Abstract
Head injury is considered as a potential risk factor for amyotrophic lateral sclerosis (ALS). However, several recent studies have suggested that head injury is not a cause, but a consequence of latent ALS. We aimed to evaluate such a possibility of reverse causation with meta-analyses considering time lags between the incidence of head injuries and the occurrence of ALS. We searched Medline and Web of Science for case–control, cross-sectional, or cohort studies that quantitatively investigated the head-injury-related risk of ALS and were published until 1 December 2016. After selecting appropriate publications based on PRISMA statement, we performed random-effects meta-analyses to calculate odds ratios (ORs) and 95% confidence intervals (CI). Sixteen of 825 studies fulfilled the eligibility criteria. The association between head injuries and ALS was statistically significant when the meta-analysis included all the 16 studies (OR 1.45, 95% CI 1.21–1.74). However, in the meta-analyses considering the time lags between the experience of head injuries and diagnosis of ALS, the association was weaker (OR 1.21, 95% CI 1.01–1.46, time lag ≥ 1 year) or not significant (e.g. OR 1.16, 95% CI 0.84–1.59, time lag ≥ 3 years). Although it did not deny associations between head injuries and ALS, the current study suggests a possibility that such a head-injury-oriented risk of ALS has been somewhat overestimated. For more accurate evaluation, it would be necessary to conduct more epidemiological studies that consider the time lags between the occurrence of head injuries and the diagnosis of ALS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a rare neurodegenerative motor neuron disease that shows spreading weakness of the muscles and results in life-threatening situations, such as respiratory failure and dysphagia, within approximately 2–5 years following their diagnoses [1,2,3]. Previous epidemiological studies have linked the occurrence of ALS with a variety of environmental and occupational factors ranging from the history of military service [4,5,6] and physical activity [7,8,9,10,11,12] to the exposures to electric shock [13], several chemical substances [14], and particular metals [11, 15,16,17,18,19,20].
In particular, the link between the history of head traumas and the occurrence of ALS has repeatedly been argued for more than a century [21,22,23]. Although the first meta-analysis about this relationship found its statistical significance in 2007 [24], a consensus has not been fully reached mainly because of a concern of reverse causation [25, 26]: this association may be attributable to the data collected from ALS patients who experienced head injuries as an early symptom of undiagnosed ALS. In fact, some recent studies have reported that the head-injury-ALS association was not statistically significant when they excluded cases in which head traumas occurred less than 1 year before the ALS diagnosis [21, 27, 28].
To address this concern, we aimed to re-examine the association between the history of head trauma and the occurrence of ALS by conducting (1) an up-to-date meta-analysis including recent studies and (2) another meta-analysis that considered the time lags between the onset of head injuries and the diagnoses of the motor neuron disease.
Methods
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [29]. To evaluate the pooled odds ratio (OR) between the history of head injuries and the occurrence of ALS, we conducted meta-analyses using case–control, cross-sectional, or cohort studies that quantitatively investigated this association and were published on or before the 1st of December in 2016.
Data sources
A comprehensive literature search was conducted using PubMed and Web of Science. In PubMed, we used MeSH terms and searched for studies with either “Motor Neuron Disease” or “Amyotrophic Lateral Sclerosis” and either “Craniocerebral Trauma”, “Head Injuries, Closed”, “Head Injuries, Penetrating”, “Coma, Post-Head Injury”, or “Brain Injuries”. In Web of Science, we searched for studies that were classified as an “article” or a “review” in the domains of “science technology” or “social sciences”, and that include either “motor neuron disease” or “amyotrophic lateral sclerosis” and either “head injury”, “head trauma”, “craniocerebral trauma”, or “brain injury”. The lists of references cited in these retrieved articles and reviews were also examined, and relevant studies missed by the searches were added to the results reviewed in the following meta-analyses. Both searches were limited to English-written studies.
Eligibility criteria
Inclusion criteria were defined as: (1) quantitative epidemiological studies (i.e. cross-sectional, case–control, or cohort studies) that investigated the association between the history of head injuries and the occurrence of ALS, (2) studies that were published in scientific journals, (3) studies in which at least one group of participants was diagnosed with ALS, and (4) studies in which head injuries were defined based on medical records, military records, questionnaires, or self-reports. Exclusion criteria were defined as (1) studies that were not based on human data and (2) qualitative reviews.
Study identification
We screened titles, abstracts, and full texts of the studies found in the searches. After removing duplicated literature, irrelevant studies were excluded based on the eligibility criteria as follows. This process was confirmed by the authors separately.
First, we excluded studies whose titles included terms directly relevant to genetics, cell biology, or biochemistry (see Supplementary Methods). In every case of these exclusions, we reviewed the study’s entire title and re-confirmed that the study with such term(s) in its title was irrelevant to the current investigation. In addition to this procedure, four other studies with clearly irrelevant titles were excluded. Second, we examined the relevance of the remaining studies based on their abstracts, and excluded literature that was clearly irrelevant to this analysis (see Supplementary Methods). Finally, the full texts of all the remaining studies were reviewed, and irrelevant studies were excluded (see Supplementary Methods).
Data extraction and statistical analysis
We reviewed the remaining studies that met all the eligibility criteria, and extracted necessary data, which consisted of the number of ALS and control participants, the definition/diagnosis procedure of ALS, the definition of the history of head injury or presumably equivalent injuries, and statistics such as the OR, hazard ratio, and standardised morbidity ratio (Table 1). If a study in Table 1 used standardised morbidity ratio as an outcome, the ratio was treated as an OR in the current study. If the selected studies provided only hazard ratios, we transformed them to OR in accordance with Cochrane Handbook. If 90% CI was adopted in a selected study, it was transformed into 95% CI. When the selected studies did not contain such statistical information, we directly calculated crude ORs using the number of cases and controls reported there with a standard procedure.
Using these extracted and transformed data, we calculated combined ORs and its 95% CI in a random-effects model. Statistical heterogeneity was evaluated by visual inspection of Funnel plots, by conducting Chi squared tests, and by estimating the I 2 statistic that describes the percentage of observed heterogeneity that would not be expected by chance. These calculations were performed using RevMan Ver.5.0 (Nordic Cochrane Centre, Cochrane Collaboration 2009, Copenhagen, Denmark).
Meta-analysis using all the studies
We first performed a meta-analysis of the ORs using the data collected from all the selected studies. If one study had different ORs for different time lags, these ORs were merged within each study using a random-effects model.
Sensitivity analyses
Second, we examined the robustness of the result of meta-analysis using all the selected studies by conducting the following sensitivity analyses.
-
(I)
To control heterogeneity, we searched for studies that were the most responsible for the high heterogeneity in the original meta-analysis using all the studies. Technically, we repeatedly calculated the heterogeneity by omitting each study, and identified the studies the exclusion of which reduced the heterogeneity. Afterwards, we excluded the studies and conducted another meta-analysis.
-
(II)
To control differences in definition of ALS or head injuries, we conducted another sensitivity analysis after excluding studies whose ALS diagnoses were not based on ICD criteria, El Escorial criteria [30], or their equivalents, and studies whose definition of head injuries were not specific to the head or did not explicitly include the head.
-
(III)
To control differences in control individuals, we performed another meta-analysis excluding studies whose control groups consisted of non-healthy individuals.
-
(IV)
We also conducted another meta-analysis after excluding studies that did not provide adjusted ORs.
-
(V)
We conducted another meta-analysis after all the studies that were removed in the other four sensitivity analyses.
Meta-analyses considering the time lags between head injury and ALS
Second, we re-examined the association between the history of head injuries and the occurrence of ALS with considering the possibility of the reverse causation: technically, we used only studies in which ALS was diagnosed more than 1/3/5/10 years after the last incident of head injuries. These lengths of the time lag (i.e. 1–10 years) were determined because in the typical progression pattern of ALS, ALS symptoms sometimes do not clearly manifest in the first 1 or 2 years, whereas only 10% of ALS patients live more than 10 years after diagnosis [3].
Meta-analyses considering the age at head injuries and the repetition of head injuries
Additionally, according to previous studies [21, 24, 27, 31,32,33], we examined whether the association between the history of head injuries and the occurrence of ALS was affected by the following two factors: the age at head injuries and the repetition of head injuries.
The head injury-related risk of ALS considering the age at head injuries was evaluated by conducting meta-analyses using five studies that reported age-specific ORs [24, 27, 32,33,34]. To use as many studies as possible for the meta-analyses, we set the age threshold at 40 and did not distinguish the age of the last head trauma from that of the first one.
The ALS risk considering the number of head injuries was estimated by performing meta-analyses using six studies that reported different ORs for cases with different numbers of head injuries [21, 24, 27, 31,32,33].
Results
Literature search
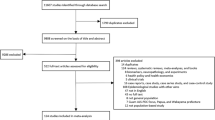
The current electronic literature search identified 118 potentially relevant studies in PubMed and 755 records in Web of Science (Fig. 1). After removing 48 duplicated studies, 570 records were excluded based on their titles, and 234 other studies were excluded based on their abstracts. After adding six articles that were used in a previous systematic meta-analysis [24] but were not detected in the electronic search, we examined full texts of the remaining 27 studies, and excluded 11 of them. Consequently, the remaining 16 studies, which consisted of 13 case–control studies and 3 retrospective cohort studies, were used in the following meta-analyses (Table 1) [21, 24, 27, 28, 31,32,33,34,35,36,37,38,39,40,41,42].
Meta-analysis using all the 16 studies
Although the heterogeneity across the analysed data was moderately large (I 2 38%), the meta-analysis using all the 16 articles found a statistically significant association between the occurrence of ALS and the experience of head injuries (OR 1.45, 95% CI 1.21–1.74, Fig. 2; Funnel plot, Fig. 3).
Sensitivity analysis I: controlling heterogeneity
As a first sensitivity analysis, we examined whether the primary result was preserved after controlling for heterogeneity.
Technically, we identified two studies the exclusion of which reduced the heterogeneity by repeatedly calculating the heterogeneity after excluding each study [36, 40]. The exclusion of a case–control study by Kondo and Tsubaki reduced the heterogeneity (I 2) from 38 to 0% [36], and that of another case–control study by Chiò et al. mitigated it from 38 to 12% [40]. In contrast, the exclusion of any of the other studies deteriorated the heterogeneity.
In addition to this operational reason, the insufficient quality of the control groups in these two studies could be another reason to exclude them [36, 40]. In the first study [36], its controls consisted of the spouses of the ALS patients, and thus, sex difference would not be sufficiently controlled. Moreover, considering that spouses are likely to share a large part of behavioural and environmental factors, such a choice of controls is likely to increase the homogeneity artificially, which could result in a biased observation. In the second study [40], its controls were not healthy individuals like most of the other studies, but mostly patients with non-ALS neurological diseases. Given that some other neurological diseases may be associated with the history of head injuries [43,44,45], such a control group would underestimate the head-injury-related risk for ALS.
Considering these quantitative and qualitative observations, we conducted a new meta-analysis after excluding the two case–control studies [36, 40], and confirmed the robustness of the primary results (OR 1.45, 95% CI 1.27–1.66, heterogeneity I 2 0%).
Sensitivity analysis II: controlling differences in ALS/head injury definition
Second, we conducted another sensitivity analysis after excluding a study whose ALS diagnosis was not explicitly based on El Escorial criteria or ICDs [34] and other three research whose definition of injuries are not specified to the head or obscure [35, 37, 40]. Even after this exclusion of the four studies, we could still observe a significant association between head injuries and ALS (OR 1.54, 95% CI 1.29–1.85, heterogeneity I 2 26%).
Sensitivity analysis III: controlling the heterogeneity of the control groups
The third sensitivity analysis excluded six studies whose control groups did not consist of healthy individuals [31, 38,39,40,41], and still found a statistically significant head-injury-related risk for ALS (OR 1.45, 95% CI 1.13–1.86, heterogeneity I 2 57%).
Sensitivity analysis IV: excluding crude ORs
To control for the potential confounding factors such as sex and age, the fourth sensitivity analysis was performed after excluding four studies that did not explicitly report adjusted ORs [35, 36, 38, 39]. Even in this analysis, the significant association between head injury history and ALS occurrence was preserved (OR 1.36, 95% CI 1.18–1.57; heterogeneity I 2 10%).
Sensitivity analysis V: excluding the nine studies used in the above sensitivity analyses
Finally, we conducted another sensitivity analysis after excluding all the nine studies [31, 34,35,36,37,38,39,40,41] that had been removed in the above-described four sensitivity analyses, and confirmed the association (OR 1.42, 95% CI 1.21–1.66, heterogeneity I 2 0%).
Meta-analyses considering time lags between head injuries and ALS
We then conducted a secondary meta-analysis that considered the time lags between the last incident of head injuries and the diagnosis of ALS (Fig. 4). This analysis was performed using six of the 16 selected studies [21, 27, 28, 33, 38, 42], only which calculated different adjusted ORs for different time lags. If one study showed different ORs for different time lags, these ORs were merged into one pooled OR within the study using a random-effects model.
When the analysis was conducted in individuals who experienced their head injury at least 1 year before being diagnosed with ALS using the six studies [21, 27, 28, 33, 38, 42], the pooled OR was marginally significant (OR 1.21, 95% CI 1.01–1.46; heterogeneity I 2 20%; Fig. 2a). This pooled OR did not survive statistically after we excluded one study [38] that was removed in the sensitivity analysis V (OR 1.91, 95% CI 0.98–1.44).
This association was not significant for the longer time lag. When the time lag was set at ≥ 3 years, the pooled OR based on eight ORs listed in four studies [21, 22, 28, 33, 42] was 1.16 (95% CI 0.84–1.59; Fig. 4b). For ≥ 5-year time lag, the pooled OR based on seven ORs in the same four studies [21, 22, 28, 33, 42] was 1.18 (95% CI 0.85–1.64; Fig. 4c). For ≥ 10-year time lag, the OR based on three ORs in two studies [21, 28] was 1.05 (95% CI 0.74–1.50; Fig. 4c). Note that these analyses did not include any study that was excluded in the above-stated sensitivity analysis V; therefore, the results were not affected even when we controlled possible confounding factors. In addition, these observations were qualitatively preserved when we did not merge different ORs within each study (Supplementary Table 1).
ALS risk considering the age at head injuries and the repetition of head injuries
We also examined the head injury-related risk of ALS by considering two potential confounding factors: the age at head injuries and the repetition of head injuries.
First, the ORs considering the age at head injuries were evaluated using five studies that explicitly described such ages and calculated different ORs for different age group [24, 27, 32,33,34] (Table 1). When the age at head injuries was ≤ 40 years, the pooled OR was 1.20 (95% CI 0.88–1.63; Supplementary Fig. 1a), which was qualitatively preserved after we excluded one study [34] that was removed in the above sensitivity analysis V (OR 1.21, 95% CI 0.86–1.70). When the age was > 40 years, the pooled OR showed a slightly lower figure (OR 1.08, 95% CI 0.62–1.89; Supplementary Fig. 1b), which was not affected by the sensitivity analysis V because none of the studies used in this meta-analysis was removed in the sensitivity analysis.
In this analysis, we did not distinguish the age of the last injury from that of the first one due to the small number of each type of study: four of the five studies used here reported the age at the last injury [24, 27, 32, 34], whereas one study stated that at the first trauma [33]. However, in this first-trauma-based study [33], more than 85% of individuals with any history of head injuries experienced only a single head trauma (Supplementary Table 2); therefore, the age at the first head injury in this study was expected to be close to that at the last head injury. Given this, we may be able to interpret that the result of this meta-analysis indicates the effects of the age at the last head injury on the head trauma-related risk of ALS.
Second, the ORs considering the number of head injuries were estimated using six studies that calculated different ORs for different numbers of head injuries [21, 24, 27, 31,32,33] (Table 1). When focusing on cases with only one head injury, we found a significant association between the head injury and ALS occurrence (OR 1.23, 95% CI 1.08–1.42; Supplementary Fig. 2a). In contrast, such a significant association was not seen when we focused on cases with multiple head injuries (OR 1.17, 95% CI 0.73–1.89; Supplementary Fig. 2b). Both observations were qualitatively preserved even after we excluded one study [31] that was removed in the above sensitivity analysis V (One head injury, OR 1.18, 95% CI 1.01–1.38; Multiple head injuries, OR 1.00, 95% CI 0.70–1.42).
Discussion
Consistent with a previous meta-analysis conducted in 2007 (OR 1.7, 95% CI 1.3–2.2) [24], our analysis has confirmed a significant association between the history of head injuries and the occurrence of ALS even after including the most recent results (OR 1.45, 95% CI 1.21–1.74). In addition, the association was robust against the multiple sensitivity analyses controlling several confounding factors. However, this head-injury-ALS link was merely marginal or not significant when the meta-analyses considered the possibility of the reverse causation. These results suggest that although we cannot deny it, the association between head injuries and ALS may have been overestimated.
The influence of such reverse causation between the history of head injuries and the occurrence of ALS has been repeatedly argued [22, 46,47,48,49]. A recent case–control study has also suggested that the head-injury-related risk of ALS became statistically insignificant when they excluded the cases whose time lags between the experience of head injuries and the ALS diagnosis were less than 1 year [21]. The results of the current time-lag meta-analysis add further evidence for this concern, which indicates the necessity of more epidemiological studies that consider such time lags between head injuries and ALS for more accurate evaluation of the head-injury-oriented risk of the motor neuron disease.
In the meantime, we should note that this potential reverse causation is not the only way to interpret the current findings of the time-lag analyses. For example, recall bias caused by cognitive impairments in ALS [50] may underlie this observation. If ALS patients had more difficulty in remembering their experiences of old traumas due to their cognitive impairments than the controls, the association between the history of old head injuries and the occurrence of ALS would be underestimated.
Statistically, the current observation using all the 16 studies was not necessarily preserved in the additional meta-analyses considering the age at head injuries and the number of the head injuries (Supplementary Figs. 1 and 2). Qualitatively, however, these results classified by the age and injury repetition were consistent with previous epidemiological and biological literature [27, 32, 33, 51]. The higher ALS risk in individuals with head injuries at younger ages (Supplementary Fig. 1) is consistent with the previous case–control study [32, 33] and may be explained by the higher levels of some hormones, such as testosterone, during young ages [51]. The higher ALS risk in cases with not multiple but a single head injury is also consistent with the previous epidemiological studies [27, 32, 33]. In the meantime, we should note that these observations are not conclusive because the numbers of the studies considering the ages at injuries and the injury repetition are limited and some potential confounding factors may be not controlled sufficiently. For example, the larger risk of ALS for single head injury might be affected by recall bias and the severity of the injuries, because individuals who experienced a severe head injury may be more likely to recall the heavy trauma only.
Head-injury-related risks have been investigated in other neurological diseases, such as multiple sclerosis (MS), Parkinson’s disease (PD), and Alzheimer’s disease (AD), and similarly to ALS, the associations between these three diseases and the history of head traumas are still somewhat controversial. For example, several meta-analyses reported a significant head-injury-related risk for MS [45, 52, 53], but a recent meta-analysis could not find such a significant association when it focused on the results of cohort studies [45]. For PD, some meta-analyses reported that the history of head injuries is a risk factor for the disease [23, 54, 55]; however, a recent large-scale case–control study could not reproduce the finding, and implied that such seemingly significant associations between head injuries and PD could be explained by reverse causality [56]. For AD, a meta-analysis reported a significant link between AD and the history of head injuries [44], but a recent large-scale cohort study could not find a significant association [57], which has cast doubt on the causal link between head injuries and AD [58]. These situations are similar to that of studies on the association between head injuries and ALS, and therefore, future studies about head-injury-related risks for these neurological diseases may need comprehensive consideration about a wide range of confounding factors, including the repetition of head traumas, the age at head injury, the severity of the injuries, and the effects of reverse causality.
The current result of the primary meta-analysis (Fig. 2) could contain four methodological limitations: regional and ethnical diversity, recall bias, publication bias, and selection bias.
First, it was difficult to entirely control the influence of the diversity across regions and ethnicities. The prevalence rate of ALS is known to widely vary among geographically different regions or different ethnic groups [2, 49, 59,60,61]. Such diversity in the prevalence rate could affect the statistical estimation of the association between head injuries and ALS.
Second, the current information about the history of head injuries may have been influenced by recall bias, because most of the studies used here investigated individual histories of head injuries using questionnaires (Table 1). Thus, the definition of head injury could be different between different individuals, and the information about the head injury experience could be severely affected by recall bias. In particular, after the potential association between head injuries and ALS was publicly disseminated [62], patients with ALS may become more likely to reflect on their experience of physical accidents—including head injuries—and to remember such events than control groups. Moreover, 13 of the 16 studies used in the primary meta-analysis are not cohort but case–control studies (Table 1), and their results would be confounded by various factors including recall bias and selection bias. Although a meta-analysis using the remaining three cohort studies [28, 34, 41] yielded qualitatively the same OR (1.45, 95% CI 1.05–2.01), it should be noted that the current result may overestimate the association between history of head injuries and occurrence of ALS.
Third, the current meta-analyses could be affected by publication bias. The funnel plot for the primary meta-analysis using all the 16 studies (Fig. 3) implies the possibility that researchers are not likely to report small studies when they have found positive associations between head injuries and ALS (here, OR > 1).
Forth, the current analyses used three studies that were based on hospital-based datasets [24, 32, 40], which would potentially induce selection bias. In particular, given the low prevalence of ALS, such selection bias could be enlarged [63]. Although the exclusion of the three hospital-based studies did not affect the result qualitatively (a new pooled OR without the three studies = 1.55, 95% CI 1.31–1.83), we need to care about this confounding effect of the publication bias when interpreting the current observations.
The observations in the time-lag analyses (Fig. 4) could also be affected by the small number of studies and several residual confounding factors.
First, the current time-lag meta-analysis was based on a relatively small number of studies. This small number may be partly because quantitative investigations considering the time lags were not intensively conducted until recently. Therefore, it would be necessary to re-evaluate the current findings after more studies considering the time lags have been published.
In addition, these time-lag analyses could be more affected by multiple residual confounding factors compared to the primary meta-analysis.
For example, differently from the primary meta-analysis, the time-lag analyses mainly used epidemiological studies that were based on nation-wide medical registries: in fact, five of the six studies employed here analysed large population-based datasets (Table 1) [21, 27, 28, 33, 42]. Such well-characterised and comprehensive medical records allowed the estimation of ALS risk considering the time lags between the head injuries and the occurrence of ALS. However, these official registries often defined “head injury” as “head traumas that required medical cares” (Table 1), and thus, the studies using such nation-wide datasets may underestimate the number of head injuries and the associations between ALS and minor head traumas.
Moreover, the time-lag analyses may be more affected by population bias than the primary analysis. Four of the six studies used in the time-lag analyses were based on datasets mainly collected from Germanic people (i.e. English [28], Swedish [21], Dutch [42], and Danes [33]). Given a substantial heterogeneity of the incidence rate of ALS across different ethnic groups [2, 49, 59,60,61, 64, 65], the current results of the time-lag analyses should be tested for different ethnicities.
The current up-to-date meta-analysis has confirmed a significant association between the history of head injuries and the occurrence of ALS. However, the association was merely marginal or not significant when the analyses considered the possibility of the reverse causation. These observations have implied that the head-injury-oriented risk of ALS may have been overestimated and shown the necessity of more epidemiological investigations that minimize the effects of the reverse causation.
References
Rowland LP, Shneider NA. Amyotrophic lateral sclerosis. N Engl J Med. 2001;344:1688–700.
Chiò A, Logroscino G, Traynor BJ, Collins J, Simeone JC, Goldstein LA, et al. Global epidemiology of amyotrophic lateral sclerosis: a systematic review of the published literature. Neuroepidemiology. 2013;41:118–30.
Swinnen B, Robberecht W. The phenotypic variability of amyotrophic lateral sclerosis. Nat Rev Neurol. 2014;10:661–70.
Haley RW. Excess incidence of ALS in young Gulf War veterans. Neurology. 2003;61:750–6.
Horner RD, Kamins KG, Feussner JR, Grambow SC, Hoff-Lindquist J, Harati Y, et al. Occurrence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology. 2003;61:742–9.
Weisskopf MG, O’Reilly EJ, McCullough ML, Calle EE, Thun MJ, Cudkowicz M, et al. Prospective study of military service and mortality from ALS. Neurology. 2005;64:32–7.
Longstreth WT, McGuire V, Koepsell TD, Wang Y, van Belle G. Risk of amyotrophic lateral sclerosis and history of physical activity: a population-based case-control study. Arch Neurol. 1998;55:201–6.
Scarmeas N, Shih T, Stern Y, Ottman R, Rowland LP. Premorbid weight, body mass, and varsity athletics in ALS. Neurology. 2002;59:773–5.
Chiò A, Benzi G, Dossena M, Mutani R, Mora G. Severely increased risk of amyotrophic lateral sclerosis among Italian professional football players. Brain. 2005;128:472–6.
Veldink JH, Kalmijn S, Groeneveld GJ, Titulaer MJ, Wokke JHJ, van den Berg LH. Physical activity and the association with sporadic ALS. Neurology. 2005;64:241–5.
Felmus MT, Patten BM, Swanke L. Antecedent events in amyotrophic lateral sclerosis. Neurology. 1976;26:167–72.
Gallo V, Vanacore N, Bueno-de-Mesquita HB, Vermeulen R, Brayne C, Pearce N, et al. Physical activity and risk of amyotrophic lateral sclerosis in a prospective cohort study. Eur J Epidemiol. 2016;31:255–66.
Abhinav K, Al-Chalabi A, Hortobagyi T, Leigh PN. Electrical injury and amyotrophic lateral sclerosis: a systematic review of the literature. J Neurol Neurosurg Psychiatry. 2007;78:450–3.
Gallo V, Bueno-de-Mesquita HB, Vermeulen R, Andersen PM, Kyrozis A, Linseisen J, et al. Smoking and risk for amyotrophic lateral sclerosis: analysis of the EPIC cohort. Ann Neurol. 2009;65:378–85.
Kamel F, Umbach DM, Hu H, Munsat TL, Shefner JM, Taylor JA, et al. Lead exposure as a risk factor for amyotrophic lateral sclerosis. Neurodegener Dis. 2005;2:195–201.
Wang N, Gray M, Lu X-H, Cantle JP, Holley SM, Greiner E, et al. Neuronal targets for reducing mutant huntingtin expression to ameliorate disease in a mouse model of Huntington’s disease. Nat Med. 2014;20:536–41.
Perl DP, Gajdusek DC, Garruto RM, Yanagihara RT, Gibbs CJ. Intraneuronal aluminum accumulation in amyotrophic lateral sclerosis and Parkinsonism-dementia of Guam. Science. 1982;217:1053–5.
Gresham LS, Molgaard CA, Golbeck AL, Smith R. Amyotrophic lateral sclerosis and occupational heavy metal exposure: a case-control study. Neuroepidemiology. 1986;5:29–38.
Mitchell JD. Heavy metals and trace elements in amyotrophic lateral sclerosis. Neurol Clin. 1987;5:43–60.
Armon C, Kurland LT, Daube JR, O’Brien PC. Epidemiologic correlates of sporadic amyotrophic lateral sclerosis. Neurology. 1991;41:1077–84.
Peters TL, Fang F, Weibull CE, Sandler DP, Kamel F, Ye W. Severe head injury and amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14:267–72.
Fournier CN, Gearing M, Upadhyayula SR, Klein M, Glass JD. Head injury does not alter disease progression or neuropathologic outcomes in ALS. Neurology. 2015;84:1788–95.
Perry DC, Sturm VE, Peterson MJ, Pieper CF, Bullock T, Boeve BF, et al. Association of traumatic brain injury with subsequent neurological and psychiatric disease: a meta-analysis. J Neurosurg. 2016;124:511–26.
Chen H, Richard M, Sandler DP, Umbach DM, Kamel F. Head injury and amyotrophic lateral sclerosis. Am J Epidemiol. 2007;166:810–6.
Fondell E, Fitzgerald KC, Falcone GJ, O’Reilly EJ, Ascherio A. Early-onset alopecia and amyotrophic lateral sclerosis: a cohort study. Am J Epidemiol. 2013;178:1146–9.
Pearce N, Gallo V, McElvenny D. Head trauma in sport and neurodegenerative disease: an issue whose time has come? Neurobiol Aging. 2015;36:1383–9.
Schmidt S, Kwee LC, Allen KD, Oddone EZ. Association of ALS with head injury, cigarette smoking and APOE genotypes. J Neurol Sci. 2010;291:22–9.
Turner MR, Abisgold J, Yeates DGR, Talbot K, Goldacre MJ. Head and other physical trauma requiring hospitalisation is not a significant risk factor in the development of ALS. J Neurol Sci. 2010;288:45–8.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535–b25345.
Brooks BR, Miller RG, Swash M, Munsat TL, World Federation of Neurology Research Group on Motor Neuron Diseases. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293–309.
Pupillo E, Messina P, Logroscino G, Zoccolella S, Chiò A, Calvo A, et al. Trauma and amyotrophic lateral sclerosis: a case-control study from a population-based registry. Eur J Neurol. 2012;19:1509–17.
Binazzi A, Belli S, Uccelli R, Desiato MT, Talamanca IF, Antonini G, et al. An exploratory case-control study on spinal and bulbar forms of amyotrophic lateral sclerosis in the province of Rome. Amyotroph Lateral Scler. 2009;10:361–9.
Seals RM, Hansen J, Gredal O, Weisskopf MG. Physical trauma and amyotrophic lateral sclerosis: a population-based study using Danish National registries. Am J Epidemiol. 2016;183:294–301.
Savica R, Parisi JE, Wold LE, Josephs KA, Ahlskog JE. High school football and risk of neurodegeneration: a community-based study. Mayo Clin Proc. 2012;87:335–40.
Kurtzke JF, Beebe GW. Epidemiology of amyotrophic lateral sclerosis 1. A case-control comparison based on ALS deaths. Neurology. 1980;30:453–63.
Kondo K, Tsubaki T. Case-control studies of motor neuron disease: association with mechanical injuries. Arch Neurol. 1981;38:220–6.
Deapen DM, Henderson BE. A case-control study of amyotrophic lateral sclerosis. Am J Epidemiol. 1986;123:790–9.
Gallagher JP, Sanders M. Trauma and amyotrophic lateral sclerosis: a report of 78 patients. Acta Neurol Scand. 1987;75:145–50.
Granieri E, Carreras M, Tola R, Paolino E, Tralli G, Eleopra R, et al. Motor neuron disease in the province of Ferrara, Italy, in 1964–1982. Neurology. 1988;38:1604–8.
Chiò A, Meineri P, Tribolo A, Schiffer D. Risk factors in motor neuron disease: a case-control study. Neuroepidemiology. 1991;10:174–84.
Williams DB, Annegers JF, Kokmen E, O’Brien PC, Kurland LT. Brain injury and neurologic sequelae: a cohort study of dementia, parkinsonism, and amyotrophic lateral sclerosis. Neurology. 1991;41:1554–7.
Seelen M, van Doormaal PTC, Visser AE, Huisman MHB, Roozekrans MHJ, de Jong SW, et al. Prior medical conditions and the risk of amyotrophic lateral sclerosis. J Neurol. 2014;261:1949–56.
Jafari S, Etminan M, Aminzadeh F, Samii A. Head injury and risk of Parkinson disease: a systematic review and meta-analysis. Mov Disord. 2013;28:1222–9.
Li Y, Li Y, Li X, Zhang S, Zhao J, Zhu X, et al. Head injury as a risk factor for dementia and Alzheimer’s disease: a systematic review and meta-analysis of 32 observational studies. PLoS ONE. 2017;12:e0169650.
Lunny CA, Fraser SN, Knopp-Sihota JA. Physical trauma and risk of multiple sclerosis: a systematic review and meta-analysis of observational studies. J Neurol Sci. 2014;336:13–23.
Armon C, Nelson LM. Is head trauma a risk factor for amyotrophic lateral sclerosis? An evidence based review. Amyotroph Lateral Scler. 2012;13:351–6.
Pinto S, Swash M, de Carvalho M. Does surgery accelerate progression of amyotrophic lateral sclerosis? J Neurol Neurosurg Psychiatry. 2014;85:643–6.
Hamidou B, Couratier P, Besançon C, Nicol M, Preux PM, Marin B. Epidemiological evidence that physical activity is not a risk factor for ALS. Eur J Epidemiol. 2014;29:459–75.
Chancellor AM, Warlow CP. Adult onset motor neuron disease: worldwide mortality, incidence and distribution since 1950. J Neurol Neurosurg Psychiatry. 1992;55:1106–15.
Phukan J, Pender NP, Hardiman O. Cognitive impairment in amyotrophic lateral sclerosis. Lancet Neurol. 2007;6:994–1003.
Wicks P. Hypothesis: higher prenatal testosterone predisposes ALS patients to improved athletic performance and manual professions. Amyotroph Lateral Scler. 2012;13:251–3.
Warren SA, Olivo SA, Contreras JF, Turpin KVL, Gross DP, Carroll LJ, et al. Traumatic injury and multiple sclerosis: a systematic review and meta-analysis. Can J Neurol Sci. 2013;40:168–76.
Belbasis L, Bellou V, Evangelou E, Ioannidis JPA, Tzoulaki I. Environmental risk factors and multiple sclerosis: an umbrella review of systematic reviews and meta-analyses. Lancet Neurol. 2015;14:263–73.
Jafari S, Etminan M, Aminzadeh F, Samii A. Head injury and risk of Parkinson disease: a systematic review and meta-analysis. Mov Disord. 2013;28:1222–9.
Noyce AJ, Bestwick JP, Silveira-Moriyama L, Hawkes CH, Giovannoni G, Lees AJ, et al. Meta-analysis of early nonmotor features and risk factors for Parkinson disease. Ann Neurol. 2012;72:893–901.
Kenborg L, Rugbjerg K, Lee P-C, Ravnskjær L, Christensen J, Ritz B, et al. Head injury and risk for Parkinson disease: results from a Danish case-control study. Neurology. 2015;84:1098–103.
Crane PK, Gibbons LE, Dams-O’Connor K, Trittschuh E, Leverenz JB, Keene CD, et al. Association of traumatic brain injury with late-life neurodegenerative conditions and neuropathologic findings. JAMA Neurol. 2016;73:1062–9.
Weiner MW, Crane PK, Montine TJ, Bennett DA, Veitch DP. Traumatic brain injury may not increase the risk of Alzheimer disease. Neurology. 2017. doi:10.1212/WNL.0000000000004608.
Román GC. Neuroepidemiology of amyotrophic lateral sclerosis: clues to aetiology and pathogenesis. J Neurol Neurosurg Psychiatry. 1996;61:131–7.
Cronin S, Hardiman O, Traynor BJ. Ethnic variation in the incidence of ALS: a systematic review. Neurology. 2007;68:1002–7.
Wolfson C, Kilborn S, Oskoui M, Genge A. Incidence and prevalence of amyotrophic lateral sclerosis in Canada: a systematic review of the literature. Neuroepidemiology. 2009;33:79–88.
Robbins L, Conidi F. Stop football … save brains: a point counterpoint discussion. Headache. 2013;53:817–23.
Logroscino G, Traynor BJ, Hardiman O, Chiò A, Couratier P, Mitchell JD, et al. Descriptive epidemiology of amyotrophic lateral sclerosis: new evidence and unsolved issues. J Neurol Neurosurg Psychiatry. 2008;79:6–11.
Malaspina A, Zaman R, Mazzini L, Camana C, Poloni E, Curti D, et al. Heterogeneous distribution of amyotrophic lateral sclerosis patients with SOD-1 gene mutations: preliminary data on an Italian survey. J Neurol Sci. 1999;162:201–4.
Marin B, Boumédiene F, Logroscino G, Couratier P, Babron M-C, Leutenegger AL, et al. Variation in worldwide incidence of amyotrophic lateral sclerosis: a meta-analysis. Int J Epidemiol. 2017;46:57–74.
Acknowledgements
We acknowledge Dr Valentina Gallo for her support. TW acknowledges the support from European Commission.
Author contribution
YW designed the study. YW and TW conducted the analyses and wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Watanabe, Y., Watanabe, T. Meta-analytic evaluation of the association between head injury and risk of amyotrophic lateral sclerosis. Eur J Epidemiol 32, 867–879 (2017). https://doi.org/10.1007/s10654-017-0327-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-017-0327-y