anti-nociceptive drug. Although, further clinical trials to confirm this issue, is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain is an unpleasant sensory experience created following the tissue damage that is resulting from chemical, thermal, mechanical and electrical stimuli and it is either acute or chronic (Luedde and Schwabe 2011).
Inflammation is one of the factors giving rise to pain which is known to cause an increase in the sensitivity of the terminal nerves via prostaglandins hence causing the feeling of pain. Inflammation is a general mechanism for many diseases. Notwithstanding the value of managing of inflammation, common anti-inflammatory medicines, non-steroid anti-inflammatory drugs (NSAIDs), which work via suppression of the cyclooxygenase (COX-1 and COX-2) isozymes have various biological effects; first, analgesic activity is due to COX-2 prevention. They have several side effects especially cardiovascular and gastrointestinal adverse effects caused by COX-1 and COX-2 inhibition, which restrict their clinical application (Taler et al. 2007). Hence, the development of new anti-inflammatory substances is still necessary. On the inflammation pathway, the created free radicals cause an increase in the production of inflammatory cytokines like IL-6, TNF-α and prostaglandins (PGs) that not only increase the inflammation rate but also cause an increase in the sensitivity of the axonal terminals to pain and create inflammatory pains (Bavill 1997; Surh et al. 2001). Reactive oxygen species (ROSs) and reactive nitrogen species (RNSs) are free radicals that are produced during many of the body’s reactions. If the radicals overcome the antioxidants in the body, it leads to oxidative stress (Hosseini and Abdollahi 2013). Inflammatory intermediaries such as IL-1 and IL-6 and ROS cause an increase in the sensitivity and activation of pain neurons. Such an increase in the sensitivity to pain mostly occurs in the nerve cells in the vicinity of the wound area and leads to an increase in the topical pain (Sayyah et al. 2002).
Pain and inflammation, either acute or chronic influence the patient’s quality of life. Due to the same reason, relieving of the pain and inflammation and elevating the patient’s quality of life are amongst the priorities of treating the patients. To relieve the pain NSAIDs are used as the first line of treatment. Moreover, opioid drugs are used as the second line to decline pain. These two groups of medications have many side effects including: gastrointestinal, cardiovascular, renal, and hepatic adverse effects for NSAIDs linked to their corresponding inhibitory effect for COX-1 and COX-2 (Brune and Patrignani 2015) and respiratory depression, nausea, vomiting, constipation, tolerance, dependence, pruritus, urinary retention, sedation and withdrawal effects for opioids (Schug et al. 1992). Thus, specialists are looking for an alternative drug for reducing inflammation and relieving pain (Bavill 1997).
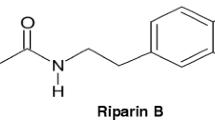
Antidepressants constitute a set of drugs that are known to have analgesic effects. Researchers have paid a great deal of attention to milnacipran, an antidepressant inhibiting the reabsorption of serotonin and noradrenaline, amongst the other antidepressants (Dharmshaktu et al. 2012). In the previous studies, regarding acute or chronic pain, milnacipran has exhibited analgesic effects in patients with fibromyalgia (Derry et al. 2012). Recently, it has been reported that inflammation and inflammatory pathways are participating in the pathophysiology of fibromyalgia (Kadetoff et al. 2012; Littlejohn and Guymer 2018; Rodriguez-Pintó et al. 2014). It has also been proved that it is effective in reducing the pains resulting from intestinal inflammation and neuropathic pains (Berrocoso et al. 2011).
According to the prevalence of pain and importance of pain relieving for patients and considering the position of milnacipran in reducing pain and also knowing the scarcity of research on the anti-inflammatory effects of milnacipran, the present study aimed to investigate the anti-inflammatory and analgesic effects of milnacipran in the carrageenan intraplantarly injected male Wistar rats.
Materials and method
Animals
Male Wistar rats, weighing 170–220 g, have been used in this study. The rats were kept in the animal’s room a few days before starting the tests. Six rats were housed per cage in a controlled room at a temperature of 24 ± 2 ºC and humidity of 50–60%. They maintained on a 12-h light–dark cycle. Food and water were constantly available to them (Kheradmand et al. 2016a). All procedures used in the present study were done in accordance with the National Institutes of Health ethical guidelines for the Care and Use of Laboratory Animals and approved by the University of Medical Sciences of Hamadan (UMSHA) Ethical Committee, Hamadan, Iran (ID: IR.UMSHA.REC.1396.363).
Drugs
Milnacipran and λ-carrageenan were obtained from Sigma Chemical Co. (USA), and they were prepared in sterile normal saline. Indomethacin was purchased from Sigma Chemical Co. (USA), it was solved in DMSO solvent (5%). Milnacipran and indomethacin were administered intraperitoneally, and carrageenan injected intraplantarilly.
Experiment design
Animals (n = 42) randomly divided into eight groups (6 rats): 1. Control group (normal saline), 2. Carrageenan (100 µl 1% v/v in normal saline), 3. Carrageenan + indomethacin (10 mg/kg in DMSO), 4, 5 and 6. Carrageenan + milnacipran (10, 20 and 40 mg/kg, ip), 7. Sham group (normal saline containing 5% DMSO injected ip). Milnacipran in the dose (10, 20 or 40 mg/kg, ip) or indomethacin in a dose (10 mg/kg, ip) were injected 30 min before intraplantar administration of carrageenan.
Carrageenan-induced rat paw edema
Inflammation was induced by λ-carrageenan 1%. Carrageenan was dissolved in saline (1% v/v) and was injected (100 µl/rat) into the plantar surface of the right hind paw (Sharma et al. 2020). Plethysmometer (Tajhiz Gostar Iranian, Iran) was used to quantify hind paw edema before and 1, 2 and 3 h after carrageenan injection. The inhibition percentage of inflammation was measured for each group with respect to its vehicle group. The anti-inflammatory percent was calculated by a formula as below:
anti-inflammatory percent = (Vt – V0)/V0 × 100.
Vt = the volume (ml) of the right hind paw after injection of carrageenan in the different times, V0 = the volume (ml) of the right hind paw immediately before carrageenan injection.
Pain assessment
Carrageenan intraplantar administration resulted in acute thermal hyperalgesia (Sammons et al. 2000). The rats were placed on a hot plate surface (55 ± 0.5 ºC) and the latency time of the animals to reflex to the hot stimuli was recorded when animals start jumping or licking the hind paw. The light beam power was set to create a base latency time of 3 s. To prevent tissue damage, 9 s were considered as the cut off time of the test. Hot plate was done immediately before injections and then 30, 60 and 90 min after carrageenan injection.
Analgesia was quantified as percentage of maximum possible effect (MPE%), to equalize the bases latency time in different animals, according to the following formula (Yaksh 1981):
where MPE = maximum possible effect, TL = test latency time, BL = base latency time (i.e., initial (0th) hot plate latency time), CT = cut off time.
Sampling
The rats were euthanized and then paw samples were isolated after removing of the skin and stored in a freezer at −80 ºC for next tests.
Myeloperoxidase activity assay
MPO activity is a marker of inflammation in the tissue. The MPO activity was assessed as reported previously (Haddadi et al. 2018b). Briefly, to measure the amount of this enzyme, tissue samples were homogenized in a solution containing 0.5% hexa-decyl-trimethyl-ammonium for 1 min. After three freeze-defreeze, they were placed in a sonication device (Bandelin DT510H, USA) for 5 min. They were centrifuged for 30 min with about 10,000 rpm. 100 μl of supernatant with 2.9 ml of solution containing O-dianisidine, Buffer phosphate (pH 6) and H2O2 were mixed and after 5 min, 100 ml of chlorhydric acid solution (1.2 M) was added. At the end, samples absorbance was read spectrophotometrically at a 400 nm wavelength.
Interleukin (IL)-1β, IL-6 and tumor necrosis factor (TNF)-α assessment
The hind paw tissue levels of IL-1β, IL-6 and TNF-α were measured using the ELISA kits (Rat IL-1β, IL-6 and TNF-α, Biolegend, California, USA) based on the manufacture's guideline. Conditions were equal for all tests. In summary, the frozen hind paw tissue samples were homogenated in RIPA buffer, as reported before (Haddadi et al. 2018a). After centrifugation, the supernatants were incubated in the wells and after washing, diluted streptavidin-HRP-conjugated anti-rat IL-1β, IL-6 or TNF-α were added. Finally, after adding of stop solution, the absorbance was read at 450 nm using an ELISA reader. The concentration of the cytokines was expressed as pg/ml of tissue homogenate.
Lipid peroxidation assessment
The level of peroxidation of lipid was evaluated as reported previously, via MDA measurement (Kheradmand et al. 2016b). Measurement of MDA is a standard method for detecting the amount of lipid peroxidation in tissue samples. Malondialdehyde produces a pink product due to the production of thiobarbituric reactive substances at boiling temperature, which can be accurately measured at a nanoscale by colorimetric method at 532 nm.
Nitric oxide assay
Nitric oxide (NO) swiftly oxidized to nitrite and nitrate subsequent to its creation. The level of total NO was evaluated via nitrite and nitrate measurement according to the Griess reaction, as reported previously (Haddadi et al. 2018b). In this colorimetric method, the final product absorbance can be determined at a wavelength of 540 nm in a microplate reader.
Total antioxidant capacity (TAC) assay
The level of TAC was determined in the hind paw tissue homogenate according to ferric reduction antioxidant power (FRAP) method, as reported before (Haddadi et al. 2018b). In summary, at low pH, which was determined by the use of acetate buffer (pH = 3.6), the reduction of Fe-3–TPTZ complex creates a drastic blue color that can be calculated at 593 nm.
Data analysis
The data were analyzed by SPSS software using one-way or two-way ANOVA and Tukey post-test as appropriate and the results were reported as mean ± SEM. A value of p ≤ 0.05 was regarded as significant. The graphs were prepared using Graph Pad Prism software (version 6, Graph Pad software Inc., San Diego, CA, USA).
Results
For each groups of experiment, we had six male Wistar rats. Mean age and body weight in each group were not statistically significant (p = 0.48 and 0.73, respectively). The results of the sham group showed no significant difference with the control group in behavioral and biochemical assessments (results not shown in graphs).
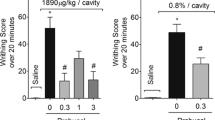
Milnacipran and indomethacin attenuated carrageenan-induced hyperalgesia
The results indicated that intraplantar injection of carrageenan significantly (p < 0.001) reduced paw withdrawal latency in comparison with the control group in all trials, which is an indicator of carrageenan-induced hyperalgesia. The highest decrease in paw withdrawal latency occurred 90 min after carrageenan injection. Injection of indomethacin (10 mg/kg: ip), 30 min before carrageenan, significantly (p ≤ 0.001) increased the paw withdrawal latency when compared with carrageenan group. Intra-peritoneal injection of milnacipran (20 and 40 mg/kg), half an hour before carrageenan injection, caused a significant increase in the paw withdrawal latency (p ≤ 0.001) versus carrageenan group. The analgesic effect of milnacipran (20 and 40 mg/kg) in the time 90 min after carrageenan injection was significantly (p ≤ 0.01) higher than indomethacin. It should be stated that, milnacipran in the dose of 10 mg/kg (ip) have had no significant analgesic effect on carrageenan-induced hyperalgesia (Fig. 1).
The effect of intra-peritoneal injection of indomethacin (10 mg/kg) and milnacipran (10, 20 and 40 mg/kg) on the paw withdrawal latency within 0–90 min after intraplantar injection of carrageenan. (Data shown as mean ± SEM of MPE%) (two-way ANOVA with repeated measurement followed by Tukey’s post hoc test, n = 6). ###p ≤ 0.001 vs carrageenan group. ***p ≤ 0.001, versus the control group. &&p ≤ 0.01 vs carrageenan + indomethacin group
Milnacipran attenuated carrageenan-induced inflammation and paw edema
As demonstrated in Fig. 2a, carrageenan significantly increased the volume of the paw edema 60 (p ≤ 0.05), 120 (p ≤ 0.001) and 180 (p ≤ 0.001) min after injection when compared with the control group in the same times (Fig. 2a).
The effect of intra-peritoneal injection of milnacipran (10, 20 and 40 mg/kg) and indomethacin (10 mg/kg) on a the edema volumes of paws and on b the inflammation percentage of the paw resulting from the intraplantar injection of carrageenan solution (1%) within 0–180 min after carrageenan injection. Data presented as a ΔV (n = 6 rats, two-way ANOVA with repeated measurement followed by Tukey’s post hoc test) and b inflammation percentage (n = 6 rats, one-way ANOVA with repeated measurement followed by Tukey’s post hoc test). *p < 0.05, ***p < 0.001 versus the control group; ##p ≤ 0.01, ###p ≤ 0.001 vs carrageenan group; &p ≤ 0.05, &&&p ≤ 0.001 vs milnacipran (20 mg/kg) + carrageenan group; +p ≤ 0.05, ++p ≤ 0.01 vs milnacipran (20 mg/kg) + carrageenan group
According to Fig. 2b, intraplantar injection of carrageenan into the right hind paw significantly increased (p < 0.001) inflammation percentage compared with the control group.
Milnacipran (40 mg/kg: ip) decreased the volume of the paw 60 and 180 min after carrageenan injection in a significant manner (p ≤ 0.01 and p ≤ 0.001, respectively). Also, milnacipran (20 mg/kg: ip) significantly decreased (p ≤ 0.001) the volume of the paw 180 min after carrageenan injection when compared with the carrageenan group, but milnacipran (10 mg/kg: ip) have had no significant effect on paw volume when compared with the control group. On the other hand, indomethacin (10 mg/kg) significantly prevented (p ≤ 0.001) the increase of the paw volume 120 and 180 min after carrageenan injection when compared with carrageenan group. As shown in Fig. 2a, indomethacin significantly decreased paw edema volume more than milnacipran (20 mg/kg: ip) 120 (p ≤ 0.05) and 180 (p ≤ 0.01) after carrageenan injection (Fig. 2a).
Injection of milnacipran (20 and 40 mg/kg: ip) before carrageenan significantly and dose-dependently prevented (65 ± 3.2%; p ≤ 0.01 and 42 ± 6.2%; p ≤ 0.001, respectively) from increase of inflammation induced by carrageenan. Also, injection of indomethacin (10 mg/kg: ip) 30 min before carrageenan-reduced inflammation (16.5 ± 3.1%) in right hind paw at a significance level (p ≤ 0.001) compared to carrageenan group. The results showed that the effect of indomethacin injection on carrageenan-induced inflammation was more than milnacipran injection at a significance level (p ≤ 0.001) (Fig. 2b).
Effects of carrageenan and milnacipran on the myeloperoxidase activity in the paw tissue
Myeloperoxidase activity was evaluated as the primary indicator of the inflammatory responses. The results were indicated that intraplantar injection of carrageenan significantly increased (71.6 ± 6.3; p ≤ 0.001) myeloperoxidase activity in the paw tissue when compared with control group (25 ± 2.4). Intra-peritoneal injection of indomethacin (10 mg/kg) significantly decreased (27.8 ± 2.5; p ≤ 0.001) carrageenan-induced myeloperoxidase activity in the paw tissue. Also, milnacipran (20 and 40 mg/kg) 30 min before intraplantar injection of carrageenan prevented from the increase of enzymatic activity of myeloperoxidase (38.6 ± 1.8 and 30.6 ± 1.2, respectively) at a significance level (p ≤ 0.001) compared with carrageenan group (Fig. 3a).
The effect of intra-peritoneal injection of indomethacin (10 mg/kg), milnacipran (10, 20 and 40 mg/kg) and intraplantar administration of carrageenan on the a enzymatic activity of myeloperoxidase, b TNF-α, c IL-6 and d IL-1β in the paw tissue 3 h after carrageenan injection (data showed as mean ± SEM, one-way ANOVA followed by Tukey’s post hoc test, n = 6 rats per group). ***p ≤ 0.001 vs the control group. ###p ≤ 0.001 vs carrageenan group
Effects of carrageenan and milnacipran on the paw tissue level of pro-inflammatory cytokines
To confirm the role of inflammation, the level of TNF-α, IL-6 and IL-1β as the pro-inflammatory cytokines were assessed in the hind paw tissue. First, as presented in Fig. 3b, intraplantar injection of carrageenan increased the level of TNF-α (812.6 ± 35) in a significant manner (p ≤ 0.001) when compared with control group (165.3 ± 12.1). As anticipated, indomethacin injection (10 mg/kg, ip) significantly diminished (p ≤ 0.001) the level of TNF-α in the hind paw tissue following to carrageenan injection. Also, administration of milnacipran (20 and 40 mg/kg, ip) 30 min prior to carrageenan impeded from elevation of TNF-α level in the hind paw tissue (559.6 ± 18.2 and 365.7 ± 15.6, respectively) in a considerable amount (p ≤ 0.001) (Fig. 3b).
Second, carrageenan injection meaningfully increased the level of IL-6 (1426.8 ± 83; p ≤ 0.001) when compared with control group (422 ± 35.1) (Fig. 3c). Indomethacin injection (10 mg/kg, ip) significantly attenuated the level of IL-6 (523 ± 25.2; p ≤ 0.001) in the hind paw tissue versus carrageenan group. On the other hand, milnacipran injection (20 and 40 mg/kg, ip) half an hour before carrageenan prevented from augmentation of IL-6 level in the hind paw tissue (825.3 ± 39.2 and 597.1 ± 61.2, respectively) in a meaningful level (p ≤ 0.001) (Fig. 3c).
Finally, as demonstrated in Fig. 3d, carrageenan intraplantar injection significantly increased (p ≤ 0.001) the level of IL-1β when compared with the control group. Indomethacin administration (10 mg/kg, ip), as well as milnacipran (20 and 40 mg/kg, ip) injection, 30 min before carrageenan meaningfully reduced (p ≤ 0.001) level of IL-1β in the hind paw tissue compared with carrageenan group (Fig. 3d).
Effects of carrageenan and milnacipran on the lipid peroxidation in the paw tissue
To evaluate the participation of lipid peroxidation as a marker of oxidative stress in the inflammation induced by carrageenan, the concentration of malondialdehyde was measured in all groups. The results indicated that intraplantar injection of carrageenan increased malondialdehyde (12.6 ± 1.1) in significant level (p ≤ 0.01) in comparison with the control group (6.3 ± 0.6). Intra-peritoneal injection of indomethacin significantly prevented the MDA elevation by carrageenan in the hind paw tissue (8.5 ± 1.2; p ≤ 0.05). On the other hand, milnacipran (10, 20 and 40 mg/kg: ip) 30 min before intraplantar injection of carrageenan-reduced malondialdehyde amount at a significance level (9.4 ± 1.3; p ≤ 0.05, 7.2 ± 1.5; p ≤ 0.05 and 6 ± 0.7; p ≤ 0.01, respectively) in comparison with the carrageenan group (Fig. 4a).
The effect of intra-peritoneal injection of indomethacin (10 mg/kg), milnacipran (10, 20 and 40 mg/kg) and intraplantar injection of carrageenan alone on the level of a lipid peroxidation, b nitric oxide (NO) and c TAC status in the paw tissue 3 h after carrageenan injection. Data are shown as mean ± SEM (one-way ANOVA followed by Tukey’s post hoc test, n = 6 rats). **p ≤ 0.01, ***p ≤ 0.001 vs the control group. #p ≤ 0.05, ##p ≤ 0.01 and ###p ≤ 0.001 vs carrageenan group
Effects of carrageenan and milnacipran on the paw tissue level of nitric oxide
The impacts of milnacipran administration (10, 20, and 40 mg/kg; ip) on the NO concentration, as a hallmark of nitosative stress, in the hind paw tissue of rats administrated with carrageenan (10 mg/kg), are demonstrated in Fig. 4b. It was observed that the concentration of NO was meaningfully augmented in the carrageenan group (168.3 ± 12; p ≤ 0.001) versus the control group (53 ± 4.3). Augmentation of NO degree subsequent to carrageenan injection in the paw tissue was suppressed by milnacipran injection (20 and 40 mg/kg, ip) in a considerable amount (72.9 ± 9.2; p ≤ 0.001 and 54.1 ± 7.2; p ≤ 0.001, respectively). Also, it was found that indomethacin (10 mg/kg; ip) significantly decreased the level of NO (67.1 ± 8; p ≤ 0.001) in the hind paw tissue in comparison with carrageenan group (Fig. 4b).
Effects of carrageenan and milnacipran on the paw tissue level of TAC
To determine the alteration in antioxidant level of hind paw tissue of rats in this study, TAC assay was carried out. The influence of milnacipran administration (10, 20, and 40 mg/kg; ip) on TAC status in the paw tissue of rats injected with carrageenan, is indicated in Fig. 4c. The results show that intraplantar injection of carrageenan meaningfully (p ≤ 0.001) attenuated the status of total antioxidant capacity. Downgrading of TAC status was impeded by ip injection of milnacipran (10, 20, and 40 mg/kg) in a significant amount (p ≤ 0.05, p ≤ 0.01, p ≤ 0.001, respectively), versus carrageenan group. Also, we found that indomethacin (10 mg/kg; ip) increased TAC level in a significant manner (p ≤ 0.05) in the hind paw tissue in comparison with carrageenan group (Fig. 4c).
Discussion
In the current study, the effect of milnacipran on the nociception threshold and inflammation had been investigated following carrageenan intraplantar administration in male rats. The results of the current study demonstrated that milnacipran considerably declined the pain and inflammation induced by carrageenan. Also, in this study, we revealed the analgesic impacts of milnacipran, displaying that its mechanism of action aims peripheral IL-1β, IL-6, TNF-α, oxidative stress and MPO activation.
Carrageenan has been applied to produce different kinds of paw edema, inflammation, and acute algesia in many animal investigations. Carrageenan creates hypersensitivity to thermal stimuli. The hyperalgesia induced by carrageenan injection is an appropriate pathway for investigating the peripheral and central mechanism of sensory pain (Bach-Rojecky and Lackovic 2005; Tsuruoka et al. 2003). Also, this model has broadly been utilized as a proper model for investigating the effectiveness of potential candidates of analgesic and/or anti-inflammatory drugs (Bach-Rojecky and Lackovic 2005; Hwang et al. 2008). The results of the present study indicated that the intraplantar injection of carrageenan caused a significant decrease in the paw withdrawal latency time on the hot plate which proves hyperalgesia induction. These results were consistent with the findings of the prior reports that had reported carrageenan-induced hyperalgesia (Bach-Rojecky and Lackovic 2005; Khattab 2006). The carrageenan-induced hyperalgesia in the present study was evaluated by the hot plate test as reported previously (Bach-Rojecky and Lackovic 2005; Ruiz-Miyazawa et al. 2015), which the results of the current study are found in line with their findings.
In recent studies, antidepressant drugs have been considered as the analgesic and anti-inflammatory agent. For example, some studies reported that duloxetine and milnacipran have similar effects on the treatment of fibromyalgia (Dharmshaktu et al. 2012). Milnacipran is a reuptake inhibitor of serotonin and noradrenalin. In the present study, milnacipran in the doses of 20 and 40 mg/kg significantly increased the paw withdrawal latency time on the hot plate. Whereas, in another study, the chronic use of milnacipran had exerted no effect on muscular stress induced pain-like behaviors in a preclinical study in the rats (Suarez-Roca et al. 2006). In accordance with the results of the current study, Berrescoso et al. reported that milnacipran has positive effects on the CCI model of sciatic nerve induced neuropathic pain (Berrocoso et al. 2011). Also, based on the study by King et al. (2006), the acute intra-peritoneal injection of milnacipran reduced the sensitivity to radiative heat.
In the present study, carrageenan was found to increase the edema and inflammation of the hind paw and this was also in compliance with the results of the previous researches (Khattab 2006). On the other hand, in the present study, the intra-peritoneal injection of milnacipran in the doses of 20 and 40 mg/kg and/or indomethacin significantly prevented the inflammatory edema induced by intraplantar injection of carrageenan. In agreement with the current study, it has been reported that indomethacin significantly reduced the inflammation following intraplantar injection of carrageenan (Buritova et al. 1995). Additionally, in the another study, which investigated the effect of milnacipran and indomethacin on polyarthritis rats, indomethacin was found effective against both stress levels but milnacipran was found effective only in low pressure level (Mico et al. 2011), which this is totally in accordance to the results of the current research.
Another important finding of the present study was that milnacipran prevented MPO activity induced by carrageenan in the hind paw tissue, which is an indirect assessment of the number of macrophages and the number of neutrophils. Many studies have shown that the release of MPO from leukocytes in the injured area leads to the activation of neutrophils and monocytes, that extraction of neutrophils and secretion of more prostaglandins produce carrageenan inflammation. It has been reported that carrageenan-induced edema is a biphasic phenomenon. During this process, MPO activity and level of neutrophil activity significantly increased within 0–4 h after induction of inflammation by carrageenan that is in accordance with the findings of the current study (Bach-Rojecky and Lackovic 2005; Fröde and Medeiros 2001). Varghese et al. (2006) reported that desipramine (a tricyclic antidepressant) could decrease the level of MPO activity in a significant manner. It can be postulated that the anti-inflammatory effect of milnacipran in the current study may be exerted through its neutrophil recruitment reduction, as appraised by MPO activity suppression.
To confirm the role of inflammation in the anti-inflammatory and analgesic effects of milnacipran, the level of TNF-α, IL-6 and IL-1β were assessed in the hind paw tissue. Subsequent to tissue damage, inflammatory responses augmented pain feeling. The peripheral sensitization is initiated by IL-1β and TNF-α as pro-inflammatory cytokines, as well as reactive oxygen species and free radicals. Extra to their participation in the inflammation onset, these cytokines straightly activate their receptors and nociceptors terminals to decrease the threshold of pain, causing hyperalgesia and inflammatory pain (Kadetoff et al. 2012; Stejskal et al. 2013). The results of the current study revealed that the level of this pro-inflammatory cytokines after injection of carrageenan significantly increased in paw tissue. This totally agrees with the previous reports. For example, the increase in the TNF-α and IL-1β levels have been previously reported in paw tissue following carrageenan-induced inflammation (Mizokami et al. 2016; Ruiz-Miyazawa et al. 2015). Pretreatment with milnacipran in the doses of 20 and 40 mg/kg impeded the elevation of TNF-α, IL-6 and IL-1β in hind paw tissue which injected with carrageenan. Similar effects have been previously reported from some of serotonin and noradrenalin reuptake inhibitor antidepressant drugs such as amitriptyline (Handy and Moore 1998; Menendez et al. 2002). The precise mechanism by which antidepressants exert their anti-inflammatory activity remains to be clarified. The analgesic and anti-inflammatory effects of NSAIDs are mediated by prevention of prostaglandins (PGs) production via suppression of COX-1 and COX-2 (Rao and Knaus 2008). Pro-inflammatory cytokines increased COX activity and subsequently PGs release (Neeb et al. 2011; Yang et al. 2008). It is plausible that milnacipran may decrease pain and inflammation through inhibition of COX isoenzymes. In this regard, it has been demonstrated that amitriptyline decreased the activity of COX-2 in macrophages (Rafiee et al. 2017). Also, in another study, it has been shown that selective serotonin reuptake inhibitors attenuated COX-2 expression in human T lymphocytes (Taler et al. 2007). Many reports also have indicated that antidepressants hinder the PGs production (Tynan et al. 2012; Yaron et al. 1999). In the present study, milnacipran analgesic and anti-inflammatory effects were at least in part exerted through its suppression of MPO activity and inflammatory mediators, such as IL-1β, IL-6 and TNF-α. Carrageenan triggers neutrophil recruitment and MPO activity, and activates the cytokines production, including IL-1β, IL-6 and TNF-α, which are accountable for inflammation and pain (Littlejohn and Guymer 2018; Rodriguez-Pintó et al. 2014; Ruiz-Miyazawa et al. 2015). Suppression of MPO activity, IL-1β, IL-6 and TNF-α abolish carrageenan-induced hyperalgesia (Littlejohn and Guymer 2018; Mizokami et al. 2016). Hence, we suppose that suppression of MPO activity, reducing IL-1β, IL-6 and TNF-α secretion, are crucial determinant of milnacipran analgesic and anti-inflammatory influences.
Oxidative and nitrosative stress in the tissue is a pivotal parameter in the carrageenan paw inflammation (Mizokami et al. 2016). Since milnacipran prevented inflammation induced by carrageenan, it was convincing to define whether milnacipran also prevents oxidative stress. Therefore, another factor in the carrageenan-induced inflammation pathway is malondialdehyde that it increased during the oxidative stress reaction. Neutrophils create a lot of the anions of superoxide, thereby participating in several of the harmful consequences of inflammation, including hyperalgesia following tissue damage and oxidative stress (Littlejohn and Guymer 2018). In accordance with this, the level of MDA as a lipid peroxidation marker increased subsequent to carrageenan injection in the hind paw tissue in the current study, which proves the involvement of oxidative stress in the carrageenan-induced inflammation. According to the study of Bilici et al. (2002) intraplantar injection of carrageenan can increase the level of MDA and oxidative stress significantly which is in agreement with the findings of the present study. Furthermore, in the present study, it has revealed that milnacipran in all doses attenuated oxidative stress level as measured by MDA level in the hind paw tissue. In accordance with these findings, Hammody et al. examined the effect of pregabalin and amitriptyline on patients with fibromyalgia and concluded that amitriptyline can decrease MDA level and oxidative stress (Hammody et al. 2015).
Furthermore, in the present study, carrageenan increased the level of NO, as a nitrosative stress hallmark, in the inflamed paw tissue. NO is a crucial mediator in the first and second phases of carrageenan-induced rat paw inflammation, which contributes to edema progression and augmentation of hyperalgesia (Namgyal and Sarwat 2020; Sharma et al. 2020). The results of this study are totally in agreement with the previous reports on the increasing of NO production following carrageenan injection in the paw tissue (Mizokami et al. 2016; Namgyal and Sarwat 2020; Sharma et al. 2020). On the other hand, milnacipran in the doses of 20 and 40 mg/kg prevented from carrageenan-induced NO generation in the paw tissue. Macrophages and neutrophils are the potential origins of NO in the course of inflammation (Guay et al. 2004; Morris 2003), hence, a possible goal of milnacipran effect. Therefore, the attenuation in the recruitment of neutrophil in the paw tissue may be responsible for the milnacipran suppression of carrageenan-induced NO creation in the paw tissue.
It is outstanding to notice that, in the current study, total antioxidant capacity in the paw tissue attenuated after carrageenan injection. Also, we demonstrated that milnacipran in all doses prevented the carrageenan-induced peripheral reduction in total antioxidant capacity in paw tissue. Hence, the effect of milnacipran in restricting MDA and NO secretion and enhancing of TAC may be as a result of the reduction of tissue injuries concurrently with the decrease of oxidative stress. It can be assumed that antioxidative effect of milnacipran in this study may be exerted via its oxidative/nitrosative stress factors reduction, as appraised by MDA and NO level attenuation as well as TAC augmentation. However, more investigations are essential to clarify the effects of milnacipran on RNS/ROS production.
Conclusion
Based on the findings of the current study, it can be concluded that milnacipran has had analgesic and anti-inflammatory effects on carrageenan-induced pain and inflammation, and proposes some possible mechanisms of action. We suppose that suppression of MDA and NO production and MPO activity inhibition, reducing IL-1β, IL-6 and TNF-α secretion, and enhancement of TAC are crucial determinant of milnacipran analgesic and anti-inflammatory influences in the injured site. It seems that milnacipran can be considered as an alternative or combination therapy for the treatment of pain and inflammation in the future. But there is a need for some clinical trials study to confirm this statement.
References
Bach-Rojecky L, Lackovic Z (2005) Antinociceptive effect of botulinum toxin type a in rat model of carrageenan and capsaicin induced pain. Croat Med J 46:201–208
Bavill J (1997) Mechanisms of action of opioid and non-steroidal antiœinflammatory drug. Eur J Anesthesiol 14:9
Berrocoso E, Mico J-A, Vitton O, Ladure P, Newman-Tancredi A, Depoortère R, Bardin L (2011) Evaluation of milnacipran, in comparison with amitriptyline, on cold and mechanical allodynia in a rat model of neuropathic pain. Euro J Pharmacol 655:46–51
Bilici D, Akpinar E, Kiziltunc A (2002) Protective effect of melatonin in carrageenan-induced acute local inflammation. Pharmacolog Res 46:133–139
Brune K, Patrignani P (2015) New insights into the use of currently available non-steroidal anti-inflammatory drugs. J Pain Res 8:105
Buritova J, Honoré P, Besson J-M (1995) Indomethacin reduces both Krox-24 expression in the rat lumbar spinal cord and inflammatory signs following intraplantar carrageenan. Brain Res 674:211–220
Derry S, Gill D, Phillips T, Moore RA (2012) Milnacipran for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev 3(3):CD008244
Dharmshaktu P, Tayal V, Kalra BS (2012) Efficacy of antidepressants as analgesics: a review. J Clin Pharmacol 52:6–17
Fröde TS, Medeiros Y (2001) Myeloperoxidase and adenosine-deaminase levels in the pleural fluid leakage induced by carrageenan in the mouse model of pleurisy. Mediators Inflamm 10:223–227
Guay J, Bateman K, Gordon R, Mancini J, Riendeau D (2004) Carrageenan-induced paw edema in rat elicits a predominant prostaglandin E2 (PGE2) response in the central nervous system associated with the induction of microsomal PGE2 synthase-1. J Biol Chem 279:24866–24872
Haddadi R, Nayebi AM, Brooshghalan SE (2018a) Silymarin prevents apoptosis through inhibiting the bax/caspase-3 expression and suppresses toll like receptor-4 pathway in the SNc of 6-OHDA intoxicated rats. Biomed Pharmacother 104:127–136
Haddadi R, Poursina M, Zeraati F, Nadi F (2018b) Gastrodin microinjection suppresses 6-OHDA-induced motor impairments in parkinsonian rats: insights into oxidative balance and microglial activation in SNc Inflammopharmacology. Inflammopharmacology 26(5):1305–1316
Hammody LE, Matloub SY, Shihab SS (2015) Pregabalin versus amitriptyline in the treatment of fibromyalgia patients (a double blind comparative study). Iraqi Acad Sci J 14:38–44
Handy RL, Moore PK (1998) Effects of selective inhibitors of neuronal nitric oxide synthase on carrageenan-induced mechanical and thermal hyperalgesia. Neuropharmacology 37:37–43
Hosseini A, Abdollahi M (2013) Diabetic neuropathy and oxidative stress: therapeutic perspectives oxidative medicine and cellular longevity 2013:168039
Hwang H-J, Lee H-J, Kim C-J, Shim I, Hahm D-H (2008) Inhibitory effect of amygdalin on lipopolysaccharide-inducible TNF-alpha and IL-1beta mRNA expression and carrageenan-induced rat arthritis. J Microbiol Biotechnol 18:1641–1647
Kadetoff D, Lampa J, Westman M, Andersson M, Kosek E (2012) Evidence of central inflammation in fibromyalgia—increased cerebrospinal fluid interleukin-8 levels. J Neuroimmunol 242:33–38
Khattab MM (2006) TEMPOL, a membrane-permeable radical scavenger, attenuates peroxynitrite-and superoxide anion-enhanced carrageenan-induced paw edema and hyperalgesia: a key role for superoxide anion. Euro J Pharmacol 548:167–173
Kheradmand A, Mohajjel Nayebi A, Jorjani M, Haddadi R (2016a) Effect of WR-1065 on 6-hydroxydopamine-induced catalepsy and IL-6 level in rats. Iran J Basic Med Sci 19:490–496
Kheradmand A, Nayebi AM, Jorjani M, Khalifeh S, Haddadi R (2016b) Effects of WR1065 on 6-hydroxydopamine-induced motor imbalance: possible involvement of oxidative stress and inflammatory cytokines. Neurosci Lett 627:7–12. https://doi.org/10.1016/j.neulet.2016.05.040
King T, Rao S, Vanderah T, Chen Q, Vardanyan A, Porreca F (2006) Differential blockade of nerve injury-induced shift in weight bearing and thermal and tactile hypersensitivity by milnacipran. J Pain 7:513–520
Littlejohn G, Guymer E (2018) Neurogenic inflammation in fibromyalgia. Seminars in immunopathology, vol 3. Springer, Berlin, pp 291–300
Luedde T, Schwabe RF (2011) NF-κB in the liver—linking injury, fibrosis and hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol 8:108
Menendez L, Lastra A, Hidalgo A, Baamonde A (2002) Unilateral hot plate test: a simple and sensitive method for detecting central and peripheral hyperalgesia in mice. J Neurosci Methods 113:91–97
Mico JA, Berrocoso E, Vitton O, Ladure P, Newman-Tancredi A, Bardin L, Depoortère R (2011) Effects of milnacipran, duloxetine and indomethacin, in polyarthritic rats using the Randall–Selitto model. Behav Pharmacol 22:599–606
Mizokami SS et al (2016) Pimaradienoic acid inhibits carrageenan-induced inflammatory leukocyte recruitment and edema in mice: inhibition of oxidative stress, nitric oxide and cytokine production. PLoS ONE 11:e0149656
Morris CJ (2003) Carrageenan-induced paw edema in the rat and mouse. Inflammation protocols. Springer, Berlin, pp 115–121
Namgyal D, Sarwat M (2020) Saffron as a neuroprotective agent. Saffron. Elsevier, Netherlands, pp 93–102
Neeb L, Hellen P, Boehnke C, Hoffmann J, Schuh-Hofer S, Dirnagl U, Reuter U (2011) IL-1β stimulates COX-2 dependent PGE2 synthesis and CGRP release in rat trigeminal ganglia cells. PLoS ONE 6(3):e17360
Rafiee L, Hajhashemi V, Javanmard SH (2017) In vitro and in vivo modulation of LPS and carrageenan-induced expression of inflammatory genes by amitriptyline. J Pharm Pharmacog Res 5:144–155
Rao P, Knaus EE (2008) Evolution of nonsteroidal anti-inflammatory drugs (NSAIDs): cyclooxygenase (COX) inhibition and beyond. J Pharm Pharmaceut Sci 11:81–110
Rodriguez-Pintó I, Agmon-Levin N, Howard A, Shoenfeld Y (2014) Fibromyalgia and cytokines. Immunol Lett 161:200–203
Ruiz-Miyazawa KW, Zarpelon AC, Pinho-Ribeiro FA, Pavão-de-Souza GF, Casagrande R, Verri WA Jr (2015) Vinpocetine reduces carrageenan-induced inflammatory hyperalgesia in mice by inhibiting oxidative stress, cytokine production and NF-κB activation in the paw and spinal cord. PLoS ONE 10:e0118942
Sammons MJ, Raval P, Davey PT, Rogers D, Parsons AA, Bingham S (2000) Carrageenan-induced thermal hyperalgesia in the mouse: role of nerve growth factor and the mitogen-activated protein kinase pathway. Brain Res 876:48–54
Sayyah M, Mandgary A, Kamalinejad M (2002) Evaluation of the anticonvulsant activity of the seed acetone extract of Ferula gummosa Boiss. against seizures induced by pentylenetetrazole and electroconvulsive shock in mice. J Ethnopharmacol 82:105–109
Schug SA, Zech D, Grond S (1992) Adverse effects of systemic opioid analgesics. Drug Saf 7:200–213
Sharma B, Kumar H, Kaushik P, Mirza R, Awasthi R, Kulkarni G (2020) Therapeutic benefits of saffron in brain diseases: new lights on possible pharmacological mechanisms. Saffron. Elsevier, Netherlands, pp 117–130
Stejskal V, Öckert K, Bjørklund G (2013) Metal-induced inflammation triggers fibromyalgia in metal-allergic patients. Neuroendocrinol Lett 34:559–565
Suarez-Roca H, Quintero L, Arcaya JL, Maixner W, Rao SG (2006) Stress-induced muscle and cutaneous hyperalgesia: differential effect of milnacipran. Physiol Behav 88:82–87
Surh Y-J, Chun K-S, Cha H-H, Han SS, Keum Y-S, Park K-K, Lee SS (2001) Molecular mechanisms underlying chemopreventive activities of anti-inflammatory phytochemicals: down-regulation of COX-2 and iNOS through suppression of NF-κB activation. Mutat Res Fundament Mol Mech Mutagene 480:243–268
Taler M et al (2007) Immunomodulatory effect of selective serotonin reuptake inhibitors (SSRIs) on human T lymphocyte function and gene expression. Eur Neuropsychopharmacol 17:774–780
Tsuruoka M, Arai Y-CP, Nomura H, Matsutani K, Willis WD (2003) Unilateral hindpaw inflammation induces bilateral activation of the locus coeruleus and the nucleus subcoeruleus in the rat. Brain Res Bull 61:117–123
Tynan RJ, Weidenhofer J, Hinwood M, Cairns MJ, Day TA, Walker FR (2012) A comparative examination of the anti-inflammatory effects of SSRI and SNRI antidepressants on LPS stimulated microglia. Brain Behav Immun 26:469–479
Varghese AK, Verdú EF, Bercik P, Khan WI, Blennerhassett PA, Szechtman H, Collins SM (2006) Antidepressants attenuate increased susceptibility to colitis in a murine model of depression. Gastroenterology 130:1743–1753
Yaksh TL (1981) The antinociceptive effects of intrathecally administered levonantradol and desacetyllevonantradol in the rat. J Clin Pharmacol 21(S1):334S–340S
Yang N, Zhang W, Shi XM (2008) Glucocorticoid-induced leucine zipper (GILZ) mediates glucocorticoid action and inhibits inflammatory cytokine-induced COX-2 expression. J Cell Biochem 103:1760–1771
Yaron I, Shirazi I, Judovich R, Levartovsky D, Caspi D, Yaron M (1999) Fluoxetine and amitriptyline inhibit nitric oxide, prostaglandin E2, and hyaluronic acid production in human synovial cells and synovial tissue cultures. Arthritis Rheum Off J Am Coll Rheumatol 42:2561–2568
Acknowledgements
These data were adopted from the Pharm D. thesis of Dr. Rojin Rashtiani. The authors would like to thank Research and Technology Vice-Chancellor of Hamadan University of Medical Sciences (Hamadan, Iran) for supporting this study.
Funding
This work was supported by a grant from Research and Technology Vice-Chancellor of Hamadan University of Medical Sciences, Hamadan, Iran (code: 9605103034).
Author information
Authors and Affiliations
Contributions
RH, the supervisor of the study, was involved in concept, design, support of study, interpretation of data, drafting and final check of the draft. RR carried out the behavioral experiments, biochemical analyzes, statistical analyzes and drafting. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haddadi, R., Rashtiani, R. Anti-inflammatory and anti-hyperalgesic effects of milnacipran in inflamed rats: involvement of myeloperoxidase activity, cytokines and oxidative/nitrosative stress. Inflammopharmacol 28, 903–913 (2020). https://doi.org/10.1007/s10787-020-00726-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-020-00726-2