Abstract
Amomum tsao-ko (A. tsao-ko) has been used as a traditional medicine for the treatment of infectious and digestive disorders. In the present study, we report the anti-inflammatory activity and molecular mechanism of 2,8-decadiene-1,10-diol (DDO) isolated from the extract of A. tsao-ko in lipopolysaccharide-stimulated RAW 264.7 cells. DDO treatment inhibited the production of nitric oxide and prostaglandin E2 by downregulating inducible nitric oxide synthase and cyclooxygenase-2 expression, respectively. Moreover, DDO suppressed the production of pro-inflammatory cytokines such as interleukin-6 and tumor necrosis factor-α. These inhibitory effects of DDO on the expression of inflammatory proteins were found to be mediated through the inactivation of mitogen-activated protein kinases (MAPKs) such as extracellular signal-regulated kinase, c-Jun-N-terminal kinase and p38MAPK, and inhibition of nuclear factor-κB (NF-κB) pathways including degradation of inhibitor of κB-α and nuclear localization of NF-κB. Taken together, these findings demonstrate the pharmacological roles and molecular mechanisms of DDO in regulating inflammatory responses, and suggest further evaluation and development of DDO as a potent therapeutic agent for the treatment of inflammatory disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Amomum tsao-ko (A. tsao-ko) Crevost et Lemaire (Zingiberaceae) is a fruit that is widely used as a traditional medicine for the treatment of a variety of infectious and digestive disorders such as malaria, throat infection, dyspepsia, nausea, abdominal pain, and diarrhea. A. tsao-ko has lots of bioactive constituents including phenolic compounds, tannins, organic acids, saponins, flavonoids, anthraquinones, coumarins, lactones, cardiac glycosides, steroids, terpenoids, volatile oils, and anthocyanins, indicating the pharmacological roles in mediating anti-oxidant, anti-proliferative, anti-fungal, and anti-inflammatory activities [1–4]. Although some advances have been made in understanding the roles of A. tsao-ko in inflammation, no effects and action mechanisms of bioactive components isolated from the extract of A. tsao-ko on inflammatory responses have been clearly reported to date.
Inflammation is a normal and critical defense mechanism against pathological stimuli. A variety of pro-inflammatory cytokines and enzymes including tumor necrosis factor (TNF)-α, interleukin (IL)-6, inducible nitric oxide synthase (iNOS), and cyclooxygenase-2 (COX-2) are produced in the various types of lymphocytes as well as macrophages [5, 6]. Nuclear factor-κB (NF-κB), a key transcription factor for regulation of inflammation, controls the expression of pro-inflammatory proteins [7–9]. Excessive inflammatory responses by overexpression of pro-inflammatory proteins have been known to induce the occurrence and progression of chronic diseases including asthma, psoriasis, atherosclerosis, obesity, rheumatoid arthritis, inflammatory bowel disease, and cancer [10–15]. Therefore, NF-κB and intracellular signaling pathways responsible for production of pro-inflammatory proteins are widely appreciated as the therapeutic targets for inflammatory responses. Identification of molecular mechanisms and targets in regulating inflammatory responses may help to develop potential therapeutic strategies for the treatment and prevention of inflammation-related diseases.
In the present study, we report for the first time the regulatory effects and molecular mechanisms of 2,8-decadiene-1,10-diol, a phytochemical isolated from the ethanolic extract of A. tsao-ko, on lipopolysaccharide-induced inflammatory responses in RAW 264.7 cells.
MATERIALS AND METHODS
Reagents
The following chemicals and antibodies were purchased from commercial sources: dimethyl sulfoxide and 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (Duchefa Biochemie, Haarlem, The Netherlands); N-(1-naphthyl) ethylenediamine dihydrochloride and sulfanilamide (Merck Millipore, Billerica, MA, USA); lipopolysaccharide from Escherichia coli serotype 0111:B4, bovine serum albumin, RIPA buffer, protease inhibitor, and NG-methyl-L-arginine acetate salt (Sigma-Aldrich, St. Louis, MO, USA); anti-phosphor-JNK (T183/Y185), anti-JNK, anti-phosphor-ERK (T202/Y204), anti-ERK, anti-phosphor-p38MAPK (T180/Y182), anti-p38MAPK, anti-NF-κB p65, anti-NF-κB p50, anti-phosphor-IκB-α (S32/36), and anti-IκB-α (Cell Signaling, Beverly, MA, USA); anti-iNOS (Abcam, Cambridge, UK); anti-COX-2, anti-Lamin B, and anti-actin antibodies (Santa Cruz Biotechnology, Santa Cruz, CA, USA).
Preparation of A. Tsao-ko Extract and Isolation of 2,8-Decadiene-1,10-Diol
The dried fruits of A. tsao-ko were identified by Professor Joa Sub Oh (College of Pharmacy, Dankook University), purchased from the Gyeongdong Oriental Medicine Market (Seoul, Republic of Korea) in February 2012, and deposited at the herbarium of Bio-center, Gyeonggi Institute of Science & Technology Promotion (Suwon, Republic of Korea). Nine thousand five hundred grams of A. tsao-ko were extracted two times with 80 % ethanol at room temperature for 72 h. The extract was concentrated, suspended in water, and then partitioned with methylene chloride. The methylene chloride extract (146 g) was suspended in n-hexane and partitioned with 50 % methanol. The 50 % methanol layer was subjected to silica gel column chromatography (230–400 mesh, 13 × 15 cm) using n-hexane/acetone (1:0, 10:1, 7:1, 5:1, 3:1, 2:1, 1:1, 1:2) and methylene chloride/methanol (5:1, 2:1, 1:1) gradient elution system. Among thirteen fractions eluted column chromatography, the ninth fraction was further separated by liquid column chromatography (Sephadex LH-20, 5.0 × 155 cm) eluting with chloroform/MeOH (19:1, 9:1, 1:1) and subsequent chromatography (ODS-A, 2 × 30 cm) eluting with water/methanol (70:30, 60:40) gradient mode to yield 2,8-decadiene-1,10-diol (12 mg). 1H-, and 13C-NMR spectra were recorded on the Bruker Ascend 700 MHz NMR spectrometer (Bruker, Billerica, MA, USA).
Spectrometric Analysis of 2,8-Decadiene-1,10-Diol
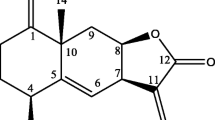
Pale yellow oil; 1H-NMR (CDCl3, 700 MHz): δ 5.69 (2H, m, H-3 and 8), 5.66 (2H, m, H-2 and 9), 4.10 (4H, d, J = 5.6 Hz, H-1 and 10), 2.07 (4H, d, J = 5.6 Hz, H-4 and 7), 1.41 (4H, s, H-5 and 6); 13C-NMR (CDCl3, 175 MHz): δ 133.2 (C-3 and 8), 129.0 (C-2 and 9), 63.8 (C-1 and 10), 32.0 (C-4 and 7), 28.6 (C-5 and 6). The structure of 2,8-decadiene-1,10-diol is presented in Fig. 1a.
DDO inhibits NO production in LPS-stimulated RAW 264.7 cells. a The chemical structure of DDO. b Cells were pretreated with DDO (6.25–200 μM) for 1 h, followed by LPS (1 μg/ml) stimulation for 24 h. NO production was determined by measuring the concentration of NO2 − and NO3 − in the cell culture supernatant. L-NMMA (100 μM) was used as a positive control. Values represent the mean ± SD of three independent experiments. Statistical significance is indicated (*P < 0.05; **P < 0.01, compared with LPS-treated cells). c Cells were treated as in panel (b). The results from three independent experiments (mean ± SD) are presented as the percentage of cell viability by LPS in the absence of DDO.
Cell Culture Conditions
The murine macrophage cell line RAW 264.7 (TIB-71) was purchased from the American Type Culture Collection (Manassas, VA, USA), and maintained in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10 % fetal bovine serum (FBS) and 1 % penicillin (100 U/ml)-streptomycin (100 μg/ml) (Invitrogen, Carlsbad, CA, USA).
Cell Viability Assay
RAW 264.7 cells, plated on 96-well plates (4 × 104 cells/well), were treated with 2,8-decadiene-1,10-diol (2,8-decadiene-1,10-diol (DDO), 6.25–200 μM) for 1 h prior to lipopolysaccharide (LPS, 1 μg/ml) stimulation for 24 h. Following culture for 24 h, 10 μl of MTT solution (5 mg/ml in phosphate-buffered saline (PBS), pH 7.4) was added to each well, and the cells were further incubated for 2 h. Cell viability was determined using a SpectraMax 190PC microplate reader (Molecular Devices, Sunnyvale, CA, USA). The results from triplicate determinations (mean ± standard deviation) are presented as the percentage of LPS-treated cell viability.
Nitric Oxide Production Assay
RAW 264.7 cells, plated on 96-well plates (4 × 104 cells/well), were treated with DDO (6.25–200 μM) for 1 h prior to LPS (1 μg/ml) stimulation for 24 h. The production of nitric oxide (NO) was determined by measuring the concentration of nitrite in the culture medium using the Griess reagent (Sigma-Aldrich), according to the manufacturer’s instructions.
Enzyme-Linked Immunosorbent Assay (ELISA)
RAW 264.7 cells, plated on 6-well plates (1 × 106 cells/well), were treated with DDO (50–200 μM) for 1 h prior to LPS (1 μg/ml) stimulation for 24 h. The concentration of prostaglandin E2 (PGE2), IL-6, or TNF-α in the cell culture supernatant was measured by using ELISA kits (R&D Systems, Minneapolis, MN, USA; eBioscience, Vienna, Austria), according to the manufacturer’s instructions.
Reverse Transcription-Polymerase Chain Reaction (RT-PCR)
RAW 264.7 cells, plated on 6-well plates (1 × 106 cells/well), were treated with DDO (50–200 μM) for 1 h prior to LPS (1 μg/ml) stimulation for different time points, as indicated. Total RNA was isolated using Trizol reagent (Invitrogen). One microgram of RNA was used as a template for each RT-PCR reaction using a SuperScript®III First-Strand Synthesis System and Taq DNA polymerase (Invitrogen). Primers for PCR were synthesized by Bioneer Corporation (Daejeon, Republic of Korea). Primer sequences are as follows: IL-6, forward 5′-CACTTCACAAGTCGGAGGCTT-3′ and reverse 5′-GCAAGTGCATCATCGTTGTTC-3′; TNF-α, forward 5′-CTGAGACAATG AACGCTACA-3′ and reverse 5′-TTCTTCCACATCTATGCCAC-3′; iNOS, forward 5′-GAGTTCGAGACTTCTGTGA-3′ and reverse 5′-GGCGATCTGGTAGTAGTAG-3′; COX-2, forward 5′-GTCAAAGACACTCAGGTAGA-3′ and reverse 5′-CTGTACTCCT GGTCTTCAAT -3′; and glyceraldehyde-3-phosphate dehydrogenase (GAPDH), forward 5′-CAGGTAAACTCAGGAGAGTG-3′ and reverse 5′-GTAGACTCCACGACATACT C-3′. Bands of interest were integrated and quantified by the use of ChemiDoc XRS system and Quantity One software (Bio-Rad Laboratories, Hercules, CA, USA).
Western Blot Analysis
RAW 264.7 cells, plated on 6-well plates (1 × 106 cells/well), were treated with DDO (50–200 μM) for 1 h prior to LPS (1 μg/ml) stimulation for different time points, as indicated. Cells were rinsed twice with ice-cold PBS and lysed by RIPA buffer containing protease inhibitors. Cell lysates were clarified at 13,000×g for 10 min at 4 °C, and the supernatants were subjected to Western blot analysis as described previously [16, 17]. All Western blots are representative of at least three independent experiments.
Immunofluorescence Microscopy
RAW 264.7 cells on glass cover-slips in 12-well plates (1 × 105 cells/well) were treated with DDO (200 μM) for 1 h prior to LPS (1 μg/ml) stimulation for 24 h, washed with PBS for 5 min, fixed with 3.7 % formaldehyde for 5 min, permeabilized with 0.1 % Triton X-100 for 10 min, washed with PBS for 5 min, and blocked with PBS containing 5 % bovine serum albumin for 1 h. Primary antibodies were incubated for 2 h, washed with PBS, and followed by fluorescein isothiocynate-labeled secondary antibodies (Invitrogen). Images were obtained with a Nikon Digital Sight DS-U1 microscope (Nikon, Tokyo, Japan).
Subcellular Fractionation
Following treatments as indicated, cells were washed three times with ice-cold PBS; lysed in buffer containing 10 mM Tris–HCl (pH 7.5), 150 mM NaCl, 1 % Nonidet P-40, and 1 mM phenylmethylsulfonyl fluoride (PMSF); and followed by centrifugation at 3000×g for 10 min at 4 °C. The supernatants were collected as cytosolic extracts. The pellets were resuspended in buffer containing 20 mM HEPES (pH 7.9), 10 mM KCl, 1.5 mM MgCl2, 0.2 mM EDTA, 0.5 mM DTT, 25 % (v/v) glycerol, and 0.5 mM PMSF, and centrifuged at 15,000×g for 15 min at 4 °C. The supernatants were collected as nuclear extracts.
Statistical Analysis
Statistical analysis was performed using one-way analysis of variance (ANOVA) with Dunnett’s test and Student t test, and was based on at least three different experiments. The results were considered to be statistically significant when P < 0.05.
RESULTS
DDO Inhibits LPS-Induced NO Production by Downregulation of iNOS Expression
To investigate the effects and molecular mechanisms of DDO on LPS-induced inflammatory responses, we first examined the ability of DDO to regulate NO production in response to LPS stimulation. DDO treatment inhibited LPS-induced NO production in a dose-dependent manner (6.25–200 μM), with an IC50 value of approximately 136.66 μM (Fig. 1b). We next examined cell viability to determine whether the inhibitory effect of DDO on NO production was attributable to nonspecific cytotoxicity. As shown in Fig. 1c, DDO treatment did not significantly affect cell viability at concentrations up to 300 μM (data not shown), indicating the safety and therapeutic potential of DDO in the regulation of inflammatory responses. In addition, NG-methyl-L-arginine (L-NMMA, 100 μM), an inhibitor of NOS, mimicked the suppressive effect of DDO on LPS-induced NO production in RAW 264.7 cells (Fig. 1b). These observations led us to investigate whether DDO regulates the expression of iNOS in LPS-treated cells. As shown in Fig. 2, RT-PCR and Western blot analyses showed that DDO treatment dose-dependently suppressed LPS-induced expression of iNOS in RAW 264.7 cells. Collectively, these results demonstrate that DDO inhibits LPS-induced NO production by downregulating iNOS expression.
DDO suppresses iNOS mRNA and protein levels in LPS-stimulated RAW 264.7 cells. Cells were pretreated with DDO (50–200 μM) for 1 h, followed by LPS (1 μg/ml) stimulation for 24 h. a The expression of iNOS mRNA was determined by RT-PCR analysis. GAPDH served as an internal control. b The expression of iNOS protein was determined by Western blot analysis. Actin served as an internal control. Values represent the mean ± SD of three independent experiments. Statistical significance is indicated (**P < 0.01, compared with LPS-treated cells).
DDO Inhibits LPS-Induced PGE2 Production by Downregulation of COX-2 Expression
We next examined the effects of DDO on the levels of PGE2 and COX-2 in LPS-stimulated RAW 264.7 cells. As shown in Fig. 3a, DDO treatment significantly inhibited the production of PGE2 at the highest concentration. In addition, DDO inhibited the expression of COX-2 messenger RNA (mRNA) and protein in LPS-stimulated RAW 264.7 cells, demonstrating that DDO-mediated inhibition of PGE2 production was mediated through downregulation of COX-2 expression (Fig. 3b, c, d). Although the potency of DDO in regulating the levels of inflammatory enzymes and their products was slightly different (Figs. 1b, 2, and 3), these findings indicate that DDO effectively inhibits the expression of pro-inflammatory enzymes such as iNOS and COX-2 in LPS-stimulated RAW 264.7 cells.
DDO inhibits COX-2 expression and PGE2 production in LPS-stimulated RAW 264.7 cells. Cells were pretreated with DDO (50–200 μM) for 1 h, followed by LPS (1 μg/ml) stimulation for 24 h. a PGE2 production analysis was carried out by using cell culture supernatant as described in “MATERIALS AND METHODS.” The expression of COX-2 mRNA and protein was determined by RT-PCR (b) and Western blot (c) analyses, respectively. Values represent the mean ± SD of three independent experiments. Statistical significance is indicated (**P < 0.01, compared with LPS-treated cells). d The cellular expression of COX-2 was detected by immunofluorescence microscopy analysis. DNA was stained with 4,6-diamidino-2-phenylindole (DAPI).
DDO Suppresses LPS-Induced Expression of IL-6 and TNF-α in RAW 264.7 Cells
Based on inhibitory effect of DDO on iNOS and COX-2 expression, we next examined the changes in pro-inflammatory cytokines such as IL-6 and TNF-α in DDO-treated RAW 264.7 cells. As shown in Fig. 4, LPS stimulation markedly induced the expression of IL-6 and TNF-α mRNA in RAW 264.7 cells. In contrast, DDO treatment inhibited LPS-induced expression of IL-6 and TNF-α mRNA in a dose-dependent manner. This inhibitory effect of DDO on IL-6 and TNF-α expression was sustained up to 24 h in LPS-stimulated cells (Fig. 4, right panel). In addition, the release of cytokines was also significantly suppressed by DDO treatment. These inhibitory effect and potency of DDO on IL-6 and TNF-α production were very similar to the patterns of COX-2 as previously observed (Fig. 3).
DDO inhibits the expression of IL-6 and TNF-α in LPS-stimulated RAW 264.7 cells. Cells were pretreated with DDO (50–200 μM) for 1 h, followed by LPS (1 μg/ml) stimulation for 1 h (a, left panel) or 24 h (a, right panel). a The expression of IL-6 and TNF-α mRNA was determined by RT-PCR analysis. Cells were treated as in panel (a, right panel), and the cell culture supernatant was subjected to IL-6 (b) and TNF-α (c) cytokine ELISA as described in “MATERIALS AND METHODS.” Values represent the mean ± SD of three independent experiments. Statistical significance is indicated (**P < 0.01, compared with LPS-treated cells).
DDO Inhibits LPS-Induced Nuclear Localization of NF-κB in RAW 264.7 Cells
NF-κB functions as a key transcription factor that regulates the expression of a variety of genes such as iNOS, COX-2, IL-6, and TNF-α in response to inflammatory stimuli [6, 7]. NF-κB must be present in the cell nucleus to activate inflammation-related target genes. Nuclear localization of NF-κB is controlled by phosphorylation and degradation of IκB-α, a cognate regulatory subunit of NF-κB [18]. Therefore, we examined the effects of DDO on NF-κB pathways including phosphorylation and degradation of IκB-α as well as nuclear translocation of NF-κB in LPS-stimulated RAW 264.7 cells. As expected, LPS stimulation for 1 h dramatically induced the phosphorylation and degradation of IκB-α in the cytosolic compartments, and subsequent localization of NF-κB in the nuclear compartments (Fig. 5). However, DDO treatment inhibited LPS-induced phosphorylation and degradation of IκB-α, and nuclear localization of NF-κB in a dose-dependent manner, indicating that DDO might regulate the expression of pro-inflammatory proteins through inhibition of NF-κB signaling pathways.
DDO inhibits NF-κB nuclear localization in LPS-stimulated RAW 264.7 cells. Cells were pretreated with DDO (50–200 μM) for 1 h, followed by LPS (1 μg/ml) stimulation for 1 h, and then subjected to subcellular fractionation into cytosolic and nuclear extracts as described in “MATERIALS AND METHODS.” The fractions were Western-blotted with anti-phospho-IκB-α, anti-IκB-α, anti-NF-κB p65, anti-NF-κB p50, anti-actin, or anti-Lamin B antibodies. Actin served as a marker for the cytosol and Lamin B for the nucleus. Results shown are representative of at least three independent experiments.
DDO Inhibits LPS-Induced Phosphorylation of MAPKs in RAW 264.7 Cells
LPS-stimulated NF-κB activation and inflammatory responses are mediated by a variety of signaling pathways including IκB kinase (IKK), NF-κB-inducing kinase, and mitogen-activated protein kinases (MAPKs) [8, 19–21]. Since DDO inhibited the phosphorylation of IκB-α on residues Ser 32 and Ser 36, sites specific for IKK phosphorylation (Fig. 5) [18, 22, 23], we next investigated the ability of DDO to regulate MAPK signaling pathways such as ERK, JNK, and p38MAPK in LPS-stimulated RAW 264.7 cells [24–26]. As shown in Fig. 6, DDO treatment dose-dependently suppressed LPS-induced phosphorylation/activation of ERK, JNK, and p38MAPK, suggesting that DDO exerts anti-inflammatory activity through inhibition of MAPKs as well as NF-κB signaling pathways.
DDO inhibits the phosphorylation of ERK, JNK, and p38MAPK in LPS-stimulated RAW 264.7 cells. Cells were pretreated with DDO (50–200 μM) for 1 h, followed by LPS (1 μg/ml) stimulation for 30 min. Cell lysates were Western-blotted with anti-phospho-ERK, anti-ERK, anti-phospho-JNK, anti-JNK, anti-phospho-p38MAPK, anti-p38MAPK, or anti-actin antibodies. Results shown are representative of at least three independent experiments.
DISCUSSION
The transcription factor NF-κB, which regulates the expression of inflammation-related proteins involved in pathological inflammatory responses as well as physiological immunity, has widely been considered as an important target for the development of anti-inflammatory drugs [6–8, 12]. However, many investigations indicate that the roles and molecular mechanisms of NF-κB in modulating inflammatory responses are very complex. Therefore, further understanding of signaling pathways and key molecular targets of NF-κB in inflammation is required for the development of potent therapeutic strategies to treat a variety of inflammation-related diseases including cancer [12, 27].
In the present study, we report that 2,8-decadiene-1,10-diol (DDO) isolated from the extract of A. tsao-ko negatively regulates inflammatory responses to LPS stimulation. DDO treatment significantly inhibits the expression of pro-inflammatory proteins such as iNOS, COX-2, IL-6, and TNF-α, and subsequent production of NO and PGE2 in LPS-stimulated RAW 264.7 cells. Blockade of MAPKs including ERK, JNK, and p38MAPK as well as the NF-κB signaling pathway mediates the anti-inflammatory activities of DDO in LPS-stimulated RAW 264.7 cells, indicating that DDO acts simultaneously on multiple molecular targets in mediating inhibition of inflammatory responses. These findings also suggest the possibility that DDO may regulate the expression and activity of pharmacologically important targets in a variety of pathological conditions as well as inflammation. Furthermore, DDO showed little or no change in cell morphology and viability at higher concentration than used in this study (300 μM, data not shown), demonstrating the safety and therapeutic efficacy of DDO in the regulation of inflammation.
In conclusion, this is the first report to demonstrate the pharmacological roles and therapeutic efficacy of DDO in the regulation of inflammatory responses, and warrants further investigation and development of DDO as a potent therapeutic agent for the treatment and prevention of inflammation-related diseases.
References
Yang, Y., Y. Yue, Y. Runwei, and Z. Guolin. 2010. Cytotoxic, apoptotic and antioxidant activity of the essential oil of Amomum tsao-ko. Bioresource Technology 101: 4205–4211.
Moon, S.S., J.Y. Lee, and S.C. Cho. 2004. Isotsaokoin, an antifungal agent from Amomum tsao-ko. Journal of Natural Products 67: 889–891.
Yu, L., N. Shirai, H. Suzuki, N. Sugane, T. Hosono, Y. Nakajima, et al. 2010. The effect of methanol extracts of tsaoko (Amomum tsao-ko Crevost et Lemaire) on digestive enzyme and antioxidant activity in vitro, and plasma lipids and glucose and liver lipids in mice. Journal of Nutritional Science and Vitaminology 56: 171–176.
Li, B., H.J. Choi, D.S. Lee, H. Oh, Y.C. Kim, J.Y. Moon, et al. 2014. Amomum tsao-ko suppresses lipopolysaccharide-induced inflammatory responses in RAW264.7 macrophages via Nrf2-dependent heme oxygenase-1 expression. The American Journal of Chinese Medicine 42: 1229–1244.
Medzhitov, R. 2010. Inflammation 2010: new adventures of an old flame. Cell 140: 771–776.
Hayden, M.S., A.P. West, and S. Ghosh. 2006. NF-κB and the immune response. Oncogene 25: 6758–6780.
Lawrence, T. 2009. The nuclear factor NF-κB pathway in inflammation. Cold Spring Harbor Perspectives in Biology 1: a001651.
Ghosh, S., and M.S. Hayden. 2008. New regulators of NF-κB in inflammation. Nature Reviews Immunology 8: 837–848.
Barnes, P.J., and M. Karin. 1997. Nuclear factor-κB—a pivotal transcription factor in chronic inflammatory diseases. New England Journal of Medicine 336: 1066–1071.
Hotamisligil, G.S. 2006. Inflammation and metabolic disorders. Nature 444: 860–867.
Lumeng, C.N., and A.R. Saltiel. 2011. Inflammatory links between obesity and metabolic disease. The Journal of Clinical Investigation 121: 2111–2117.
Ben-Neriah, Y., and M. Karin. 2011. Inflammation meets cancer, with NF-κB as the matchmaker. Nature Immunology 12: 715–723.
Kaser, A., S. Zeissig, and R.S. Blumberg. 2010. Inflammatory bowel disease. Annual Review of Immunology 28: 573–621.
Lizzul, P.F., A. Aphale, R. Malaviya, Y. Sun, S. Masud, V. Dombrovskiy, et al. 2005. Differential expression of phosphorylated NF-κB//RelA in normal and psoriatic epidermis and downregulation of NF-κB in response to treatment with etanercept. Journal of Investigative Dermatology 124: 1275–1283.
Gillooly, K.M., M.A. Pattoli, T.L. Taylor, L. Chen, L. Cheng, K.R. Gregor, et al. 2009. Periodic, partial inhibition of IκB kinase β-mediated signaling yields therapeutic benefit in preclinical models of rheumatoid arthritis. Journal of Pharmacology and Experimental Therapeutics 331: 349–360.
Ahn, E.K., J.A. Lee, D.W. Seo, S.S. Hong, and J.S. Oh. 2012. 1β-Hydroxy-2-oxopomolic acid isolated from Agrimonia pilosa extract inhibits adipogenesis in 3T3-L1 cells. Biological and Pharmaceutical Bulletin 35: 643–649.
Ahn, E.K., and J.S. Oh. 2013. Lupenone isolated from Adenophora triphylla var. Japonica extract inhibits adipogenic differentiation through the downregulation of PPARγ in 3T3-L1 cells. Phytotherapy Research 27: 761–766.
Karin, M., and Y. Ben-Neriah. 2000. Phosphorylation meets ubiquitination: the control of NF-κB activity. Annual Review of Immunology 18: 621–663.
Vermeulen, L., G. De Wilde, P. Van Damme, W. Vanden Berghe, and G. Haegeman. 2003. Transcriptional activation of the NF-κB p65 subunit by mitogen- and stress-activated protein kinase-1 (MSK1). The EMBO Journal 22: 1313–1324.
Carter, A.B., K.L. Knudtson, M.M. Monick, and G.W. Hunninghake. 1999. The p38 mitogen-activated protein kinase is required for NF-κB-dependent gene expression: the role of TATA-binding protein (TBP). Journal of Biological Chemistry 274: 30858–30863.
Kim, H.J., H.S. Lee, Y.H. Chong, and J.L. Kang. 2006. p38 mitogen-activated protein kinase up-regulates LPS-induced NF-κB activation in the development of lung injury and RAW 264.7 macrophages. Toxicology 225: 36–47.
Zandi, E., D.M. Rothwarf, M. Delhase, M. Hayakawa, and M. Karin. 1997. The IκB kinase complex (IKK) contains two kinase subunits, IKKα and IKKβ, necessary for IκB phosphorylation and NF-κB activation. Cell 91: 243–252.
Delhase, M., M. Hayakawa, Y. Chen, and M. Karin. 1999. Positive and negative regulation of IκB kinase activity through IKKβ subunit phosphorylation. Science 284: 309–313.
Guha, M., and N. Mackman. 2001. LPS induction of gene expression in human monocytes. Cellular Signalling 13: 85–94.
Bode, J.G., C. Ehlting, and D. Häussinger. 2012. The macrophage response towards LPS and its control through the p38MAPK–STAT3 axis. Cellular Signalling 24: 1185–1194.
Hommes, D.W., M.P. Peppelenbosch, and S.J.H. van Deventer. 2003. Mitogen activated protein (MAP) kinase signal transduction pathways and novel anti-inflammatory targets. Gut 52: 144–151.
Karin, M. 2006. Nuclear factor-κB in cancer development and progression. Nature 441: 431–436.
Acknowledgments
This study was supported by the research fund of Dankook University in 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Mi-Sun Kim and Eun-Kyung Ahn contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kim, MS., Ahn, EK., Hong, S.S. et al. 2,8-Decadiene-1,10-Diol Inhibits Lipopolysaccharide-Induced Inflammatory Responses Through Inactivation of Mitogen-Activated Protein Kinase and Nuclear Factor-κB Signaling Pathway. Inflammation 39, 583–591 (2016). https://doi.org/10.1007/s10753-015-0283-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-015-0283-1