Abstract
—Histamine is widely distributed in the lungs and increases capillary permeability and P-selectin expression. To observe the role of histamine in acute lung injury (ALI), we measured the histamine and protein concentrations and cell numbers in the bronchoalveolar lavage (BAL) of LPS-induced ALI in rats. We instilled LPS (3 mg/kg) intratracheally, in conjunction with the intravenous histamine receptor antagonists (mepyramine, a H1-receptor antagonist, or ranitidine, a H2-receptor antagonist). LPS increased protein concentration and neutrophil numbers in the BAL as well as myeloperoxidase (MPO) activity in lungs after 6 h. LPS also increased histamine concentration in BAL after 2 h. Mepyramine and ranitidine attenuated the increased histamine concentrations. Total cell number in the BAL and MPO activity in the lungs were significantly decreased and neutrophil numbers and protein concentration in the BAL seemed to decrease with the administration of ranitidine at 6 h. In conclusion, endogenous histamine might be involved in the recruitment of neutrophils and protein leaks in LPS-induced ALI via the H2 receptors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute lung injury (ALI) is characterized by increased alveolar-capillary permeability with acute, bilateral pulmonary edema and severe hypoxia [1]. Sepsis, arising as a consequence of exposure to bacterial lipopolysaccharide (LPS), is one of the main contributing factors to the development of ALI [2]. Activated neutrophils may play a central role in its pathogenesis by releasing several inflammatory mediators in sepsis-induced ALI [3–6].
Histamine is widely distributed on the mast cells surrounding pulmonary vasculatures. It has been considered to be an important mediator in many immunologic and inflammatory responses. Histamine can constrict or dilate pulmonary vasculatures and increase capillary permeability [7]. It is involved in endothelial cell injury and the migration of neutrophils to tissues [8–12]. Histamine reacts on its receptors on vascular endothelial cells [13] and increases the expression of P-selectin, which influences the migration of neutrophils to the tissues or endothelial cell surfaces [14, 15]. In addition, histamine induces interleukin (IL)-8, a potent neutrophil chemoattractant secreted by endothelial cells [16], and increases the chemokinesis of neutrophils [9]. Moreover, the release of endogenous histamine from the mast cells around pulmonary vasculature is increased by IL-1, a main proinflammatory cytokine in the pathophysiology of sepsis [17, 18]. We previously reported that, in Sprague–Dawley rats, histamine, administered in conjunction with TNF-α or IL-1, augmented the TNF-α- or IL-1-induced infiltration of neutrophils into the lung tissues and increased neutrophil numbers in the BAL fluid after 5 h. There was, however, no additional increase in the leakage of the pulmonary vasculature [19]. It can be assumed, therefore, that endogenous histamine may be involved in sepsis-induced ALI. However, the role of histamines on the pathogenesis of ALI has not been thoroughly addressed.
At least three different types of histamine receptors are distributed on several cells in the lung tissues. The H1 receptors are involved in bronchoconstriction and pulmonary vascular constriction, and the H2 receptors mediate mild bronchodilation, mucus release, and pulmonary vascular relaxation [20]. H1 receptors are known to be the main receptors involved in the increased permeability of the alveolar capillary endothelial cells [21], meanwhile, H2 receptors also seem to be involved in the increased permeability of alveolar epithelial cells [22]. We hypothesized that histamine could be involved in the mechanism of LPS-induced neutrophil infiltration in lung tissues leading to an increase in capillary permeability in rats. To address this hypothesis, this study aimed to 1) examine whether LPS increases endogenous histamine production, 2) observe the effect of co-treatment of histamine receptor antagonists on neutrophil infiltration into the lung tissue, and 3) determine their effect on capillary permeability in LPS-induced ALI. In this study, we evaluated the degree of neutrophil infiltration by measuring the number of neutrophils in the BAL fluid and myeloperoxidase (MPO) activity in the lung tissue. Measurement of the protein and histamine concentrations in the BAL fluid assessed the capillary permeability in the lung tissue and the degree of endogenous histamine production.
Materials and Methods
Experimental Animals
Species pathogen-free(SPF) male Sprague–Dawley rats (Section of Laboratory Animals, Asan Institute for Life Science, Seoul, Korea) weighing 270–370 g were used for this investigation. Rats were fed a controlled diet (Sam-yang Feed Company, Seoul, Korea) and were housed in cages before the experiment. The Animal Care Committee of the Asan Institute for Life Science approved the experimental protocol. The rats were cared for and handled according to the guidelines of the National Health Institute.
Experimental Design
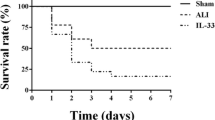
Rats were divided into six groups with eight animals in each group: 1) a saline (control) group of rats, administered 0.5 ml saline intratracheally, 2) a lipopolysaccharide (LPS) group, administered 3 mg/kg body weight of LPS (Escherichia coli lipopolysaccharide, 055;B5, Sigma Chemical Co., St. Louis, MO, USA) in 0.5 ml saline intratracheally, 3) the two histamine receptor antagonist treatment groups, treated intravenously with either the H1 receptor antagonist mepyramine (pyrilamine, Sigma Chemical, St. Louis, MO, USA) at a dose of 10 mg/kg of body weight (H1RA/saline group) [8] or with the H2 receptor antagonist ranitidine (Zantac®:Glaxo Smith Kleine, USA) at a dose of 10 mg/kg of body weight (H2RA/saline group) [8] with intratracheal saline infusion, and 4) the two histamine receptor antagonist/LPS co-treatment groups, treated by mepyramine (LPS/H1RA group) or by the H2 receptor antagonist ranitidine (LPS/H2RA group) just before LPS instillation. The doses of histamine receptor antagonists were chosen based on several reports used histamine as the mediators of inflammation [8, 9]. Recent evidence indicates that a sufficient inflammatory response can be induced in the lung 6 h after LPS treatment, demonstrable as neutrophil accumulation in the lung and neutrophil oxidant burst in the lung [23]. Therefore, we examined the rats 6 h after LPS treatment.
Experimental Process
Rats underwent intraperitoneal instillation of ketamine (45 mg/kg, Boerhinger Ingelheim, St. Joseph, MO, USA) and xylazine (3 mg/kg, Haver, NY, USA) while enflurane was administered by inhalation. Subsequently, normal saline or LPS with or without histamine receptor antagonists via trachea or vein was administered. Air was infused with a 3-ml syringe two times to ensure delivery of the drugs into the lung tissues after intratracheal instillation of normal saline or LPS. Rats were kept awake so that they would be active until the next experiment. Five hours and 50 min after the treatment, anesthesia was induced again by intraperitoneal administration of ketamine (90 mg/kg) and xylazine (7 mg/kg). A 16-gauge stub adaptor tube was then inserted into the trachea and connected with a ventilator. Then, 200 U of heparin were injected via the right ventricle after an open thoracotomy and laparotomy. The venous blood from the right ventricle was obtained and centrifuged at 3,000 rpm for 10 min and stored as plasma. Heart and lungs were extracted during the perfusion of phosphate-buffered saline (PBS) by an infusion pump (masterflex pump, Cole-Parmer Instrument Co. Barrington, IL, USA). The extracted lung tissues were stored immediately at −70°C until myeloperoxidase (MPO) activity could be measured. Control rats received identical anesthesia and surgery. To minimize experimental bias, we treated six rats simultaneously, one from each of the separate six groups throughout the whole experiment.
Acquisition of the BAL Samples for Measurement of Histamine Concentrations and Cell Numbers
At 1, 2, and 6 h after LPS administration, we inserted a 16-gauge stub adaptor tube into the trachea of the rats after the induction of anesthesia. BAL samples were recovered from the airway lumen by flushing the airways with 6 ml of saline delivered through the tracheal cannula and retrieved. This collection procedure was repeated three times. The BAL samples from each group were then centrifuged at 1,400 rpm for 10 min, and then aliquots from the supernatants were frozen at −60°C and used for the measurements. Centrifuged BAL cell pellets were resuspended in 1 ml of supernatant. The total cell number was measured by hemocytometer and the percentage of neutrophils was counted after cytospin and Wright stain.
Measurement of Histamine Concentrations in Plasma and BAL Samples
We obtained the plasma and BAL samples from each group at 1, 2, and 6 h and measured the histamine concentration by automatic photometry using the Astoria Analyzer Series 300 (Clackamas, OR, USA) [24].
Measurement of the Activity of Myeloperoxidase (MPO) in Lung Tissues
The lung tissues were homogenized by Vertishear tissue homogenizer (Virtis, Gardiner, NY, USA) using 4 ml of phosphate buffer. The samples were then centrifuged using the Sorvall RC-5B refrigerated centrifuge (Dupont Instruments, Irving, TX, U.S.A.) at 4°C with 30,000 g for 30 min. After the acquisition of pellets, 4 ml of phosphate buffer and 0.5% hexadecyl—trimethyl ammonium bromide were added to the pellets, which were then sonicated with Kontes micro-ultrasonic cell disrupter (Vineland, NJ, USA). The broken samples were heated for 2 h at 60°C to inactivate the tissue MPO inhibitors. The activity of MPO was measured by spectrometry using O-dianisidine [25].
Measurement of the Indices of Lung Inflammation and Injury
The protein concentrations of plasma and BAL were measured by the bicinchoninic acid (BCA) method [26].
Statistical Analysis
Data are presented as mean ± standard error of the means. The comparison between groups was performed with the nonparametric Kruskal–Wallis test and Mann–Whitney U test using SPSS 11.0 (SPSS Inc., Chicago, IL, USA). A p value of <0.05 was considered significant.
Results
The Effects of LPS on Histamine Concentration in BAL Fluid
Figure 1A shows the histamine concentration in the BAL fluids from rats sacrificed after 1, 2 and 6 h of saline or LPS intratracheal instillation. The histamine concentrations were similar in all time periods for the saline control group. In the LPS group, histamine concentration in the BAL fluid was significantly higher at 2 h than in the control group (p = 0.016), and returned to baseline at 6 h. In the H1RA/saline group and H2RA/saline groups, histamine concentrations were also similar in all the time periods, showing no significant difference when compared to control group. In the H1RA/LPS group, the histamine concentration at 6 h was significantly higher than in the control group (p = 0.002). When compared to the H1RA/saline group, the histamine concentration seemed to be higher in the H1RA/LPS group (at 1 h: p = 0.028, at 6 h: p = 0.05) without any significant difference compared to the LPS group. At 2 h after the treatment, the histamine concentration in the H1RA/LPS group was significantly lower than in the LPS group (p = 0.015). The histamine concentrations in the H2RA/LPS group showed no significant difference in any of the time periods compared with the control group or the H2RA/saline group. Two hours after the treatment, the histamine concentration in the H2RA/LPS group was significantly lower than that in the LPS group (p = 0.005). The decrease of the histamine concentration compared to the LPS group was more prominent in the H2RA/LPS group than in the H1RA/LPS group.
The Effects of LPS on Histamine Concentration in Plasma
Figure 1B shows the histamine concentration in the plasma. The histamine concentrations in the plasma were similar in all time periods for the saline control group. In the LPS group: histamine concentration showed no significant difference compared with the control group. The histamine concentration in the H1RA/saline group was higher than in the control group at 6 h after the treatment (p = 0.001). In the H2RA/saline group, histamine concentrations in the plasma were significantly higher at all the time periods (p = 0.006, p = 0.028, and p = 0.001 in each). In the H1RA/LPS group, the histamine concentration at 6 h was significantly higher than in the control group (p = 0.001) without showing any significant difference with the H1RA/saline group. When compared to the LPS group, the histamine concentration in the H1RA/LPS group showed no significant difference. The histamine concentration in the H2RA/LPS group showed no significant difference compared to the H2RA/saline control group or the LPS group for all measured time periods.
Total Cell Numbers in BAL Fluid
Figure 2A shows the total cell numbers in the BAL fluid in all six groups of animals. In the saline control group, the total cell number showed no significant change according to the time process. In the LPS group, the total cell number was significantly higher than in the control groups at 6 h (p = 0.001). In the H1RA/saline group and the H2RA/saline group, the total cell numbers showed no significant difference when compared to the control group at any time. In the H1RA/LPS group, the total cell number was significantly higher than in the H1RA/saline group at 6 h (p < 0.000). But, when compared with the LPS group, there was no difference in total cell number at 6 h. In the H2RA/LPS group, the total cell number was significantly higher than in the H2RA/saline group at 6 h (p = 0.004). When compared with LPS group, however, the total cell number in the H2RA/LPS group was significantly lower than that in the LPS group (p = 0.038).
Total cell number (A) and Neutrophil number (B) in BAL fluids (BALF) at 1, 2 and 6 h after the intratracheal dose of saline or lipopolysaccharide (LPS) in different groups. ★ or # represents that p values were less than 0.05 as compared to the saline control group (★) or LPS group (#). + represents that p values were less than 0.05 as compared to the matched control group.
Neutrophil Numbers in BAL Fluid
Figure 2B shows the neutrophil numbers in the BAL fluid in all six groups of animals. In the saline control group, the neutrophil numbers showed no significant change according to the time process. In the LPS group, the neutrophil number was significantly higher than in the control groups at 6 h (p = 0.001). In the H1RA/saline group and the H2RA/saline group, the neutrophil number showed no significant difference from the control group at any time. In the H1RA/LPS group, neutrophil number was significantly higher than in the H1RA/saline group at 2 and 6 h (p = 0.001, p < 0.000 each). When compared with the LPS group, there was no difference in neutrophil number at any time. In the H2RA/LPS group, the neutrophil number was significantly higher than that of the H2RA/saline group at 2 and 6 h (p = 0.021, p = 0.000 each). When compared with the LPS group, the neutrophil number showed a tendency to decrease (p = 0.053).
Total Protein Concentrations in BAL Fluid
Total protein concentrations in the BAL fluids at the same time periods are shown in Fig. 3. In the saline control group, the total protein concentration showed no interval change during the entire time process. In the LPS group, total protein concentration was significantly higher at 6 h compared to the control group (p = 0.000). In the H1RA/saline and H2RA/saline groups, the total protein concentrations showed no significant differences with the control group at any time. In the H1RA/LPS group, the total protein concentration was significantly higher than that of the H1RA/saline group (p = 0.000). The H1RA/LPS group also showed no significant difference compared with the LPS group. In the H2RA/LPS group, the total protein concentration showed no significant difference compared to the control and H2RA/saline groups. The H2RA/LPS group did, however, tend to be lower than the LPS group at 6 h (p = 0.05).
MPO Activities in the Lung Tissues
The MPO activities of all six groups, examined as an indicator of neutrophil infiltration and activity in lung tissues, are shown in Fig. 4. MPO activity in the saline control group, expressed as the median and range, was 5.6 (3.82–7.96) U/g. In the LPS group, the MPO activity [25.10 (15.33–42.09)] was higher than in the control group (p = 0.000). The MPO activity in rats treated with histamine receptor antagonists were 4.18 (3.24–10.80) U/g in the H1RA/saline group and 5.22 (3.16–10.31) U/g in the H2RA/saline group, respectively, showing no significant difference compared to the control group. In the H1RA/LPS group, the MPO activity [23.13, (16.28–45.01)] was significantly higher than in the control group but not significantly different compared with the LPS group. The MPO activity [13.99 (4.88–20.89)] in the H2RA/LPS group, however, was significantly lower than the LPS group (p < 0.01).
Levels of MPO activity in lung tissues at 6 h after intratracheal LPS instillation in different groups. Lines within the box indicate median (dashed) and mean (solid) values; Whiskers indicate the minimum and maximum values. ★ or # represent that p values were less than 0.05 as compared to the saline control group (★) or LPS group (#).
Discussion
It is known that neutrophils accumulate in the lungs of ARDS patients and play a central role in experimental models of ALI [27]. Because neutrophils should initially be recruited before participating in ALI, chemotactic factors that elicit neutrophil migration are important. Histamine is abundantly distributed in lung and increases the expression of P-selectin [13], which is involved in neutrophil migration to tissues at the surface of the vascular endothelial cells [14, 15]. Furthermore, histamine has been reported to increase the release of IL-8 [16] and the chemokinesis of neutrophils via other pathways like phospholipase C and nitric oxide synthase isozymes [10]. Therefore, it can be assumed that endogenous histamine may be involved in neutrophil accumulation in ALI. The role of histamine in ALI, however, has not been well elucidated. We used a LPS-induced ALI model to observe the effect of endogenous histamines on ALI because activated neutrophils seem to be essential in the pathogenesis of sepsis-induced ALI [3–6].
As a first step, to estimate the effect of LPS on endogenous histamine production, we measured the histamine concentrations in BAL fluid and plasma. Histamine concentration in BAL fluid was significantly elevated 2 h after LPS instillation compared to that of the control group in our study, suggesting that LPS may augment endogenous production of histamine. This is supported by results showing that the co-treatment of histamine receptor antagonists attenuated the increased histamine production in BAL fluids by LPS instillation. In the case of plasma histamine concentration in the LPS group, there was no significant difference compared with the control.
When we measured histamine concentration in BAL fluids after administration of histamine receptor antagonists without LPS, no definite effect of histamine blockade was found. This might reflect the local production of histamine in the lung did not affected by use of receptor antagonists in usual condition. On the other hand, histamine concentration in plasma was elevated with H2RA treatment from 1 h after LPS or saline instillation and onward. The plasma histamine concentration was higher in the H2RA/saline group than in the control group from 1 h onward, and significantly higher at 6 h in the H1RA/saline group. However, when comparing the histamine receptor antagonist/LPS co-treatment group to the LPS group, we found no significant difference. One possible explanation for the higher plasma histamine concentration in the H2RA/saline group might be that histamine degradation might be lowered by H2 receptor antagonist. Histamine methyl transferase (HMT), one of the two important enzymes involved in histamine metabolism, is possibly inhibited by typical H1 and H2 histamine receptor antagonists [20]. HMT is also widely distributed in the lung tissue. Therefore, the action of HMT could partly explain the changes in the plasma histamine concentrations.
The mechanism by which LPS increases the endogenous histamine concentration is not certain. It has been reported that LPS increases production of many pro-inflammatory cytokines like TNF-α or IL-1β. Histamine release from basophils or mast cells is increased with cytokines like IL-1β, IL-3 or GM-CSF [12, 28]. The pro-inflammatory cytokines released by LPS, therefore, might play an important role in the release of histamines.
We compared the neutrophil numbers in BAL fluids and MPO activities in the lung tissues of rats treated by LPS with or without histamine receptor antagonists to find the relationship between the increased endogenous histamine production and the neutrophil accumulation in the lungs of our model. We found that ranitidine, a kind of H2 receptor antagonist, tends to decrease the elevated neutrophil numbers in BAL fluid. We also found that ranitidine significantly decreased the elevated MPO activity in lung tissue by LPS in this model. These results suggest that endogenous histamine may be involved in the neutrophil infiltration in lung tissues via the H2 receptor, which is distributed most widely in the endothelial cells [13]. In the literature, the augmentation of neutrophil infiltration by histamine in the lung tissues, along with IL-8 administration, were blocked only by mepyramine, an H1 receptor antagonist [8], and the increased neutrophil activity by histamines was via the activation of the H2 receptor [10]. The increase in the production of IL-8 by histamine, however, was blocked by H1 and H2 receptor antagonists in the endothelial cells [16]. According to these results (including ours), the involved histamine receptors would be different depending on the experimental models. It is well known that the importance of inflammatory mediators responding to LPS varies with the design of the studies, the origin of LPS production, the method of LPS delivery (e.g., intravenous, intratracheal, or intraperitoneal administrations) and even with the strain of animals studied [27].
We thought that the increases in neutrophil numbers 2 h after in LPS + H1RA, LPS + H2RA group compared with their matched control (saline + H1RA, saline + H2RA in each) might be mainly due to LPS effect because there were no significant differences in the comparison of either between saline only and saline with the histamine receptor antagonists groups or between LPS group and LPS with the histamine receptor antagonists groups. The possibility of an additional effect of the two histamine receptor antagonists in the recruitment of neutrophils at 2 h after LPS treatment seems to be remote, because there were no significant differences in between LPS group and LPS with the histamine receptor antagonists groups.
Because neutrophils were known to perform their main action on the acute vascular and lung epithelial permeability induced by LPS, and because H2 receptor was involved in the histamine induced acute lung leak [22], we expected that the H2 receptor antagonist would attenuate the acute leak in our model by decreasing the neutrophil infiltration in the lung tissues. If so, the H2 receptor antagonist can have a very important clinical implication. Patients with ALI often receive preventive measures for stress ulcers during ventilatory support. In clinical practice, surface coating agents such as sucralfate or an H2 histamine receptor antagonist such as ranitidine have been administered for this purpose. If an H2 histamine receptor antagonist can attenuate the ALI via modulation of neutrophilic inflammation, it could be more strongly and primarily considered for the prevention of stress ulcers in patients with ALI. In our model, the H2 receptor antagonist tends to attenuate acute protein leaks by LPS. It did not, however, reach statistical significance (p = 0.05). The H2 receptor antagonist, therefore, did not definitely attenuate the acute protein leak in our model. This result suggests that the dose of histamine receptor antagonist administered in our study could not definitively modulate the recruited neutrophils' toxic action or, alternatively, that endogenous histamine may not have important role in the pathogenesis of LPS-induced ALI.
In our data, the histamine concentration in the BAL fluid increased at 2 h. The total cell and neutrophil number and the protein concentration in BAL fluid showed peak levels at 6 h after LPS instillation. Pro-inflammatory cytokines like TNF-α, IL-1β and some chemokines, like CINC-1 and MIP-2, are increased 2∼4 h after aerosol delivery or intratracheal instillation of moderate doses of LPS [27, 29]. It is suggested that the histamine could increase the cytokines or chemokines along with the stimulation of LPS by an uncertain mechanism or vice versa, with resultant neutrophil recruitment. Because we did not measure the levels of pro-inflammatory cytokines or chemokines, we could not prove the relationship of histamine and cytokines or chemokines in our model. Alternatively, histamines could recruit neutrophils by increased P-selectin expression.
The increase of endogenous histamine in BAL fluid was not sustained in our model, which might suggest that the effect of intratracheal LPS on endogenous histamine production is temporary. The preventive effect of histamine receptor antagonists for recruitment of neutrophils could be limited to only around 2 h. These results, then, suggest that histamine may be sufficient but not necessary for the recruitment of inflammatory cells into the lung following the LPS challenge.
In conclusion, endogenous histamines might be involved in the recruitment of neutrophils in LPS-induced ALI via the H2 receptor. Its role in ALI, however, would not be important in this model.
References
Bernard, G. R., A. Artigas, K. L. Brigham, J. Carlet, K. Falke, L. Hudson, M. Lamy, J. R. LeGall, A. Morris, and R. Spragg. 1994. Report of the American–European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. Am. J. Respir. Crit. Care Med. 149:818–824
Brigham K. L., and B. Meyrick. 1986. LPS and lung injury. Am. Rev. Respir. Dis. 133:913–927
Pugin J., B. Ricou, K. P. Steinberg, P. M. Suter, and T. R. Martin. 1996. Proinflammatory activity in bronchoalveolar lavage fluids from patients with ARDS, a prominent role for interleukin-1. Am. J. Respir. Crit. Care Med. 153:1850–1856
Jorens, P. G., J. Van Damme, W. De Backer, L. Bossaert, R. F. De Jongh, A. G. Herman, and M. Rampart. 1992. Interleukin-8 (IL-8) in the bronchoalveolar lavage fluid from patients with the adult respiratory distress syndrome (ARDS) and patients at risk for ARDS. Cytokine 4:592–597
Armstrong, L., and A. B. Millar. 1997. Relative production of tumor necrosis factor alpha and interleukin 10 in adult respiratory distress syndrome. Thorax. 52:442–446
Parsons, P. E., M. Moss, J. L. Vannice, E. E. Moore, F. A. Moore, and J. E. Repine. 1997. Circulating IL-1β and IL-10 concentrations are increased but do not predict the development of acute respiratory distress syndrome in at-risk patients. Am. J. Respir. Crit. Care Med. 155:1469–1473
Ahmed, T., K. B. Mirbahar, J. W. Oliver, P. Eyre, and A. Wanner. 1982. Characterization of H1 and H2 receptor function in pulmonary and systemic circulations of sheep. J. Appl. Physiol. 53:1765–1784
Perretti, M., T. G. Harris, and R. J. Flower. 1994. A role for endogenous histamine in interleukin-8-induced neutrophil infiltration into mouse air-pouch: investigation of the modulatory action of systemic and local dexamethasone. Br. J. Phamacol. 112:801–808
Yamaki, K., H. Thorlacius, X. Xie, L. Lindbom, P. Hedqvist, and J. Raud. 1998. Characteristics of histamine-induced leukocyte rolling in the undisturbed microcirculation of the rat mesentery. Br. J. Pharmacol. 123:390–399
Schaefer, U., A. Schneider, D. Rixen, and E. Neugbauer. 1998. Neutrophil adhesion to histamine stimulated cultured endothelial cells is primarily mediated via activation of phospholipase C and nitric oxide synthase isozymes. Inflamm. Res. 47:256–264
Anderson, R., A. Glover, and A. R. Rabson. 1977. The in vitro effects of histamine and metiamide on neutrophil motility and their relationship to intracellular cyclic nucleotide concentrations. J. Immunol. 118:1690–1697
Alam, R, J. B. Welter, P. A. Forsythe, M. A. Lett-Brown, and J. A. Grant 1989. Comparative effect of recombinant IL-1, -2, -3, -4 and 6, IFN-γ, GM-CSF, TNF and histamine-releasing factors on the secretion of histamine from basophils. J. Immunol. 142:3431–3435
Simionescu, N, C. Heltianu, F. Antohe, and M. Simionescu. 1982. Endothelial cell receptors for histamine. Ann. NY Acad. Sci. 401:132–149
Jones, D. A., O. Abbassi, L. V. McIntire, R. P. McEver, and C. W. Smith. 1993. P-selectin mediates neutrophil rolling on histamine-stimulated endothelial cells. Biophys. J. 65:1560–1569
Kubes, P., and S. Kanwar. 1994. Histamine induces leukocyte rolling in post-capillary venules. A P-selectin-mediated event. J. Immunol. 152:3570–3577
Jeannin, P., Y. Delneste, P. Gosset, and A. B. Tonnel. 1994. Histamine induces Interleukin-8 secretion by endothelial cells. Blood 84:2229–2233
Subramanian, N., and M. A. Bray 1987. Interleukin-1 releases histamine from human basophils and mast cells in vitro. J. Immunol. 138:271–275
Liu, M. C., D. Proud, L. M. Lichtenstein, D. W. MacGlashan Jr., R. P. Schleimer, N. F. Adkinson Jr., A. Kagey-Sobotka, E. S. Schulman, and M. Plaut. 1986. Human lung macrophage-derived histamine-releasing activity is due to IgE-dependent factors. J. Immunol. 136:2588–2595
Koh, Y. S., B. M. Hybertson, E. K. Jepson, M. J. Kim, C. M. Lim, S. D. Lee, W. S. Kim, D. S. Kim, and W. D. Kim. 1996. The study for the roles of intratracheally administered histamine in the neutrophil-mediated acute lung injury in rats. Tuberculosis and Lung Diseases 43:308–322
Rangachari, P. K. 1992. Histamine: mercurial messenger in the gut(editorial). Am. J. Physiol. 2621(1 Pt 1):G1–G13
Barnes, P. J. 1991. Histamine receptors in the lung. Agents Actions 33:103–122
Braude, S., D. Royston, C. Coe, and P. J. Barnes. 1984. Histamine increases lung permeability by an H2-receptor mechanism. Lancet. 2:372–374
Bloomfield, G. L., S. Holloway, P. C. Ridings, B. J. Fisher, C. R. Blocher, M. Sholley, T. Bunch, H. J. Sugerman, and A. A. Fowler. 1997. Pretreatment with inhaled nitric oxide inhibits neutrophil migration and oxidative activity resulting in attenuated sepsis-induced acute lung injury. Crit. Care Med. 25:584–593
Siraganian, R. P. 1974. An automated continuous flow system for the extraction and fluorometric analysis of histamine. Anal. Biochem. 57:383–394
Krawisz, H. E., P. Sharon, and W. F. Stenson. 1984. Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Gastroenterology 87:1344–1350
Smith, P. K., R. I. Krohn, G. T. Hermanson, A. K. Mallia, F. H. Gartner, M. D. Provenzano, E. K. Fujimoto, N. M. Goeke, B. J. Olson, and D. C. Klenk. 1985. Measurement of protein using bicinchoninic acid. Anal. Biochem. 150:76–85
Jasson, A. H., C. Eriksson, and X. Wang. 2004. Lung inflammatory responses and hyperinflation induced by an intratracheal exposure to lipopolysaccharide in rats. Lung 182:163–171
Subramanian, N., and M. A. Bray. 1987. Interleukin 1 releases histamine from human basophils and mast cells in vitro. J. Immunol. 138:271–275
Haddad, E. B., K. McCluskie, M. A. Birrell, D. Dabrowski, M. Pecoraro, S. Underwood, B. Chen, G. T. De Sanctis, S. E. Webber, M. L. Foster, and M. G. Belvisi. 2002. Differential effects of Ebselen on neutrophil recruitment, chemokine, and inflammatory mediator expression in a rat model of lipopolysaccharide-induced pulmonary inflammation. J. Immunol. 169: 974–982
Acknowledgments
This work was supported by the Korea Research Foundation (2001-F00158) and research fund of Hanyang University (2003).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, TH., Yoon, H.J., Lim, C.M. et al. The Role of Endogenous Histamine on the Pathogenesis of the Lipopolysaccharide (LPS)-Induced, Acute Lung Injury: A Pilot Study. Inflammation 29, 72–80 (2005). https://doi.org/10.1007/s10753-006-9001-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-006-9001-3