Abstract
Rheumatoid arthritis (RA) is a highly relevant public health problem. RA fibroblast-like synoviocytes (RAFLSs) play an important role in RA progression. Long non-coding RNA growth arrest-specific transcript 5 (GAS5) could improve RA by inducing RAFLSs apoptosis. However, the mechanism of GAS5 in RA remains unclear. RT-qPCR detected the expressions of GAS5, microRNA-128-3p (miR-128-3p), and histone deacetylase 4 (HDAC4) in RA synovial tissues and RAFLSs. Proliferation, apoptosis, migration, and invasion were measured by Cell Counting Kit-8 assay (CCK-8), flow cytometry, and transwell assays, severally. The protein levels of B-cell lymphoma-2 (Bcl-2), C-caspase 3, Bcl-2 related X protein (Bax), Tumor Necrosis factor-α (TNF-α), Interleukin 6 (IL-6), Interleukin 17 (IL-17), HDAC4, phosphorylation-protein kinase B (p-AKT), AKT, a phosphorylation-mechanistic target of rapamycin (p-mTOR), and mTOR were assessed by western blot assay. The interaction between miR-128-3p and GAS5 or HDAC4 was predicted by ENCORI or TargetScan Human and verified by the dual-luciferase reporter, RNA Immunoprecipitation (RIP), and RNA pull-down assays. GAS5 and HDAC4 were downregulated, and miR-128-3p was upregulated in RA synovial tissues and RAFLSs. Function analysis indicated that GAS5 curbed proliferation, migration, invasion, inflammation, and facilitated apoptosis of RAFLSs. Rescue assay confirmed that miR-128-3p overexpression or HDAC4 knockdown weakened the inhibitory effect of GAS5 or anti-miR-128-3p on RA development. GAS5 acted as a miR-128-3p sponge to upregulate HDAC4 expression. Besides, GAS5/miR-128-3p/HDAC4 axis regulated RA progression partially through the AKT/mTOR pathway. Our studies disclosed that GAS5 restrained inflammation in synovial tissue partly through regulating HDAC4 via miR-128-3p, suggesting a potential lncRNA-targeted therapy for RA treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA), a chronic autoimmune disease, is characterized by joint damage caused by an immune-inflammatory response, which can lead to joint dysfunction and persistent synovitis [1]. With the rapid increase in incidence, RA has become a highly relevant public health problem [2]. Although environmental, immunological, and genetic factors have been identified as the major triggers, RA’s definite etiology of RA remains unclear. Currently, numerous reporters have confirmed that RA fibroblast-like synoviocytes (RAFLSs), a class of mesenchymal cells of synovial joint, are closely related to the progression of RA [3]. Meanwhile, numerous reporters have confirmed that RAFLSs activity could activate pro-inflammatory pathways, promoting the development of RA [4]. Therefore, suppression of RAFLSs proliferation and promotion of apoptosis might be an effective therapeutic method for RA treatment.
In the recent years, long non-coding RNAs (lncRNAs) are defined as non-coding transcripts consisting of longer than 200 nucleotides (nts), which participated in the regulation of the formation and development in multiple diseases, including RA [5]. Growth arrest-specific transcript 5 (GAS5), a tumor-suppressive lncRNA, has been reported to play a pivotal role in diverse human diseases [6,7,8]. A recent study confirmed that GAS5 was decreased in RA, and overexpression of GAS5 could improve RA by promoting RAFLSs apoptosis [9]. Hence, exploring the molecular mechanism of GAS5 is urgent for RA treatment.
MicroRNAs (miRNAs), which refer to non-coding RNAs with approximately 22 nts, could exert the negative regulation of gene expression through suppressing protein translation [10]. A growing number of research studies have confirmed that miRNAs play crucial mediators in physiological and cellular processes, such as proliferation, apoptosis, immune response, and signaling transduction [11,12,13]. In a recent publication, Xia et al. reported that miR-128-3p knockdown could repress RA progression by inhibiting the inflammation response [14]. However, the regulatory mechanism of miR-128-3p involved in RA is still further exploration.
Histone deacetylase 4 (HDAC4), an epigenetic modifier enzyme, has been implicated in tumorigenesis and inflammatory response regulation [15, 16]. Interestingly, the recent literature has proved that HDAC4 could exert the inhibitory effect by hindering RA-related inflammatory cytokine expression in the progression of RAFLSs [17], suggesting the vital function of HDAC4 in RA development.
Herein, our results discovered that GAS5 suppressed the growth, metastasis, and inflammation of RAFLSs in RA. Moreover, GAS5 could upregulate HDAC4 expression by interacting with miR-128-3p; thereby, restraining RA development. Our findings first provided the evidence for the GAS5/miR-128-3p/HDAC4 axis, promising an underlying target for RA patients.
Materials and methods
Clinical samples and cell culture
RA synovial tissues from 40 RA patients (23 males and 17 females, 30–62 years, 47.3 ± 6.8 years) were collected during total knee replacement surgery, and normal synovial tissues from 20 non-RA patients s (12 males and 8 females, 28–64 years, 43.7 ± 7.6 years) were provided by the emergency amputation surgery at Shandong Otolaryngology Hospital from January 2016 to July 2018. Inclusion criteria of the patient group: (1) no history of malignancies; (2) no therapies received within 3 months before admission; (3) first time diagnosis. Exclusion criteria: (1) patients have other rheumatic diseases, autoimmune diseases, tumors, liver and kidney insufficiency, pregnancy or lactation, and mental disorders; (2) patients without complete medical records. The approval of the ethics committee was permitted by the Shandong Otolaryngology Hospital in this study. Written informed consent was obtained from each participant.
RA fibroblast-like synoviocytes (RAFLSs) and normal synovial cells were separated and cultured in accordance with the previous description [18]. In brief, synovial tissues (RA sample and normal sample) were washed with sterile phosphate-buffered saline (PBS, Solarbio, Beijing, China) and minced, then digested at 37˚C for 4 h with collagenase type I (1 mg/mL, Gibco, Carlsbad, CA, USA). The primary RAFLSs cells were in fusiform with oval nuclei located in the center by morphological observation. The obtained cells were maintained in a humidified atmosphere containing 5% CO2 at 37˚C with Dulbecco’s modified Eagle medium (DMEM, Gibco) containing 10% fetal bovine serum (FBS, Invitrogen Carlsbad, CA, USA), 1% penicillin/streptomycin (Gibco). RAFLSs of passages 3–8 were used for all experiments.
Cell transfection
For the overexpression of GAS5, the pcDNA 3.1 vector (pcDNA, Addgene, Inc., Cambridge, MA, USA) possessing the sequence of GAS5 were acquired from RiboBio (Guangzhou, China), termed as pcDNA 3.1-GAS5 (pcDNA-GAS5) and the pcDNA 3.1 empty vector as the negative control (pcDNA-NC). GAS5 small interference RNA (si-GAS5) and its negative control (si-NC), miR-128-3pmimic and its negative control (NC), miR-128-3p inhibitor (anti-miR-128-3p), and its negative control (anti-NC), HDAC4 small interference RNA (si-HDAC4) and its negative control (scramble) were collected from GenePharma (Shanghai, China). Cells were transfected with the indicated oligonucleotide and vector using Lipofectamine 3000 reagents (Invitrogen) referring to the supplier’s direction.
Real-time quantitative polymerase chain reaction (RT-qPCR)
In line with the operation manual of TRIzol (Invitrogen) and the treatment of proteinase K at 55℃ for 15 min, total RNA from synovial tissues and cells was extracted. For GAS5 and HDAC4 mRNA detection, complementary DNA (cDNA) was synthesized with PrimeScript™ RT Master Mix Kit (Takara, Tokyo, Japan), and RT-qPCR was implemented using an SYBR® PremixEx Taq™ reagent (TaKaRa) following the user’s guidebook. For miR-128-3p detection, reverse transcription was performed by a MicroRNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA), and RT-qPCR was carried out with All-in-One™ miRNA RT-qPCR Detection Kit (GeneCopoeia, Guangzhou, China). Subsequently, the fluorescence was conducted on a LightCycler 480 System II (Roche Life Science, Indianapolis, IN, USA). Genes levels were calculated according to 2–Ct method, normalizing to glyceraldehyde-3-phosphate dehydrogenase (GAPDH; for GAS5 and HDAC4) and U6 small nuclear RNA (for miR-128-3p). The specific primers were exhibited as follows:
GAS5: 5′-CCATGGATGACTTGCTTGG-3′ (sense), 5′-GCATGCTTGCTTGTTGTGG-3′ (antisense);
miR-128-3p: 5′-GGTCACAGTGAACCGGTC-3′ (sense), 5′-GTGCAGGGTCCGAGGT-3′ (antisense);
HDAC4: 5′-AGGCTCAGACTTGCGAGAAC-3′ (sense), 5′-ATGGGCTCCTCATCTGGTCT-3′ (antisense);
U6: 5′-CTCGCTTCGGCAGCACA-3′ (sense), 5′-AACGCTTCACGAATTTGCGT-3′ (antisense);
GAPDH: 5′-TGGCCTTCCGTGTTCCTAC-3′ (sense), 5′-GAGTTGCTGTTGAAGTCGCA-3′ (antisense).
Immunohistochemistry
Immunohistochemical staining was performed as previously described [19], with antibodies specific for tumor necrosis factor-α (TNF-α, 1 µg/mL, ab66579, Abcam, Cambridge, MA, USA), Interleukin 6 (IL-6, 1:50, ab233706, Abcam), Interleukin 17 (IL-17, 5 µg/mL, ab79056, Abcam). The immunoreactivity in each tissue section was assessed by at least two pathologists.
Cell viability assay
Cell Counting Kit-8 assay (CCK-8, Dojindo Laboratories, Kumamoto, Japan) was performed to measure cell proliferation based on the supplier’s direction. Generally, transfected RAFLSs (6 × 103 cells per well) were incubated for 0 h, 24 h, 48 h, and 72 h, then 10µL CCK-8 solution (Dojindo Laboratories) was added per well, followed by incubation at 37 C for another 2 h. At last, the absorbance was examined under a microplate reader as per the instruction guidelines.
Cell apoptosis assay
Annexin (V-fluorescein isothiocyanate) V-FITC/Propidium Iodide (PI) (Solarbio) was applied to analyze the apoptosis rate of RAFLSs according to the instruction guidelines. In this assay, transfected RAFLSs were collected and resuspended in binding buffer, and then Annexin V-FITC/PI (Solarbio) was used for staining these RAFLSs for 15 min in the dark. Finally, RAFLSs apoptosis was detected with a FACScan flow cytometer (BD Bioscience, San Jose, CA, USA).
Western blot assay
Briefly, the tissues or cells of each group were ice-bathed for 30 min with the lysis buffer supplemented with phenylmethyl sulfonylfluoride, followed by centrifugation at 4℃ for 15 min at 10,000 rpm. And then, these tissue and cell extracts were loaded and isolated with 10% sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE), transferred onto polyvinylidene fluoride (PVDF) membranes (Millipore, Bedford, MA, USA), and followed by incubation with primary antibodies against B-cell lymphoma-2 (Bcl-2, 1:1000, ab32124, Abcam), C-caspase 3 (1:1000, ab4051, Abcam), Bcl-2 related X protein (Bax, 1:1000, ab7888, Abcam), TNF-α(1:500, ab66579, Abcam), IL-6(1:1000, ab6672, Abcam), IL-17(1:1000, ab79056, Abcam), HDAC4 (1:1000, ab12172, Abcam), phosphorylation–protein kinase B (p-AKT, 1:1000, ab131443, Abcam), AKT (1:1000, ab179463, Abcam), phosphorylation-mechanistic target of rapamycin (p-mTOR, 1:1000, ab32028, Abcam), mTOR (1:1000, ab109268, Abcam) and GAPDH (1:2000, ab9485, Abcam) overnight 4℃. Whereafter, horseradish peroxidase (HRP)-conjugated secondary antibodies were incubated onto these membranes, and protein bands were analyzed with enhanced chemiluminescence (ECL, Amersham Biosciences, Pittsburg, PA, Sweden).
Cell migration and invasion assay
For migration assay, transfected RAFLSs (5 × 104 cells/well) in serum-free DMEM medium was introduced into the upper chambers of Transwell (24-well, Corning Incorporated, Corning, NY, USA). For invasion assay, RAFLSs (1 × 105 cells/well) were added into the upper chambers treated with Matrigel (BD Biosciences). In both assays, the complete medium as a chemotactic agent was added to the lower chambers. After 24 h incubation, cotton swabs were used to scrape, and these non-migratory and noninvasive RAFLSs insides the upper chamber, while methanol and crystal violet were applied to fix and stain these migrated and invaded RAFLSs insides the lower chamber. Finally, the staining cells were photographed with an inverted microscope.
Dual-luciferase reporter assay
Based on the online prediction software ENCORI starBase (http://starbase.sysu.edu.cn) or TargetScan (www.targetscan.org), the binding sites between miR-128-3p and GAS5 or HDAC4 were predicted, as proved by dual-luciferase reporter assays. In short, GAS5-wt/mut and HDAC4-wt/mut were constructed through amplifying and subcloning their sequences into psiCHECK vectors (Sangon Biotech Co., Ltd., Shanghai, China). And then, RAFLSs were transfected with the constructed reporter plasmids and miR-128-3p or NC, severally. At 48 h after transfection, a dual-luciferase reporter assay kit (Promega, Madison, WI, USA) was used for the detection of luciferase activity. Relative firefly luciferase levels were normalized to the corresponding renilla luciferase internal control.
RNA immunoprecipitation (RIP) assay
In this assay, referring to the producer’s protocol, a Magna RIP kit (Millipore) was applied to verify the underlying binding between miR-128-3p and GAS5 or HDAC4.In brief, transfected RAFLSs were collected and lysed in a complete RIP lysis buffer. Subsequently, these cell extracts were incubated with RIP buffer containing magnetic beads connected with anti-Argonaute2 (Ago2, Millipore) or anti-immunoglobulin G (IgG, Millipore) as a negative control. After digesting with proteinase K, the enrichment levels of GAS5, HDAC4 and miR-128-3p were tested by RT-qPCR in immunoprecipitated RNA.
RNA pull-down assay
Biotinylated NC (Bio-NC) and miR-128-3p (Bio-miR-128-3p) were transfected into RAFLSs with Lipofectamine RNAiMax reagent (Invitrogen). Then, cells were lysed in radioimmunoprecipitation buffer (RIPA; Beyotime, Shanghai, China), followed by incubation with Dynabeads M-270 streptavidin (Invitrogen). At last, the eluted RNA was detected with RT-qPCR assay.
Statistical analysis
Statistical analysis was analyzed with GraphPad Prism7.0 software and presented as mean ± standard deviation (SD). The expression correlation of GAS5, miR-128-3p, or HDAC4 was detected using Pearson’s correlation analysis. Statistical significance of differences was evaluated using the Mann–Whitney U test, Student’s t test, or one-way of variance (ANOVA). Statistical significance was considered as P values less than 0.05.
Results
GAS5 suppressed growth, migration, invasion, and inflammation of RAFLSs in vitro
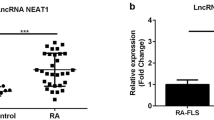
To investigate the function of GAS5, its expression was first assessed using RT-qPCR assay. The data showed that the GAS5 level was obviously downregulated in RA synovial tissues (n = 40) relative to Normal synovial tissues (n = 20) (Fig. 1a). Moreover, when compared with normal synovial cells, the expression of GAS5 was strikingly decreased in RAFLSs (Fig. 1b). According to the previous study [20], the transcription factor NF-κB acted as a pivotal mediator of inflammatory responses, which could induce the expression of various pro-inflammatory genes and participate in the inflammasome regulation. Meanwhile, the phosphorylation of p65 led to the NF-κB activation during target cell recognition [21]. Western blot assay exhibited that the p-p65/p65 protein level was increased in RA synovial tissues and cells with respect to their respective controls (Figure S1), implying the activation of the NF-κB signal pathway in RA. Meanwhile, immunohistochemical staining presented the upregulation of inflammatory cytokines (TNF-α, IL-6, and IL-17) in RA synovial tissues relative to normal synovial tissues (Fig. 1c), further suggesting the inflammation response in RA synovial tissues. Considering the lower expression of GAS5 in RAFLSs, we over-expressed GAS5 in RAFLSs. The results displayed that GAS5 expression was significantly increased in pcDNA-GAS5-transfected RAFLSs (Fig. 1d). Then, the functional analysis suggested that the overexpression of GAS5 markedly inhibited proliferation (Fig. 1e), migration (Fig. 1h), invasion (Fig. 1i), and facilitated apoptosis (Fig. 1f) in RAFLSs. To further prove the effect of GAS5 on RAFLSs apoptosis, apoptosis-related factors (Bcl-2, C-caspase 3, and Bax) were detected. As shown in Fig. 1g, decreased Bcl-2 protein level and increased the protein level of C-caspase 3 and Bax further confirmed the promoting function of GAS5 on cell apoptosis in RAFLSs. Besides, we further explored the effect of GAS5 on inflammation of RAFLSs. Western blot assay presented that GAS5 overexpression could reduce the protein level of p-p65/p65 in RAFLSs (Figure S1). Also, the high expression of GAS5 hindered the protein level of TNF-α, IL-6, and IL-17, indicating GAS5 overexpression blocked the inflammation of RAFLSs (Figure S2). These data suggested that GAS5 could inhibit proliferation, migration, invasion, inflammation, and expedite apoptosis of RAFLSs.
GAS5 represses proliferation, migration, invasion, inflammation, and accelerated apoptosis of RAFLSs. a RT-qPCR assay is performed to measure the expression of GAS5 in RA synovial tissues (n = 40) and normal synovial tissues (n = 20). b Relative expression of GAS5 in RAFLSs and normal synovial cells is measured. c The expression of TNF-α, IL-6, and IL-17 was examined by immunohistochemical staining assay. d GAS5 level is examined in pcDNA-GAS5-transfected RAFLSs. e Cell viability in pcDNA-GAS5-transfected RAFLSs is detected by CCK-8 assay. f Apoptosis rates in pcDNA-GAS5-transfected RAFLSs are measured by flow cytometry assay. g The protein levels of Bcl-2, C-caspase 3, and Bax are tested by western blot assay in pcDNA-GAS5-transfected RAFLSs. h and i Migration and invasion are assessed transwell assay in pcDNA-GAS5-transfected RAFLSs. The data were shown as mean ± SD. N = 3, *P < 0.05 vs. Normal synovial tissues, Normal synovial cells, pcDNA-NC
MiR-128-3p served as the target of GAS5
A previous study suggested that miR-128-3p downregulation could weaken RA progression by binding to TNFAIP3 [14]. Therefore, the miR-128-3p level in RA was detected by RT-qPCR assay. As presented in Fig. 2a,b, in comparison with respective control groups, miR-128-3p expression was strikingly upregulated in RA synovial tissues and RAFLSs. Intriguingly, we observed that the miR-128-3p level was inversely related to the GAS5 level in RA synovial tissues (Fig. 2c). Subsequently, we used a web-based tool ENCORI to predict the relationship between miR-128-3p and GAS5 in RAFLSs. As a result, miR-128-3p was found to contain some complementary sequences with GAS5 (Fig. 2d), and then a dual-luciferase reporter assay was performed to confirm the predicted results. The data suggested that miR-128-3p mimics reduced the luciferase activity of the GAS5-wt reporter vector, but not that of the GAS5-mut reporter vector in RAFLSs (Fig. 2e). Moreover, RIP assay was applied to verify the binding between miR-128-3p and GAS5. According to the results exhibited in Fig. 2f, the levels of miR-128-3p and GAS5 were strikingly enriched in the Anti-Ago2 group compared with the Anti-IgG control group, which was consistent with bioinformatics analysis and dual-luciferase reporter assay. What’s more, to further confirm the interaction, RNA pull-down assay was conducted in RAFLSs. The data suggested that GAS5 enrichment was markedly enhanced in Bio-miR-128-3pgroup in contrast to the Bio-NC group (Fig. 2g). In addition, RT-qPCR assay proved that GAS5 overexpression repressed miR-128-3p level, while GAS5 knockdown boosted miR-128-3p expression in RAFLSs (Fig. 2h). Collectively, GAS5 could interact with miR-128-3p to repress its expression.
MiR-128-3p is a direct target of GAS5. a Relative expression of miR-128-3p in RA synovial tissues (n = 40) and normal synovial tissues (n = 20) is detected. b MiR-128-3p level in RAFLSs and normal synovial cells is detected. c In RA synovial tissues, Pearson correlation analysis is utilized to assess the expression association between GAS5 and miR-128-3p. d Binding sites between GAS5 and miR-128-3p are predicted by ENCORI. e Dual-luciferase reporter assay is applied to prove the binding between GAS5 and miR-128-3p in RAFLSs. f RIP assay is carried out in RAFLSs extracts to detect miR-128-3p endogenously associated with GAS5. g RNA pull-down assay is performed to test the interactions between GAS5 and miR-128-3p in RAFLSs. h MiR-128-3p level is assessed in pcDNA-GAS5-transfected or si-GAS5-transfected RAFLSs. The data were shown as mean ± SD. N = 3, *P < 0.05 vs. Normal synovial tissues, Normal synovial cells, NC, Anti-IgG, Bio-NC, pcDNA-NC, or si-NC
MiR-128-3p partially mitigated the effect of GAS5 overexpression on growth, metastasis, and inflammation of RAFLSs in vitro
As mentioned above, we inferred that GAS5 could exert its function by interacting with miR-128-3p in RAFLSs. As exhibited in Fig. 3a, GAS5 overexpression retarded miR-128-3p level, which was remarkably relieved by miR-128-3p mimics in RAFLSs. Functionally, miR-128-3p overexpression abated the negative influence of GAS5 on proliferation (Fig. 3b), migration (Fig. 3e), and invasion (Fig. 3f) in RAFLSs. The promotion of apoptosis rate triggered by GAS5 upregulation was attenuated by a miR-128-3p mimic in RAFLSs (Fig. 3c). Meanwhile, GAS5 upregulation led to an overt decline in Bcl-2 protein level and a prominent increase in C-caspase 3 and Bax levels, while miR-128-3p overexpression drastically recovered these effects (Fig. 3d), supporting the influence of miR-128-3p on GAS5 in RAFLSs apoptosis. Besides, western blot results manifested that re-introduction of miR-128-3p obviously overturned GAS5 overexpression-caused reduction in the protein levels of TNF-α, IL-6, and IL-17, implying that miR-128-3p could apparently undermine the suppression effect of GAS5 on inflammatory response in RAFLSs (Figure S2). All these results demonstrated that miR-128-3p partly attenuated GAS5-mediated proliferation, metastasis, apoptosis, and inflammation of RAFLSs.
MiR-128-3p attenuates the effect of GAS5 on growth, migration, invasion, and inflammation of RAFLSs in vitro. a miR-128-3p level is examined in RAFLSs transfected with pcDNA-NC, pcDNA-GAS5, pcDNA-GAS5 + NC, and pcDNA-GAS5 + miR-128-3p. b CCK-8 assay is used to detect the proliferative ability in transfected RAFLSs c Flow cytometry assay is applied to test the apoptosis rate in transfected RAFLSs. d Western blot assay is conducted to assess the protein levels of Bcl-2, C-caspase 3, and Bax in transfected RAFLSs. e and f Transwell assay is carried out to examine the ability of migration and invasion in transfected RAFLSs. The data were shown as mean ± SD. N = 3, *P < 0.05 vs. pcDNA-NC or pcDNA-GAS5 + NC
HDAC4 was a direct target of miR-128-3p
HDAC4, an epigenetic regulator, has been confirmed to inhibit inflammatory cytokines expression of synoviocytes in RA [17]. Thus, we examined the expression level of HDAC4 by RT-qPCR assay. When compared with normal synovial tissues and normal synovial cells, the HDAC4 level was downregulated in RA synovial tissues and RAFLSs, respectively (Fig. 4a–c). Noteworthily, there existed a negative correlation between HDAC4 and miR-128-3p, and the positive relationship between HDAC4 and GAS5 in RA synovial tissues (Fig. 4d, e). Therefore, the connection between HDAC4 and miR-128-3p was further explored by the bioinformatics analysis. As presented in Fig. 4f, HDAC4 was found to have some putative binding sites with miR-128-3p in RAFLSs. Then, the predicted result was further proved with the dual-luciferase reporter assay. The data suggested that miR-128-3p upregulation effectively repressed the luciferase activity of HDAC4 3′UTR-wt reporter vector, while had little effect on the luciferase activity of HDAC4 3′UTR-mut reporter vector (Fig. 4g). Furthermore, to further demonstrate the binding sites between HDAC4 and miR-128-3p, RIP assay was carried out. In accordance with bioinformatics analysis and dual-luciferase reporter assay, the level of HDAC4 was strikingly elevated in the anti-Ago2 group in contrast to that in the anti-normal IgG group (Fig. 4h). Besides, western blot results manifested that miR-128-3p upregulation curbed the protein level of HDAC4 in RAFLSs, which was effectively recuperated after co-transfection with pcDNA-GAS5 (Fig. 4i), suggesting that GAS5 could regulate HDAC4 expression by interacting with miR-128-3p. All of these data indicated that miR-128-3p directly bound HDAC4.
HDAC4 works as the target of miR-128-3p. a and b HDAC4 level in RA synovial tissues (n = 40) and normal synovial tissues (n = 20) is measured by RT-qPCR assay and western blot assay. (c) HDAC4 protein level in RAFLSs and normal synovial cells is detected by western blot assay. d and e Pearson correlation analysis is implemented to analyze the expression association between HDAC4 and miR-128-3p or GAS5 in RA synovial tissues. f The binding sites between miR-128-3p and HDAC4 3′UTR is predicted by TargetScan Human bioinformatics analysis. g Dual-luciferase reporter assay is used to detect the effect of miR-128-3p overexpression on luciferase activity of HDAC4-wt 3′UTR or HDAC4-mut 3′UTR reporters in RAFLSs. h RIP assay is applied to test the binding between miR-128-3p and HDAC4 3′UTR in RAFLSs. i Western blot assay is performed to examine the protein level of HDAC4 in RAFLSs transfected with NC, miR-128-3p, miR-128-3p + pcDNA and miR-128-3p + pcDNA-GAS5. The data were shown as mean ± SD. N = 3, *P < 0.05 vs. Normal synovial tissues, Normal synovial cells, NC, miR-128-3p + pcDNA, or si-NC
HDAC4 knockdown partially relieved the inhibitory effect of miR-128-3p deletion on the development and inflammation of RAFLSs in vitro
Then, to further identify whether miR-128-3p could exert its performance by regulating HDAC4, rescue experiments were executed in RAFLSs. The results suggested that miR-128-3p knockdown accelerated the HDAC4 level, while the silence of HDAC4 notably receded the effect (Fig. 5a). Moreover, CCK-8 assay and transwell assay presented that the downregulation of miR-128-3p constrained proliferation (Fig. 5b), migration (Fig. 5e), and invasion (Fig. 5f), which were weakened by the repression of HDAC4. Synchronously, the apoptosis rate enhanced by miR-128-3p silencing was inhibited by knockdown of HDAC4 in RAFLSs (Fig. 5c). Similar to the flow cytometry results, the deficiency of miR-128-3p reduced the Bcl-2 protein level and improved the protein levels of C-caspase 3 and Bax, and subsequently, the deletion of HDAC4 reverted these effects (Fig. 5d). In addition, western blot results displayed that HDAC4 knockdown drastically impaired the negative effect of miR-128-3p downregulation on the protein levels of TNF-α, IL-6, and IL-17 in RAFLSs (Figure S1). Collectively, miR-128-3p-triggered proliferation, apoptosis, migration, invasion, and inflammation were overturned by regulating HDAC4 expression.
HDAC4 knockdown mitigates miR-128-3p downregulation-mediated growth, migration, invasion, and inflammation of RAFLSs in vitro. a Protein level of HDAC4 is detected by western blot assay in RAFLSs transfected with anti-NC, anti-miR-128-3p, anti-miR-128-3p + scramble and anti-miR-128-3p + si-HDAC4. b Proliferation in transfected RAFLSs is assessed by CCK-8 assay. c Apoptosis rate in transfected RAFLSs is detected by flow cytometry assay. d The protein levels of Bcl-2, C-caspase 3, and Bax in transfected RAFLSs are tested by western blot assay. e and f Migration and invasion in transfected RAFLSs are measured by transwell assay. The data were shown as mean ± SD. N = 3, *P < 0.05 vs. anti-NC or anti-miR-128-3p + scramble
GAS5/miR-128-3p/HDAC4 axis regulated proliferation, migration, invasion, inflammation, and apoptosis of RAFLSs partly by AKT/mTOR signaling pathway in vitro
Finally, the AKT/mTOR pathway analysis was applied to further explore the impact of the GAS5/miR-128-3p/HDAC4 axis on development and inflammatory response in RAFLSs. As displayed in Fig. 6a, b, GAS5 overexpression or miR-128-3p knockdown induced HDAC4 expression and hindered the protein levels of p-AKT and p-mTOR, and miR-128-3p upregulation or HDAC4 deletion apparently abrogated these effects in RAFLSs. Although the protein levels of AKT and mTOR had no obviously change in all groups (Control, pcDNA-GAS5, pcDNA-GAS5 + miR-128-3p, anti-miR-128-3p, and anti-miR-128-3p + si-HDAC4). Overall, these results indicated that GAS5 overexpression or miR-128-3p silencing could be inactive the AKT/mTOR signaling pathway, and co-transfection of miR-128-3p mimics or si-HDAC4 could re-activate the AKT/mTOR pathway in RAFLSs. In other words, the GAS5/miR-128-3p/HDAC4 axis might affect active synovitis in RA partially through the AKT/mTOR pathway.
GAS5/miR-128-3p/HDAC4 regulates proliferation, migration, invasion, inflammation, and apoptosis of RAFLSs partly by AKT/mTOR signaling pathway in vitro. a Protein levels HDAC4, p-AKT, AKT, p-mTOR, and mTOR are detected by western blot assays in RAFLSs transfected with control, pcDNA-GAS5, pcDNA-GAS5 + miR-128-3p, anti-miR-128-3p, and anti-miR-128-3p + si-HDAC4. b Quantitative analysis of the optical densities of HDAC4 p-AKT/AKT and p-mTOR/mTOR in transfected RAFLSs. The data were shown as mean ± SD. N = 3, *P < 0.05 vs. pcDNA-GAS5 or anti-miR-128-3p
Discussion
In the recent years, increasing evidence suggests that lncRNAs exert vital roles in a variety of biological processes, such as proliferation, metastasis, apoptosis, and inflammation [22,23,24]. Indeed, several documents have proved that the abnormal expression of lncRNAs is closely related to various diseases, including RA [25]. Notably, some reports have presented in RAFLSs, GAS5 expression level was decreased, and the upregulation of GAS5 could impede RA progression [26]. However, the underlying molecular mechanism of GAS5 in RA development is still largely unknown. In this study, GAS5 was identified as a low expression in RA synovial tissues and RAFLSs versus their respective control groups. Functionally, GAS5 blocked proliferation, migration, invasion, inflammatory cytokines expression, and boosted apoptosis of RAFLSs, indicating that GAS5 plays a vital role in RA progression and may be a therapeutic target. In addition, our results also show that more RAFLSs die and divide less, and fewer healthy cells are able to migrate/invade.
It has been widely believed that lncRNAs could exert their function through the interaction with miRNAs [27, 28]. In this paper, miR-128-3p was upregulated in RA synovial tissues and RAFLSs. Intriguingly, there was an inverse relationship between GAS5 and miR-128-3p in RA tissues. Thus, bioinformatics software was utilized to analyze the potential targeting relationship. Whereafter, a dual-luciferase reporter assay, RIP assay and RNA pull-down assay further confirmed the interaction between GAS5 and miR-128-3p in RAFLSs. Furthermore, miR-128-3p has been confirmed to be tightly linked to RA’s inflammation response [14]. In this paper, the functional analysis suggested that the re-introduction of miR-128-3p mitigated the inhibitory effect of GAS5 on RAFLSs. In other words, GAS5 improved RA at least partially by targeting miR-128-3p.
Mounting studies have proved that lncRNAs performed as miRNAs sponges to impact mRNAs expression (29). In our research, HDAC4 was expressed at a low level in both RA synovial tissues and RAFLSs. Meanwhile, HDAC4 expression was opposite with miR-128-3p in RA synovial tissues. Hence, HDAC4 was deemed as the underlying target gene of miR-128-3p through bioinformatics prediction, as confirmed by dual-luciferase reporter assay and RIP assay. Simultaneously, it has been reported that HDAC4 could hinder inflammatory cytokines expression of RAFLSs [17]. In view of the foregoing, we inferred that the role of miR-128-3p on RA progression might be mediated by modulating HDAC4. In this study, the absence of HDAC4 could abrogate the promoting action of miR-128-3p knockdown on RAFLSs apoptosis, while HDAC4 deletion could weaken the suppressive action of miR-128-3p downregulation on growth, metastasis, and inflammation. That was to say, miR-128-3p accelerated the RA development partly through regulating HDAC4. Besides, to further verify whether GAS5 could act as a miR-128-3p sponge to affect HDAC4expression, we also explored the effect of GAS5 on HDAC4 expression in RAFLSs. Expectedly, GAS5 overexpression effectively attenuated the inhibiting effect of miR-128-3p on HDAC4 expression level.
In addition, available literature suggested that AKT/mTOR signaling pathway could participate in proliferation, apoptosis, metastasis, and inflammation [30, 31]. AKT and mTOR were significant factors of the AKT/mTOR pathway. Moreover, the hyperactivation of the mechanistic target of rapamycin complex 1 (mTORC1) could expedite osteoarthritis development by regulating HDAC4 (32). In this study, the re-introduction of miR-128-3p mimics or si-HDAC4 could abate the suppressive function of GAS5 upregulation or miR-128-3p downregulation on the AKT/mTOR signaling pathway. Namely, the regulatory function of GAS5/miR-128-3p/HDAC4 in the inflammation of RA synovial tissue was possibly mediated by the AKT/mTOR signaling pathway. This study is limited by the small sample size and the lack of animal model experiments. Our future studies will try to include more patients and construct RA animal models to further confirm our conclusions. In addition, without a histologic assessment of the included tissues that confirms lymphoplasmacytic inflammation/typical RA features, heterogeneity of tissue samples in the RA cohort is also a potential limitation.
In summary, this study is the first to reveal that GAS5 performed as the miR-128-3p sponge to upregulate HDAC4 expression; thus, hampering RA progression. Our results confirmed that GAS5 can be used as a diagnostic biomarker and potential target in RA therapy. Meanwhile, these findings expounded an underlying regulatory mechanism of GAS5 in synovial tissue inflammation, providing a better understanding of the function of lncRNAs in RA pathogenesis and feasible therapeutic targets for clinical use.
References
Meier FM, Frerix M, Hermann W, Muller-Ladner U (2013) Current immunotherapy in rheumatoid arthritis. Immunotherapy 5(9):955–974
Minichiello E, Semerano L, Boissier MC (2016) Time trends in the incidence, prevalence, and severity of rheumatoid arthritis: A systematic literature review. Joint Bone Spine 83(6):625–630
Wu J, Qu Y, Zhang YP, Deng JX, Yu QH (2018) RHAMM induces progression of rheumatoid arthritis by enhancing the functions of fibroblast-like synoviocytes. BMC Musculoskelet 19(1):455
Neumann E, Lefevre S, Zimmermann B, Gay S, Muller-Ladner U (2010) Rheumatoid arthritis progression mediated by activated synovial fibroblasts. Trends Mol Med 16(10):458–468
Li Z, Li X, Jiang C, Qian W, Tse G, Chan MTV, Wu WKK (2018) Long non-coding RNAs in rheumatoid arthritis. Cell Prolif. https://doi.org/10.1111/cpr.12404
Cao Q, Wang N, Qi J, Gu Z, Shen H (2016) Long noncoding RNAGAS5 acts as a tumor suppressor in bladder transitional cell carcinoma via regulation of chemokine (CC motif) ligand 1 expression. Mol Med Rep 13(1):27–34
Shen S, Zheng X, Zhu Z, Zhao S, Zhou Q, Song Z, Wang G, Wang Z (2019) Silencing of GAS5 represses the malignant progression of atherosclerosis through upregulation of miR-135a. Biomed Pharmacother. https://doi.org/10.1016/j.biopha.2019.109302
Liu SD, Meng WX, Xu L, Chi C, Sun X, Liu HY (2018) GAS5 promotes myocardial apoptosis in myocardial ischemia-reperfusion injury via upregulating LAS1 expression. Eur Rev Med Pharmacol Sci 22(23):8447–8453
Ma C, Wang W, Li P (2019) LncRNA GAS5 overexpression downregulates IL-18 and induces the apoptosis of fibroblast-like synoviocytes. Clin Rheumatol 38(11):3275–3280
Bartel DP (2009) MicroRNAs: target recognition and regulatory functions. Cell 136(2):215–233
Zhang Y, Xu S, Huang E, Zhou H, Li B, Shao C, Yang Y (2018) MicroRNA-130a regulates chondrocyte proliferation and alleviates osteoarthritis through PTEN/PI3K/Akt signaling pathway. Int J Mol Med 41(6):3699–3708
Zhou Y, Li S, Chen P, Yang B, Yang J, Liu R, Li J, Xia D (2019) MicroRNA-27b-3p inhibits apoptosis of chondrocyte in rheumatoid arthritis by targeting HIPK2. Artif Cells Nanomed Biotechnol 47(1):1766–1771
Alivernini S, Gremese E, McSharry C, Tolusso B, Ferraccioli G, McInnes IB, Kurowska-Stolarska M (2017) MicroRNA-155-at the Critical Interface of Innate and Adaptive Immunity in Arthritis. Front Immunol. https://doi.org/10.3389/fimmu.2017.01932
Xia Z, Meng F, Liu Y, Fang Y, Wu X, Zhang C, Liu D, Li G (2018) Decreased MiR-128–3p alleviates the progression of rheumatoid arthritis by up-regulating the expression of TNFAIP3. Biosci Rep. https://doi.org/10.1042/BSR20180540
Lu Y, Li Z, Xie B, Song Y, Ye X, Liu P (2019) hsa-miR-20a-5p attenuates allergic inflammation in HMC-1 cells by targeting HDAC4. Mol Immunol 107:84–90
Cai JY, Xu TT, Wang Y, Chang JJ, Li J, Chen XY, Chen X, Yin YF, Ni XJ (2018) Histone deacetylase HDAC4 promotes the proliferation and invasion of glioma cells. Int J Oncol 53(6):2758–2768
Shao L, Hou C (2019) miR-138 activates NF-kappaB signaling and PGRN to promote rheumatoid arthritis via regulating HDAC4. Biochem Biophys Res Commun 519(1):166–171
Li Z, Cai J, Cao X (2016) MiR-19 suppresses fibroblast-like synoviocytes cytokine release by targeting toll like receptor 2 in rheumatoid arthritis. Am J Transl Res 8(12):5512–5518
Xu X, Chen H, Zhang Q, Xu J, Shi Q, Wang M (2017) MiR-650 inhibits proliferation, migration and invasion of rheumatoid arthritis synovial fibroblasts by targeting AKT2. Biomed Pharmacother 88:535–541
Liu T, Zhang L, Joo D, Sun SC (2017) NF-κB signaling in inflammation. Signal Transduct Target Ther 2:17023
Kwon HJ, Choi GE, Ryu S, Kim SC, Booth C, Nichols KE, Kim HS (2016) Stepwise phosphorylation of p65 promotes NF-κB activation and NK cell responses during target cell recognition. Nat Commun 7:11686
Chen WK, Yu XH, Yang W, Wang C, He WS, Yan YG, Zhang J, Wang WJ (2017) lncRNAs: novel players in intervertebral disc degeneration and osteoarthritis. Cell Prolif. https://doi.org/10.1111/cpr.12313
Ye Y, Gao X, Yang N (2018) LncRNA ZFAS1 promotes cell migration and invasion of fibroblast-like synoviocytes by suppression of miR-27a in rheumatoid arthritis. Hum Cell 31(1):14–21
Ai D, Yu F (2019) LncRNA DNM3OS promotes proliferation and inhibits apoptosis through modulating IGF1 expression by sponging MiR-126 in CHON-001 cells. Diagn Pathol 14(1):106
Pearson MJ, Jones SW (2016) Review: Long Noncoding RNAs in the Regulation of Inflammatory Pathways in Rheumatoid Arthritis and Osteoarthritis. Arthritis Rheumatol 68(11):2575–2583
Li G, Liu Y, Meng F, Xia Z, Wu X, Fang Y, Zhang C, Liu D (2018) Tanshinone IIA promotes the apoptosis of fibroblast-like synoviocytes in rheumatoid arthritis by up-regulating lncRNA GAS5. Biosci Rep. https://doi.org/10.1042/BSR20180626
Mo BY, Guo XH, Yang MR, Liu F, Bi X, Liu Y, Fang LK, Luo XQ, Wang J, Bellanti JA, Pan YF, Zheng SG (2018) Long Non-Coding RNA GAPLINC Promotes Tumor-Like Biologic Behaviors of Fibroblast-Like Synoviocytes as MicroRNA Sponging in Rheumatoid Arthritis Patients. Front Immunol. https://doi.org/10.3389/fimmu.2018.00702
Dolcino M, Pelosi A, Fiore PF, Patuzzo G, Tinazzi E, Lunardi C, Puccetti A (2018) Long Non-Coding RNAs Play a Role in the Pathogenesis of Psoriatic Arthritis by Regulating MicroRNAs and Genes Involved in Inflammation and Metabolic Syndrome. Front Immunol. https://doi.org/10.3389/fimmu.2018.01533
Yoon JH, Abdelmohsen K, Gorospe M (2014) Functional interactions among microRNAs and long noncoding RNAs. Semin Cell Dev Biol. https://doi.org/10.1016/j.semcdb.2014.05.015
Feng FB, Qiu HY (2018) Effects of Artesunate on chondrocyte proliferation, apoptosis and autophagy through the PI3K/AKT/mTOR signaling pathway in rat models with rheumatoid arthritis. Biomed Pharmacother 102:1209–1220
Liu K, Zhang Y, Liu L, Yuan Q (2019) miR-125 regulates PI3K/Akt/mTOR signaling pathway in rheumatoid arthritis rats via PARP2. Biosci Rep. https://doi.org/10.1042/BSR20180890
Wang H, Zhang H, Sun Q, Yang J, Zeng C, Ding C, Cai D, Liu A, Bai X (2019) Chondrocyte mTORC1 activation stimulates miR-483–5p via HDAC4 in osteoarthritis progression. J Cell Physiol 234(3):2730–2740
Funding
None.
Author information
Authors and Affiliations
Contributions
TP developed the idea, HJ and YJ collected the clinical samples, TP performed all the complicated laboratory research work at the bench.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no financial conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Peng, T., Ji, D. & Jiang, Y. Long non-coding RNA GAS5 suppresses rheumatoid arthritis progression via miR-128-3p/HDAC4 axis. Mol Cell Biochem 476, 2491–2501 (2021). https://doi.org/10.1007/s11010-021-04098-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-021-04098-1