Abstract—
Rheumatoid arthritis (RA) is chronic inflammatory autoimmune disease. The crucial role of long non-coding RNA (lncRNA) in the progression of RA has been highlighted. Hence, this study was designed to explore the specific downstream mechanism of lncRNA nuclear-enriched abundant transcript 1 (NEAT1) in RA. Initially, the expression of NEAT1, p-p65, p300, and IL-18 in clinical tissues and cells was determined. Then, interactions among p65, NEAT1, p300, CBP, and IL-18 were investigated by immunofluorescence staining, dual luciferase reporter gene assay, RT-qPCR assay ChIP assay, and RIP assay followed by the analysis of their effects on RA in vivo and in vitro after expression alteration. The expressions of NEAT1, p-p65, p300, and IL-18 were all upregulated in the synovial tissues from the mice and patients with RA. NEAT1 silencing reduced the infiltration of CD4+ T cells and macrophages in synovial tissues, downregulated expression of blood inflammatory factors, relieved RA severity, and lowered incidence of RA in mice. Further, p-p65 could increase the expression of NEAT1 by binding to the NEAT1 promoter region, NEAT1 could co-locate and interact with p300, thus regulating the expression of IL-18 by regulating histone acetylation modification in IL-18 promoter region. NEAT1 aggravated RA via p300/CBP/IL-18 axis, representing a promising therapeutic target in RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Rheumatoid arthritis (RA) is an autoimmune disorder that mainly acts on synovial joints, which induces synovitis, joint synovial hypertrophy, cartilage, and bone impairment, autoantigen generation, and generalized symptoms [1]. RA is characterized by the production of eicosanoids, cell factors, adhesion molecules, and T and B lymphocytes infiltration in the synovial membrane [2]. Risk factors for RA include gender, smoking, and family history [3]. The main targets of RA disease management are remission and low disease activity attainment [4, 5]. The identification of new targets and their association with disease vulnerability may be of help to better understand RA pathogenesis [6]. Therefore, more efficient therapies are expected, and this study aims to supply a gap by making an in-depth research on the working mechanism of long non-coding RNA nuclear-enriched abundant transcript 1 (lncRNA NEAT1) in RA on a molecular level.
LncRNAs are a group of transcripts with over 200 nucleotides without open reading frame, which participate in the regulation of a series of cellular processes, such as genomic integrity, chromatin organization, genetic expression, transcription, and cell signaling [7]. Recent researches have proposed lncRNAs as important biological regulators, and it has been demonstrated that the aberrant expression of lncRNAs is of great importance in the pathological processes of RA [8, 9]. For instance, lncRNA 162 presents a high expression in synovial fluid of patients with RA, and its suppression was confirmed to alleviate RA [10]. More importantly, NEAT1 knockdown has been reported to be an inhibitor of Th17/CD4+ T cell differentiation, thereby further playing a repressing role in the development of RA [11]. p300 is a histone acetyltransferase, which has been illustrated as a key mediator in numerous diseases, such as malignancies [12]. CBP, another histone acetyltransferase, can regulate transcription by acetylating histone and non-histone substrates [13]. p300 and CBP are two well-known closely related multifunctional transcriptional co-activators, which serve as prospective targets for cancers and immune system disorders management [14]. For example, it was reported that p300/CBP repression could be novel targets for RA treatment [15]. Interleukin 18 (IL-18) is a pleiotropic cytokine, which is responsible for the regulation of natural and adaptive immune response [16]. Besides, IL-18 inhibition acts as a novel therapeutic target for RA treatment [17]. Taken together, it can be inferred that repression of NEAT1, p300/CBP, or IL-18 can all exert a reliving role on the progression of RA, but their specific interactions with each other remains largely uncertain in RA. Hence, the present study was conducted for exploration purpose to ultimately provide a novel solution to a highly effective RA therapy.
MATERIALS AND METHODS
Ethics Statement
The current study was performed with the approval of the ethics committee of Xianyang Central Hospital and has conformed to the Declaration of Helsinki. Written informed consent was obtained from each participant. All animal experiments were performed in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health.
Study Subjects
Forty-two patients with RA (18 males and 24 females with a mean age of 50.57 ± 3.35 years) and 48 patients (19 male and 29 females and a mean age of 50.17 ± 4.39 years) who underwent bone joint replacements (including patients with comminuted fractures due to car accident and other causes) were selected. The healthy joint synovial tissues were obtained from 48 patients who underwent bone joint replacements due to car accidents and other reasons. None of these 48 patients had history of acute or chronic joint diseases. Patient’s clinical data are listed in Supplementary Table 1. Synovial tissues and serum were collected. Synovial tissues were collected aseptically and placed in a sterile 50-mL centrifuge tube after surgery and placed on ice. Then, the adipose tissues, bones, and blood vessels were removed on a sterile operating table. The collected synovial tissues were washed with physiological saline three times and put in the sterile tube and frozen in a liquid nitrogen tank for subsequent research.
Mouse Model of RA Induced by Type II Collagen
Male DBA/1 mice (8 weeks old) are purchased from the Qingdao Experimental Animal Center (Qingdao, China) for use as model establishment. The modeled mice were co-infected with lentivirus (lenti)-short hairpin RNA (sh)-negative control (NC), lenti-sh-NEAT1, overexpressed (oe)-NC + sh-NC, oe-NEAT1 + sh-NC, oe-NEAT1 + sh-p300, oe-p65 + sh-NC, and oe-p65 + sh-IL-18, respectively, 15 DBA/1 mice for each treatment. On the first day, type II collagen (Chondrex, Seattle, WA, USA) was fully mixed with complete Freund’s adjuvant. DBA/1 mice were immunized by injecting the sample subcutaneously at the tail base, 0.1 mL each. On the 21st day, type II collagen and incomplete Freund’s adjuvant were used for the second immunization for the first time. The model was established and then identified to ensure successful modeling. The occurrence of inflammation after induction of collagen-induced arthritis (CIA) was regularly observed to determine the incidence of arthritis and conduct clinical evaluation of arthritis according to the malignant degree of arthritis development. The blank control group was immunized with normal saline instead of type II collagen, and the specific operation was consistent with that of a modeled mice. To examine the effect of NEAT1 knockdown on arthritis, lentivirus-expressing lenti-sh-NEAT1 was injected into mice via the tail vein after the second immunization. Arthritis assessment was performed every 3 days after injection of the lentivirus. All mice were euthanized after modeling, and their joint synovial tissues were taken to extract the total RNA and protein of the cells for subsequent use.
Arthritis clinical evaluation was conducted as follows: (1) The pathological changes of the paws in the front and rear of the mice were observed, and the 0–4 score system was employed to score arthritis index. (2) The score of each mouse was the sum of the scores of the front and rear feet, and the highest score was 16 points. (3) Scoring criteria were 0 points for no symptoms, 1 point for slight swelling of the toe joint, 2 points for slight swelling of the toe joint and foot plantar, 3 points for moderate swelling of the paw from below the ankle, and 4 points for swelling of the paws or joint stiffness of the extremities of all of the feet.
Enzyme-linked Immunosorbent Assay (ELISA)
The peripheral blood of the mice was taken to detect the expression of inflammatory factors TNF-α (MTA00B), IFN-γ (DY485), IL-6 (M6000B), and IL-18 (DY122-05) by an ELISA kit (R&D Systems, Minneapolis, MN, USA). The optical density (OD) value was measured by using a microplate reader (Bio-Rad, Hercules, CA, USA) at an absorbance of 450 nm (A450).
Hematoxylin and Eosin (HE) Staining
The synovial tissues were dehydrated with gradient ethanol solutions of 70%, 80%, 90%, and 100% concentration in turn, cleared by xylene, immersed in paraffin, embedded, fixed on a microtome, and sliced into a 4-μm-thick cross section. Then sections were dewaxed using xylene I and II for 5 min each, hydrated with gradient alcohol of 100%, 95%, 85%, and 70% for 3 to 5 min each, washed with distilled water for 3 min, stained with hematoxylin for 10 min, and then washed using tap water for 10 min. Next, sections were treated by 1% hydrochloric acid ethanol for 2 s; rinsed under running water; stained by eosin for 10 min; dehydrated with gradient ethanol solutions of 70%, 80%, 90%, and 100%; cleared by xylene for 2 to 10 s; sealed by neutral gum; and photographed with an optical microscope. Synovial tissue score: 0 for normal morphology, 1 for minor injury, 2 for moderate injury, and 3 for severe injury.
Immunohistochemistry (IHC) Staining
Paraffin sections were dewaxed to water, dehydrated with gradient alcohol, washed with tap water for 2 min, treated in 3% methanol in H2O2 for 20 min, washed with distilled water for 2 min, washed with 0.1 M phosphate-buffered saline (PBS) for 3 min, repaired in antigen repair solution with water bath, and cooled by tap water. Sections were then added with normal goat serum-blocking solution (C-0005, Shanghai Haoranbio Co. Ltd., Shanghai, China) dropwisely and left at room temperature for 20 min. Then, sections were incubated with primary antibody [CD4: 25,229, Cell Signaling Technology (CST, Danvers, MA, USA), F4/80: 70,076, CST] overnight at 4 °C, washed 3 times in 0.1 M PBS for 5 min/time, incubated with secondary antibody horseradish peroxidase (HRP)-labeled working solution (0343-10000U, Imunbio Co. Ltd., Beijing, China) at 37 °C for 20 min, developed by 3,3′-diaminobenzidine tetrahydrochloride (ST033, Guangzhou Whiga Technology Co., Ltd., Guangzhou, Guangdong, China), washed, counterstained with hematoxylin (PT001, Shanghai Bogoo Biological Technology Co., Ltd., Shanghai, China) for 1 min, returned to blue by 1% ammonia water, dehydrated using a certain concentration of gradient alcohol, cleared using xylene, sealed with resin film, and observed and photographed under microscope. Five high-power fields were randomly selected for each section, and 100 cells were counted in each field.
Immunofluorescence Staining
The paraffin sections were dehydrated conventionally, sealed by goat serum, and allowed to stand for 30 min. Cells were incubated with primary antibody prepared by PBS and incubated at 4 °C overnight, then incubated with secondary antibody for 1 h in the dark at room temperature, stained with 4′-6-diamidino-2-phenylindole (DAPI) for 15 min in the dark, washed 3 times with PBS in the dark, and mounted by the fluorescence quencher. The control group adopted the sample without the primary antibody, and remaining steps are the same. Observation and photograph were conducted under the same exposure conditions under a fluorescence microscope.
Cell Primary Culture and Transfection
Synovial tissues were washed 3 times with PBS without calcium and magnesium and cut into small pieces of about 1 to 2 mm3 and put into a 6-well plate. Then, tissues were incubated with 2 mL 10% calf serum F12 + DMEM and 2 mL type III collagenase (2 mg/mL) for 2 h at 37 °C with 5% CO2. Non-adherent cells (adherent cells were macrophages from synovial tissues) were transferred into a centrifuge tube and centrifuged at 1000 rpm for 10 min with the supernatant discarded. The samples were then disrupted with 4 mL of trypsin at 37 °C with 5% CO2 for 30 min, filtered through a 200-mesh stainless steel mesh, and the filtrate was centrifuged at 1000 rpm for 10 min. Then 1 × 105/mL cells per well were counted in the 6-well plate and incubated at 37 °C, with 5% CO2 for 24 h. Non-adherent cells (such as monocytes, lymphocytes, and red blood cells) were discarded. The adherent cells were the primary synovial cells. siRNA (si)-p65, si-NAET1, and si-p300 used in the cell transfection were synthesized by GenePharma (Shanghai, China), and two pairs of siRNAs were synthesized for each gene, and siRNA with the best knockdown effect was selected for subsequent experiments.
Reverse Transcription-Quantitative Polymerase Chain Reaction (RT-qPCR)
Total RNA was extracted using Trizol reagent (15,596,026, Invitrogen, Carlsbad, CA, USA), RNA was reversely transcribed according to the instructions of PrimeScriptRT reagent Kit (RR047A, Takara, Tokyo, Japan), and the synthesized complementary (cDNA) was subjected to RT-qPCR detection using Fast SYBR Green PCR reagent (Applied Biosystems Inc., Carlsbad, CA, USA) and ABI PRISM 7300 RT-PCR system (Applied Biosystems), and three replicates were set for each well. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as an internal reference, and the relative gene expression was analyzed by 2−ΔΔCt method. Primer sequences used for RT-qPCR are presented in Supplementary Table 2.
Western Blot Analysis
Cells were trypsinized and then lysed with the enhanced radioimmunoprecipitation assay lysis buffer (Boster Biological Technology Co. Ltd., Wuhan, Hubei, China) containing protease inhibitors, and then, the protein concentration was determined using the bicinchoninic acid protein quantification kit (Boster Biological Technology Co. Ltd.). Proteins were then separated by 10% sodium dodecyl sulfate–polyacrylamide gel electrophoresis gel, and the separated proteins were electro-transferred to a polyvinylidene fluoride membrane. Then, the membrane was blocked by 5% BSA at room temperature for 2 h to block non-specific binding, incubated with diluted primary antibodies at 4 °C overnight, and incubated with HRP-labeled secondary antibodies at room temperature for 1 h. The membrane was then treated with ECL working solution (EMD Millipore, Billerica, MA, USA) at room temperature for 1 min, sealed, exposed, and imaged. Image J analysis software was used to quantify the gray levels of each group of bands in Western blot images, and β-actin was used as an internal reference.
Fluorescence In Situ Hybridization (FISH)
The location of NEAT1 in cells was identified using FISH technology according to the instructions of Ribo™ lncRNA FISH Probe Mix (Red) (RiboBio Company, Guangzhou, Guangdong, China). Briefly, a cover slip was put in a 6-well plate, and normal synovial cells (105 cells/well) were seeded into the plate upon 80% confluence after 1 day of culturing. The slip was taken out and fixed with 1 mL of 4% paraformaldehyde at room temperature. After treatment with proteinase K (2 μg/mL), glycine, and acetalization reagent, cells were incubated with 250 μL of prehybridization solution at 42 °C for 1 h, then the hybridization solution were aspirated, and cells were incubated with 250 μL of hybridization solution containing NEAT1 probe (300 ng/mL) (cat: SMF-3010–1, Biosearch Technologies, Petaluma, CA, USA) at 42 °C overnight. After being washed with PBST three times, cells were added with phosphate-buffered saline/Tween (PBST)-diluted DAPI (1:800) to stain the nucleus in a 24-well culture plate for 5 min and mounted with anti-fluorescence quencher. Five different fields of view were selected under a fluorescence microscope (Olympus, Tokyo, Japan), observed, and photographed.
RNA-Binding Protein Immunoprecipitation (RIP) Assay
The binding of NEAT1 to p300/CREB-binding protein (CBP) complex was explored using a RIP kit (Millipore). Cells were washed with pre-cooled PBS, and the supernatant was discarded. Cells were lysed with an equal volume of RIPA lysis buffer (P0013B, Beyotime, Shanghai, China) in an ice bath for 5 min, and centrifuged at 14,000 rpm and 4 °C for 10 min to obtain supernatant. A part of the cell extract was taken as an input, and a part was incubated with antibody for co-precipitation. The sample and input were disrupted with proteinase K to extract RNA and were used for subsequent RT-qPCR detection of NEAT1.
Chromatin Immunoprecipitation (ChIP) Assay
When cell confluence reached 70 to 80%, the cells were fixed with 1% formaldehyde at room temperature for 10 min to cross-link DNA and protein in the cells. After ultra-sonication treatment, the cells were broken into fragments of appropriate size and centrifuged at 4 °C and 13,000 rpm, and the supernatant was collected into three tubes, added with positive control antibody RNA polymerization enzyme II, negative control antibody Normal IgG, and H3K4Me3 antibody (ab8580, Abcam, Cambridge, UK) or H3K27Me3 antibody (ab6002, Abcam) or H3K27Ac antibody (ab4729, Abcam), respectively, and incubated at 4 °C overnight. Protein agarose/sepharose was used to precipitate endogenous DNA–protein complexes, the supernatant was discarded after a short time of centrifugation, and the non-specific complex was washed. Next, the cross-linking was terminated overnight at 65 °C, and the DNA fragments were recovered by phenol/chloroform extraction. The expression of the promoter was measured by RT-qPCR.
Dual Luciferase Reporter Gene Assay
The artificially synthesized IL-18 5′UTR gene fragment was introduced into the pGL3-basic vector (Promega, Madison, WI, USA) by enzyme digestion, and the correctly sequenced IL-18 luciferase reporters were co-transfected with oe-NC, oe-NEAT1, si-NC, or si-NEAT1 into HEK293T cells. After 48 h of transfection, cells were collected and lysed, and luciferase was detected on the Luminometer TD-20/20 detector (model: E5311, Promega) using the Dual-Luciferase Reporter Assay System kit (Promega).
Artificially synthesized IL-18 5′UTR gene fragment was introduced into pGL3-basic vector (Promega) by enzyme digestion, and correctly sequenced IL-18 luciferase reporters were co-transfected with oe-NC, oe-p300, si-NC, or si-p300 into HEK293T cells. The following experimental procedures were the same as above.
Statistical Analysis
All experimental data were analyzed using the Statistic Package for Social Science (SPSS) 21.0 statistical software (IBM Corp, Armonk, NY, USA). The measurement data were expressed as mean ± standard deviation. Comparison between two groups was analyzed by unpaired t test. Comparisons among multiple groups were performed using one-way analysis of variance (ANOVA) with Tukey’s post hoc test. Comparison among multiple groups at different time points was performed by repeated measures ANOVA with Tukey’s post hoc test. Results of RIP assay were analyzed using two-way ANOVA with Tukey’s post hoc test. A p value less than 0.05 was considered statistically significant.
RESULTS
NEAT1 Presents a High Expression in Synovial Tissues of RA Patients and Silencing NEAT1 Can Alleviate RA
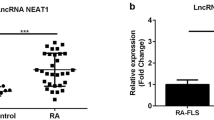
The expression of lncRNA in 42 synovial tissues of RA patients and bone joint replacement patients was determined. The results of RT-qPCR showed that compared with that of normal synovial tissues, the expression of NEAT1 increased in the synovial tissues of RA patients (Fig. 1A). In the synovial tissues of RA mice induced by type II collagen, RT-qPCR results illustrated that the expression of NEAT1 in the synovial tissues of CIA mice was increased notably compared with that of the control mice (Fig. 1B). CIA mouse model induced by type II collagen was injected with lentivirus expressing sh-NEAT1, and the expression of NEAT1 in knee joint synovial tissues was determined by RT-qPCR. Results presented that after sh-NEAT1 injection, the expression of NEAT1 was suppressed, validating the successful infection (Fig. 1C). Throughout the development of the disease, the arthritis score of CIA mice injected with lentivirus expressing sh-NEAT1 was obviously lower than that of mice injected with lentivirus expressing sh-NC, which suggested that NEAT1 silencing can relieve RA in mice (Fig. 1D).
Inhibition of NEAT1 alleviates RA. A The expression of NEAT1 in synovial tissues of RA patients and bone joint replacement patients determined by RT-qPCR, control = 48, RA = 42. B The expression of NEAT1 in synovial tissues of RA mice and control mice determined by RT-qPCR, n = 15. C The expression of NEAT1 after injection of lentivirus expressing Lenti-sh-NEAT1 measured by RT-qPCR, n = 15. D Observation of mouse limbs at different times after injection of lentivirus according to the severity of arthritis score, n = 15. E Synovial tissue damage observed by HE staining, n = 15. F, Kaplan–Meier curve of the incidence of RA in mice, n = 15. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Measurement data were expressed as mean ± standard deviation. Comparison between two groups was analyzed by unpaired t test. Comparisons among multiple groups were performed using one-way ANOVA with Tukey’s post hoc test. Comparison among multiple groups at different time points was performed by repeated measures ANOVA with Tukey’s post hoc test.
HE staining was performed on the synovial tissues of the mouse joints, which demonstrated that compared with that of control mice, the synovial tissues of model mice injected with Lenti-sh-NC thickened to form the Pannus layer (P), leading to severe joint damage and infiltration of a large number of immune cells in the downstream of the Pannus layer (N), whereas the damage of mice injected with lentivirus expressing sh-NEAT1 was better than that of mice injected with lentivirus expressing sh-NC (Fig. 1E). Statistics of the incidence of arthritis revealed that the incidence of arthritis in mice injected with lentivirus expressing sh-NEAT1 was also markedly lower than that of the mice injected with lentivirus expressing sh-NC (Fig. 1F). Abovementioned results supported that NEAT1 was highly expressed in the synovial tissues of RA mice, and inhibition of NEAT1 could alleviate the progression of RA.
NEAT1 Knockdown Relieves Inflammation of Synovial Tissues
To study the effect of NEAT1 silencing on inflammation of mouse joint synovial tissues, IHC staining was used to detect CD4+ T cells and F4/80+ macrophages in synovial tissues, and results displayed that CD4+ T cells and F4/80+ macrophages in synovial tissues of CIA mice were both increased compared with that of control mice, and injection of Lenti-sh-NEAT1 resulted in less number of CD4+ T cells and F4/80+ macrophages than that of mice injected with Lenti-sh-NC (Fig. 2A and B). ELISA results showed that the serum pro-inflammatory factors IL6, TNF-α, IFN-γ, and IL-18 of CIA mice were increased compared with that of the control mice; Lenti-sh-NEAT1 treatment reduced serum inflammatory factors, among which IL-18 changed most notably (Fig. 2C–F). Interestingly, neutrophil-derived lactoferrin (LTF) produced by neutrophils could also stimulate the production of pro-inflammatory factors, such as IL-6, CCL20, and IL-18 [6]. To sum up, the infiltration of CD4+ T cells and F4/80+ macrophages in the synovial tissues of arthritis mice increased, and the inflammatory factors in the blood increased, which was alleviated by silencing of NEAT1.
Knockdown of NEAT1 relieves inflammation in synovial tissues. A The infiltration of CD4+ T cells (n = 15) in synovial tissues of mice not immunized, injected with Lenti-sh-NC and Lenti-sh-NEAT1, respectively, determined by IHC staining. B The infiltration of F4/80+ macrophages (n = 15) in synovial tissues of mice not immunized, injected with Lenti-sh-NC and Lenti-sh-NEAT1, respectively, determined by IHC staining. C The expression of blood inflammatory factors TNF-α in mice not immunized, injected with Lenti-sh-NC, and Lenti-sh-NEAT1, respectively, determined by ELISA. D The expression of blood inflammatory factors IFN-γ (n = 15) in mice not immunized, injected with Lenti-sh-NC and Lenti-sh-NEAT1, respectively, determined by ELISA. E The expression of blood inflammatory factors IL-6 (n = 15) in mice not immunized, injected with Lenti-sh-NC and Lenti-sh-NEAT1, respectively, determined by ELISA. F The expression of blood inflammatory factors IL-18 (n = 15) in mice not immunized, injected with Lenti-sh-NC and Lenti-sh-NEAT1, respectively, determined by ELISA. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Measurement data were expressed as mean ± standard deviation. Comparisons among multiple groups were performed using one-way ANOVA with Tukey’s post hoc test.
Phosphorylated (p)-p65 Regulates NEAT1 Transcription Positively by Binding to the Promoter Region of NEAT1
The expression of p-p65 in the synovial tissues of patients with RA and normal synovial tissues was initially determined. Western blot results presented that p-p65 expression increased in the synovial tissues of patients with RA (Fig. 3A), and the expression of p-p65 in the synovial tissues of CIA mice also increased compared with that of control mice (Fig. 3B). Then, p65 was overexpressed or silenced in synovial cells from mice followed by determination of the expression of p-p65 by Western blot analysis. Results illustrated that overexpression of p65 caused a sharp increase in p-p65 expression, and knockdown of p65 decreased p-p65 expression (Fig. 3C). Besides, determination of expression of NEAT1 in synovial cells from mice by RT-qPCR results demonstrated that upregulation of p65 elevated NEAT1 expression, whereas downregulation of p65 decreased the expression of NEAT1 (Fig. 3D). ChIP assays were conducted to study the binding of p-p65 to the NEAT1 promoter region, and it was found that the binding of p-p65 antibody to the NEAT1 promoter region was dramatically higher than the binding of IgG to the NEAT1 promoter region, and NEAT1 silencing reduced the amount of p-p65 antibody in NEAT1 promoter region in synovial cells from mice (Fig. 3E). In short, p-p65 in synovial cells was bound to the NEAT1 promoter to regulate NEAT1 transcription.
NEAT1 transcription is regulated positively by p-p65. A The p-p65 expression in synovial tissues of human with RA and normal synovial tissues determined by Western blot analysis, control = 48, RA = 42. B The p-p65 expression in synovial tissues of CIA mice and normal mice determined by Western blot analysis (n = 15). C The p-p65 expression in synovial cells from mice transfected with oe-NC, oe-p65, sh-NC, or sh-p65 determined by Western blot analysis. D The NEAT1 expression in synovial cells from mice transfected with oe-NC, oe-p65, sh-NC, or sh-p65 determined by RT-qPCR. E The binding of p-p65 antibody and IgG to the NEAT1 promoter region detected by ChIP assay. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Measurement data were expressed as mean ± standard deviation. Comparison between two groups was analyzed by unpaired t test. Results of RIP assay were analyzed using two-way ANOVA with Tukey’s post hoc test. The experiments were repeated three times.
NEAT1 Co-localizes with p300/CBP Complex
NEAT1 can bind to p300/CBP complex to further change the H3K27 acetylation levels near the transcription start site of some genes [18]. Therefore, it was speculated that NEAT1 affects the level of H3K27 acetylation near the transcription start site of IL-18 by interacting with p300, thereby affecting IL-18 expression. To verify this hypothesis, the interaction between NEAT1 and p300 in synovial cells was examined. The expression of p300 in the synovial tissues of patients with RA and normal synovial tissues was measured. Results of Western blot analysis uncovered that the expression of p300/CBP complex increased in the synovial tissues of patients with RA (Fig. 4A). Compared with that of control mice, the expression of p300/CBP complex in synovial tissues of CIA mice also elevated (Fig. 4B).
Co-localization of NEAT1 and p300/CBP complex. A The expression of p300 and CBP in synovial tissues of patients with RA and normal synovial tissues determined by Western blot analysis. control = 48, RA = 42. B The expression of p300 and CBP in synovial tissues in CIA mice and normal mice determined by Western blot analysis (n = 15). C Statistical diagram of possible binding sites of p300 and CBP on the NEAT1 sequence, the boxes represent primer amplification regions. D The binding sites of p300/CBP to NEAT1 in synovial cell lysate from mice determined by RIP assay. E, Confocal images of NEAT1 probe and p300 antibody or CBP antibody (green) in synovial cells from mice (scare bar = 25 μm). *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Measurement data were expressed as mean ± standard deviation. Comparison between two groups was analyzed by unpaired t test. Comparison among multiple groups was analyzed by one-way ANOVA with Tukey’s post hoc test. The experiments were repeated three times.
Then, synovial cell lysate from mice was collected and immunoprecipitated with p300 antibody or IgG antibody by conducting RIP assay, and the NEAT1 fragment was detected by RT-qPCR. The results demonstrated that p300 bound to fragments 1, 2, 3, 5, and 6 of NEAT1, and CBP bound to fragments 1, 2, 3, 4, and 5 of NEAT1 (Fig. 4C and D). Subsequently, RNA-FISH and immunofluorescence assays showed that NEAT1 co-localized with p300 and CBP in synovial cells from mice (Fig. 4E). To conclude, NEAT1 could interact with p300/CBP complex by co-localizing with them in synovial cells.
NEAT1 Positively Regulates IL-18 Expression by Regulating Histone Modification in the IL-18 Promoter Region
The expression of IL-18 in the synovial tissues of patients with RA and normal synovial tissues was initially measured with the results revealing that the expression of IL-18 increased in the synovial tissues of patients (Fig. 5A) and in the synovial tissues of CIA mice (Fig. 5B) when compared with their separate controls. To study the regulatory effect of NEAT1 on IL-18, synovial cells from mice were transfected with oe-NEAT1 or sh-NEAT1 with the overexpression and silencing efficiency confirmed by RT-qPCR (Fig. 5C). Subsequently, RT-qPCR determination demonstrated that overexpression of NEAT1 in synovial cells increased the IL-18 mRNA level, whereas NEAT1 knockdown decreased it (Fig. 5D). Luciferase assay supported that NEAT1 overexpression promoted the transcription of the IL-18 promoter reporter, and NEAT1 knockdown inhibited the transcription of the IL-18 promoter reporter (Fig. 5E). Considering that NEAT1 may affect IL-18 transcription by affecting histone modifications in the IL-18 promoter region, histone modifications near the IL-18 promoter region, including H3K4Me3, H3K27Ac, and H3K27Me3, were detected by ChIP assay. Among them, H3K4Me3 modification and H3K27Ac modification near the transcription start site activated gene transcription, and H3K27Me3 modification inhibited gene transcription, illustrating that NEAT1 silencing reduced H3K27Ac modification near the transcription start site of IL-18 (Fig. 5F). In addition, the synovial cells of CIA mice and control mice were obtained, the IL-18 promoter region was immunoprecipitated, and H3K27Ac protein was determined by Western blot analysis. It was found that compared with that of the control mice, H3K27Ac modification in IL-18 promoter region in the CIA mouse was increased sharply (Fig. 5G). All in all, NEAT1 could positively regulate IL-18 transcription by changing the histone modification status of the IL-18 promoter region.
IL-18 is regulated by NEAT1 through histone modification regulation. A The expression of IL-18 in synovial tissues of patients with RA and normal synovial tissues determined by Western blot analysis and RT-qPCR, control = 48, RA = 42. B The expression of IL-18 in synovial tissues of mice with CIA and normal mice determined by Western blot analysis and RT-qPCR (n = 15). C The expression of NEAT1 in synovial cells from mice transfected with oe-NC or oe-NEAT1 determined by RT-qPCR. D The expression of IL-18 in synovial cells from mice transfected with oe-NEAT1, sh-NEAT1, or their negative controls (oe-NC, sh-NC) determined by RT-qPCR. E The luciferase activity of synovial cells co-transfected with oe-lNEAT1, sh-NEAT1, or their negative controls (oe-NC, sh-NC) determined by dual luciferase reporter gene assay. F The histone modifications near the IL-18 promoter region, including H3K4Me3, H3K27Ac, and H3K27Me3 in synovial cells from mice detected by ChIP assay. G The expression of H3K27Ac in IL-18 promoter region after immunoprecipitation in synovial tissues of CIA mice or normal mice determined by Western blot analysis. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Measurement data were expressed as mean ± standard deviation. Comparison between two groups was analyzed by unpaired t test. The experiments were repeated three times.
NEAT1 Regulates IL-18 Expression by Positively Mediating p300 Transcriptional Level
To investigate whether p300 can regulate the expression of IL-18 at the transcription level during the pathogenesis of RA, synovial cells from mice were initially transfected with oe-p300, sh-p300, or their NCs (oe-NC and sh-NC). Western blot analysis for measuring the protein expression of p300 revealed that oe-p300 transfection elevated p300 expression in synovial cells, whereas sh-p300 transfection reduced p300 expression, validating the transfection efficiency of p300 (Fig. 6A). Besides, transfection of oe-p300 increased the IL-18 mRNA expression notably, whereas transfection of sh-p300 led to the opposite trend (Fig. 6B). Luciferase reporter gene assay demonstrated that co-transfection of IL-18 luciferase reporters with oe-p300 in HEK293T cell increased the luciferase activity, whereas co-transfection of IL-18 luciferase reporters with si-p300 reduced the luciferase activity (Fig. 6C).
IL-18 is regulated by p300 transcriptional level. A The expression of p300 in synovial cells from mice after different transfection determined by Western blot analysis. B The expression of IL-18 in synovial cells from mice after different transfection determined by RT-qPCR. C Luciferase activity of synovial cells from mice after co-transfection of IL-18 luciferase reporter plasmid and oe-NC, oe-p300, sh-NC, or sh-p300 determined by dual luciferase reporter gene assay. D The expression of NEAT1 in synovial cells from mice after different transfection determined by Western blot analysis (n = 15). E The expression of p300 in synovial cells from mice after different transfection determined by Western blot analysis (n = 15). F The expression of IL-18 in synovial cells from mice after different transfection determined by RT-qPCR (n = 15). G Arthritis scores of mice after different transfection (n = 15). *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Measurement data were expressed as mean ± standard deviation. Comparison between two groups was analyzed by unpaired t test. Comparison among multiple groups was analyzed by one-way ANOVA with Tukey’s post hoc test. The experiments were repeated three times.
To further prove that the regulatory effect of NEAT1 on IL-18 was through p300, synovial cells were co-transfected with oe-NC + sh-NC, oe-NEAT1 + sh-NC, or oe-NEAT1 + sh-p300; RT-qPCR results illustrated that compared with that of cells co-transfected with oe-NC + sh-NC, the expression of NEAT1 in cells co-transfected with oe-NEAT1 + sh-NC or oe-NEAT1 + sh-p300 increased (Fig. 6D). Results of Western blot analysis presented that compared with that of cells co-transfected with oe-NC + sh-NC, the expression of p300 elevated sharply in cells co-transfected with oe-NEAT1 + sh-NC. Compared with that of cells co-transfected with oe-NEAT1 + sh-NC, the expression of p300 in cells co-transfected with oe-NEAT1 + sh-p300 reduced remarkably (Fig. 6E). ELISA results displayed that compared with that of cells co-transfected with oe-NC + sh-NC, the expression of IL-18 in cells co-transfected with oe-NEAT1 + sh-NC upregulated markedly. Compared with that of cells co-transfected with oe-NEAT1 + sh-NC, the expression of IL-18 in cells co-transfected with oe-NEAT1 + sh-p300 downregulated obviously (Fig. 6F). After tail vein injection, the degree of RA was observed and scored. The results demonstrated that compared with that of mice injected with oe-NC + sh-NC, mice injected with oe-NEAT1 + sh-NC presented more severe RA. Compared with that of mice injected with oe-NEAT1 + sh-NC, RA in mice injected with oe-NEAT1 + sh-p300 was relieved (Fig. 6G). In a word, NEAT1 could regulate the expression of IL-18 at the transcription level through p300.
p65 Aggravates RA by Regulating IL-18 Positively
To prove that p65 can indeed affect RA by regulating IL-18, synovial cells from mice were co-transfected with oe-NC + sh-NC, oe-p65 + sh-NC, or oe-p65 + sh-IL-18. The results of RT-qPCR presented that compared with that of cells co-transfected with oe-NC + sh-NC, the expression of NEAT1 increased in cells co-transfected with oe-p65 + sh-NC or oe-p65 + sh-IL-18 (Fig. 7A). Western blot analysis results identified that compared with that of cells co-transfected with oe-NC + sh-NC, the expression of p-p65 and p300 increased in cells co-transfected with oe-p65 + sh-NC or oe-p65 + sh-IL-18 (Fig. 7B). ELISA illustrated that compared with that of cells co-transfected with oe-NC + sh-NC, the IL-18 expression increased in cells co-transfected with oe-p65 + sh-NC. Compared with that of cells co-transfected with oe-p65 + sh-NC, the IL-18 expression declined in cells co-transfected with oe-p65 + sh-IL-18 (Fig. 7C).
The progression of RA is regulated by p65 through IL-18. A The expression of NEAT1 in synovial cells from mice after different treatment determined by RT-qPCR (n = 15). B The expression of p-p65, p65, and p300 in synovial cells from mice after different treatment determined by Western blot analysis (n = 15). C The expression of IL-18 in synovial cells from mice after different treatment determined by ELISA (n = 15). D The degree of RA of CIA mice injected with different viruses in the tail vein (n = 15). E The CD4+ T cells in mice after different treatment detected by IHC staining (n = 15). F The F4/80+ macrophages in mice after different treatment detected by IHC staining (n = 15).*p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Measurement data were expressed as mean ± standard deviation. Comparisons among multiple groups were performed using one-way ANOVA with Tukey’s post hoc test. Comparison among multiple groups at different time points was performed by repeated measures ANOVA with Tukey’s post hoc test. The experiments were repeated three times.
The results of in vivo experiments uncovered that compared with that of mice injected with oe-NC + sh-NC, RA of mice after co-transfection of oe-p65 + sh-NC became more severe. Compared with that of mice injected with oe-p65 + sh-NC, RA in mice injected with oe-p65 + sh-IL-18 was relieved (Fig. 7D). IHC staining revealed that the infiltration of CD4+ T cells and F4/80+ macrophages became more severe in mice after transfection of oe-p65 + sh-NC than that of mice co-transfected with oe-NC + sh-NC. Compared with that of cells co-transfected with oe-p65 + sh-NC, CD4+ T cells and F4/80+ macrophages infiltrated in mice co-transfected with oe-p65 + sh-IL-18 were relieved (Fig. 7E and F).
DISCUSSION
RA is a chronic disease affecting several joints of the body and resulting in foot or ankle pain in 90% of patients with RA [19]. Although the clinical outcomes of RA have been improved in the past two decades, treatment for RA was still impeded by delayed diagnosis, problematic access to specialists, and difficulties adhering to treat-to-target principles [20, 21]. Mounting evidence has continued to highlight the significance of lncRNAs in RA as potential therapeutic targets [22]. Hence, the current study investigated the roles of NEAT1 in the progression of RA through well-designed experiments and subsequently concluded that NEAT1 was positively mediated by p-p65 to elevate the expression of IL-18 through p300/CBP upregulation, which ultimately aggravated RA.
Initially, a key finding of our study indicated NEAT1 was upregulated in synovial tissues of patients with RA and NEAT1 silencing reduced inflammation in synovial tissues and serum of CIA mice and ultimately attenuated RA severity. Similar results have been presented in another study in which NEAT1 was highly expressed in osteoarthritis tissues and its downregulation repressed osteopontin expression, the renowned mediator of inflammatory factors related to osteoarthritis pathogenesis, representing an efficient solution for osteoarthritis treatment [23]. More importantly, additional research demonstrated that NEAT1 also presents a high expression in peripheral blood mononuclear cells, and Th17 cells in vitro induced from CD4+ T cells of patients with RA and NEAT1 knockdown relieved the degree of RA [11]. In a word, NEAT1 silencing serves as a suppressor for RA development.
In subsequent experiments, the effects involved the regulation mechanism of NEAT1 in RA were explored, and results demonstrated that NEAT1 was increased by NF-κB p-p65, and it is then able to elevate the expression of IL-18 through p300/CBP upregulation, thereby exerting an aggravated role for RA progression. p65, as the crucial subunit of NF-κB, is responsible for the regulation of the transcription of multiple inflammatory and immune-related genes [24]. Besides, a prior study revealed that NEAT1 expression is positively regulated by p65 in lung cancer cells, and the decrease of p65-activated NEAT1 expression is a potential strategy of lung cancer treatment [25]. Meanwhile, p-p65 downregulation is a solution for RA improvement [26]. p300 and its paralog CBP are pleiotropic lysine acetyl transferases, which act as key transcriptional co-activators that are vital for cellular processes and gene transcription [27, 28]. The connection between NEAT1 and p300/CBP has been discussed in previous study, which has indicated that NEAT1 is related to p300/CBP complex and further affect Alzheimer’s disease progression [18]. In addition, p300/CBP was reported to be repressed by delphinidin, which can also reduce p65 acetylation in RA synovial cells, representing a useful strategy to prevent inflammatory arthritis [29]. IL-18 is a member of the superfamily of IL-1 protein [30]. Previous researches have confirmed that IL-18 presented an abnormally high expression in synovial tissues and synovial fluids of patients with RA and was regarded as a key pro-inflammatory cytokine whose suppression exerted an alleviating role in RA [17, 31, 32]. Furthermore, it was uncovered that IL-18 p1 promoter activity can be enhanced by p300 and show dose dependence [33]. To sum up, knockdown of NF-κB p-p65-mediated NEAT1 relieved RA by decreasing IL-18 through p300/CBP downregulation.
Taken together, the findings confirmed that NEAT1 expression was increased by NF-κB p-p65, and NEAT1 can further elevate p300/CBP/IL-18 expression, which ultimately aggravated RA (Fig. 8). Thus, in accordance with the evidence presented, it is proposed that NEAT1 knockdown may have therapeutic implications. However, this is a relatively new field of research, and more studies and additional research areas are required to establish enhanced treatment methods for patients with RA. Nevertheless, the current study provides a platform for a better understanding of the mechanisms of RA progression.
Availability of Data and Material
The data sets generated/analyzed during the current study are available.
References
Littlejohn, E.A., and S.U. Monrad. 2018. Early diagnosis and treatment of rheumatoid arthritis. Primary Care 45 (2): 237–255.
Hoxha, M. 2018. A systematic review on the role of eicosanoid pathways in rheumatoid arthritis. Advances in Medical Sciences 63 (1): 22–29.
Wasserman, A. 2018. Rheumatoid arthritis: Common questions about diagnosis and management. American Family Physician 97 (7): 455–462.
Fatel, E.C.S., F.T. Rosa, A.N.C. Simao, and I. Dichi. 2018. Adipokines in rheumatoid arthritis. Adv. Rheumatol 58 (1): 25.
Miranda, J.P., S.P. Camoes, M.M. Gaspar, J.S. Rodrigues, M. Carvalheiro, R.N. Barcia, P. Cruz, H. Cruz, S. Simoes, and J.M. Santos. 2019. The secretome derived from 3D-cultured umbilical cord tissue Mscs counteracts manifestations typifying rheumatoid arthritis. Frontiers in Immunology 10: 18.
Giannini, D., M. Antonucci, F. Petrelli, S. Bilia, A. Alunno, and I. Puxeddu. 2020. One year in review 2020: Pathogenesis of rheumatoid arthritis. Clinical and Experimental Rheumatology 38 (3): 387–397.
Puvvula, P. K. 2019. LncRNAs Regulatory Networks in Cellular Senescence. Int J Mol Sci 20 (11).
Yuan, M., S. Wang, L. Yu, B. Qu, L. Xu, L. Liu, H. Sun, C. Li, Y. Shi, and H. Liu. 2017. Long noncoding RNA profiling revealed differentially expressed lncRNAs associated with disease activity in PBMCs from patients with rheumatoid arthritis. PLoS One 12 (11): e0186795.
Zhang, Y., Y.Z. Xu, N. Sun, J.H. Liu, F.F. Chen, X.L. Guan, A. Li, F. Wang, Q.F. Zhao, H.Y. Wang, S.S. Song, W. Yu, J.N. Zhao, and X.J. Li. 2016. Long noncoding RNA expression profile in fibroblast-like synoviocytes from patients with rheumatoid arthritis. Arthritis Research & Therapy 18 (1): 227.
Bi, X., X.H. Guo, B.Y. Mo, M.L. Wang, X.Q. Luo, Y.X. Chen, F. Liu, N. Olsen, Y.F. Pan, and S.G. Zheng. 2019. LncRNA PICSAR promotes cell proliferation, migration and invasion of fibroblast-like synoviocytes by sponging miRNA-4701-5p in rheumatoid arthritis. eBioMedicine 50: 408–420.
Shui, X., S. Chen, J. Lin, J. Kong, C. Zhou, and J. Wu. 2019. Knockdown of lncRNA NEAT1 inhibits Th17/CD4(+) T cell differentiation through reducing the STAT3 protein level. Journal of Cellular Physiology 234 (12): 22477–22484.
Liu, R., Z. Zhang, H. Yang, K. Zhou, M. Geng, W. Zhou, M. Zhang, X. Huang, and Y. Li. 2019. Design, synthesis, and biological evaluation of a new class of histone acetyltransferase p300 inhibitors. European Journal of Medicinal Chemistry 180: 171–190.
Duval, R., L. Fritsch, L.C. Bui, J. Berthelet, F. Guidez, C. Mathieu, J.M. Dupret, C. Chomienne, S. Ait-Si-Ali, and F. Rodrigues-Lima. 2015. An acetyltransferase assay for CREB-binding protein based on reverse phase-ultra-fast liquid chromatography of fluorescent histone H3 peptides. Analytical Biochemistry 486: 35–37.
Zhang, F.C., Z.Y. Sun, L.P. Liao, Y. Zuo, D. Zhang, J. Wang, Y.T. Chen, S.H. Xiao, H. Jiang, T. Lu, P. Xu, L.Y. Yue, D.H. Du, H. Zhang, C.P. Liu, and C. Luo. 2020. Discovery of novel CBP bromodomain inhibitors through TR-FRET-based high-throughput screening. Acta Pharmacologica Sinica 41 (2): 286–292.
Yoshida, K., A. Nakai, K. Kaneshiro, N. Hashimoto, K. Suzuki, K. Uchida, T. Hashimoto, Y. Kawasaki, K. Tateishi, N. Nakagawa, N. Shibanuma, Y. Sakai, and A. Hashiramoto. 2018. TNF-alpha induces expression of the circadian clock gene Bmal1 via dual calcium-dependent pathways in rheumatoid synovial cells. Biochemical and Biophysical Research Communications 495 (2): 1675–1680.
Wawrocki, S., M. Druszczynska, M. Kowalewicz-Kulbat, and W. Rudnicka. 2016. Interleukin 18 (IL-18) as a target for immune intervention. Acta Biochimica Polonica 63 (1): 59–63.
Nozaki, Y., J. Ri, K. Sakai, K. Niki, K. Kinoshita, M. Funauchi, and I. Matsumura. 2019. Inhibition of the IL-18 receptor signaling pathway ameliorates disease in a murine model of rheumatoid arthritis. Cells 9 (1).
Wang, Z., Y. Zhao, N. Xu, S. Zhang, S. Wang, Y. Mao, Y. Zhu, B. Li, Y. Jiang, Y. Tan, W. Xie, B.B. Yang, and Y. Zhang. 2019. NEAT1 regulates neuroglial cell mediating Abeta clearance via the epigenetic regulation of endocytosis-related genes expression. Cellular and Molecular Life Sciences 76 (15): 3005–3018.
Jastifer, J.R., and A. Green. 2017. Gastrocnemius contracture in patients with rheumatoid arthritis. Foot and Ankle International 38 (12): 1362–1366.
McInnes, I.B., and G. Schett. 2017. Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet 389 (10086): 2328–2337.
Burmester, G.R., and J.E. Pope. 2017. Novel treatment strategies in rheumatoid arthritis. Lancet 389 (10086): 2338–2348.
Jiang, H., X.J. Qin, W.P. Li, R. Ma, T. Wang, and Z.Q. Li. 2016. LncRNAs expression in adjuvant-induced arthritis rats reveals the potential role of LncRNAs contributing to rheumatoid arthritis pathogenesis. Gene 593 (1): 131–142.
Wang, Q., W. Wang, F. Zhang, Y. Deng, and Z. Long. 2017. NEAT1/miR-181c Regulates osteopontin (OPN)-mediated synoviocyte proliferation in osteoarthritis. Journal of Cellular Biochemistry 118 (11): 3775–3784.
Wang, H., Y. Zhu, X. Xu, X. Wang, Q. Hou, Q. Xu, Z. Sun, Y. Mi, and C. Hu. 2016. Ctenopharyngodon idella NF-kappaB subunit p65 modulates the transcription of IkappaBalpha in CIK cells. Fish & Shellfish Immunology 54: 564–572.
Zhou, W., X. Chen, Q. Hu, X. Chen, Y. Chen, and L. Huang. 2018. Galectin-3 activates TLR4/NF-kappaB signaling to promote lung adenocarcinoma cell proliferation through activating lncRNA-NEAT1 expression. BMC Cancer 18 (1): 580.
Ji, Y. R., Y. Chen, Y. N. Chen, G. L. Qiu, J. G. Wen, Y. Zheng, X. F. Li, H. Cheng, Y. H. Li, and J. Li. 2020. Dexmedetomidine inhibits the invasion, migration, and inflammation of rheumatoid arthritis fibroblast-like synoviocytes by reducing the expression of NLRC5. Int Immunopharmacol 82: 106374.
Zhang, Z. R., and N. Yang. 2020. MiR-33a-5p inhibits the growth and metastasis of melanoma cells by targeting SNAI2. Neoplasma.
Wu, F., Y. Hua, S. Kaochar, S. Nie, Y.L. Lin, Y. Yao, J. Wu, X. Wu, X. Fu, R. Schiff, C.M. Davis, M. Robertson, E.A. Ehli, C. Coarfa, N. Mitsiades, and Y. Song. 2020. Discovery, structure-activity relationship, and biological activity of histone-competitive inhibitors of histone acetyltransferases P300/CBP. Journal of Medicinal Chemistry 63 (9): 4716–4731.
Seong, A.R., J.Y. Yoo, K. Choi, M.H. Lee, Y.H. Lee, J. Lee, W. Jun, S. Kim, and H.G. Yoon. 2011. Delphinidin, a specific inhibitor of histone acetyltransferase, suppresses inflammatory signaling via prevention of NF-kappaB acetylation in fibroblast-like synoviocyte MH7A cells. Biochemical and Biophysical Research Communications 410 (3): 581–586.
Yadav, B.S., N. Chaturvedi, P.K. Yadav, N. Marina, M. Ganash, G.E. Barreto, G.M. Ashraf, K. Ahmad, and M.H. Baig. 2019. Protein modeling, molecular network and molecular dynamics study of newly sequenced interleukin-18 (IL-18) gene in Mus musculus. Journal of Cellular Physiology 234 (8): 14285–14295.
Volin, M.V., and A.E. Koch. 2011. Interleukin-18: A mediator of inflammation and angiogenesis in rheumatoid arthritis. Journal of Interferon and Cytokine Research 31 (10): 745–751.
Khalid, S., M.J. Yousaf, A. Rashid, and S.A. Khan. 2019. Gene expression of Interleukin-18 in rheumatoid arthritis patients on disease modifying anti-rheumatic drug therapy. Pak J Med Sci 35 (3): 802–806.
Sun, H., J. Lu, X. Xu, S. Jin, X. Wang, L. Wei, M. Dong, and B. Huang. 2005. Histone acetyltransferase activity of p300 enhances the activation of IL-18 promoter. Journal of Cellular Biochemistry 94 (3): 566–572.
Funding
This study was supported by the General Projects of the Natural Science Foundation of Provincial Science and Technology Department in 2020 (no. 2020JM-702).
Author information
Authors and Affiliations
Contributions
Tuanmao Guo and Yanli Xing designed the study. Zhongning Chen collected the data. Haiyun Zhu carried out the data analyses. Lan Yang produced the initial draft of the manuscript. Yuan Xiao and Jiang Xu contributed to drafting the manuscript. All authors have read and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The current study was performed with the approval of the ethics committee of Xianyang Central Hospital and conformed to the Declaration of Helsinki. Written informed consent was obtained from each participant. All animal experiments were performed in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health.
Consent for Publication
Not applicable.
Competing Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Guo, T., Xing, Y., Chen, Z. et al. Long Non-Coding RNA NEAT1 Knockdown Alleviates Rheumatoid Arthritis by Reducing IL-18 through p300/CBP Repression. Inflammation 45, 100–115 (2022). https://doi.org/10.1007/s10753-021-01531-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-021-01531-x