Abstract
The cellular DNA mismatch repair (MMR) pathway, involving the DNA mismatch repair genes MLH1 and MSH2, detects and repairs DNA replication errors. Defects in MSH2 and MLH1 account for most cases of hereditary non-polyposis colorectal cancer as well as for sporadic colorectal tumors. Additionally, increased expression of MSH2 RNA and/or protein has been reported in various malignancies. Loss of DNA MMR in mammalian cells has been linked to resistance to certain DNA damaging agents including clinically important cytotoxic chemotherapeutics. Due to other functions besides its role in DNA repair, that include regulation of cell proliferation and apoptosis, MSH2 has recently been shown to be of importance for pathogenesis and progression of cancer. This review summarizes our present understanding of the function of MSH2 for DNA repair, cell cycle control, and apoptosis and discusses its importance for pathogenesis, progression and therapy of cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
MSH2 and DNA mismatch repair
The MSH2 gene is a component of the highly conserved post-replicative DNA mismatch repair system. DNA mismatch repair (MMR) proteins contribute to DNA replication fidelity by removing insertion/deletion loops that result from template primer slippage at repetitive DNA sequences, and by correcting single base mismatches that escape polymerase proofreading, thereby preventing the accumulation of spontaneous mutations and ensuring the integrity and stability of the genome (Quinn et al. 1995; Charames and Bapat 2003; Muller and Fishel 2002).
The MMR-System is best described in Escherichia coli. It consists of the proteins MutS, MutL, MutH and Uvr. MutS detects mismatches in DNA duplexes and initiates the MMR machinery (Wagner and Meselson 1976; Cox et al. 1972). It makes a connection between the recognition of a mismatch and the excision of the mismatch from the strand within which it is contained (Sancar and Hearst 1993). This is done by the interaction of a MutL homodimer with MutS (Galio et al. 1999) where it stimulates the endonuclease activity of MutH (Hall and Matson 1999). MutL also loads UvrD, a DNA helicase II that unwinds the DNA duplex from the nick generated by MutH (Dao and Modrich 1998; Hall et al. 1998) onto the DNA. In eukaryotes, MutS and MutL are represented by multiple orthologs. The MutS homodimer is represented by two heterodimers consisting of MSH2/MSH6 and MSH2/MSH3. The MSH2/MSH6 heterodimer recognizes single base mismatches and short insertion–deletion loops in the DNA. On the other hand the MSH2/MSH3 heterodimer recognizes larger loops. (Genschel et al. 1998; Umar et al. 1998). MutL is also represented in the eukaryotes by several heterodimers. There are four homologs of MutL in both yeast and mammals, MLH1 and Pms2 bind to form a MutL heterodimer. In addition, MLH3 and Pms1 dimerize with MLH1, however little is known about their role in response to DNA-damage (Kramer et al. 1989; Prolla et al. 1994; Wang et al. 1999a, b; Hafe et al. 2000a). Extensive genetic studies in yeast have failed to find orthologs of MutH and UvrD in the MMR system, and there may be no homolog of these two proteins in the eukaryotic genome (Hafe and Robertson 2000b).
MSH2 and cancer
The implication of MSH2 in the pathogenesis of cancer is well recognized. MSH2 and MLH1 are the most frequently impaired genes in hereditary non-polyposis colorectal cancer (HNPCC) (Quinn et al. 1995; Charames et al. 2003; Muller and Fishel 2002), a familial condition with a predisposition to cancers of the colon, endometrium, stomach, ovary, and biliary tracts (Lynch et al. 1998). Additionally, MSH2 mutations have been detected in sporadic tumors of the colon (Lothe et al. 1993), endometrium (Caduff et al. 1996), stomach (Renault et al. 1996), head and neck (Field et al. 1995), and prostate (Watanabe et al. 1996).
It has been shown that approximately 30–70% of patients with a clinical diagnosis of HNPCC have a germline mutation in one of the MMR genes, most commonly in MLH1 or MSH2, less often in PMS1, PMS2, or MSH6 (Aaltonen et al. 1998; Bapat et al. 1999; Leach et al. 1993; Liu et al. 1996; Wheeler et al. 2000). Carriers of mutations in MLH1 or MSH2 have up to a 70–80% lifetime risk of developing colorectal cancer (Aarnio et al. 1999; Boland 2000; Vasen et al. 1996). Tumors with MMR abnormalities have a common phenotype charcterized by microsatellite instability (MSI). MSI is a genetic mechanism important in the development of various human cancers that is characterized by length changes at repetitive loci scattered throughout the genome (Loeb 1994; Fishel et al. 1993).
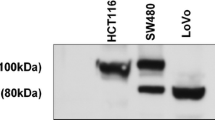
It has been demonstrated that the majority of inactivating mutations in the MSH2 gene leads to a lack of expression or the expression of a truncated protein not detectable by the antibody (clone FE11) used in many studies (Thibodeau et al. 1996; Leach et al. 1996; Katabuchi et al. 1995; Shia et al. 2004). Therefore, it has been suggested that the immunohistochemical analysis of MSH2 protein in tumor tissues may be a useful screen for the detection of defective MSH2 mediated mismatch repair. Due to the fact that antibody staining is more available as compared to DNA analysis in a clinical setting, it has been speculated that the use of immunohistochemistry (IHC) may offer a relatively convenient and rapid technique for prescreening tumors for defects in the expression of mismatch repair genes (Thibodeau et al. 1996; Leach et al. 1996; Shia et al. 2004). In conclusion, it has been shown that malignancies with inactivating mutations in the MSH2 gene may lack MSH expression.
Increased expression of MSH2 in malignancies
On the other hand, findings reported in the literature indicate that MSH2 expression is elevated at least in a part of neoplasm that have no inactivating mutation in the MSH2 gene. Increased expression of MSH2 RNA and/or protein has been reported in various malignancies (Srivastava et al. 2004; Leach et al. 2000; Hamid et al. 2002; Hussein et al. 2002, 2006; Aubry et al. 2001; Castrilli et al. 2002; Rass et al. 2001). However, the underlying mechanisms that cause increased levels of MSH2 in malignancies are still unknown. It has been hypothesized that the up-regulation of MSH2 levels may be related to the genomic instability in malignant tumors or may be related to an increased cell proliferation rate. Elevated levels for MSH2 have been shown to be associated with increased proliferation both in malignant and benign tissues (Srivastava et al. 2004; Leach et al. 2000; Hamid et al. 2002; Aubry et al. 2001; Castrilli et al. 2002; Rass et al. 2001). IHC staining of Glioblastoma shows an increased number of cells staining positively for MSH2 in highly proliferating Grade IV glioblastoma multiforme (GBM) as compared with Grade II astrocytoma (AS) (Srivastava et al. 2004). Leach et al. (2000) reported that MSH2 expression was increased in both high- and low-grade urothelial neoplasms, as compared to normal tissues. In other studies, 24 cases of endometrial cancer (70.8%) showed strong immunopositivity for hMSH2 (Hamid et al. 2002) and positive immunostaining of MLH1 and MSH2 was detected in all 33 bronchioalveolar carcinomas investigated (Aubry et al. 2001). IHC in salivary gland tumors for the expression of MSH2 and MLH1 revealed immunopositivity in all primary tumor samples studied, with the carcinomas showing a much higher proportion of MSH2 and MLH1 positive cells as compared with low-grade pleomorphic adenomas (Castrilli et al. 2002). In malignant melanoma and its metastases, Rass et al. (2001) observed a much higher protein and mRNA expression of MSH2, as compared to benign acquired melanocytic nevi.
In prostate cancer a higher Gleason score significantly correlated with higher MSH2 expression. Low MSH2 expression correlated with increased overall, disease free survival (Prtilo et al. 2005).
MSH2, growth stimulation, cell cycle progression and apoptosis
As mentioned before, it has been speculated that the elevated expression of MSH2 in malignancies may be associated with a higher rate of cell proliferation. An increased expression of MSH2 during cell proliferation was documented by Marra et al. (1996). This increase was, overall constant throughout the cell cycle, decreasing slightly in G1 and early S phase, but increasing in replicative and post-replicative cells. Additionally, MSH2 protein expression varies in the normal endometrium throughout the menstrual cycle and is positively correlated to protein expression of the proliferation marker proliferating cell nuclear antigen (PCNA) (Hamid et al. 2002). In the normal endometrium, both glandular cells and stromal cells in the functional layer enter the cell cycle actively during the proliferative phase of the menstrual cycle. In the secretory phase, only stromal cells maintain cell proliferation. The expression of MSH2 protein in the glandular cells of the functional layer was obviously positive in the proliferative phase. In contrast, weak to negative expression of this protein was found in the glandular cells in the secretory phase. In normal endometrium, expression of MSH2 protein in the glandular cells of the functional layer changes during the menstrual cycle. In summary, these findings indicate that the MSH2 protein is induced in association with cell proliferation. Leach et al. (1996) reported consistent findings in the normal digestive tract. In their study, they reported that MSH2 expression was confined to the replicative compartment in the epithelium of the digestive mucosa, namely, the basal zone, in the esophagus of the bottom half of the crypts in the small or large intestinal mucosa. Taken together, it is possible to speculate that MSH2 protein expression is controlled under the influence of cell cycle regulation. In tissues with high proliferative activity, such as digestive mucosa or endometrium, the increase in MSH2 protein expression may be required to protect cells from DNA replication errors. Other authors speculated that the elevated expression of MSH2 in malignancies may be due to an induction of MSH2 expression by the p53 protein. In malignant melanocytic tumors, an increased MSH2 expression was shown to be associated with high levels of p53 protein. DNA damage through UV irradiation has been shown to cause p53 dependent activation of MSH2 transcription (Scherer et al. 1996).
Since DNA is continuously exposed to genotoxic stresses, the DNA repair systems must continuously monitor and repair damaged DNA. Findings published previously indicate that the association of MSH2 expression with proliferation may be related to MSH2-induced cell cycle progression or growth stimulation. It has been demonstrated that MSH2 is induced by overexpression of the transcription factor E2F, which plays crucial roles in cell growth control (Iwanaga et al. 2004). Moreover, MSH2 is markedly induced by growth stimulation in fibroblasts that were rendered quiescent by serum starvation and then stimulated to re-enter into the cell cycle synchronously by the addition of serum (Iwanaga et al. 2004). Additionally, MSH2 protein expression is increased in normal peripheral blood lymphocytes when cell proliferation is induced by mitogen stimulation (Iwanaga et al. 2004). The induction of MLH1, MSH2 and Rad51 genes by growth stimulation is conceivable because the lesions to be repaired are produced more frequently during DNA replication. It is expected that a higher MMR gene expression than needed for mismatch correction is required for checkpoint activation to stop the cell cycle in case of DNA damage during cell growth (Claij and Te Riele 2002). This may explain the induction of MSH2 and MLH1 gene expression by growth stimulation. In contrast, Meyers et al. (1997) reported that the expression of MSH2, MLH1 and PMS2 showed only slight (within 50%) changes during the cell cycle. This discrepancy is likely due to the difference between cycling cells and cells entering the cell cycle from quiescence. Several lines of evidence indicate that in addition to repairing replicative errors within the genome, the MMR system is a component in signalling events that activate cell cycle checkpoint or apoptosis (Zhang et al. 1999; Goldmacher et al. 1986; Kat et al. 1993). Zhang et al. (1999) showed that the overexpression of MSH2 and MLH1 but not PMS1 induced apoptosis in vitro. Additionally, MMR proteins mediate apoptosis in response to exogenous substances or to UV-B. Cell lines are defective in MMR or MMR deficient show increased mutation rates and increased resistance to the genotoxic effects of DNA damaging agents. Loss of expression of MMR leads to tolerance of alkylated DNA and may lead to reduced competence for activation of apoptotic pathways. As shown for alkylating agents, loss of MMR decreases the cellular response to UV-induced damage. Primary mouse embryonic fibroblasts (MEFs) from MSH2-null and MSH6-null mice are less susceptible to the cytotoxic effects of UVB than wild type MEFs (Peters et al. 2003; Young et al. 2003). Furthermore MMR-deficiency was associated with reduced levels of apoptosis and increased residual of UVB-induced DNA adducts in the epidermis and MSH2-null mice developed UVB-induced skin tumors at lower dosages UVB than wild type mice (Young et al. 2004). Furthermore, the absence of MSH2 also resulted in a reduction in the phosphorylation of p53.
MSH2-deficient cells are resistant to DNA damaging agents, including methylation agents, cisplatin and UV radiation (Fink et al. 1998; Wang and Lippard 2005). Studies on the roles of MSH2 in response to DNA damage permit the assumption, that the MMR system is believed to trigger a process of DNA metabolism that activates cell-cycle checkpoints. MSH2 binds to CHK1 and CHK2 in vivo and in vitro (Adamson et al. 2005) and this interaction is enhanced after N-methyl-N′-nitro-N-nitrosoguanidine (MNNG) exposure, supporting the assumption that the MMR system functions as a molecular scaffold at the sites of DNA damage that facilitates the activation of these kinases. MNNG exposure results in activation of the cell cycle checkpoint kinases, ATM (ataxia-telangiectasia-mutated kinase), CHK1, and CHK2, each of which has been implicated in the triggering of the G2/M checkpoint response (reviewed in O’Brien and Brown 2006). The G2/M checkpoint prevents cells from initiating mitosis when they experience DNA damage during G2, or when they progress into G2 with unrepaired damage incurred during the previous S or G1 phase (Cejka et al. 2003). In addition, MSH2 physically interacts with ATR (ATM- and Rad3-related kinase) in response to DNA methylating agents and their interaction is required for the phosphorylation of CHK1 (Wang and Qin 2003).
MMR is required for the activation of the S-phase checkpoint in response to ionizing radiation (Brown et al. 2003). Cells deficient in MMR proteins MLH1 and MSH2 showed “radioresistant DNA synthesis” (RDS), a phentotypic hallmark of ataxia-telangiectasia, and a cancer-prone disorder caused by mutations in ATM (Painter 1981). Restoration of mismatch repair function restored normal S-phase checkpoint function in vitro. In vitro and in vivo studies both show that MSH2 binds to CHK2 and the association of MLH1 with ATM indicates that the MMR complex formed at the site of DNA damage facilitates the phosphorylation of CHK2 by ATM (Brown et al. 2003).
XPC(−/−)MSH2(−/−) mice and derived keratinocytes show that the MMR protein MSH2 plays a role in the generation of the UVB-induced arrested cells: a MSH2-deficiency lowered the percentage of arrested cells in vivo (40–50%) and in vitro (30–40%). UV-B-induced apoptosis is reduced in MSH2-deficient cells, and it correlates with decreased activation of p53, which suggests that MSH2 may act upstream of p53 to induce post UV-B apoptosis (van Oosten et al. 2005). When cells are exposed to DNA-damaging agents, p53 products accumulate in the nuclei and cause cell cycle arrest in the G1 phase, preventing the cells from replicating their DNA. After UV exposure, a transient G1 arrest is observed in cells with wild type-p53 (wt-p53), while cells lacking p53 did not stop in the G1 phase, suggesting the importance of the wt-p53 function in G1 arrest after UV irradiation (Iwamoto et al. 1999). Following UV irradiation, p53 activates transcription of the human MMR gene MSH2. Interestingly, this up-regulation critically depends on the functional interaction with c-Jun (Scherer et al. 2000). However, it seems that MSH2 and p53 may act as a kind of positive feedback regulation for the DNA damage response after UV irradiation and MSH2 have probably also meaning in UV induced G1 arrest.
MSH2, DNA repair and UV-induced skin cancer
Epidemiologic and in vitro studies have shown that sunlight exposure is an etiologic agent for the development of malignant melanoma (MM) (Fears et al. 1977; Setlow et al. 1993). The important role of the DNA repair system in the multistep process of MM tumorigenesis is demonstrated in the autosomal recessive disease xeroderma pigmentosum, where the development of multiple skin tumours including malignant melanoma early in life is associated with deficient nucleotide excision repair (NER) of pyrimidine dimers induced by UV irradiation (Cleaver 1968, 1969; Sato et al. 1993). The fact that this mechanism underlies skin cancer in general is supported by the evidence that UV-fingerprint mutations such as C/T or CC/TT are frequently found in skin tumours from patients with and without xeroderma pigmentosum. Interestingly, disruptions of the DNA MMR genes mutS and mutL were found to reduce transcription-coupled NER of the lactose operon in E. coli; and human cells with mutations in particular MMR genes were likewise found to have a deficiency in transcription-coupled repair of UV-induced pyrimidine dimers (Mellon and Champe 1996a; Mellon et al. 1996b). Thus, defective mismatch repair may be a risk factor involved in the multistep tumorogenesis of MM. Analysis of MLH1 and MSH2 in malignant melanoma using various techniques, including polymerase chain reaction (PCR) assays, in situ hybridization and immunohistochemistry, demonstrated that it is not mutation in MLH1 and MSH2, but rather the loss of expression of these genes (both the RNA and protein level), that affects tumor progression (Korabiowska et al. 2000, 2004). Loss of the MMR gene expression correlated with high aneuploidy ratio (Korabiowska et al. 1999) and increased Clark levels (Korabiowska et al. 2000), observed in negative cases of MM. Deletions in DNA mismatch repair proteins, MSH2 and MLH1, were present in both lentigo maligna and in MM and correlated with DNA ploidy-related parameters, prognosis and protein expression levels (Korabiowska et al. 2001). Conversely, other studies have found that MMR levels are increased in the skin tumour as compared to the adjacent normal tissue (Rass et al. 2000). UVB irradiation can induce apoptosis, morphologic changes, and altered expression of p53, Bcl-2, and MSH2 in radial growth phase melanoma cell lines. While up-regulation of p53, Bcl-2, and MSH2 suggests that these factors are involved in the altered balance between survival and apoptosis induced by UVB (Hussein et al. 2006). Furthermore, UVB irradiation induces additional mutations in the MMR repair genes MSH2 and MLH1 (Hussein and Wood 2003).
In summary, UV-induced DNA damage is primarily removed by NER. There is some evidence that MMR proteins interact with UV-induced DNA damage but the role of MMR in post UV response has been controversial. MMR proteins interact with NER proteins (Bertrand et al. 1998) and MSH2/MSH6 heterodimers bind oligoduplexes containing cyclobutane pyrimidine dimers (CPD) (Mu et al. 1997; Wang et al. 1999a, b).
Conclusions, future outlook
In conclusion, there is overwhelming evidence for an important role of MSH2 in various types of cancers. Interestingly, we know today that the importance of MSH2 for pathogenesis, progression, and therapy of these malignancies is not exclusively related to its function in DNA repair, but is at least in part related to other, independent mechanisms that include regulation of cell cycle progression and apoptosis. These newly recognized functions of MSH2 may in the future not only lead to a better understanding of cancer pathogenesis and progression, but may also lead to the introduction of new cancer therapies that target MSH2 or MSH2-antagonists (e.g. via siRNA or antisense technology), most likely in combination with cytotoxic agents.
References
Aaltonen LA, Salovaara R, Kristo P, Canzian F, Hemminki A, Peltomaki P, Chadwick RB, Kaariainen H, Eskelinen M, Jarvinen H, Mecklin JP, de la Chapelle A (1998) Incidence of hereditary nonpolyposis colorectal cancer and the feasibility of molecular screening for the disease. N Engl J Med 338:1481–1487
Aarnio M, Sankila R, Pukkala E, Salovaara R, Aaltonen LA, de la Chapelle A, Peltomaki P, Mecklin JP, Jarvinen HJ (1999) Cancer risk in mutation carriers of DNA-mismatch-repair genes. Int J Cancer 81:214–218
Adamson AW, Beardsley DI, Kim WJ, Gao Y, Baskaran R, Brown KD (2005) Methylator-induced, mismatch repair-dependent G2 arrest is activated through Chk1 and Chk2. Mol Biol Cel 16:1513–1526
Aubry MC, Halling KC, Myers JL, Tazelaar HD, Yang P, Thibodeau SN (2001) DNA mismatch repair genes hMLH1, hMSH2, and hMSH6 are not inactivated in bronchioloalveolar carcinomas of the lung. Cancer 92:2898–2901
Bapat BV, Madlensky L, Temple LK, Hiruki T, Redston M, Baron DL, Xia L, Marcus VA, Soravia C, Mitri A, Shen W, Gryfe R, Berk T, Chodirker BN, Cohen Z, Gallinger S (1999) Family history characteristics, tumor microsatellite instability and germline MSH2 and MLH1 mutations in hereditary colorectal cancer. Hum Genet 104:167–176
Bertrand P, Tishkoff DX, Filosi N, Dasgupta R, Kolodner RD (1998) Physical interaction between components of DNA mismatch repair and nucleotide excision repair. Proc Natl Acad Sci USA 95:14278–14283
Boland CR (2000) Molecular genetics of hereditary nonpolyposis colorectal cancer. Ann NY Acad Sci 910:50–61
Brown KD, Rathi A, Kamath R, Beardsley DI, Zhan Q, Mannino JL, Baskaran R (2003) The mismatch repair system is required for S-phase checkpoint activation. Nat Genet 33:80–84
Caduff RF, Johnston CM, Svoboda-Newman SM, Poy EL, Merajver SD, Frank TS (1996) Clinical and pathological significance of microsatellite instability in sporadic endometrial carcinoma. Am J Pathol 148:1671–1678
Castrilli G, Fabiano A, La Torre G, Marigo L, Piantelli C, Perfetti G, Ranelletti FO, Piantelli M (2002) Expression of hMSH2 and hMLH1 proteins of the human DNA mismatch repair system in salivary gland tumors. J Oral Pathol Med 31:234–238
Cejka P, Stojic L, Mojas N, Russell AM, Heinimann K, Cannavo E, di Pietro M, Marra G, Jiricny J (2003) Methylation-induced G(2)/M arrest requires a full complement of the mismatch repair protein hMLH1. EMBO J 22:2245–2254
Charames GS, Bapat B (2003) Genomic instability and cancer. Curr Mol Med 3:589–596
Claij N, Te Riele H (2002) Methylation tolerance in mismatch repair proficient cells with low MSH2 protein level. Oncogene 21:2873–2879
Cleaver JE (1968) Defective repair replication of DNA in xeroderma pigmentosum. Nature 218:652–656
Cleaver JE (1969) Xeroderma pigmentosum: a human disease in which an initial stage of DNA repair is defective. Proc Natl Acad Sci USA 63:428–435
Cox EC, Degnen GE, Scheppe ML (1972) Mutator gene studies in Escherichia coli: the mutS gene. Genetics 72:551–567
Dao V, Modrich P (1998) Mismatch-, MutS-, MutL-, and helicase II-dependent unwinding from the single-strand break of an incised heteroduplex. J Biol Chem 273:9202–9207
Fears TR, Scotto J, Schneiderman MA (1977) Mathematical models of age and ultraviolet effects on the incidence of skin cancer among whites in the United States. Am J Epidemiol 105:420–427
Field JK, Kiaris H, Howard P, Vaughan ED, Spandidos DA, Jones AS (1995) Microsatellite instability in squamous cell carcinoma of the head and neck. Br J Cancer 71:1065–1069
Fink D, Aebi S, Howell SB (1998) The role of DNA mismatch repair in drug resistance. Clin Cancer Res 4:1–6
Fishel R, Lescoe MK, Rao MR (1993) The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell 75:1027–1038
Galio L, Bouquet C, Brooks P (1999) ATP hydrolysis-dependent formation of a dynamic ternary nucleoprotein complex with MutS and MutL. Nucleic Acids Res 27:2325–2331
Genschel J, Littman SJ, Drummond JT, Modrich P (1998) Isolation of MutSβ from human cells and comparison of the mismatch repair specificities of MutSβ and MutSα. J Biol Chem 273:19895–19901
Goldmacher VS, Cuzick RA Jr, Thilly WG (1986) Isolation and partial characterization of human cell mutants differing in sensitivity to killing and mutation by methylnitrosourea and N-methyl-N′-nitro-N-nitrosoguanidine. J Biol Chem 261:12462–12471
Hafe BD, Robertson SJ (2000b) DNA mismatch repair and genetic instability. Annu Rev Genet 34:359–399
Hafe BD, Minesinger BK, Jinks-Robertson S (2000a) Discrete in vivo roles for the MutL homologs Mlh2p and Mlh3p in the removal of frameshift intermediates in budding yeast. Curr Biol 10:145–148
Hall MC, Matson SW (1999) The Escherichia coli MutL protein physically interacts with MutH and stimulates the MutH-associated endonuclease activity. J Biol Chem 274:1306–1312
Hall MC, Jordan JR, Matson SW (1998) Evidence for a physical interaction between the Escherichia coli methyl-directed mismatch repair proteins MutL and UvrD. EMBO J 17:1535–1541
Hamid AA, Mandai M, Konishi I, Nanbu K, Tsuruta Y, Kusakari T, Kariya M, Kita M, Fujii S (2002) Cyclical change of hMSH2 protein expression in normal endometrium during the menstrual cycle and its overexpression in endometrial hyperplasia and sporadic endometrial carcinoma. Cancer 94:997–1005
Hussein MR, Wood GS (2003) hMLH1 and hMSH2 gene mutations are present in radial growth-phase cutaneous malignant melanoma cell lines and can be induced further by ultraviolet-B irradiation. Exp Dermatol 12:872–875
Hussein MR, Sun M, Roggero E, Sudilovsky EC, Tuthill RJ, Wood GS, Sudilovsky O (2002) Loss of heterozygosity, microsatellite instability, and mismatch repair protein alterations in the radial growth phase of cutaneous malignant melanomas. Mol Carcinog 34:35–44
Hussein MR, El-Ghorori RM, El-Rahman YG (2006) Alterations of p53, BCL-2, and hMSH2 protein expression in the normal brain tissues, gliosis, and gliomas. Int J Exp Pathol 87:297–306
Iwamoto K, Shinomiya N, Mochizuki H (1999) Different cell cycle mechanisms between UV-induced and X-ray-induced apoptosis in WiDr colorectal carcinoma cells. Apoptosis 4:59–66
Iwanaga R, Komori H, Ohtani K (2004) Differential regulation of expression of the mammalian DNA repair genes by growth stimulation. Oncogene 23:8581–8590
Kat A, Thilly WG, Fang WH, Longley MJ, Li GM, Modrich P (1993) An alkylation-tolerant, mutator human cell line is deficient in strand-specific mismatch repair. Proc Natl Acad Sci USA 90:6424–6428
Katabuchi H, van Rees B, Lambers AR (1995) Mutations in DNA mismatch repair genes are not responsible for microsatellite instability in most sporadic endometrial carcinomas. Cancer Res 55:5556–5560
Korabiowska M, Brinck U, Ruschenburg I, Honig JF, Stachura J, Droese M (1999) Loss of DNA-mismatch repair gene expression in oral melanomas. Oncol Rep 6:921–923
Korabiowska M, Brinck U, Dengler H, Stachura J, Schauer A, Droese M (2000) Analysis of the DNA mismatch repair proteins expression in malignant melanomas. Anticancer Res 20:4499–4505
Korabiowska M, Ruschenburg I, Schlott T, Kubitz A, Brinck U, Droese M (2001) Relation between DNA ploidy status and the expression of the DNA-mismatch repair genes MLH1 and MSH2 in cytological specimens of melanoma lymph node and liver metastases. Diagn Cytopathol 24:157–162
Korabiowska M, Konig F, Verheggen R, Schlott T, Cordon-Cardo C, Romeike B, Brinck U (2004) Altered expression and new mutations in DNA mismatch repair genes MLH1 and MSH2 in melanoma brain metastases. Anticancer Res 24:981–986
Kramer W, Kramer B, Williamson MS, Fogel S (1989) Cloning and nucleotide sequence of DNA mismatch repair gene PMS1 from Saccharomyces cerevisiae: homology of PMS1 to procaryotic MutL and HexB. J Bacteriol 171:5339–5346
Leach FS, Nicolaides NC, Papadopoulos N, Liu B, Jen J, Parsons R, Peltomaki P, Sistonen P, Aaltonen LA, Nystrom-Lahti M (1993) Mutations of a mutS homolog in hereditary nonpolyposis colorectal cancer. Cell 75:1215–1225
Leach FS, Polyak K, Burrell M (1996) Mutations of the human mismatch repair gene hMSH-2 in normal and neoplastic tissues. Cancer Res 56:235–240
Leach FS, Hsieh JT, Molberg K, Saboorian MH, McConnell JD, Sagalowsky AI (2000) Expression of the human mismatch repair gene hMSH2: a potential marker for urothelial malignancy. Cancer 88:2333–2341
Liu B, Parsons R, Papadopoulos N, Nicolaides NC, Lynch HT, Watson P, Jass JR, Dunlop M, Wyllie A, Peltomaki P, de la Chapelle A, Hamilton SR, Vogelstein B, Kinzler KW (1996) Analysis of mismatch repair genes in hereditary non-polyposis colorectal cancer patients. Nat Med 2:169–174
Loeb LA (1994) Microsatellite instability: marker of a mutator phenotype in cancer. Cancer Res 54:5059–5063
Lothe RA, Peltomaki P, Meling GI, Aaltonen LA, Nystrom-Lahti M, Pylkkanen L, Heimdal K, Andersen TI, Moller P, Rognum TO, Fossa SD, Haldorsent T, Langmarg F, Brogger A, De La Chapelle A, Borresen AL (1993) Genomic instability in colorectal cancer: relationship to clinicopathological variables and family history. Cancer Res 53:5849–5852
Lynch HT, Smyrk T, Lynch JF (1998) Molecular genetics and clinical-pathology features of hereditary nonpolyposis colorectal carcinoma (Lynch syndrome): historical journey from pedigree anecdote to molecular genetic confirmation. Oncology 55:103–108
Marra G, Chang CL, Laghi LA, Chauhan DP, Young D, Boland CR (1996) Expression of human MutS homolog 2 (hMSH2) protein in resting and proliferating cells. Oncogene 13:2189–2196
Mellon I, Champe GN (1996a) Products of DNA mismatch repair genes mutS and mutL are required for transcription-coupled nucleotide-excision repair of the lactose operon in Escherichia coli. Proc Natl Acad Sci USA 93:1292–1297
Mellon I, Rajpal DK, Koi M, Boland CR, Champe GN (1996b) Transcription-coupled repair deficiency and mutations in human mismatch repair genes. Science 272:557–560
Meyers M, Theodosiou M, Acharya S, Odegaard E, Wilson T, Lewis JE, Davis TW, Wilson-Van Patten C, Fishel R, Boothman DA (1997) Cell cycle regulation of the human DNA mismatch repair genes hMSH2, hMLH1, and hPMS2. Cancer Res 57:206–208
Mu D, Tursun M, Duckett DR, Drummond JT, Modrich P, Sancar A (1997) Recognition and repair of compound DNA lesions (base damage and mismatch) by human mismatch repair and excision repair systems. Mol Cell Biol 17:760–769
Muller A, Fishel R (2002) Mismatch repair and the hereditary non-polyposis colorectal cancer syndrome (HNPCC). Cancer Invest 20:102–109
O’Brien V, Brown R (2006) Signalling cell cycle arrest and cell death through the MMR System. Carcinogenesis 27:682–692
Painter RB (1981) Radioresistant DNA synthesis: an intrinsic feature of ataxia telangiectasia. Mutat Res 84:183–190
Peters AC, Young LC, Maeda T, Tron VA, Andrew SE (2003) Mammalian DNA mismatch repair protects cells from UVB-induced DNA damage by facilitating apoptosis and p53 activation. DNA Repair (Amst) 2:427–435
Prtilo A, Leach FS, Markwalder R, Kappeler A, Burkhard FC, Cecchini MG, Studer UE, Thalmann GN (2005) Tissue microarray analysis of hMSH2 expression predicts outcome in men with prostate cancer. J Urol 174:1814–1818
Prolla T, Christie DM, Liskay RM (1994) Dual requirement in yeast DNA mismatch repair for MLH1 and PMS1, two homologs of the bacterial mutL gene. Mol Cell Biol 14:407–415
Quinn AG, Healy E, Rehman I, Sikkink S, Rees JL (1995) Microsatellite instability in human non-melanoma and melanoma skin cancer. J Invest Dermatol 104:309–312
Rass K, Gutwein P, Muller SM, Friedrich M, Meineke V, Welter C, Tilgen W, Reichrath J (2000) Immunohistochemical analysis of DNA mismatch repair enzyme hMSH-2 in normal human skin and basal cell carcinomas. Histochem J 32:93–97
Rass K, Gutwein P, Tilgen W, Welter C, Meineke V, Reichrath J (2001) DNA mismatch repair enzyme hMSH2 in malignant melanoma: increased immunoreactivity as compared to acquired melanocytic nevi and strong mRNA expression in melanoma cell lines. Histochem J 33:459–467
Renault B, Calistri D, Buonsanti G, Nanni O, Amadori D, Ranzani GN (1996) Microsatellite instability and mutations of p53 and TGF-beta RII genes in gastric cancer. Hum Genet 98:601–607
Sancar A, Hearst JE (1993) Molecular matchmakers. Science 259:1415–1420
Sato M, Nishigori C, Zghal M, Yagi T, Takebe H (1993) Ultraviolet-specific mutations in p53 gene in skin tumors in xeroderma pigmentosum patients. Cancer Res 1253:2944–2946
Scherer SJ, Welter C, Zang KD, Dooley S (1996) Specific in vitro binding of p53 to the promoter region of the human mismatch repair gene hMSH2. Biochem Biophys Res Commun 221:722–728
Scherer SJ, Maier SM, Seifert M, Hanselmann RG, Zang KD, Muller-Hermelink HK, Angel P, Welter C, Schartl M (2000) p53 and c-Jun functionally synergize in the regulation of the DNA repair gene hMSH2 in response to UV. J Biol Chem 275:37469–37473
Setlow RB, Grist E, Thompson K, Woodhead AD (1993) Wavelengths effective in induction of malignant melanoma. Proc Natl Acad Sci USA 90:6666–6670
Srivastava T, Chattopadhyay P, Mahapatra AK, Sarkar C, Sinha S (2004) Increased hMSH2 protein expression in glioblastoma multiforme. J Neurooncol 66:51–57
Shia J, Ellis NA, Klimstra DS (2004) The utility of immunohistochemical detection of DNA mismatch repair gene proteins. Virchows Arch 445:431–441
Thibodeau SN, French AJ, Roche PC (1996) Altered expression of hMSH-2 and hMLH-1 in tumors with microsatellite instability and genetic alterations in mismatch repair genes. Cancer Res 56:4836–4840
Umar A, Risinger JI, Glaab WE, Tindall KR, Barrett JC, Kunkel TA (1998) Functional overlap in mismatch repair by human MSH3 and MSH6. Genetics 148:1637–1646
van Oosten M, Stout GJ, Backendorf C, Rebel H, de Wind N, Darroudi F, van Kranen HJ, de Gruijl FR, Mullenders LH (2005) Mismatch repair protein Msh2 contributes to UVB-induced cell cycle arrest in epidermal and cultured mouse keratinocytes. DNA Repair (Amst) 4:81–89
Vasen HF, Wijnen JT, Menko FH, Kleibeuker JH, Taal BG, Griffioen G, Nagengast FM, Meijers-Heijboer EH, Bertario L, Varesco L, Bisgaard ML, Mohr J, Fodde R, Khan PM (1996) Cancer risk in families with hereditary nonpolyposis colorectal cancer diagnosed by mutation analysis. Gastroenterology 110:1020–1027
Wagner R, Meselson M (1976) Repair tracts in mismatched DNA heteroduplexes. Proc Natl Acad Sci USA 73:4135–4139
Wang D, Lippard SJ (2005) Cellular processing of platinum anticancer drugs. Nat Rev Drug Discov 4:307–320
Wang H, Lawrence CW, Li GM, Hays JB (1999a) Specific binding of human MSH2.MSH6 mismatch-repair protein heterodimers to DNA incorporating thymine- or uracil-containing UV light photoproducts opposite mismatched bases. J Biol Chem 274:16894–16900
Wang TF, Kleckner N, Hunter N (1999b) Functional specificity of MutL homologs in yeast: evidence for three Mlh1-based heterocomplexes with distinct roles during meiosis in recombination and mismatch correction. Proc Natl Acad Sci USA 96:13914–13919
Wang Y, Qin J (2003) MSH2 and ATR form a signaling module and regulate two branches of the damage response to DNA methylation. Proc Natl Acad Sci USA 100:15387–15392
Watanabe M, Imai H, Kato H, Shiraishi T, Ushijima T, Nagao M, Yatani R (1996) Microsatellite instability in latent prostate cancers. Int J Cancer 69:394–397
Wheeler JM, Loukola A, Aaltonen LA, Mortensen NJ, Bodmer WF (2000) The role of hypermethylation of the hMLH1 promoter region in HNPCC versus MSI+ sporadic colorectal cancers. J Med Genet 37:588–592
Young LC, Peters AC, Maeda T, Edelmann W, Kucherlapati R, Andrew SE, Tron VA (2003) DNA mismatch repair protein Msh6 is required for optimal levels of ultraviolet-B-induced apoptosis in primary mouse fibroblasts. J Invest Dermatol 121:876–880
Young LC, Thulien KJ, Campbell MR, Tron VA, Andrew SE (2004) DNA mismatch repair proteins promote apoptosis and suppress tumorigenesis in response to UVB irradiation: an in vivo study. Carcinogenesis 25:1821–1827
Zhang H, Richards B, Wilson T, Lloyd M, Cranston A, Thorburn A, Fishel R, Meuth M (1999) Apoptosis induced by overexpression of hMSH2 or hMLH1. Cancer Res 59:3021–3027
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seifert, M., Reichrath, J. The role of the human DNA mismatch repair gene hMSH2 in DNA repair, cell cycle control and apoptosis: implications for pathogenesis, progression and therapy of cancer. J Mol Hist 37, 301–307 (2006). https://doi.org/10.1007/s10735-006-9062-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10735-006-9062-5