Abstract
Sevoflurane is one of the most commonly used volatile anesthetics. Recent studies have shown that sevoflurane plays an important role in modulation of inflammation and immunity. However, little is known about the related molecular mechanisms. This study was designed to investigate the effects and mechanisms of sevoflurane on inflammatory cell death pyroptosis in the murine macrophage cell line J774 cells. Sevoflurane combined with ATP could increase the level of activated caspase-1, pyroptosis, and reactive oxygen species (ROS). Furthermore, treatment of cells with the caspase-1 inhibitor Ac-YVAD-CMK dramatically decreased the percentage of pyroptosis. In addition, inhibition of ROS with N-acetyl-l-cysteine or diphenyleneiodonium significantly reduced the activated levels of caspase-1. These results demonstrated that sevoflurane combined with ATP could activate caspase-1 and trigger caspase-1-dependent pyroptosis through the modulation of ROS production.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Sevoflurane, one of the most common volatile anesthetics, is widely used in surgical procedures not only because of its high-speed and non-irritation but also of its anti-inflammatory, organ protection features and its immune modulating properties [1–3]. Previous studies have demonstrated that both sevoflurane pre- and postconditioning have protective effects and inflammatory and immune regulation characteristics [4–6]. In recent years, the modulation of sevoflurane on inflammation and immunity has been extensively studied. However, the specific molecular mechanism remains unclear.
Caspase-1, one of the cysteinyl aspartate-specific proteases, is synthesized as an inactive pro-caspase-1, P45. The cleavage and activation of P45 are triggered by the assembly of inflammasome, the NOD-like receptor (NLR)/caspase-1 complex [7, 8], and then forming the activated subunits which are composed of P10 and P20 [9]. The activated caspase-1 can further trigger pyroptosis [10–12]. This newly discovered form of cell death is characterized by a unique morphological and biochemical features. It can produce specific membrane pores between 1.1 and 2.4 nm in diameter and dissipate ionic gradients leading to water uptake and cell swelling; ultimately, cells undergo osmotic lysis with release of intracellular contents [11]. Caspase-1-deficient mice are more susceptible to intracellular pathogens, for example Francisella tularensis, Salmonella typhimurium, etc. [12]. Caspase-1-dependent pyroptosis contributes to eliminate the intracellular bacteria [13, 14]. Additionally, it has been identified that caspase-1 activation plays an important role in the pathogenesis of chronic inflammatory and autoimmune diseases [15, 16].
Up to now, caspase-1 and caspase-1-dependent pyroptosis are important in inflammatory and immune regulation. However, whether sevoflurane affects these processes is still unknown. Herein, we investigated the effect of sevoflurane on the activation of caspase-1 and the extent of caspase-1-dependent pyroptosis in mouse macrophage cell line.
MATERIALS AND METHODS
Cell Culture
The murine J774 macrophage cell line was cultured in DMEM medium (Gibco, Grand Island, NY) containing 10 % fetal bovine serum (Invitrogen, Carlsbad, CA) and 1 % penicillin–streptomycin (Invitrogen, Carlsbad, CA) at 37 °C in a humidified incubator (5 % CO2 and 95 % air; Thermo Electron, Waltham, MA). Before experiment, J774 cells were seeded in 24-well plates at 1 × 106 cells/well and incubated for 24 h.
Exposure of Cultured Cells to Sevoflurane
Anesthetic-enriched medium was prepared as described in a previous study [17]. Continuous sevoflurane (Maruishi Pharmaceutical Co. Ltd., Osaka, Japan) infusion was used to reduce the volatilization loss of sevoflurane from the anesthetic-enriched medium. Additionally, the J774 cells were exposed to different volume percent of sevoflurane. High concentration (≥6 %) of sevoflurane presented a significant activation of caspase-1 and caspase-1-dependent pyroptosis (data not shown), which is in accordance with previous studies [18].
After incubation of 24 h, the J774 cells were stimulated with or without 1 μg/mL LPS (Sigma, St. Louis, MO) for 4 h. The old medium was aspirated and the anesthetic-enriched medium was added, simultaneously stimulated with or without 5 mM ATP (Roche Diagnostics, Indianapolis, IN). Meanwhile, the J774 cells were placed in an air-tight, humidified specifically modified incubator with inflow and outflow connectors for 0.5 h at 37 °C. The inlet port was connected to the sevoflurane vaporizer (Blease Medical Equipment Ltd, Chesham, UK) to deliver 6 % sevoflurane at 3 L/min. The outlet port was connected to a Datex-Ohmeda 5250 RGM gas analyzer (Dräger, Lübeck, Germany) which measured sevoflurane concentration. Non-sevoflurane group cells were seeded in the anesthetic-free medium then exposed to 95 % air and 5 % CO2 in a specifically modified incubator. After 0.5 h, the cells were harvested for further analysis.
Additionally, for pharmacological assessments, cells were pretreated with or without 10 mM N-acetyl-l-cysteine (NAC; Sigma, St. Louis, MO) or 12.5 μM diphenyleneiodonium (DPI; Sigma, St. Louis, MO) for 15 min before ATP stimulation, after that the cells were exposed to ATP and 6 % sevoflurane for 0.5 h.
Western Blotting Analysis
Cells were lysed in lysis buffer containing protease inhibitors phenylmethylsulfonyl fluoride, followed by incubation on ice for 45 min. The cell lysates were clarified by centrifugation for 15 min. 20 μg of each clarified lysate were separated on 12 % SDS polyacrylamide gels, transferred to nitrocellulose membranes. Membranes were blocked in TBS-T containing 5 % BSA for 1 h. Membranes were washed three times in TBS-T for 10 min and incubated with rabbit polyclonal caspase-1 antibody SC-514 (Santa Cruz, CA) or anti-mouse β-actin antibody overnight. Membranes were washed three times with TBS-T, followed by anti-rabbit horseradish peroxidase-conjugated secondary antibody for 2 h. Thereafter, membranes were washed three times in TBS-T and detected by chemiluminescence.
Ethidium Bromide and EthD-2 Staining
After being washed twice with PBS, cells of each group were stained with the membrane permeable dye 4′,6-diamidino-2-phenylindole (DAPI; Molecular Probe, Eugene, OR) for 10 min and caspase-1 inhibitor Ac-YVAD-CMK (Merck Chemicals, Kilsyth, Victoria, Australia), the red membrane impermeant dyes, EtBr (MW394 Da; Molecular Probe, Eugene, OR) or EthD-2 (MW 1,293 Da; Molecular Probe, Eugene, OR) according to the manufacturer’s instructions. Coverslips were analyzed using Olympus IX81 fluorescence microscope (Tokyo, Japan). The percentage of positive cells was derived from counting a minimum of 300 cells/sample under each experimental condition.
ROS Detection
Intracellular ROS was determined with the ROS-specific fluorescent probe CM-H2DCFDA (Molecular Probe, Eugene, OR) [19]. Cells of each group were loaded for 15–30 min with 10 mM CM-H2DCFDA, washed twice with OPTI-MEM (Gibco, Grand Island, NY). The level of fluorescence was determined by flow cytometry (BD LSRII System; BD Biosciences, San Jose, CA).
Cell Viability Assay
Cell viability was detected using Cell Counting Kit-8 (CCK-8; Dojindo, Kumamoto, Japan). J774 cells were pated at a density of 5,000 cells/well in 96-well plates. Pre-incubate the plate for 24 h in the incubator. Then the cells were exposed to 6 % sevoflurane/95 % air and 5 % CO2 with or without 5 mM ATP. After that, 10 μL of CCK-8 solution was added to each well of the plate and incubated for 2 h. After incubation, the optical density was measured at 450 nm using a microplate reader (Bio-Rad Laboratories, Richmond, CA).
Statistical Analysis
Statistical comparisons between different treatments were performed by Student’s t test (two-tailed) or analysis of variance with Tukey’s post hoc pairwise comparisons using SPSS16.0 for Windows (SPSS, Inc., Chicago, IL). Values were reported as mean ± SD from three independent experiments. Differences were considered significant for P < 0.05.
RESULTS
LPS and ATP Activate Caspase-1 in Murine J774 Macrophages
LPS (1 μg/mL) treatment prior to 5 mM ATP pulse induced caspase-1 activation (Fig. 1) in murine J774 macrophages but not sevoflurane or ATP alone.
Sevoflurane Combined with ATP Activates Caspase-1
In the level of activated caspase-1, P10 was markedly increased in the sevoflurane-ATP group compared with that in the non-sevoflurane ATP group (220.4 ± 75.6 vs. 44.9 ± 24.1 Int/mm2, P = 0.019) (Fig. 2a) while, sevoflurane alone or sevoflurane combined with LPS could not activate caspase-1 (Fig. 2a). Sevoflurane did not significantly affect the viability of the cells in the presence and absence of ATP (Fig. 2b).
Sevoflurane combined with ATP activates caspase-1. The J774 cells were seeded in 24-well plates at 1 × 106 cells/well and incubated for 24 h. After that, the cells were stimulated with LPS (1 μg/mL, 4 h), ATP (5 mM, 0.5 h), and/or sevoflurane (6 %, 0.5 h). The negative control was exposed to 95 % air and 5 % CO2 for 0.5 h. a Expression of P10 under stimulation with sevoflurane, LPS, or ATP. Results are mean ± SD from three independent experiments. *P < 0.05 versus ATP+SEVO sample. b The effect of sevoflurane on J744 cell viability. J774 cells were pated at 5,000 cells/well in 96-well plates and incubated for 24 h. Then the cells were exposed to 6 % sevoflurane/95 % air and 5 % CO2 with or without 5 mM ATP, followed by a CCK-8 assay performed to quantitatively assess the cell viability using adsorption of OD450 nm.
Sevoflurane Combined with ATP Triggers Caspase-1-Dependent Pyroptosis
The membrane impermeant dye EtBr, EthD-2 and the membrane permeable dye DAPI were used to examine membrane pore formation during pyroptosis [11]. Consistent with results shown in Fig. 2a, the percentage of EtBr uptake was significantly increased in the sevoflurane group (87.9 ± 1.3 vs. 20.0 ± 2.2 %, P < 0.001) and can be inhibited by the caspase-1 inhibitor Ac-YVAD-CMK (87.9 ± 1.3 vs. 10.7 ± 3.3 %, P < 0.001) (Fig. 3). However, the EthD-2 uptake was similar between the two groups (5.0 ± 2.2 vs. 9.1 ± 2.1 %, P = 0.10) (Fig. 3).
Sevoflurane combined with ATP triggers caspase-1-dependent pyroptosis. Each group of cells after being exposed to sevoflurane or 95 % air and 5 % CO2 for 0.5 h, were washed twice with PBS, then cells were stained with the membrane permeable dye DAPI for 10 min and the red membrane impermeant dyes EtBr or EthD-2 as directed by the manufacturer’s instructions. The percentage of positive cells was derived from counting a minimum of 300 cells per sample for each experimental condition. Results are mean ± SD from three independent experiments. **P < 0.001 versus ATP+SEVO sample; number sign no significant difference versus ATP+SEVO sample.
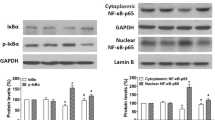
Sevoflurane Combined with ATP Regulates Caspase-1 Activation by Modulating ROS Production
Sevoflurane upregulated caspase-1 activation and caspase-1-dependent pyroptosis. Since ROS is believed to be a common NLR/caspase-1 complex activator [20], we hypothesized that sevoflurane mediates caspase-1 activation via ROS production. The level of ROS production in J774 cells was measured with CM-H2DCFDA. As predicted, the ROS fluorescence was significantly increased after sevoflurane plus ATP stimulation in J774 cells and the LPS plus ATP stimulation group than that in the non-sevoflurane ATP group (1,270.0 ± 81.3 vs. 780.0 ± 8.8 Int/mm2, P < 0.001; 1,175.7 ± 70.6 vs. 780.0 ± 8.8 Int/mm2, P = 0.001) (Fig. 4a). To further address whether ROS was involved in sevoflurane combined with ATP-regulated caspase-1 activation, J774 cells were treated with ROS inhibitor NAC or DPI before ATP stimulation. The activation of caspase-1 was reduced by both NAC (196.1 ± 26.0 vs. 37.8 ± 20.4, P = 0.013) and DPI (196.1 ± 26.0 vs. 62.8 ± 31.8, P = 0.028), which disrupted the ROS production (Fig. 4b).
Sevoflurane combined with ATP regulates caspase-1 activation by modulating ROS production. a Sevoflurane modulates ROS production. Each group of cells were exposed to 6 % sevoflurane or 95 % air and 5 % CO2 for 0.5 h, and then loaded for 15–30 min with 10 mM CM-H2DCFDA. Results are mean ± SD from three independent experiments. *P < 0.05; **P < 0.001. b ROS inhibitor reduced the activation of caspase-1. The J774 cells were seeded in 24-well plates at 1 × 106 cells/well and incubated for 24 h. Cells were pretreated with or without 10 mM NAC or 12.5 μM DPI for 15 min, and then the anesthetic-enriched medium was added, simultaneously stimulated with 5 mM ATP and/or 6 % sevoflurane for 0.5 h. Negative stimulated with PBS. Results are mean ± SD from three independent experiments. *P < 0.05 compared with all other groups.
DICUSSION
The present study demonstrated that 6 % sevoflurane combined with 5 mM ATP could activate caspase-1, trigger caspase-1-dependent pyroptosis in murine J774 macrophages by modulating ROS production.
Caspase-1 plays an important role in both innate and acquired immune responses. Studies have shown that caspase-1-mediated innate immunity and the downstream proinflammatory response can protect host against many invading pathogens. Recently, Miao et al. indentified that caspase-1-mediated macrophage pyroptosis is an innate immune effector mechanism against intracellular bacteria. Indeed, this effect resulted in the intracellular pathogens releasing into the extracellular space. The latter then were uptaken and killed by neutrophils efficiently [14]. In addition, current studies have indicated that pyroptosis eliminates cellular niches for bacterial replication, recruits and activates immune effector cells to the site of infection and enhances the host defense against the pathogenic microorganisms [10, 11, 13].
Sevoflurane, one of the most frequently used volatile anesthetics, has been extensively studied due to its inflammatory and immune modulatory effect. The present study firstly reveals that sevoflurane plus ATP may regulate macrophages through activation of caspase-1 and triggering caspase-1-dependent pyroptosis. Virtually, many kinds of cells such as stimulated T cells, polymorphonuclear granulocytes and intact cells can release ATP during conditions of inflammation or hypoxia [21–23]. Considering the immune regulatory properties of caspase-1-mediated pyroptosis, our results provides preliminary evidences that perioperative sevoflurane application may enhance host immune defense function and benefit for preventing from postoperative infection. It might be particularly helpful for patients suffering from immune dysfunction, especially in sepsis patients with pro-caspase-1 and activated caspase-1 markedly inhibited [24]. Therefore, further exploration of the role of pyroptosis initiated by sevoflurane in vivo may lead to new therapies for both infectious and inflammatory diseases.
Activation of caspase-1 needs the formation of NLR/caspase-1 complex. It has also been demonstrated that K+ efflux is mediated by P2X7, phagosomal destabilization and reactive oxygen species involve in the activation of NLR/caspase-1complex [25–27]. Studies have shown that lysosomal destabilization mainly participates in triggering the formation of NLR/caspase-1complex induced by small crystalline materials [20, 25]. Additionally, ATP could increase the level of ROS, and sevoflurane plays an important role in organ-protecting through ROS-dependent mechanism [28–30]. Therefore, we speculate that sevoflurane mediates caspase-1 activation through ROS production. As predicted, our results confirmed that ROS significantly increased after sevoflurane plus ATP stimulation in J774 cells for 0.5 h, which was even higher than the LPS plus ATP stimulation. These findings are consistent with previous studies. The speculation was further confirmed by the finding that ROS inhibitors NAC and DPI reduced the activation of caspase-1 by sevoflurane combined with ATP. The current study also demonstrated that promoting ROS production was the main mechanism in sevoflurane plus ATP induced activation of caspase-1 and caspase-1-dependent pyroptosis in murine macrophages.
There are potential limitations regarding the interpretation of our data. In this paper, we focused on the J774 macrophage cell line in vitro and presented a preliminary result on the immune regulation of sevoflurane. To our knowledge, cell lines might be different from primary cells in some of the biological activities. So, further ex vivo and in vivo study is warranted. However, based on the common characteristics shared by the cell line and primary cells, cell lines are routinely adopted models in pilot studies before in-depth investigations. On the other hand, differences in the molecular conformation and structure-activity relationships of halogenated anesthetic agents may lead to different biological functions. Therefore, the sevoflurane-mediated effects observed in this study might not be generalized to the other halogenated anesthetics.
In summary, sevoflurane combined with ATP can activate caspase-1 and trigger caspase-1-dependent pyroptosis. The possible mechanism is related to sevoflurane increased ROS production. These results indicate that sevoflurane might regulate immune response via activating caspase-1 and caspase-1-dependant pyroptosis of macrophages in vivo, which may be beneficial for better choice of clinical anesthesia and the witness of sevoflurane immune regulatory mechanism.
REFERENCES
Kawamura, T., M. Kadosaki, N. Nara, A. Kaise, H. Suzuki, S. Endo, J. Wei, and K. Inada. 2006. Effects of sevoflurane on cytokine balance in patients undergoing coronary artery bypass graft surgery. Journal of Cardiothoracic and Vascular Anesthesia 20: 503–508.
Kong, H.Y., S.M. Zhu, L.Q. Wang, Y. He, H.Y. Xie, and S.S. Zheng. 2010. Sevoflurane protects against acute kidney injury in a small-size liver transplantation model. American Journal of Nephrology 32: 347–355.
Lee, H.T., M. Kim, M. Jan, and C.W. Emala. 2006. Anti-inflammatory and antinecrotic effects of the volatile anesthetic sevoflurane in kidney proximal tubule cells. American Journal of Physiology-Renal Physiology 291: F67–F78.
Ding, Q., Q. Wang, J. Deng, Q. Gu, S. Hu, Y. Li, B. Su, Y. Zeng, and L. Xiong. 2009. Sevoflurane preconditioning induces rapid ischemic tolerance against spinal cord ischemia/reperfusion through activation of extracellular signal-regulated kinase in rabbits. Anesthesia and Analgesia 109: 1263–1272.
Kidani, Y., T. Taniguchi, H. Kanakura, Y. Takemoto, K. Tsuda, and K. Yamamoto. 2005. Sevoflurane pretreatment inhibits endotoxin-induced shock in rats. Anesthesia and Analgesia 101: 1152–1156.
Obal, D., S. Dettwiler, C. Favoccia, H. Scharbatke, B. Preckel, and W. Schlack. 2005. The influence of mitochondrial KATP-channels in the cardioprotection of preconditioning and postconditioning by sevoflurane in the rat in vivo. Anesthesia and Analgesia 101: 1252–1260.
Franchi, L., T. Eigenbrod, R. Munoz-Planillo, and G. Nunez. 2009. The inflammasome: a caspase-1-activation platform that regulates immune responses and disease pathogenesis. Nature Immunology 10: 241–247.
Martinon, F., K. Burns, and J. Tschopp. 2002. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Molecular Cell 10: 417–426.
Martinon, F., and J. Tschopp. 2004. Inflammatory caspases: linking an intracellular innate immune system to autoinflammatory diseases. Cell 117: 561–574.
Brodsky, I.E., and R. Medzhitov. 2011. Pyroptosis: macrophage suicide exposes hidden invaders. Current Biology 21: R72–R75.
Fink, S.L., and B.T. Cookson. 2006. Caspase-1-dependent pore formation during pyroptosis leads to osmotic lysis of infected host macrophages. Cellular Microbiology 8: 1812–1825.
Mariathasan, S., D.S. Weiss, V.M. Dixit, and D.M. Monack. 2005. Innate immunity against Francisella tularensis is dependent on the ASC/caspase-1 axis. The Journal of Experimental Medicine 202: 1043–1049.
Lara-Tejero, M., F.S. Sutterwala, Y. Ogura, E.P. Grant, J. Bertin, A.J. Coyle, R.A. Flavell, and J.E. Galan. 2006. Role of the caspase-1 inflammasome in Salmonella typhimurium pathogenesis. The Journal of Experimental Medicine 203: 1407–1412.
Miao, E.A., I.A. Leaf, P.M. Treuting, D.P. Mao, M. Dors, A. Sarkar, S.E. Warren, M.D. Wewers, and A. Aderem. 2010. Caspase-1-induced pyroptosis is an innate immune effector mechanism against intracellular bacteria. Nature Immunology 11: 1136–1142.
Cunha, T.M., J. Talbot, L.G. Pinto, S.M. Vieira, G.R. Souza, A.T. Guerrero, F. Sonego, W.A. Verri Jr., D.S. Zamboni, S.H. Ferreira, and F.Q. Cunha. 2010. Caspase-1 is involved in the genesis of inflammatory hypernociception by contributing to peripheral IL-1beta maturation. Molecular Pain 6: 63.
Tsuji, N.M., H. Tsutsui, E. Seki, K. Kuida, H. Okamura, K. Nakanishi, and R.A. Flavell. 2004. Roles of caspase-1 in Listeria infection in mice. International Immunology 16: 335–343.
Eilers, H., F. Cattaruzza, R. Nassini, S. Materazzi, E. Andre, C. Chu, G.S. Cottrell, M. Schumacher, P. Geppetti, and N.W. Bunnett. 2010. Pungent general anesthetics activate transient receptor potential-A1 to produce hyperalgesia and neurogenic bronchoconstriction. Anesthesiology 112: 1452–1463.
Roesslein, M., M. Frick, V. Auwaerter, M. Humar, U. Goebel, C. Schwer, K.K. Geiger, H.L. Pahl, B.H. Pannen, and T. Loop. 2008. Sevoflurane-mediated activation of p38-mitogen-activated stress kinase is independent of apoptosis in Jurkat T-cells. Anesthesia and analgesia 106: 1150–1160. table of contents.
Hu, Y., K. Mao, Y. Zeng, S. Chen, Z. Tao, C. Yang, S. Sun, X. Wu, G. Meng, and B. Sun. 2010. Tripartite-motif protein 30 negatively regulates NLRP3 inflammasome activation by modulating reactive oxygen species production. Journal of Immunology 185: 7699–7705.
Martinon, F., A. Mayor, and J. Tschopp. 2009. The inflammasomes: guardians of the body. Annual Review of Immunology 27: 229–265.
Corriden, R., and P.A. Insel. 2010. Basal release of ATP: an autocrine-paracrine mechanism for cell regulation. Science Signaling 3: re1.
Piccini, A., S. Carta, S. Tassi, D. Lasiglie, G. Fossati, and A. Rubartelli. 2008. ATP is released by monocytes stimulated with pathogen-sensing receptor ligands and induces IL-1beta and IL-18 secretion in an autocrine way. Proceedings of the National Academy of Sciences of the United States of America 105: 8067–8072.
Seo, D.R., S.Y. Kim, K.Y. Kim, H.G. Lee, J.H. Moon, J.S. Lee, S.H. Lee, S.U. Kim, and Y.B. Lee. 2008. Cross talk between P2 purinergic receptors modulates extracellular ATP-mediated interleukin-10 production in rat microglial cells. Experimental and Molecular Medicine 40: 19–26.
Giamarellos-Bourboulis, E.J., F.L. van de Veerdonk, M. Mouktaroudi, M. Raftogiannis, A. Antonopoulou, L.A. Joosten, P. Pickkers, A. Savva, M. Georgitsi, J.W. van der Meer, and M.G. Netea. 2011. Inhibition of caspase-1 activation in Gram-negative sepsis and experimental endotoxemia. Critical Care 15: R27.
Hornung, V., F. Bauernfeind, A. Halle, E.O. Samstad, H. Kono, K.L. Rock, K.A. Fitzgerald, and E. Latz. 2008. Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nature Immunology 9: 847–856.
Petrilli, V., S. Papin, C. Dostert, A. Mayor, F. Martinon, and J. Tschopp. 2007. Activation of the NALP3 inflammasome is triggered by low intracellular potassium concentration. Cell Death and Differentiation 14: 1583–1589.
Zhou, R., A. Tardivel, B. Thorens, I. Choi, and J. Tschopp. 2010. Thioredoxin-interacting protein links oxidative stress to inflammasome activation. Nature Immunology 11: 136–140.
Bouwman, R.A., R.J. Musters, B.J. van Beek-Harmsen, J.J. de Lange, R.R. Lamberts, S.A. Loer, and C. Boer. 2007. Sevoflurane-induced cardioprotection depends on PKC-alpha activation via production of reactive oxygen species. British Journal of Anaesthesia 99: 639–645.
Cruz, C.M., A. Rinna, H.J. Forman, A.L. Ventura, P.M. Persechini, and D.M. Ojcius. 2007. ATP activates a reactive oxygen species-dependent oxidative stress response and secretion of proinflammatory cytokines in macrophages. The Journal of Biological Chemistry 282: 2871–2879.
Yang, Q., H. Dong, J. Deng, Q. Wang, R. Ye, X. Li, S. Hu, and L. Xiong. 2011. Sevoflurane preconditioning induces neuroprotection through reactive oxygen species-mediated up-regulation of antioxidant enzymes in rats. Anesthesia and Analgesia 112: 931–937.
ACKNOWLEDGMENTS
The authors thank the Major Program of National Natural Science Foundation of China (81130036) and National Science Fund for Distinguished Young Scholars from National Natural Science Foundation of China (30825037).
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yue Jin and Hui Li contributed equally to this work.
Rights and permissions
About this article
Cite this article
Jin, Y., Li, H., Xie, G. et al. Sevoflurane Combined with ATP Activates Caspase-1 and Triggers Caspase-1-Dependent Pyroptosis in Murine J774 Macrophages. Inflammation 36, 330–336 (2013). https://doi.org/10.1007/s10753-012-9550-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-012-9550-6