Abstract
To investigate the prevalence of frailty in a Dutch elderly population and to identify adverse health outcomes associated with the frailty phenotype independent of the comorbidities. Cross-sectional and longitudinal analyses within the Rotterdam Study (the Netherlands), a prospective population-based cohort study in persons aged ≥55 years. Frailty was defined as meeting three or more of five established criteria for frailty, evaluating nutritional status, physical activity, mobility, grip strength and exhaustion. Intermediate frailty was defined as meeting one or two frailty criteria. Comorbidities were objectively measured. Health outcomes were assessed by means of questionnaires, physical examinations and continuous follow-up through general practitioners and municipal health authorities for mortality. Of 2,833 participants (median age 74.0 years, inter quartile range 9) with sufficiently evaluated frailty criteria, 163 (5.8 %) participants were frail and 1,454 (51.3 %) intermediate frail. Frail elderly were more likely to be older and female, to have an impaired quality of life and to have fallen or to have been hospitalized. 108 (72.0 %) frail participants had ≥2 comorbidities, compared to 777 (54.4 %) intermediate frail and 522 (44.8 %) non-frail participants. Adjusted for age, sex and comorbidities, frail elderly had a significantly increased risk of dying within 3 years (HR 3.4; 95 % CI 1.9–6.4), compared to the non-frail elderly. This study in a general Dutch population of community-dwelling elderly able to perform the frailty tests, demonstrates that frailty is common and that frail elderly are at increased risk of death independent of comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
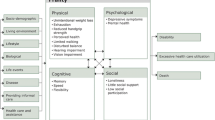
Elderly people of the same chronological age demonstrate that there is a large heterogeneity in terms of biological age [1, 2]. Some are still fit and energetic while a relatively large number of elderly people has an accelerated decline in well-being and resilience [3]. Given the expanding elderly population and the major impact on health and social care, the identification of this frail group of elderly, which could benefit from more adequate interventions, becomes of increasing interest [3]. Frailty is defined as a biological syndrome in which a progressive, cumulative decline in the reserve capacity of multiple physiological systems elicits an abnormal vulnerability to common stressors [4]. In short, frailty could be defined as the disability to compensate function loss. Increasing evidence suggests that frail elderly are at an increased risk of adverse health outcomes (disability, falls, hospitalizations, institutionalizations and death) [4–8]. Conceptually, it is important to distinguish “frailty” from “disability” and “comorbidity” and therefore, not to use an instrument integrating disability or comorbidity items to measure frailty [9]. In the Cardiovascular Health Study, more than a quarter of the elderly categorized as frail according to the Fried frailty criteria were not disabled and had no comorbidity [4]. However, these three different entities are related [3]. Those who are frail have a higher prevalence of concomitant chronic diseases and of disability than those who are non-frail. Moreover, comorbidity is a risk factor for frailty, whereas disability is an adverse outcome of frailty and disability may aggravate frailty [10]. Because of the complex relationship between comorbidity and frailty, it is not always clear whether frailty is a predictor of mortality independent of comorbidities. To our knowledge, the very few studies who investigated the association between frailty and mortality only adjusted for some selected, mainly self-reported, chronic diseases [4, 6–8, 11].
An unambiguous definition of frailty is of great importance for clinicians to identify those at an increased risk of adverse health outcomes, but also for policy makers to make cost-effective decisions in health care [2]. Since there is no distinct uniform definition of frailty, reported prevalences vary greatly from 5 to 58 % [12]. Generally, two different definitions of frailty are most commonly used [2]: a broader definition of frailty taking into account more social and psychological aspects [5]; and one based on predominantly physical criteria [4]. Within the latter definition based on physical aspects, frailty is defined as meeting three or more of five established criteria for frailty, namely evaluating: (1) nutritional status (unintentional weight loss), (2) physical activity, (3) mobility (slow walking speed), (4) weakness (reduced grip strength), and (5) exhaustion (self-reported) [4]. Elderly individuals with one or two criteria are defined as intermediate frail or pre-frail and have been found to be at increased risk of becoming frail [4]. The physical frailty definition by Fried et al. [4] is associated with a lower prevalence and less variable prevalence rates. Although it is suggested that frailty is more than a decline in physical functions, the model based on physical aspects is more practical for fundamental research since the criteria are limited in number, has clear cut-offs between frail versus non frail and constitutes a more objective measure [2, 12]. Moreover, the frailty phenotype by Fried et al is the most widely used instrument in frailty research, allowing comparisons with other studies, and has been most extensively tested for its validity, including the external validity of adverse health outcomes [4, 9].
The aim was to investigate the prevalence of physically frail elderly in a Dutch population-based cohort study and the impact on adverse health outcomes including all-cause mortality independent of comorbidity.
Methods
Study population and design
This study was embedded within cohort I and II (RSI and RSII) from the Rotterdam Study, a prospective population-based cohort study ongoing since 1990 [13]. The rationale and design of the Rotterdam Study have been extensively described [13–18]. In short, all inhabitants aged 55 years and older of one district of Rotterdam (Ommoord) were invited to the original cohort (RSI). Names and addresses were drawn from the municipal register which is reliable, complete and up to date [14]. 7,983 subjects participated (78 % of 10,215 invitees). 3,011 participants (out of 4,472 invitees) who had become 55 years of age or moved into the study district since the start of the study were added as RSII in 1999. Almost all participants are from Caucasian descent. All participants are invited every 3–5 years to the research centre for follow-up examinations, including physical examination and blood sampling. Moreover, the participants are continuously monitored for clinically meaningful outcomes. The assessment of the study participants’ characteristics and frailty criteria used in this study took place from March 2009 until March 2012 among 4,027 participants. The follow-up period started at the time of the frailty-assessment until death or end of the study period (January 1st, 2013). This study was approved by the medical ethics committee of the Erasmus Medical Center, Rotterdam, and the review board of The Netherlands Ministry of Health, Welfare and Sports. Participants gave written informed consent.
Definition of frailty
Frailty was determined using the physical definition of frailty, which has been developed in the population-based Cardiovascular Health Study and is since then the most widely used and validated instrument in frailty research [4, 9, 19]. Frailty was defined as meeting three or more of the five established frailty criteria. Grip strength was assessed using a handgrip dynamometer and the grip strength was defined as the highest value (kg) of three trials performed in the non-dominant hand [13]. Weakness was defined as having a grip strength for men ≤29 kg (if body mass index (BMI) ≤24, or ≤30 kg if BMI ≤24.1–28, or ≤32 kg if BMI >28) and for women ≤17 kg (if BMI ≤23, or ≤17.3 kg if BMI ≤23.1–26, or ≤18 kg if BMI ≤26.1–29, or ≤21 kg if BMI >29) [4]. Weight loss was defined as losing more than 5 % body weight compared to the previous examination (6 years earlier). Exhaustion was defined as answering “frequently” or “mostly” to one of the following two statements from the Center for Epidemiological Studies Depression (CES-D) scale: (a) I felt that everything I did was an effort; (b) I could not get going [20]. Physical activity was determined from an extensive questionnaire about leisure time and sports; the physical activities were weighted by their intensity and all awarded kilocalories per week were summed [4, 21]. Low physical activity was defined as expending <383 kcal per week for men and <270 kcal per week for women [4]. Finally, slowness was defined as walking at a velocity of <0.76 m/s if height was more than 173 cm for men or more than 159 cm for women (otherwise <0.65 m/s) [4]. Assessment of gait was performed in all participants using the GAITRite walkway (CIR Systems, Inc., Sparta, New Jersey). Only participants who had a sufficient number of criteria to confirm or to exclude frailty were included (e.g. at least three concordant positive or negative criteria evaluated). Participants with one or two criteria were defined as intermediate frail or pre-frail [4].
Characteristics, comorbidities and adverse health outcomes
Standardized questionnaires including information on smoking status, pack-years, falls and hospitalizations, were completed at the time of the frailty-assessment in the research center. Participants were asked “Did you fall in the past 12 months?” and “Have you been hospitalized in the past 12 months?”. Mortality information was obtained from the municipal health authorities in Rotterdam in addition to computerized reports from the general practitioners [13]. Smoking status was distinguished into never, former, and current smoking. Cigarette pack-years were computed as duration of smoking (years) multiplied by the number of smoked cigarettes, divided by 20. The BMI was calculated as weight divided by height squared.
Diabetes mellitus was defined as the use of blood glucose-lowering medication based on automated pharmacy records [22]. Chronic obstructive pulmonary disease (COPD) was assessed by spirometry, performed at the research center. The participants were classified as having COPD when the ratio of forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC) was <70 %, in the absence of asthma [23]. Hypertension was defined as the use of antihypertensive medication during follow-up, and/or a systolic brachial blood pressure of ≥160 mmHg, and/or a diastolic brachial blood pressure of ≥100 mmHg (Grade 2 according to European Society of Cardiology criteria) [24]. Coronary revascularization was defined as coronary artery bypass grafting and percutaneous coronary intervention. Myocardial infarction, heart failure, stroke and cancer were clinically validated. Osteoporosis was defined using femoral neck bone mineral density measured by Dual-energy X-ray absorptiometry applying World Health Organization (WHO) criteria [25]. Kidney disease was defined according to the National Kidney Foundation guidelines as having a glomerular filtration rate (GFR) <60 mL/min/1.73 m or as having markers of kidney damage (i.e. a urine albumin–creatinine ratio >17 mg/g in men and >25 mg/g in women) [26]. The GFR was calculated using the Modification of Diet in renal Disease Study Equation of Levy et al. [27] Anemia was defined according to the WHO guidelines <120 g/L for women and <130 g/L for men [28]. The comorbidity count which distinguishes between none, one and two or more comorbidities, was calculated for all participants of whom we had complete information on all ten diseases. Blood samples for determination of levels of serum glucose, creatinin, hemoglobin (Hb), cholesterol, and white blood cell (WBC) count were obtained at the research center.
Statistical analyses
For the baseline characteristics, logistic regression models, adjusted for age and sex, were performed. Cox proportional hazard ratios were calculated to evaluate the risk of mortality for frail elderly. The following variables were considered as potential confounders: age, sex, BMI, smoking status, pack-years and the comorbidity-index. Models were adjusted for co-variables that changed the point estimate by more than 5 %. Kaplan–Meier survival analysis was used to illustrate the percentage of participants who died during follow-up. The Log rank test was used to determine whether the difference in survival between frail elderly and intermediate and non-frail elderly was significant. Stratification for sex was performed and individual Kaplan–Meier curves were depicted. Proportionality of hazards was checked for the Cox-regression models. The influence of the use of age as time scale instead of the use of the standard survival analysis corrected for age, was evaluated using R Statistical Software (Foundation for Statistical Computing, Vienna, Austria). All other statistical analyses were performed using IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp, Armonk, NY). p values below the conventional level of significance (p < 0.05) were considered as statistically significant.
Results
Characteristics of the study population
Within the Rotterdam Study, the frailty status could be determined in 2,833 (71.6 %) of the 4,027 participants who recently visited the research centre. Of these, 1,585 participants (55.9 % of the study population) were women and the median age was 74 years (IQR 9). The prevalence of the individual frailty criteria was: (1) 1,113 (40.3 %) out of 2,765 participants had reduced grip strength, (2) 534 (19.4 %) out of 2,753 evaluated participants had ≥5 % weight loss over the past 6 years, (3) 61 (3.6 %) out of 1,688 participants exhibited a slow walking speed, (4) 118 (4.4 %) out of 2,695 participants had a low physical activity, and (5) 366 (13.0 %) out of 2,816 participants reported exhaustion (Fig. 1). No walking speed measurement was available in 1,145 (40.4 %) participants due to a postponed start period of the gait assessment. Three or more of the five frailty criteria were present in 163 participants, implicating that the prevalence of frailty in the Rotterdam Study is 5.8 % (95 % CI 5.0–6.7 %; 4.1 % in males, 7.1 % in females). 1,216 (42.9 %) and 1,454 (51.3 %) participants were non-frail and intermediate frail, respectively.
Frail participants were older and more frequently female compared to participants with less than three frailty criteria (Table 1). In addition, adjusted for age and sex, frail participants had a significantly impaired quality of life (QoL) and were more frequently current smokers with a higher number of pack-years.
Compared to the participants in whom the frailty status could be determined (n = 2,833), the participants with incomplete information (n = 1,194) were older and more frequently female, had a worse quality of life, higher mortality and more comorbidities (supplemental Table E1). In a sensitivity analysis using multiple imputation, the prevalence of frailty was not significantly higher in the participants with incomplete information (6.9 % compared to 5.8 % in the participants where the frailty status could be determined; p = 0.177).
Frailty and comorbidities
72.0 % of those who were frail had two or more comorbidities compared to 44.8 % of the non-frail participants (Table 1). Frail participants had a significantly higher prevalence of heart failure, hypertension, stroke, osteoporosis, COPD and anemia independent of age and sex than those who were non-frail and intermediate frail (Table 1). Furthermore, frail participants had lower blood levels of hemoglobin and cholesterol, whereas they had an increased white blood cell count, even when adjusted for age, sex, BMI, smoking status, pack years and the comorbidity count (p = 0.001, p = 0.003 and p = 0.040 respectively). There were no remarkable differences regarding BMI, blood glucose or creatinin levels.
Frailty and adverse health outcomes
More than one third of the frail participants had fallen in the preceding year and one quarter had been hospitalized in the previous year, compared to approximately one fifth and one tenth of the non-frail participants respectively (Table 1; Fig. 2). In Fig. 2a the percentage of participants who fell is depicted per frailty category; Fig. 2b shows the percentage of participants who were hospitalized.
During the more than 3 years of follow-up between March 2009 and January 2013 (average follow-up 805 days, SD 310 days), 118 (4.2 %) of the 2,831 participants with follow-up died. 26 (16.0 %) among the frail, 63 (4.3 %) among the intermediate frail and 29 (2.4 %) among the non-frail. Survival was significantly worse for frail elderly compared to the other two groups (Log rank p < 0.001; Fig. 3a). The Kaplan–Meier curves stratified by sex suggest a different survival pattern for men (immediate decline) compared to women (steady progressive decline) (Fig. 3b, c). When adjusting for age, sex and the comorbidity count in the Cox hazard proportion model, frail elderly had a more than threefold increased risk of mortality (HR 3.43, 95 % CI 1.85–6.36; p < 0.001, Table 2). Importantly, the addition of all enumerated potential confounders and the ten diseases of the comorbidity count to the model, did not change the independency of the frailty effect on mortality (p = 0.002). A trend towards an increased mortality risk could be noticed in the (male) pre-frail group (intermediate frail elderly); however, this was no longer significant after adjustment (Table 2). The use of age as time scale did not substantially influence the frailty point estimate (data not shown). Stratified by sex and adjusted for age and comorbidity, frail men had a 4.3 fold increased risk of mortality and frail women a 2.5 fold increased risk of mortality (Table 2). However, confidence intervals largely overlapped and the interaction term between frailty and sex was non-significant.
Discussion
Overall, we observed a prevalence of frailty of almost 6 percent within the Rotterdam Study. Compared to the non-frail, frail participants were more likely to be older and female. Frail elderly people had more falls and hospitalizations in the previous year and had an increased risk of mortality independent of age, sex and comorbidity.
Our observed frailty prevalence is in line with the 6.9 % prevalence estimate that Fried et al. [4] found in the Cardiovascular Health Study. In addition, a review by Collard et al. [2] reported an overall prevalence of frailty of 9.9 % in studies using physical frailty definitions. The results in our study confirm the consistency of the Fried frailty criteria. In the Cardiovascular Health Study, 68.0 % of the frail elderly had 2 comorbidities or more and 7.3 % had none of 9 co-morbidities [4]. Consistently, we found that 72.0 % of the frailty group had two or more, and 4.7 % had none of the co-morbidities, respectively. This indicates that frailty is not identical to comorbidity. It is more likely that these entities frequently co-exist, and that comorbidity only partly explains the presence of frailty [10].
Notably, the BMI did not differ significantly between frailty groups, which is similar to previous findings [11, 29]. Although frail people in our study had a significantly lower weight, they were also significantly shorter. As the BMI is a ratio, both parameters are important. Furthermore, not only weight loss, but also ‘sarcopenic obesity’ might be a risk factor of frailty [30]. Sarcopenia is a syndrome characterized by a progressive and generalized loss of skeletal muscle mass and muscle function (strength) with an increased risk of adverse health outcomes. ‘Sarcopenic obesity’ is the condition where lean body mass is lost, while fat mass may be preserved or even increased [31]. Thus not only loss of body weight, through loss of muscle tissue, but also intramuscular and visceral fat accumulation, are important for developing muscle weakness [31].
Interestingly, in our study we found an increased WBC count and low hemoglobin levels to be associated with frailty. Chaves et al. [32] found that the risk of being frail in community-dwelling older women progressively declined with increasing hemoglobin levels up to what is currently considered mid-normal levels (13.5 g/dL). In the Women’s Health and aging Study, higher WBC counts and IL-6 levels were independently associated with prevalent frailty [33]. Possibly, IL-6 contributes to unexplained anemia in elderly people by inhibiting erythropoietin production or by interaction with the erythropoietin receptor [34]. This supports the assumption of an association between frailty and a state of chronic systemic inflammation [3].
In the Rotterdam Study, frail elderly had an increased risk of death compared to non-frail participants, independent of age, sex and co-morbid disease. Fried and others have also found an increased risk of mortality in the frail group, although the mean follow-up period in these studies ranges from 3 to 9.7 years [4, 8, 11]. Puts et al. [6] stated that men appeared to die more suddenly, while women had a more steady progressive decline. Although our survival pattern for men compared to women seemed to confirm this statement, the mortality hazards were not significantly influenced by time in the Cox regression model. In our study, the short-term mortality risk was not significantly increased for the intermediate frail group independently of age, sex and comorbidity. Fried et al. [4] found that intermediately frail elderly were at an increased risk of becoming frail. This is in accordance with the concept that the frailty syndrome is a dynamic process, where transitions to states of greater frailty are more common, than transitions to states of lower frailty [35]. Thus, intermediate frailty could be considered as a state where the process of decline in multiple physiologic systems has already been set in motion, but reserves are still sufficient to withstand most stressors. This stage would therefore be suited for secondary prevention, including chronic disease management and geriatric assessment, fall prevention, exercise and nutritional modifications [12, 36]. Frailty, on the other hand, is often considered to be irreversible and tends to progress to an end-stage condition [4, 37]. This is shown in the study of Gill et al. [35] where, over a 54 months period, the probability of transition from being frail to non-frail was very low (rates 0–0.9 %). Moreover, in an interventional trial the benefit of the intervention (physical training) was observed only among the participants with moderate frailty, but not among those with more severe frailty. Note that in this trial moderately frail elderly were defined as having only one physical criterion, and the severe frail as having two [38].
The strengths of our study are the high quality and detail of medical information, the prospective mortality data collection, objective measurement of comorbidities and the general population-based setting of the Rotterdam Study. A potential limitation is that measurement of walking speed was only recently introduced. Because solely participants with at least three concordant positive or negative criteria were included in the study (e.g. the result of the missing gait assessment no longer mattered to conclude frailty), it is unlikely that this alone has caused misclassification of frail participants within the study. However, the percentage of intermediate frail participants within the study might have been underestimated. Second, falls and hospitalizations were assessed retrospectively. The recall of any fall in the previous year is relatively specific (91–95 %) but somewhat less sensitive (80–89 %) than intensive prospective data collection and individuals with poorer cognitive function may be less likely to recall falling (or hospitalization) in the previous 12 months [39]. Thirdly, weight loss was not self-reported but directly measured without asking whether any weight loss was intentional. Although we believe that the objective weight measurement is a strength, we cannot exclude the possibility that the actual prevalence might be lower due to intentional weight loss. In contrast, it is important to note that the true prevalence of frailty might be higher than measured if frail people do not feel fit enough to perform physical tests or complete questionnaires. The comparison of participants in whom the frailty status could be determined with those participants with incomplete information, seemed to point in the direction that the more vulnerable people are less able to perform the physical frailty tests. Consequently, the impact of frailty on mortality may be even larger if this phenomenon is limited to the most vulnerable frail people.
In conclusion, frailty is common in those participants of the Rotterdam Study able to perform the frailty tests, and more prevalent in females than males. Frail elderly are at an increased risk of dying within 3 years independent of comorbidity. We suggest that clinicians should focus on intermediate frail elderly to implement preventive measures.
Abbreviations
- BMI:
-
Body mass index
- CES-D:
-
Center for epidemiological studies depression
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- FEV1 :
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- Hb:
-
Hemoglobin
- HR:
-
Hazard ratio
- IQR:
-
Inter quartile range
- OR:
-
Odds ratio
- QoL:
-
Quality of life
- RS:
-
Rotterdam Study
- WBC:
-
White blood cells
References
Mitnitski AB, Graham JE, Mogilner AJ, et al. Frailty, fitness and late-life mortality in relation to chronological and biological age. BMC Geriatr. 2002;2:1.
Collard RM, Boter H, Schoevers RA, et al. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–92.
Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet. 2013;381(9868):752–62.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci. 2001;56(3):M146–56.
Rockwood K, Stadnyk K, MacKnight C, et al. A brief clinical instrument to classify frailty in elderly people. Lancet. 1999;353(9148):205–6.
Puts MT, Lips P, Deeg DJ. Sex differences in the risk of frailty for mortality independent of disability and chronic diseases. J Am Geriatr Soc. 2005;53(1):40–7.
Ensrud KE, Ewing SK, Cawthon PM, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009;57(3):492–8.
Ensrud KE, Ewing SK, Taylor BC, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med. 2008;168(4):382–9.
Bouillon K, Kivimaki M, Hamer M, et al. Measures of frailty in population-based studies: an overview. BMC Geriatr. 2013;13:64.
Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol Ser A Biol Sci Med Sci. 2004;59(3):255–63.
Cawthon PM, Marshall LM, Michael Y, et al. Frailty in older men: prevalence, progression, and relationship with mortality. J Am Geriatr Soc. 2007;55(8):1216–23.
Sternberg SA, Wershof Schwartz A, Karunananthan S, et al. The identification of frailty: a systematic literature review. J Am Geriatr Soc. 2011;59(11):2129–38.
Hofman A, van Duijn CM, Franco OH, et al. The Rotterdam Study: 2012 objectives and design update. Eur J Epidemiol. 2011;26(8):657–86.
Hofman A, Grobbee DE, de Jong PT, et al. Determinants of disease and disability in the elderly: the Rotterdam Elderly Study. Eur J Epidemiol. 1991;7(4):403–22.
Hofman A, Breteler MM, van Duijn CM, et al. The Rotterdam Study: objectives and design update. Eur J Epidemiol. 2007;22(11):819–29.
Hofman A, Breteler MMB, van Duijn CM, et al. The Rotterdam Study: 2010 objectives and design update. Eur J Epidemiol. 2009;24(9):553–72.
Ikram MA, van der Lugt A, Niessen WJ, et al. The Rotterdam Scan Study: design and update up to 2012. Eur J Epidemiol. 2011;26(10):811–24.
Hofman A, Darwish Murad S, van Duijn CM, et al. The Rotterdam Study: 2014 objectives and design update. Eur J Epidemiol. 2013;28(11):889–926.
de Vries NM, Staal JB, van Ravensberg CD, et al. Outcome instruments to measure frailty: a systematic review. Ageing Res Rev. 2011;10(1):104–14.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Taylor HL, Jacobs DR Jr, Schucker B, et al. A questionnaire for the assessment of leisure time physical activities. J Chronic Dis. 1978;31(12):741–55.
Executive summary: standards of medical care in diabetes–2013. Diabetes Care. 2013;36(Suppl 1):S4–S10.
Lahousse L, van den Bouwhuijsen Q, Loth DW, et al. Chronic obstructive pulmonary disease and lipid core carotid artery plaques in the Elderly: the Rotterdam Study. Am J Respir Crit Care Med. 2013;187(1):58–64.
European Society of Hypertension. European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21(6):1011–53.
WHO. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organization Technical Report Series. 1994;843:1–129.
Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–47.
Levey AS, Coresh J, Greene T, et al. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007;53(4):766–72.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System, Geneva. 2011.
Kiely DK, Cupples LA, Lipsitz LA. Validation and comparison of two frailty indexes: the MOBILIZE Boston Study. J Am Geriatr Soc. 2009;57(9):1532–9.
Morley JE, Haren MT, Rolland Y, et al. Frailty. Med Clin North Am. 2006;90(5):837–47.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39(4):412–23.
Chaves PH, Semba RD, Leng SX, et al. Impact of anemia and cardiovascular disease on frailty status of community-dwelling older women: the Women’s Health and Aging Studies I and II. J Gerontol A Biol Sci Med Sci. 2005;60(6):729–35.
Leng SX, Xue QL, Tian J, et al. Inflammation and frailty in older women. J Am Geriatr Soc. 2007;55(6):864–71.
Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annu Rev Med. 2000;51:245–70.
Gill TM, Gahbauer EA, Allore HG, et al. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006;166(4):418–23.
Hamerman D. Toward an understanding of frailty. Ann Intern Med. 1999;130(11):945–50.
Verdery RB. Failure to thrive in older people. J Am Geriatr Soc. 1996;44(4):465–6.
Gill TM, Baker DI, Gottschalk M, et al. A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med. 2002;347(14):1068–74.
Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc. 2005;53(12):2190–4.
Acknowledgments
The authors thank the study participants, the staff from the Rotterdam Study, J. Verkroost, F. van Rooij, M. Leening, R. Ruiter and the participating general practitioners. This study was supported by the Fund for Scientific Research Flanders (FWO) project G035014 N. The funding source had no involvement in the collection, analysis, writing, interpretation, nor in the decision to submit the paper for publication. Researchers were independent from funders for this work.
Conflict of interest
None of the authors has important conflicts of interest with relevance to the submitted work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Lies Lahousse and Bastiaan Maes have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lahousse, L., Maes, B., Ziere, G. et al. Adverse outcomes of frailty in the elderly: the Rotterdam Study. Eur J Epidemiol 29, 419–427 (2014). https://doi.org/10.1007/s10654-014-9924-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-014-9924-1