Abstract
Microsatellite instability (MSI) is a genetic consequence of a MisMatch Repair defect in colorectal cancer (CRC). We compared clinicopathohistological features with MSI status of CRC and evaluated prognostic significance of MSI status and BRAF mutation in the group of MSI-H tumors. 155 primary CRCs were excised surgically, 2006–2008. MSI analysis was carried out using a fluorescence-based pentaplex polymerase chain reaction technique. BRAF mutation (V600E) was analyzed by direct sequencing in MSI-H tumors. For all patients were evaluated: age, gender, localization, tumor cell type, tumor differentiation, mucin production, lymphocytic infiltration (TILs) and TNM stage. Patients’ disease-free survival (DFS) was compared according to MSI and BRAF status using Kaplan–Meier test. Of the 155 CRCs, 19 (12.3%) were MSI-H, and 136 (87.7%) were MSS/L. BRAF mutations were found in 4 of the MSI-H tumors. Patients with MSI-H CRC had lower recurrence rate (log rank test; P = 0.04) than MSS/L group. Patients with MSI-H tumor and BRAF mutation had worse DFS than MSI-H tumors without this mutation (log rank test; P = 0.01). Most of the clinicopathologic characteristics of MSI-H CRC in Serbian patients are similar to those reported in previous studies. Patients with MSI tumor phenotype had favourable prognosis, but in those with BRAF mutation higher recurrence rate was observed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Back in the 1998, Boland and colleagues reviewed the microsatellite instability (MSI) mechanism that has opened a new chapter in the biology of colorectal carcinoma (CRC) (Boland et al. 1998). MSI is a genetic consequence of a MisMatch Repair (MMR) defect in cells unable to repair errors occurring in DNA during replication, mostly at the level of repeat sequences called microsatellites. This phenomenon has attracted attention in colorectal cancer as well as in other tumor sites owing to the clinical implications associated with it. Almost all cases of Lynch syndrome which are hereditary nonpolyposis colorectal cancer (HNPCC) and approximately 15% of sporadic colon cancer cases demonstrate MSI. Several studies have demonstrated improved survival rates in patients with CRC whose tumors demonstrate MSI. (Malesci et al. 2007; Banerjea et al. 2009; Ng and Schrag 2010). The mechanism by which these tumors lead to a more favourable prognosis is unclear. Other studies found no MSI influence on survival (Lamberti et al. 2007; Westra et al. 2005; Carethers et al. 2004). These tumors also have different response to 5-FU based chemotherapy, less metastasis, more frequent extra-colorectal cancers and more frequent metachronous CRCs (Ward et al. 2001; Ribic et al. 2003; Shitoh et al. 2002). CRC with high frequency MSI (MSI-H), both hereditary and sporadic, are characterized by preferential location in the proximal colon, diploid nuclear DNA content, high prevalence of mucinous and medullary histotypes, and poor differentiation (Shitoh et al. 2002). The BRAF oncogene has been linked to the MSI pathway in tumorogenesis. BRAF mutations in sporadic CRC with MSI are more frequently detected than those in microsatellite stable cancers (MSS) (Deng et al. 2004) and are contributed to poor prognosis (Samowitz et al. 2005).
Aims of study were to examine clinicopathohistological features of CRC in Serbian cohort with/without MSI, to evaluate MSI status impact on disease course as well as BRAF mutation in group of patients with MSI-H tumors.
Materials and methods
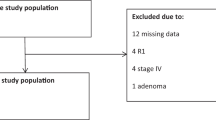
Patients
One hundred and fifty five primary CRCs were excised surgically at Digestive Surgery Clinic, Clinical Centre of Serbia, Belgrade, 2006–2008. Three patients had two metachronous or other extracolonic tumor associated with Lynch syndrome. Four patients had two synchronous tumors and only main tumor (more invasive or larger sized) was taken for MSI analysis. Patients treated by preoperative radiotherapy or chemotherapy, those with inflammatory bowel disease or a known history of familial adenomatous polyposis were excluded. We defined the time of surgery as time zero and follow the cohort up to September 2011 in term of any disease recurrence (local or distant). The main outcome was a disease-free survival (DFS) according to MSI status and BRAF mutated (mt) versus wild type (wt) in the MSI-H cases. Information about the clinical outcome was obtained by the periodic controls or direct telephone interview with the patients or their families. This study was approved by the Ethics Committee of the Clinical Centre of Serbia.
Clinicopathological analysis
Six parameters were determined for all tumors: localization (right, left colon and rectum), tumor cell type, tumor differentiation, mucin production, lymphocytic infiltration (TILs) and TNM (UICC) stage. Determination was performed independently by two experienced pathologists blinded to MSI status of tumors.
All tumors were histologically classified as adenocarcinomas. TILs are graded as none (0) or present (1). Tumors were classified as positive TILs if at least 5 lymphocytes were observed at least one of 10 high-power fields (Jass 2007). Mucin content was scored from 1 to 3 (score 1, 2 and 3 for tumor mucin volume 0–33%, 33–66% and 66–100%, respectively). Tumor differentiation was classified as poor (1), moderate (2) and well (3).
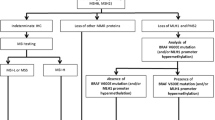
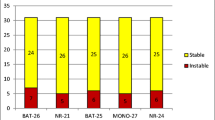
Analysis of microsatellite instability
Fresh representative tissue samples from all tumors were immediately frozen at −80°C. The genomic DNA was extracted using standard methods. We used five quasimonomorphic mononucleotide repeats and Pentaplex polymerase chain reaction (PCR) for evaluating of microsatellite tumor status as described Suraweera et al. (2002), Buhard et al. (2004). The microsatellite markers used in this study were BAT25, BAT26, NR-21, NR-22, NR-24. MSI analysis was carried out using a fluorescence-based PCR and run in an ABI PRISM 377 (Applied Biosystems, USA) automated DNA sequencer. Tumors were classified as MSI-H if three or more of five markers showed MSI, and MSI-L, if only one or two markers showed MSI. MSS tumors were characterized by the absence of MSI in all 5 markers. MSI positive markers were reexamined at least twice to confirm the result.
Analysis of BRAF mutation
DNA samples were screened for mutations in exon 15 of the BRAF gene. Exon 15 was amplified by PCR using the forward primer 5′-TGCTTGCTCTGATAGGAAAATG-3′ and the reverse primer 5′-TTTTGGCCCTGAGATGCTG-3′. These primers were previously designed with the Primer3 Input program (http://frodo.wi.mit.edu/cgi-bin/primer3-web-cgi-bin0.4.0/primer3_results.cgi). PCR conditions were as follows: denaturation at 95°C for 11 min followed by 30 cycles at 95°C for 30 s, annealing at 55°C for 30 s, and 72°C for 30 s, and a final extension at 72°C for 5 min. PCR products were bidirectionally sequenced in capillary electrophoresis (ABI PRISM Genetic Analyzer 3130; Applied Biosystems, USA) using the aforementioned primers. We have analyzed BRAF mutation (V600E) in colorectal cancers that showed MSI.
Statistics
Statistical analysis was performed between groups using independent sample T test to analyze numerical parameters, or asymptotic Chi-square and Chi-square likelihood ratio test for non-parametric data. Results are expressed as mean + SD where appropriate for parametric data. Significant P value was P < 0.05 and highly significant when P < 0.01. Multivariate logistic regression, method forward stepwise—Wald, with Bonferroni’s correction, was used to test an association of MSI with sets of five variables such as pathological (mucin production, TILs, differentiation, TNM stage) and patient`s characteristics (tumor localization). We estimated the odd ratio (OR) with confidence interval (CI) 95% using Cochran Mantel Haneszel test. Recurrence-free probabilities and survival curve were generated using the Kaplan–Meier method. The log-rank test was used for the statistical differences. The statistical package SPSS was used to analyze all data.
Results
Microsatellite status in tumors
Out of the 155 colorectal cancers, 19 (12.3%) were MSI-H, and 136 (87.7%) patients were MSS/MSI-L.
The clinical and pathological characteristics of the patients are given in Table 1. Of 155 tissue samples analyzed, 93 were from males and 62 from females. These were subdivided into two groups by MSI testing: MSS/MSI-L and MSI-H group. The mean age in MSS/MSI-L and MSI-H group was 61.65 and 62 years, respectively. The majority of the MSI-H group were males (73.5%) (Table 2). There was no statistically significant difference between MSI status and gender.
Location of the primary lesion
A total of 28 of the 155 lesions were located in the proximal, right colon (18.5%). The prevalence of proximal lesions in the MSI-H group (53%) was higher than in the MSS/MSI-L group (13%). The difference was highly statistically significant (OR 7.3, P = 0.001, CI 95%) (Table 1).
MSI and pathohistological characteristics
Differentiation
Most of the tumors were well and moderate differentiated, 47.1 and 41.9% respectively. The percentage of poor differentiated tumors was slightly lower in the MSS/MSI-L group (9%) when compared to the MSI-H group (26.5%), but the difference did not reach statistical significance (χ2, P = 0.053).
Mucin production in tumor
Among 155 samples, 1.9% (3 patients) were negative (absence of mucin production), 131 patients (84.5%) had focal mucin production (up to 66% tumor volume), and 21 tumors (13.5%) were predominantly mucin producing. The percentage of MSI-H lesions, which were predominantly mucin producing (37%) was higher than mucin producing lesions in the MSS/MSI-L group (10%). The odds ratio of patients with mucin production higher than 33% having MSI-H was 3.42 times that of the patients without mucin production (OR 3.42, P = 0.011, CI 95%). Interestingly, focal mucin production up to 33% of tumor volume was often in MSS/MSI-L group (70%), difference was statistically significant (χ2, P = 0.018). Mucin production (>33% tumor volume) as well as tumor localization (right colon) were highly predictive features for MSI-H tumors according multivariate logistic regression model with Bonferroni’s correction (overall percentage for model prediction 91%, Nagelkerke R2 = 0.345) P values, 0.003 and 0.006, respectively.
Lymphocytic infiltration in tumor
In 98 tumors (63.2%), there was no TILs. TILs were slightly more frequent in group with MSI-H tumors than in MSS/MSI-L, 53 and 34.5% respectively, but with no statistical significance (OR 2.1, P = 0.132, CI 95%).
UICC staging
The majority of patients in our series were stage II and III, 36.8 and 42.6% respectively. Only one patient in MSI-H group had IV disease stage, metastatic disease in moment of operation. There was no statistically significant differences in the stage of the lesions between MSI-H and MSS/MSI-L groups (χ2, P = 0.336). UICC stage, TILs and tumor differentiation in our model, mentioned above, do not predict MSI-H tumors (P values 0.57, 0.06 and 0.12, respectively).
MSI and BRAF mutation
Analyzing BRAF status in MSI tumors (H and L), we found four patients with MSI-H tumor who had BRAF mt. In group with MSI-L tumor we did not found BRAF mutation. Three of the 4 mutated tumors were localized in proximal colon, without tumor infiltrating lymphocytes, with high percentage of mucin content in tumor.
Survival analysis
Median follow up of the patients after surgery was 31 months (range 10–60 months). 21 patients with CRC in stage IV did not undergo curative surgery; they were then excluded from the recurrences free probabilities estimation. DFS of patients exhibiting the MSI-H phenotype was statistically significantly better than patients with MSS/L tumor (log rank test 4.2; P = 0.04) (Fig. 1). Patients with MSI-H tumor and BRAF mutation (n = 4) had statistically significant lower DFS i.e. higher recurrence rate than MSI-H tumors with BRAF wt (log rank test 6.7; P = 0.01). Two patients with MSI-H and BRAF mutation tumor had recurrent disease and no one in the group with MSI-H tumor without BRAF mutation.
Discussion
In this paper we described the MSI status in a cohort of CRC patients from Serbia. Of the 155 CRC, 19 (12.3%) were MSI-H and 136 (87.8%) were MSS/L (Table 1). 14/93 (15%) of the CRC in men and 5/62 (8%) of them in women were MSI-H. Taken together, our results demonstrated that MSI-H cancers were more frequent in males than females (probably because of more males in the series), and more frequent than MSS/L tumors in patients with proximal colon and tumors with high level of mucin production. As in another study (Ishikubo et al. 2004), we observed that the frequency of MSI-H rectal cancer is significantly higher in men than women (men: 85% vs. women: 15%) (Table 2). Women were somewhat more likely to have the MSI-H cancers in proximal lesions (men: 42% vs. women: 80%) (Table 3).
The other clinicopathological features known to be associated with the presence of MSI include poorly differentiated cancers (Kazama et al. 2007, 2008) and presence of lymphocytic infiltration in tumor (TILs) (Greenson et al. 2009). In this study of Serbian patients, primary tumor localization and presence of mucinous component are in accordance with previous publications (Kazama et al. 2007, 2008; Greenson et al. 2009; Jenkins et al. 2007). However, the degree of differentiation and percentage of TILs presence in our series was different. Although in some studies the presence of lymphocytic infiltrates was indicative of MSI in tumors, the largest number of patients with MSI in our series had no TILs. The majority of MSI-H tumors in our group of patients were found in moderate or poorly differentiated tumors as compared to the MSS/L group, the difference being near statistical significance (26.5% in MSI-H vs. 9% in MSS/L, P = 0.053).
The most controversial group are patients with tumors that show low level of microsatellite instability (MSI-L) i.e. microsatellite instability in one or two microsatellite markers. We detected 8 MSI-L tumors in our series (4 men and 4 women). Four patients had rectal cancer, and 4 cases were left colon cancers. In this group, one patient had less than 50 years and only one patient had metastatic disease at the time of surgery. A number of these tumors had no lymphocyte infiltration and all patients except one had well differentiated adenocarcinoma. Most of these tumors had stage III disease (60%) and no BRAF mt was detected in this subgroup. Yearsley et al. (2006) found no difference between MSI-L versus MSS using clinical and histological parameters such as percentage of mucin, histological type, grade, and lymphoid host response. Moreover, its molecular characteristics are more similar to those from MSS than MSI-H tumors (Pawlik et al. 2004). Accordingly, no statistical significance was found between group of MSI-L and MSS in any examined parameter in our patients.
MSI-H tumors may be sporadic or hereditary. Association of MSI and BRAF mutations is strongly indicator of a sporadic origin (Domingo et al. 2004; McGivern et al. 2004; Deng et al. 2004). In our series of 19 MSI-H tumors, 4 (21%) are likely sporadic. The remaining 15 cases could be either sporadic or hereditary depending of their MMR gene defect: methylation of the MLH1 promoter for sporadic cases and germline MMR mutation for hereditary cases.
Our patients with MSI-H and BRAF-mt tumors experienced significantly lower DFS in comparison with those with MSI-H and BRAF-wt primary tumors. Similar results have been reported regarding the prognostic significance of BRAF mutations in patients with early stage CRC (Saridaki et al. 2010; French et al. 2008). Conflicting data regarding the prognosis of MSI tumors exist. Our study showed the favourable prognosis of the microsatellite unstable CRCs. Only one patient with MSI-H tumor had metastatic disease at the time of surgery, and one patient experienced relapse. These survival data confirms that the MSI mechanism is associated with less aggressive tumor biology. Most of these patients had disease stage II and III, 9 and 8 patients respectively. Of particular interest are patients in stage II, given that microsatellite status may dictate further treatment of these patients.
The main limitation of our study was the small number of patients with BRAF mutation, as well as an inability to perform analysis of BRAF mutation in microsatellite stable CRC.
In conclusion, most of the clinicopathologic characteristics of MSI-H lesions in our study of Serbian patients are similar to those reported in previous studies, including the location of the primary tumor and extent of mucin production. However, most of the MSI-H tumors in our study group were well and moderately-differentiated with no lymphocytic infiltration in tumor tissue. MSI phenotype is linked to favourable CRC prognosis, contrary to BRAF mutation indicating a higher recurrence rate in MSI-H CRC.
For the first time the microsatellite status of colorectal tumors in a large number of patients in our country is determined. Moreover, the analysis of the MMR defect discriminating sporadic from hereditary MSI-H cases needs to be developed in order to be able to recognize Lynch cases in Serbia.
References
Banerjea A, Hands RE, Powar MP, Bustin SA, Dorudi S (2009) Microsatellite and chromosomal stable colorectal cancers demonstrate poor immunogenicity and early disease recurrence. Colorectal Dis 11(6):601–608. doi:10.1111/j.1463-1318.2008.01639
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW et al (1998) A National Cancer Institute workshop on microsatellite instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58:5248–5257
Buhard O, Suraweera N, Lectard A, Duval A, Hamelin R (2004) Quasimonomorphic mononucleotide repeats for high-level microsatellite instability analysis. Dis Markers 20(4–5):251–257. doi:10.1200/JCO.2005.02.7227
Carethers JM, Smith EJ, Behling CA et al (2004) Use of 5-fluorouracil and survival in patients with microsatellite-unstable colorectal cancer mismatch repair proficiency and in vitro response to 5-fluorouracil. Gastroenterology 126:394–401. doi:10.1053/j.gastro.2003.12.023
Deng G, Bell I, Crawley S, Gum J, Terdiman J, Allen B et al (2004) BRAF mutation is frequently present in sporadic colorectal cancer with methylated hMLH1, but not hereditary nonpolyposis colorectal cancer. Clin Cancer Res 10:191–195. doi:10.1158/1078-0432.CCR-1118-3
Domingo E, Laiho P, Ollikainen M, Pinto M, Wang L, French AJ et al (2004) BRAF screening as a low-cost effective strategy for simplifying HNPCC genetic testing. J Med Genet 41:664–668. doi:10.1136/jmg.2004.020651
French AJ, Sargent DJ, Burgart LJ, Foster NR, Kabat BF, Goldberg R et al (2008) Prognostic significance of defective mismatch repair and BRAF V600E in patients with colon cancer. Clin Cancer Res 14(11):3408–3415. doi:10.1158/1078-0432.CCR-07-1489
Greenson JK, Huang S, Herron C, Moreno V, Bonner J, Tomsho LP (2009) Pathologic predictors of microsatellite instability in colorectal cancer. Am J Surg Pathol 33(1):126–133. doi:10.1097/PAS.0b013e31817ec2b1
Ishikubo T, Nishimura Y, Yamaguchi K, Khansuwan U, Arai Y, Kobayashi T et al (2004) The clinical features of rectal cancers with high-frequency microsatellite instability (MSI-H) in Japanese males. Cancer Lett 216:55–62. doi:10.1016/j.canlet.2004.07.017
Jass JR (2007) Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology 50:113–130. doi:10.1111/j.1365-2559.2006.02549
Jenkins MA, Hayashi S, O’Shea AM, Burgart LJ, Smyrk TC, Shimizu D et al (2007) Pathology features in Bethesda guidelines predict colorectal cancer microsatellite instability: a population-based study. Gastroenterology 133(1):48–56. doi:10.1053/j.gastro.2007.04.044
Kazama Y, Watanabe T, Kanazawa T, Tanaka J, Tanaka T, Nagawa H (2007) Microsatellite instability in poorly differentiated adenocarcinomas of the colon and rectum: relationship to clinicopathological features. J Clin Pathol 60(6):701–704. doi:10.1136/jcp.2006.039081
Kazama Y, Watanabe T, Kanazawa T, Tanaka J, Tanaka T, Nagawa H (2008) Poorly differentiated colorectal adenocarcinomas show higher rates of microsatellite instability and promoter methylation of p16 and hMLH1: a study matched for T classification and tumor location. J Surg Oncol 97(3):278–283. doi:10.1002/jso.20960
Lamberti C, Lundin S, Bogdanow M et al (2007) Microsatellite instability did not predict individual survival of unselected patients with colorectal cancer. Int J Colorectal Dis 22(2):145–152. doi:10.1007/s00384-006-0131-8
Malesci A, Laghi L, Bianchi P, Delconte G, Randolph A, Torri V et al (2007) Reduced likelihood of metastases in patients with microsatellite-unstable colorectal cancer. Clin Cancer Res 13(13):3831–3839. doi:10.1158/1078-0432.CCR-07-0366
McGivern A, Wynter CV, Whitehall VL, Kambara T, Spring KJ, Walsh MD et al (2004) Promoter hypermethylation frequency and BRAF mutations distinguish hereditary non-polyposis colon cancer from sporadic MSI-H colon cancer. Fam Cancer 3:101–107. doi:10.1023/B:FAME.0000039861.30651.c8
Ng K, Schrag D (2010) Microsatellite instability and adjuvant fluorouracil chemotherapy: a mismatch? J Clin Oncol 28(20):3207–3210. doi:10.1200/JCO.2010.28.9314
Pawlik TM, Raut CP, Rodriguez-Bigas MA (2004) Colorectal carcinogenesis: MSI-H versus MSI-L. Dis Markers 20:199–206
Ribic CM, Sargent DJ, Moore MJ, Thibodeau SN, French AJ, Goldberg RM et al (2003) Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 349:247–257. doi:10.1056/NEJMoa022289
Samowitz WS, Sweeney C, Herrick J, Albertsen H, Levin TR, Murtaugh MA et al (2005) Poor survival associated with the BRAF V600E mutation in microsatellite-stable colon cancers. Cancer Res 65:6063–6069. doi:10.1158/0008-5472.CAN-05-0404
Saridaki Z, Papadatos-Pastos D, Tzardi M, Mavroudis D, Bairaktari E et al (2010) BRAF mutations, microsatellite instability status and cyclin D1 expression predict metastatic colorectal patients’ outcome. Br J Cancer 102:1762–1768. doi:10.1038/sj.bjc.6605694
Shitoh K, Konishi F, Miyakura Y, Togashi K, Okamoto T, Nagai H (2002) Microsatellite instability as a marker in predicting metachronous multiple colorectal carcinomas after surgery. Dis Colon Rectum 45:329–333. doi:10.1007/s10350-004-6177-1
Suraweera N, Duval A, Reperant M, Vaury C, Furlan D, Leroy K et al (2002) Evaluation of tumor microsatellite instability using five quasimonomorphic mononucleotide repeats and pentaplex PCR. Gastroenterology 123(6):1804–1811. doi:10.1053/gast.2002.37070
Ward R, Meagher A, Tomlinson I, O’Connor T, Norrie M, Wu R et al (2001) Microsatellite instability and the clinicopathological features of sporadic colorectal cancer. Gut 48:821–829. doi:10.1136/gut.48.6.821
Westra J, Schaapveld M, Hollema H et al (2005) Determination of TP53 mutation is more relevant than microsatellite instability status for the prediction of disease-free survival in adjuvant-treated stage III colon cancer patients. J Clin Oncol 23:5635–5643. doi:10.1200/JCO.2005.04.096
Yearsley M, Hampel H, Lehman A, Nakagawa H, de la Chapelle A, Frankel WL (2006) Histologic features distinguish microsatellite high from microsatellite-low and microsatellite-stable colorectal carcinomas, but do not differentiate germline mutations from methylation of the MLH1 promoter. Hum Pathol 37:831–838. doi:10.1016/j.humpath.2006.02.009
Acknowledgments
This work was supported by Ministry of Science; Republic of Serbia: Grant No 41033.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Markovic, S., Antic, J., Dragicevic, N. et al. High-frequency microsatellite instability and BRAF mutation (V600E) in unselected Serbian patients with colorectal cancer. J Mol Hist 43, 137–143 (2012). https://doi.org/10.1007/s10735-011-9387-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10735-011-9387-6