Abstract
Acute lung injury (ALI) and the more severe acute respiratory distress syndrome (ARDS) are forms of pulmonary edema that result from robust local and systemic inflammatory states, such as sepsis. The morbidity and mortality associated with ALI and ARDS are significant and the treatment of these conditions presents a formidable challenge. Controlling hyperglycemia with insulin is a core component of patient management in the critically ill. Insulin treatment also exerts beneficial metabolic effects beyond glucose control, as well as non-metabolic effects, in insulin-resistant states. For instance, insulin inhibits NF-κB—dependent synthesis of pro-inflammatory factors and attenuates production of ROS. Indeed, intravenous administration of insulin ameliorates pulmonary injury and dysfunction in the LPS model of ALI. Most recently, an inhalable insulin formulation was shown to effectively reduce glucose concentrations with minimal impact on long-term pulmonary function. We propose that administering inhalable insulin to hyperglycemic ALI/ARDS patients could directly reduce alveolar inflammation while reducing circulating glucose levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Acute Lung Injury and Acute Respiratory Distress Syndrome
Pulmonary edema impairs oxygen diffusion from alveoli to pulmonary capillaries, resulting in hypoxemia and respiratory distress. The rapid onset of diffuse lung injury characterized by generalized pulmonary infiltrates and severe hypoxemiaFootnote 1 (PaO2:FiO2 ratio of <200 mmHg) in the absence of overt cardiac failure was first described as acute respiratory distress syndrome (ARDS) 40 years ago. Acute Lung Injury (ALI) includes cases with less severe hypoxemia (PaO2:FIO2 ratio between 200 and 300 mmHg) and was officially introduced as a diagnoses in the 1990s [1]. ALI and ARDS are clinical syndromes that are secondary to an underlying inflammatory state. The initial clinical disorder may affect and harm the lungs directly—as occurs in diffuse pneumonia, severe lung contusion, and aspiration of gastric contents, or may injure the lungs indirectly—such as in sepsis, non-thoracic trauma, and multiple blood transfusions. In either case, an injurious inflammatory response involving the capillary-alveolar unit ensues. Severe sepsis (due to pulmonary or extra-pulmonary infection) is the leading precedent of ALI/ARDS in North America and Europe [2, 3].
The core characteristic of ALI/ARDS—refractory hypoxemia, is caused by transudation of protein-rich fluid across pulmonary capillaries after damage of the endothelial and epithelial linings of the capillary-alveolar unit. Decreased lung compliance, an additional pathohysiologic feature of this condition that increases work of respiration, also results from accumulation of fluid in the interstitial and air spaces and from surfactant depletion. Specifically, a robust inflammatory response involving the endothelial and epithelial cells, as well as of leukocytes in the pulmonary vasculature, disrupts the structure and function of the capillary-alveoli unit. Sequestration of circulating neutrophils within the pulmonary vasculature is secondary to increased expression of pro-inflammatory cytokines (e.g., TNF-α), chemokines (e.g., IL-8), neutrophil chemokine receptors, leukocyte-endothelium adhesion molecules, and enzymes that produce inflammatory mediators (iNOS, COX-2, etc.) [1, 3]. The expression of these mediators is up-regulated by activation of the pivotal pro-inflammatory transcription factor, nuclear factor-kappa B (NF-κB). Neutrophils can then transmigrate into the interstitial and alveolar spaces (During inflammation, leukocyte transudation occurs across the pulmonary capillary endothelium, as opposed to the case in the systemic circulation). Adherent and infiltrating neutrophils are in an activated state; they up-regulate the inflammatory response and induce injury to endothelial and epithelial cells by release of reactive oxygen/nitrogen species (ROS/RNS), inflammatory mediators, and proteases. Circulating monocytes are next to arrive at the scene. They are transformed to macrophages after trans-endothelial migration, joining neutrophils and alveolar macrophages in production of inflammatory mediators. Of note, ALI and ARDS have a deleterious effect on distal organs not only due to hypoxemia, but as a result of spillover of inflammatory agents into the circulation as well. Given the pathophysiology of ALI/ARDS, an anti-inflammatory agent that does not impair immune clearance of microbes should attenuate endothelium-alveolar inflammation, inhibit transudation and exudation of leukocytes, and improve the mechanic (ventilation) and diffusion components of respiration. These effects would increase the delivery of oxygen and minimize that of inflammatory mediators to vital organs, ultimately reducing the dependence on mechanical ventilation and facilitate whole-body recovery from critical illness [1–4].
Insulin Exhibits Anti-inflammatory Properties
Transient hyperglycemia is highly prevalent in Intensive Care Unit (ICU) patients, even among those without prior diabetes mellitus (DM)—it is sometimes referred to as the “diabetes of injury.” The neuro-endocrine and inflammatory responses to critical illness induce counter-regulatory (i.e., hyperglycemic) pathways and antagonize insulin signal transduction (i.e., insulin resistance). The majority of studies support a significant correlation between the severity of disease/injury at onset, the degree of hyperglycemia, and morbidity/mortality in the critically ill. A high glucose concentration per se is injurious to multiple organs and exacerbates oxidative stress and inflammation. It is therefore mandatory to treat hyperglycemic ICU patients with insulin while frequently monitoring their glucose concentrations in order to minimize both hyperglycemia and hypoglycemia [4–6].
As is the case in ambulatory patients with DM, insulin therapy likely benefits hyperglycemic ICU patients through metabolic and non-metabolic effects other than increased glucose uptake by insulin-sensitive organs. Indeed, numerous cell types significantly express the insulin receptor. For instance, lipid and lipoprotein metabolism is dysregulated in DM and critical illness and responds to treatment with insulin [7–9]. In addition, insulin beneficially influences vasomotor tone and endothelial function through its divergent effects on the endothelial and inducible isoforms of nitric oxide (NO) synthase (eNOS and iNOS), which are augmented and inhibited by insulin, respectively. This facilitates the production of basal levels of NO while preventing over-production and is vasculo-protective in DM [10] and in sepsis [11, 12]. Another non-metabolic cell-type that responds to insulin is the myeloid-derived inflammatory cell, including the monocyte-macrophage, neutrophil, and resident-macrophage sub-types. Signaling through Akt (protein kinase B), insulin inhibits NF-κB activation and the consequent transcription of genes encoding inflammatory mediators, thereby exerting an anti-inflammatory effect. In addition, insulin treatment inhibits phagocyte NADPH oxidase, a major producer of ROS in inflammatory states [13–15]. Inhibition of NF-κB and ROS by insulin has also been reported in other cell types, such as the endothelium [16]. Insulin’s effect on NF-κB and ROS is opposed to that of glucose and free fatty acids (FFA)—increased levels of which induce inflammation and oxidative stress [17, 18]. The extent to which insulin plays a physiologic role in countering the inflammatory response is unclear. Still, pharmacologic doses of insulin appear to attenuate inflammation and oxidative stress in healthy individuals and those with metabolic derangements associated with obesity, by reducing glucose/FFA levels and by direct inhibition of NF-κB and NADPH oxidase [15].
Systemic administration of lipopolysaccharide (LPS, a.k.a. endotoxin, a component of the gram negative bacteria outer cell wall) to laboratory animals induces a state that simulates human sepsis and multiple organ dysfunction. LPS binds to its cognate receptor, the Toll-like receptor 4 (TLR4), which is expressed widely by inflammatory cells and signals to NF-κB and NADPH oxidase pathways. LPS thereby elicits a robust systemic inflammatory response that injures blood vessels and numerous organs. This preclinical model is therefore utilized to elucidate the pathophysiology of the human disease and to screen for potential therapeutic interventions. Treatment with insulin reduces oxidative stress and inflammation and confers protection to vital organs including the lungs (see below) in animal models of endotoxemia [19–22]. Insulin’s anti-inflammatory action is likely operative in critically ill patients as well [11].
Insulin Delivery through Inhalation
The unpleasantness of multiple daily injections motivated researchers to develop alternative strategies of delivering insulin to DM patients. Inhalation of pharmaceutical drugs efficiently targets pulmonary tissues, e.g., bronchodilators; particles of a small enough size may reach the alveoli and also enter the pulmonary vasculature. Indeed, inhaled insulin rapidly reaches the systemic circulation to exert its pharmacodynamic effect [23]. Unfortunately, the long-term use of several inhaled insulin systems resulted in a mild but significant impairment of pulmonary function, as evident by a decrease in FEV1 and carbon monoxide diffusion capacity. Of even greater concern, an increased incidence in lung cancer among previous smokers was noted following inhaled insulin use. These detrimental consequences of insulin inhalation may be secondary to activation of the pro-proliferative insulin-like growth factor (IGF-1) pathway. These findings dampened enthusiasm regarding the clinical utility of long-term treatment with inhaled insulin [24, 25]. Most recently, an inhaled insulin formulation (AFRESA, Mannkind Corp.) that efficiently controls hyperglycemia [26, 27] was reported to preserve airway function and pulmonary diffusion capacity [28, 29]. The product’s attractive safety profile may be in virtue of the insulin monomers (rather than oligomers) and the novel method of preparation employed in its preparation, both of which serve to augment delivery of insulin to the alveoli and its entrance to the capillaries [30].
Insulin is Protective in Experimental ARDS
In rodents, intra-tracheal or intravenous injection of lipopolysaccharide (LPS, a.k.a. endotoxin), a component of the gram negative bacteria outer cell wall, induces a pulmonary inflammatory state that recapitulates human ALI/ARDS. LPS elicits an inflammatory response that injures the lung in a manner that recapitulates human ALI/ARDS. This preclinical model is therefore utilized to elucidate the pathophysiology of the human disease and to screen for potential therapeutic interventions [31]. Intravenous or subcutaneous administration of insulin reproducibly ameliorates pulmonary inflammation, oxidative/nitrosative stress, tissue injury, and organ dysfunction in the LPS model of ALI [31–35]. Insulin also attenuated trauma-induced ALI [36] and inhibited NF-κB-dependent transcription of iNOS and COX-2 in LPS-stimulated alveolar macrophages [37].
Inhalable Insulin: Can it Treat Both Hyperglycemia and ALI/ARDS?
It appears that circulating insulin targets pulmonary-marginating leukocytes, as well as alveolar macrophage, epithelial, and endothelial cells, to down-regulate activation of NF-κB and NADPH oxidase by LPS and cytokines [38]. However, the reduced alveolar-capillary diffusion capacity likely limits the concentration of insulin that can be attained in the alveolar and peri-alveolar fluid. Inhaled insulin capable of reaching the alveoli may exert a local anti-inflammatory effect on exudated neutrophils and macrophages, alveolar macrophages and epithelial cells, as well as on the local endothelium. We hypothesize that early, short-term treatment of hyperglycemic ALI/ARDS patients with the novel inhaled insulin preparation may very well attenuate pulmonary inflammation without harming long-term lung function, while facilitating glycemic control.
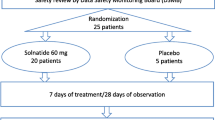
Cleary, the above hypothesis requires verification by preclinical and clinical studies. Animal studies may be employed to ascertain that insulin indeed reaches its site of action despite mechanical ventilation (as opposed to voluntary inhalation) and that it is indeed effective and safe. Researchers may assess the impact of administering inhalable insulin to ventilated, large mammals with ARDS. Outcomes could include lung weight, histopathology, oxidative and nitrosative stress, expression of inflammatory mediators, oxygenation and glucose levels, and variability. Since some survivors of ARDS develop a fibrotic lung disease fibroproliferative acute respiratory distress syndrome [39], long-term follow-up of animals will be necessary to rule out a potential IGF-1-like effect of insulin that may contribute to such a condition. Assuming positive findings in preclinical studies, a placebo-controlled study in patients could assess the effect of inhalable insulin on molecular and cellular inflammatory markers in broncho-alveolar fluid, oxygenation, lung compliance, length of ventilation, glucose control and variability, and long-term outcomes.
Notes
The ratio of the partial pressure of oxygen in arterial blood (PaO2) to the inspired oxygen fraction (FiO2) PaO2/FIO2 is a clinical measurement of oxygenation status and reflects overall function of the capillary-alveolar unit and matching of blood flow to ventilation.
References
Leaver, S.K., and T.W. Evans. 2007. Acute respiratory distress syndrome. BMJ 335(7616): 389–394.
Bernard, G.R., A. Artigas, K.L. Brigham, J. Carlet, K. Falke, L. Hudson, et al. 1994. The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. American Journal of Respiratory and Critical Care Medicine 149: 818–824.
Piantadosi, C.A., and D.A. Schwartz. 2004. The acute respiratory distress syndrome. Annals of Internal Medicine 141(6): 460–470.
Wheeler, A.P., and G.R. Bernard. 2007. Acute lung injury and the acute respiratory distress syndrome: a clinical review. Lancet 369(9572): 1553–1564.
Dungan, K.M., S.S. Braithwaite, and J.C. Preiser. 2009. Stress hyperglycaemia. Lancet 373(9677): 1798–1807.
Fahy, B.G., A.M. Sheehy, and D.B. Coursin. 2009. Glucose control in the intensive care unit. Critical Care Medicine 37(5): 1769–1776.
Hayashi, T., T. Hirano, T. Yamamoto, Y. Ito, and M. Adachi. 2006. Intensive insulin therapy reduces small dense low-density lipoprotein particles in patients with type 2 diabetes mellitus: relationship to triglyceride-rich lipoprotein subspecies. Metabolism 55(7): 879–884.
Mesotten, D., J.V. Swinnen, F. Vanderhoydonc, P.J. Wouters, and G. Van den Berghe. 2004. Contribution of circulating lipids to the improved outcome of critical illness by glycemic control with intensive insulin therapy. Journal of Clinical Endocrinology and Metabolism 89(1): 219–226.
Wendel, M., R. Paul, and A.R. Heller. 2007. Lipoproteins in inflammation and sepsis. II. Clinical aspects. Intensive Care Medicine 33(1): 25–35.
Muniyappa, R., M. Iantorno, and M.J. Quon. 2008. An integrated view of insulin resistance and endothelial dysfunction. Endocrinology and Metabolism Clinics of North America 37(3): 685–711.
Dandona, P., P. Mohanty, A. Chaudhuri, R. Garg, and A. Aljada. 2005. Insulin infusion in acute illness. Journal of Clinical Investigation 115(8): 2069–2072.
Langouche, L., I. Vanhorebeek, D. Vlasselaers, S. Vander Perre, P.J. Wouters, K. Skogstrand, T.K. Hansen, and G. Van den Berghe. 2005. Intensive insulin therapy protects the endothelium of critically ill patients. Journal of Clinical Investigation 115(8): 2277–2286.
Dandona, P., A. Aljada, P. Mohanty, H. Ghanim, W. Hamouda, E. Assian, and S. Ahmad. 2001. Insulin inhibits intranuclear nuclear factor kappaB and stimulates IkappaB in mononuclear cells in obese subjects: evidence for an anti-inflammatory effect? Journal of Clinical Endocrinology and Metabolism 86(7): 3257–3265.
Aljada, A., H. Ghanim, P. Mohanty, N. Kapur, and P. Dandona. 2002. Insulin inhibits the pro-inflammatory transcription factor early growth response gene-1 (Egr)-1 expression in mononuclear cells (MNC) and reduces plasma tissue factor (TF) and plasminogen activator inhibitor-1 (PAI-1) concentrations. Journal of Clinical Endocrinology and Metabolism 87: 1419–1422.
Dandona, P., A. Chaudhuri, P. Mohanty, and H. Ghanim. 2007. Anti-inflammatory effects of insulin. Current Opinion in Clinical Nutrition and Metabolic Care 10(4): 511–517.
Aljada, A., H. Ghanim, R. Saadeh, and P. Dandona. 2001. Insulin inhibits NFkappaB and MCP-1 expression in human aortic endothelial cells. Journal of Clinical Endocrinology and Metabolism 86(1): 450–453.
Aljada, A., P. Mohanty, H. Ghanim, T. Abdo, D. Tripathy, A. Chaudhuri, and P. Dandona. 2004. Increase in intranuclear nuclear factor kappaB and decrease in inhibitor kappaB in mononuclear cells after a mixed meal: evidence for a proinflammatory effect. American Journal of Clinical Nutrition 79(4): 682–690.
Evans, J.L., I.D. Goldfine, B.A. Maddux, and G.M. Grodsky. 2003. Are oxidative stress-activated signaling pathways mediators of insulin resistance and beta-cell dysfunction? Diabetes 52(1): 1–8.
Dugo, L., M. Collin, D.A. Allen, O. Murch, S.J. Foster, M.M. Yaqoob, and C. Thiemermann. 2006. Insulin reduces the multiple organ injury and dysfunction caused by coadministration of lipopolysaccharide and peptidoglycan independently of blood glucose: role of glycogen synthase kinase-3beta inhibition. Critical Care Medicine 34(5): 1489–1496.
Jeschke, M.G., H. Rensing, D. Klein, T. Schubert, A.E. Mautes, U. Bolder, and R.S. Croner. 2005. Insulin prevents liver damage and preserves liver function in lipopolysaccharide-induced endotoxemic rats. Journal of Hepatology 42(6): 870–879.
Kidd, L.B., G.A. Schabbauer, J.P. Luyendyk, T.D. Holscher, R.E. Tilley, M. Tencati, and N. Mackman. 2008. Insulin activation of the phosphatidylinositol 3-kinase/protein kinase B (Akt) pathway reduces lipopolysaccharide-induced inflammation in mice. Journal of Pharmacology and Experimental Therapeutics 326(1): 348–353.
Hagiwara, S., H. Iwasaka, A. Hasegawa, H. Koga, and T. Noguchi. 2008. Effects of hyperglycemia and insulin therapy on high mobility group box 1 in endotoxin-induced acute lung injury in a rat model. Critical Care Medicine 36(8): 2407–2413.
Guntur, V.P., and R. Dhand. 2007. Inhaled insulin: extending the horizons of inhalation therapy. Respiratory Care 52(7): 911–922.
Kling, J. 2008. Inhaled insulin’s last gasp? Nature Biotechnology 26(5): 479–480.
Mitri, J., and A.G. Pittas. 2009. Inhaled insulin–what went wrong. Nat Clin Pract Endocrinol Metab 5(1): 24–25.
Rave, K., T. Heise, A. Pfützner, and A.H. Boss. 2008. Coverage of postprandial blood glucose excursions with inhaled technosphere insulin in comparison to subcutaneously injected regular human insulin in subjects with type 2 diabetes. Diabetes Care 30(9): 2307–2308.
Rosenstock, J., R. Bergenstal, R.A. Defronzo, I.B. Hirsch, D. Klonoff, A.H. Boss, D. Kramer, R. Petrucci, W. Yu, B. Levy, and 0008 Study Group. 2008. Efficacy and safety of Technosphere inhaled insulin compared with Technosphere powder placebo in insulin-naive type 2 diabetes suboptimally controlled with oral agents. Diabetes Care 31(11): 2177–2182.
Bergenstal et al. Comparative Efficacy and Safety of AFRESA™ and a Rapid-Acting Analog Both Given with Glargine in Subjects with T1DM in a 52-Week Study. Abstract # 479-P, ADA conference 2009. http://ww2.aievolution.com/ada0901/index.cfm?do = abs.viewAbs&abs = 6624 accessed October 2009.
ADA 2009: New Inhaled Insulin Has Rapid Onset of Action With No Adverse Effect on Lung Function. Medscape Medical News. http://www.medscape.com/viewarticle/704092. accessed October 2009.
HOW DOES THE TECHNOSPHERE® INSULIN SYSTEM WORK? http://www.mannkindcorp.com/technosphere_insulin.aspx. accessed July 13 2009.
Gonzalez, P.K., J. Zhuang, S.R. Doctrow, B. Malfroy, P.F. Benson, M.J. Menconi, and M.P. Fink. 1996. Role of oxidant stress in the adult respiratory distress syndrome: evaluation of a novel antioxidant strategy in a porcine model of endotoxin-induced acute lung injury. Shock 6(Suppl 1): S23–S26.
Martins, J.O., F.L. Zanoni, D.O. Martins, R. Coimbra, J.E. Krieger, S. Jancar, and P. Sannomiya. 2009. Insulin regulates cytokines and intercellular adhesion molecule-1 gene expression through nuclear factor-kappaB activation in LPS-induced acute lung injury in rats. Shock 31(4): 404–409.
de Oliveira, M.J., A.R. Meyer-Pflug, T.C. Alba-Loureiro, H. Melbostad, J.W. Costa da Cruz, R. Coimbra, R. Curi, and P. Sannomiya. 2006. Modulation of lipopolysaccharide-induced acute lung inflammation: role of insulin. Shock 25(3): 260–266.
Chen, H.I., D.Y. Yeh, H.L. Liou, and S.J. Kao. 2006. Insulin attenuates endotoxin-induced acute lung injury in conscious rats. Critical Care Medicine 34(3): 758–764.
Alba-Loureiro, T.C., E.F. Martins, R.G. Landgraf, S. Jancar, R. Curi, and P. Sannomiya. 2006. Role of insulin on PGE2 generation during LPS-induced lung inflammation in rats. Life Sciences 78(6): 578–585.
Donnelly, M., C. Condron, P. Murray, and D. Bouchier-Hayes. 2007. Modulation of the glycemic response using insulin attenuates the pulmonary response in an animal trauma model. Journal of Trauma 63(2): 351–357.
Martins, J.O., M. Ferracini, N. Ravanelli, R.G. Landgraf, and S. Jancar. 2008. Insulin suppresses LPS-induced iNOS and COX-2 expression and NF-kappaB activation in alveolar macrophages. Cellular Physiology and Biochemistry 22(1–4): 279–286.
Honiden, S., and M. N. Gong. 2009. Diabetes, insulin, and development of acute lung injury. Critical Care Medicine, Jun 15. [Epub ahead of print.
Krein, P.M., P.J. Sabatini, W. Tinmouth, F.H. Green, and B.W. Winston. 2003. American Journal of Respiratory and Critical Care Medicine 167(1): 83–90.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shapiro, H., Kagan, I., Shalita-Chesner, M. et al. Inhaled Aerosolized Insulin: A “Topical” Anti-inflammatory Treatment for Acute Lung Injury and Respiratory Distress Syndrome?. Inflammation 33, 315–319 (2010). https://doi.org/10.1007/s10753-010-9187-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-010-9187-2