Abstract
Colorectal cancer (CRC) continues to rank as the third most common cancer in Western society and the second leading cause of cancer death in North America. There are at least three distinct, and relatively discreet, molecular pathways associated with this disease: chromosomal instability (CIN), microsatellite instability (MSI) and the cytosine polyguanine island methylator phenotype. Defects in the DNA mismatch repair system (MMR) account for the MSI phenotype and genotype of about 15 % of CRC. Although high frequency MSI tumors have better stage independent prognosis compared to those with CIN, MMR deficient CRC appears to be resistant to fluorouracil based treatment, but sensitive to other therapeutic regimens. This review summarises current literature on differential chemosensitivity of MMR-deficient CRC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
CRC is the third most common cancer in Western society and the second leading cause of cancer-related death in North America [1].
An understanding of uncommon highly penetrant CRC syndromes has greatly informed the field and led to a better understanding of key molecular somatic events in more common cases of the disease. In 1913, Aldred Warthin described for the first time kindreds with multigenerational cancers of the colon, stomach and uterus; noting that these familial cancers were diagnosed at younger ages compared to non-familial cases [2]. Warthin’s report on “Cancer Family Syndrome” was the first description of hereditary non-polyposis colorectal cancer (HNPCC) and his research would later be continued by Henry Lynch in the 1960s who refined the definition of HNPCC into Lynch Syndrome I, or site specific familial CRC, and Lynch Syndrome II where CRC in addition to extracolonic cancers were observed [3].
These descriptive studies were pivotal in the identification of the genetic basis of HNPCC or Lynch Syndrome in 1993, with discovery of germline mutations of DNA mismatch repair (MMR) genes as the hallmark of this syndrome [4–6]. Similarly, germline mutations of the Apc gene, manifested by more classical chromosomal instability (CIN), were shown, in 1991, to be the genetic cause of Familial Adenomatous Polyposis (FAP) [7].
A better understanding of cancer genetics, epigenetic and molecular events involved in CRC, suggest that there are at least three distinct somatic mutator phenotype pathways responsible for this disease:
(1) microsatellite instability (MSI), as is seen in HNPCC, (2) chromosomal instability (CIN), as is seen in FAP and (3) cytosine polyguanine (CpG) island methylator phenotype (CIMP).
The most common genetic alterations, identified in 85 % of all CRCs, are allelic losses or loss of heterozygosity, chromosomal amplifications and translocations at multiple tumor suppressor loci such as 5q, 17p and 18q; characteristic of the CIN or microsatellite-stable pathway.
The other 15 % of CRC arise as a result of somatic DNA MMR deficiency, leading to high frequency MSI (MSI-H) associated with mutations in critical genes involved in carcinogenesis such as transforming growth factor-β type II receptor [8] and BAX [9]. These tumors are MSI-H and occur due to the inability of cells to repair single nucleotide DNA mismatches.
Microsatellites are stretches of DNA sequence where single nucleotide (mononucleotide) or units of two or more nucleotides (di-, tri-, tetra-, or pentanucleotides) are repeated in the genome. There are at least 500,000 microsatellites in the human genome, which can occur in the intergenic regions as well as in genes. Microsatellites are commonly located in the introns of genes but there are numerous examples of microsatellites in promoters, untranslated terminal regions and in coding exons [10].
The number of repeats contained in any one particular microsatellite is, in principle, the same in every cell of the body. MSI is said to occur when some cells display one or two alleles with different number of repeats, which occurs as a somatic event after birth such as during tumorigenesis. For MSI to be detectable (present in enough cells to be identified by common detection methods), the aberrant cell is usually clonal. Hence, MSI is typically seen in tumors which are monoclonal or oligoclonal [10].
The most common methods used to detect MSI in tumor tissue are the PCR-based assay for detection of instability at selected microsatellite loci and analysis of MMR protein expression by immunohistochemistry (IHC). MSI testing and IHC are complementary, and loss of MMR protein expression has been shown to be highly concordant with DNA based MSI testing [11].
For MSI testing of CRC, a panel of five microsatellites have been validated and recommended as a reference panel [12] including three dinucleotide repeats (D2S123, D5S346, D17S250) and two mononucleotide repeats (BAT26, BAT25).
CRCs can therefore be characterized on the basis of MSI-H, if two or more of the five microsatellite markers show instability (insertion/deletion mutations), low frequency MSI (MSI-L) if only one of the five markers shows instability, and microsatellite stable (MSS) if none of the markers show instability [12].
MSI-H is a hallmark of Lynch Syndrome that results from germline mutations in MMR genes: MLH1, MSH2, MSH6 and PSM2, which are highly penetrant yet account for less than 5 % of all CRCs.
The majority of MSI-H CRCs are sporadic non-Lynch Syndrome cases that result from epigenetic inactivation of the MLH1 gene promoter by DNA hypermethylation [13]. These sporadic MSI-H CRCs often arise in the setting of a specific pathway of DNA hypermethylation, known as the CpG island methylator phenotype (CIMP) with CIMP-related silencing of MLH1.
Patients with MSI-H tumors have distinct clinical and pathological features, irrespective of their germline or sporadic origins [14]. These features include proximal colon predominance, frequent poor differentiation, mucinous histology and increased number of tumor infiltrating lymphocytes [15, 16]. Though, in addition to molecularly distinct features from Lynch syndrome tumors, sporadic MSI cancers also have associated epidemiologic features such as older age at diagnosis, female gender and increased frequency of cigarette smoking [13].
Microsatellite instability and sensitivity to chemotherapy
Following the initial discovery of MSI in Lynch Syndrome and in about 15 % of sporadic CRC, considerable data has accumulated demonstrating improved outcome for patients with MMR-deficient CRC compared with patients who have MMR-proficient or CIN tumors.
Most of this data has been collected from retrospective studies [17, 18], but also includes a population-based study [19] and a meta-analysis summarizing many studies [20].
Gryfe et al. [21] published a population based series of 607 patients with CRC, describing clinical features and outcome of patients based on tumor MSI. MSI-H was found in 17 % of cases in this series, and tumor MSI was associated with a significant survival advantage independent of all standard prognostic factors such as tumor stage (HR: 0.42; 95 % CI 0.27–0.53; p < 0.001). MSI-H CRCs also had decreased likelihood of metastasizing to regional lymph nodes (OR: 0.49; 95 % CI 0.21–0.53; p < 0.001) and distant organs (OR: 0.49; 95 % CI 0.27–0.89; p = 0.02).
Detection of MSI and deficient MMR in CRC has since gained increasing importance not only as a prognostic marker, but also as a predictive marker for the benefit of adjuvant chemotherapy in Stage II and III CRC [22], as discussed below.
Decreased efficacy of fluorouracil-based (5-FU) adjuvant chemotherapy
Since the early 1990s, adjuvant chemotherapy with fluorouracil (5-FU) plus levamisole, and later with leucovorin, has been the standard of care for patients with Stage III and selected Stage II CRC [23–26].
Adding oxaliplatin to 5-FU-based therapy was shown to improve disease free survival (DFS) and overall (OS) in patients with Stage III disease [27, 28]. However, no overall survival benefit is evident from adding oxaliplatin in unselected patients with Stage II disease [29].
Ribic et al. [30] published a series describing 570 patients with colon cancer enrolled in five prior phase 3 trials of 5-FU-based adjuvant chemotherapy following curative resection for Stage II and Stage III colon cancer. Among these patients, 16.7 % (n = 95) demonstrated MSI-H, with significant association with proximal tumor site (p < 0.001), high histologic tumor grade (p < 0.001), and improved survival (no-chemotherapy arm).
However, and somewhat surprisingly, tumor MSI-H was not correlated with increased overall survival in the group of patients who received adjuvant chemotherapy (HR: 1.07; CI 95 % 0.62–1.86; p = 0.8). The benefit of treatment differed significantly according to the tumor MSI status (p = 0.01). Adjuvant chemotherapy with 5-FU-based regimens, improved overall survival only among patients with non-MSI-H tumors (HR: 0.72; 95 % CI 0.53–0.99; p = 0.04) [30].
The lack of benefit in DFS and OS shown by Ribic et al. with fluorouracil-based adjuvant chemotherapy in MSI-H patients, makes it particularly hard to justify among unselected Stage II CRC patients [31].
Although other studies have reported contradictory results [32] [33, 34], these results were based mostly on nonrandomized trials presenting selection bias, shifts in patient populations or other biases associated with nonrandomized comparisons.
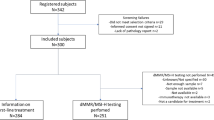
Moreover, Sargent et al. [35] recently confirmed and extended the initial findings of Ribic et al. on clinical behavior and 5-FU-based chemosensitivity of CRC based on tumor MSI status. In this latter study, 507 patients with Stage II and III colon cancer were analyzed from five completed randomized clinical trials [Federation Francophone de la Cancerologie Digestive (FFCD) 8802, North Central Cancer Treatment Group (NCCTG) 78-48-52, NCCTG 87-46-51, Intergroup (INT) 0035 and Gruppo Italiano di Valutazione Interventi in Oncologia (GIVIO)]. Sargent et al. then combined the data from these 507 patients with data from patients of four of the five clinical trials used by Ribic et al. [30]. Tumor MMR status was determined by MSH2 and MLH1 IHC, a reasonable and efficient surrogate for DNA based MSI status [11]. From 457 patients (90 %) in which MMR status was successfully determined, 70 (15 %) exhibited deficient MMR (dMMR). Patients with dMMR tumors were more likely to have Stage II (p = 0.006) disease and have poorly differentiated tumors (p = 0.002). In univariate models, dMMR status was associated with improved DFS (HR: 0.46; 95 % CI 0.22–0.95; p = 0.03), and a trend toward improved OS (HR: 0.51; 95 % CI 0.24–1.1; p = 0.06) for patients randomized to the surgery alone (no chemotherapy) arm.
In the analysis of MMR status as a predictive marker for chemotherapy response, no benefit in DFS from 5-FU-based treatment was observed for patients with dMMR status (HR: 1.39; 95 % CI 0.46–4.15; p = 0.56), whereas treatment was of benefit in patients with proficient MMR (pMMR) tumors (HR: 0.67; 95 % CI 0.48–0.93; p = 0.02) [35].
In the pooled data set, no benefit from treatment was observed among patients with dMMR tumors and either Stage II (HR: 2.03; 95 % CI 0.85–6.24; p = 0.9) or Stage III disease (HR: 1.01; 95 % CI 0.41–2.51; p = 0.98). In patients with pMMR tumors, benefit from adjuvant treatment was only observed among those with Stage III disease (HR: 0.64; p = 0.001). The interaction test between treatment efficacy for DFS was significant (p = 0.04), indicating that the effect of treatment differs by MMR status.
These observations from clinical trials have also been reproduced using a range of MLH1, MSH2 and MSH6 deficient in vitro models. dMMR tumor cells grown in vitro are approximately 18-fold more resistant to 5-FU and its analogs compared to pMMR cells [36]. The resistances of these cell lines with MLH1 deficiency due to a methylated MLH1 promoter, has also been reversed by re-expressing MLH1 with the use of the demethylating agent 5-azacytidine [37]. Xenograft experiments have also confirmed that MSI-H CRCs are resistant to 5-FU [38].
Resistance of dMMR cancer cells to 5-FU may be due to the incorporation of fluorouracil metabolites into DNA, rather than their effects on thymidylate synthetase or incorporation into RNA.
5-FU is a drug metabolized to a series of different derivatives that elicit antitumor activity. FdUMP is one derivative that inhibits thymidylate synthetase, which is essential for the generation of nucleotides required for DNA replication, whereas 5FdUTP is incorporated directly into DNA and 5FUTP into RNA. The incorporation of 5FUTP is cytotoxic as it interferes with RNA processing while 5FdUTP lesion in DNA may be lethal by causing DNA strand breaks or triggering apoptosis [39].
The FOLFOX regimen, which combines 5-FU + leucovorin with oxaliplatin, has become the current accepted adjuvant standard of care for resected Stage III colon cancer patients regardless of their MMR status, based on the MOSAIC trial [27, 29].
dMMR tumors have proven resistance to cisplatin and carboplatin treatment, maybe due to the role of MMR in recognizing cisplatin and carboplatin adducts in DNA. Since MMR proteins do not recognize oxaliplatin-related adducts, resistance to oxaliplatin in dMMR cancer cells does not occur [40, 41]. However, since there is no data to support the use of oxaliplatin as a single agent in colon cancer, the combination of FOLFOX is still used widely.
It is not known with certainty if the lack of benefit from adjuvant 5-FU in patients with dMMR tumors translates into a lack of benefit from FOLFOX. Several studies have shown that MMR deficiency is not prognostic for outcome in CRC patients who receive FOLFOX [42–44], and a retrospective study suggests that Stage III colon cancer patients with dMMR may have improved outcomes with FOLFOX versus 5-FU alone [45].
The role of dMMR status as a predictive marker for chemotherapy efficacy still awaits prospective validation. The Eastern Cooperative Oncology Group (ECOG) 5202 trial is randomly assigning patients with resected Stage II colon cancer to treatment using biomarker information. Patients with high risk tumors, based on non-MSI-H status and loss of heterozygosity (LOH) of chromosome 18q, are randomly assigned to FOLFOX with or without bevacizumab, whereas low risk patients, characterized by MSI-H tumors and no 18q LOH, do not receive adjuvant therapy. Results of this trial are yet to be published.
The best available data today does not support the use of chemotherapy in patients with average-risk Stage II colon cancer. Decision making for high-risk stage II patients (perforated tumors, obstructing tumors, adhesion or invasion of surrounding structures and aneuploidy) with MSI-H tumors, needs to be discussed on a case by case basis.
Irinotecan efficacy and MSI status
Current interest over the benefit of adjuvant chemotherapy for colon cancer patients with dMMR tumors has led to further molecular correlative studies with other chemotherapeutic regimens.
Cancer and Leukemia Group B (CLGB) 89803 was a phase III randomized trial that compared 5-FU + Leucovorin to 5-FU/Leucovorin + Irinotecan (IFL) in resected Stage III and high risk Stage II colon cancer. From a group of 723 cases, dMMR was identified in 106 (13.4 %), based on loss of MLH1 or MSH2 by immunohistochemistry. Patients with dMMR tumors treated with Irinotecan showed improved 5 year DFS compared to those with pMMR tumors (p = 0.03). This relationship was not observed among patients treated with 5-FU + Leucovorin. There was also a trend towards longer DFS among dMMR patients treated with Irinotecan based therapy compared to those treated with IFL.
This and other studies support the notion that MSI-H tumors should respond to treatment with Irinotecan. Studies in cultured cells and xenografted human CRCs have shown that dMMR tumors are more sensitive to Irinotecan than pMMR tumors [46, 47]. Other smaller retrospective studies in rectal cancer and metastatic colon cancer have also shown that MSI-H tumor status predicts improved outcome with Irinotecan therapy [48, 49].
Irinotecan inhibits the catalytic function of topoisomerase-I by stabilizing covalent complexes between this enzyme and DNA. This interaction produces single-strand breaks that are later converted to double-strand breaks after the replication fork collides. Since double-strand breaks are lethal if not repaired before mitosis, any process that inhibits DNA repair, such as loss of MMR proteins, will potentiate tumor death.
Since MSI-H tumors have multiple defects in genes governing signal transduction such as TGFβ RII, BAX, SEC53, OGT, transcriptional activation genes like TCF4, and other DNA repair genes such as hMSH6, it may be possible that not only the loss of MMR proteins but also the loss of one or more of these genes may account for increased sensitivity to Irinotecan.
Synthetic lethality and novel therapeutic strategies
Current approaches to treating dMMR colon cancers include targeting the primary mutation in the MMR genes by exploiting synthetic lethal interactions, or targeting the secondary mutations that occur as a result of dMMR. Two genes, proteins or pathways are synthetic lethal if loss of one is compatible with cellular viability, but loss of both leads to cell death A combination of treatments targeting both primary and secondary mutations might also be feasible.
The use of high throughput array technology for molecular profiling of tumor tissue, bioinformatics analysis and system biology approaches to identify genes and pathways, are currently leading towards a tailored approach to adjuvant treatment. Such techniques are being used to evaluate the efficacy of regimens, targeting for example the PI3 K/AKT/mTOR pathway [50].
The combination of Irinotecan with thymidine has also been proposed as a therapeutic approach for dMMR tumors based on data from in vitro testing. A pre clinical study demonstrated that Irinotecan with thymidine suppress colonies of dMMR tumor cells by up to 3,000-fold, compared with Irinotecan alone [51]. Cell lines used in this study were dMMR and contained a frameshift mutation in MRE11A with high sensitivity to combined Irinotecan and thymidine. Correction of the MMR defect did not result in the reversal of sensitivity to these drugs, implying that the selective effects occur as a result of targeting secondary mutations and defective double strand break repair.
In this same approach, a synthetic lethal relationship has been shown with MSH2 deficient cells and methotrexate. A screen to identify drugs that caused selective cell death in MSH2-deficient tumor cells identified methotrexate among other drugs [52]. This synthetic lethality was characterized by accumulation of 8-OHdG, which is a DNA lesion associated with oxidative stress.
This study also proved that inhibition of dihydrofolate reductase using RNA interference leads to increased cell death in MSH2-deficient cells. This would suggest that methotrexate would cause lethality via its own substrate, dihydrofolate reductase.
Chemotherapy and Lynch syndrome
The aforementioned review describes data from research addressing MSI and chemotherapy, primarily in the 15–20 % of CRC patients with somatic dMMR manifested as MSI-H tumors. Less is known about chemosensitivity of MSI-H tumors in Lynch Syndrome CRC patients with germline MMR mutations. A phase II non-randomized clinical trial of methotrexate in Lynch Syndrome MSH2-deficient metastatic CRC is currently underway (MESH, NCT00952016) and 8-OHdG is being measured as a biomarker.
Conclusion
Deficient MMR and corresponding tumor MSI-H status has proven to be an important biomarker for prognosis and chemotherapy efficacy in CRC. Over the last decade, substantial data has accumulated to support the lack of efficacy of 5-FU based adjuvant chemotherapy, particularly in Stage II patients with dMMR tumors.
FOLFOX, continues to be the adjuvant standard of care in stage III disease, hence the combined use of Oxaliplatin or Irinotecan may overcome the lack of efficacy of 5-fluorouracil in dMMR tumors.
A better understanding of somatic genetics and molecular pathways involved in dMMR CRC is guiding continued research towards novel and tailored therapeutic strategies for this disease.
References
Landis SH et al (1999) Cancer statistics. CA Cancer J Clin 49(1):8–31, 1
Lynch HT (1985) Classics in oncology. Aldred Scott Warthin, M.D., Ph.D (1866–1931). CA Cancer J Clin 35(6):345–347
Lynch HT et al (1993) Genetics, natural history, tumor spectrum, and pathology of hereditary nonpolyposis colorectal cancer: an updated review. Gastroenterology 104(5):1535–1549
Fishel R et al (1993) The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell 75(5):1027–1038
Leach FS et al (1993) Mutations of a mutS homolog in hereditary nonpolyposis colorectal cancer. Cell 75(6):1215–1225
Peltomaki P et al (1993) Genetic mapping of a locus predisposing to human colorectal cancer. Science 260(5109):810–812
Nishisho I et al (1991) Mutations of chromosome 5q21 genes in FAP and colorectal cancer patients. Science 253(5020):665–669
Parsons R et al (1995) Microsatellite instability and mutations of the transforming growth factor beta type II receptor gene in colorectal cancer. Cancer Res 55(23):5548–5550
Rampino N et al (1997) Somatic frameshift mutations in the BAX gene in colon cancers of the microsatellite mutator phenotype. Science 275(5302):967–969
de la Chapelle A, Hampel H (2010) Clinical relevance of microsatellite instability in colorectal cancer. J Clin Oncol 28(20):3380–3387
Lindor NM et al (2002) Immunohistochemistry versus microsatellite instability testing in phenotyping colorectal tumors. J Clin Oncol 20(4):1043–1048
Boland CR et al (1998) A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58(22):5248–5257
Poynter JN et al (2008) Molecular characterization of MSI-H colorectal cancer by MLHI promoter methylation, immunohistochemistry, and mismatch repair germline mutation screening. Cancer Epidemiol Biomarkers Prev 17(11):3208–3215
Sinicrope FA (2010) DNA mismatch repair and adjuvant chemotherapy in sporadic colon cancer. Nat Rev Clin Oncol 7(3):174–177
Jass JR et al (1998) Morphology of sporadic colorectal cancer with DNA replication errors. Gut 42(5):673–679
Thibodeau SN, Bren G, Schaid D (1993) Microsatellite instability in cancer of the proximal colon. Science 260(5109):816–819
Lanza G et al (2006) Immunohistochemical test for MLH1 and MSH2 expression predicts clinical outcome in stage II and III colorectal cancer patients. J Clin Oncol 24(15):2359–2367
Sinicrope FA et al (2006) Prognostic impact of microsatellite instability and DNA ploidy in human colon carcinoma patients. Gastroenterology 131(3):729–737
Samowitz WS et al (2001) Microsatellite instability in sporadic colon cancer is associated with an improved prognosis at the population level. Cancer Epidemiol Biomarkers Prev 10(9):917–923
Popat S, Hubner R, Houlston RS (2005) Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 23(3):609–618
Gryfe R et al (2000) Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med 342(2):69–77
Hutchins G et al (2011) Value of mismatch repair, KRAS, and BRAF mutations in predicting recurrence and benefits from chemotherapy in colorectal cancer. J Clin Oncol 29(10):1261–1270
Moertel CG et al (1990) Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N Engl J Med 322(6):352–358
O’Connell MJ et al (1998) Prospectively randomized trial of postoperative adjuvant chemotherapy in patients with high-risk colon cancer. J Clin Oncol 16(1):295–300
Wolmark N et al (1993) The benefit of leucovorin-modulated fluorouracil as postoperative adjuvant therapy for primary colon cancer: results from National Surgical Adjuvant Breast and Bowel Project protocol C-03. J Clin Oncol 11(10):1879–1887
Wolmark N et al (1999) Clinical trial to assess the relative efficacy of fluorouracil and leucovorin, fluorouracil and levamisole, and fluorouracil, leucovorin, and levamisole in patients with Dukes’ B and C carcinoma of the colon: results from National Surgical Adjuvant Breast and Bowel Project C-04. J Clin Oncol 17(11):3553–3559
Andre T et al (2004) Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 350(23):2343–2351
Kuebler JP et al (2007) Oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: results from NSABP C-07. J Clin Oncol 25(16):2198–2204
Andre T et al (2009) Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 27(19):3109–3116
Ribic CM et al (2003) Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 349(3):247–257
Benson AB 3rd et al (2004) American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol 22(16):3408–3419
Kim GP et al (2007) Prognostic and predictive roles of high-degree microsatellite instability in colon cancer: a National Cancer Institute-National Surgical Adjuvant Breast and Bowel Project Collaborative Study. J Clin Oncol 25(7):767–772
Elsaleh H et al (2000) Association of tumour site and sex with survival benefit from adjuvant chemotherapy in colorectal cancer. Lancet 355(9217):1745–1750
Hemminki A et al (2000) Microsatellite instability is a favorable prognostic indicator in patients with colorectal cancer receiving chemotherapy. Gastroenterology 119(4):921–928
Sargent DJ et al (2010) Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol 28(20):3219–3226
Meyers M et al (2001) Role of the hMLH1 DNA mismatch repair protein in fluoropyrimidine-mediated cell death and cell cycle responses. Cancer Res 61(13):5193–5201
Arnold CN, Goel A, Boland CR (2003) Role of hMLH1 promoter hypermethylation in drug resistance to 5-fluorouracil in colorectal cancer cell lines. Int J Cancer 106(1):66–73
Pocard M et al (2000) Response to 5-fluorouracil of orthotopically xenografted human colon cancers with a microsatellite instability: influence of P53 status. Anticancer Res 20(1A):85–90
Parker WB, Cheng YC (1990) Metabolism and mechanism of action of 5-fluorouracil. Pharmacol Ther 48(3):381–395
Nehme A et al (1997) Differential induction of c-Jun NH2-terminal kinase and c-Abl kinase in DNA mismatch repair-proficient and -deficient cells exposed to cisplatin. Cancer Res 57(15):3253–3257
Fink D et al (1997) In vitro and in vivo resistance to cisplatin in cells that have lost DNA mismatch repair. Cancer Res 57(10):1841–1845
des Guetz G et al (2007) Microsatellite instability and sensitivitiy to FOLFOX treatment in metastatic colorectal cancer. Anticancer Res 27(4C):2715–2719
Kim ST et al (2010) Clinical impact of microsatellite instability in colon cancer following adjuvant FOLFOX therapy. Cancer Chemother Pharmacol 66(4):659–667
Kim ST et al (2010) The effect of DNA mismatch repair (MMR) status on oxaliplatin-based first-line chemotherapy as in recurrent or metastatic colon cancer. Med Oncol 27(4):1277–1285
Zaanan A et al (2010) Impact of p53 expression and microsatellite instability on stage III colon cancer disease-free survival in patients treated by 5-fluorouracil and leucovorin with or without oxaliplatin. Ann Oncol 21(4):772–780
Jacob S et al (2001) The role of the DNA mismatch repair system in the cytotoxicity of the topoisomerase inhibitors camptothecin and etoposide to human colorectal cancer cells. Cancer Res 61(17):6555–6562
Magrini R et al (2002) Cellular effects of CPT-11 on colon carcinoma cells: dependence on p53 and hMLH1 status. Int J Cancer 101(1):23–31
Charara M et al (2004) Microsatellite status and cell cycle associated markers in rectal cancer patients undergoing a combined regimen of 5-FU and CPT-11 chemotherapy and radiotherapy. Anticancer Res 24(5B):3161–3167
Fallik D et al (2003) Microsatellite instability is a predictive factor of the tumor response to irinotecan in patients with advanced colorectal cancer. Cancer Res 63(18):5738–5744
Vincent F et al (2009) Angiotensinogen delays angiogenesis and tumor growth of hepatocarcinoma in transgenic mice. Cancer Res 69(7):2853–2860
Bolderson E et al (2004) ATM is required for the cellular response to thymidine induced replication fork stress. Hum Mol Genet 13(23):2937–2945
Martin SA et al (2009) Methotrexate induces oxidative DNA damage and is selectively lethal to tumour cells with defects in the DNA mismatch repair gene MSH2. EMBO Mol Med 1(6–7):323–337
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Devaud, N., Gallinger, S. Chemotherapy of MMR-deficient colorectal cancer. Familial Cancer 12, 301–306 (2013). https://doi.org/10.1007/s10689-013-9633-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-013-9633-z