Abstract
The objective of this study is to conduct a meta-analysis of published and unpublished studies that examine the association between Agent Orange (AO) exposure and the risk of spina bifida. Relevant studies were identified through a computerized literature search of Medline and Embase from 1966 to 2008; a review of the reference list of retrieved articles and conference proceedings; and by contacting researchers for unpublished studies. Both fixed-effects and random-effects models were used to pool the results of individual studies. The Cochrane Q test and index of heterogeneity (I 2) were used to evaluate heterogeneity, and a funnel plot and Egger’s test were used to evaluate publication bias. Seven studies, including two Vietnamese and five non-Vietnamese studies, involving 330 cases and 134,884 non-cases were included in the meta-analysis. The overall relative risk (RR) for spina bifida associated with paternal exposure to AO was 2.02 (95% confidence interval [CI]: 1.48–2.74), with no statistical evidence of heterogeneity across studies. Non-Vietnamese studies showed a slightly higher summary RR (RR = 2.22; 95% CI: 1.38–3.56) than Vietnamese studies (RR = 1.92 95% CI: 1.29–2.86). When analyzed separately, the overall association was statistically significant for the three case–control studies (Summary Odds Ratio = 2.25, 95% CI: 1.31–3.86) and the cross sectional study (RR = 1.97, 95% CI: 1.31–2.96), but not for the three cohort studies (RR: 2.11; 95% CI: 0.78–5.73). Paternal exposure to AO appears to be associated with a statistically increased risk of spina bifida.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spina bifida is among the most common and serious congenital malformation of humans. Although spina bifida is compatible with life, 99% of affected persons are handicapped. The prevalence of spina bifida varies from 0.2 to 3 per 1,000 total births by region, period, race and ethnicity [1]. Both environmental and hereditary factors contribute to the liability of spina bifida [2]. Agent Orange (AO) during the US war in Vietnam has been suggested to cause spina bifida in the offspring of US soldiers who were exposed [3].
There are three major types of spina bifida. A mild form is called spina bifida occulta or hidden spina bifida which usually causes no disabilities. The other two include myelomeningocele and meningocele with the former being more severe and more common than the latter. The term spina bifida and myelomenigocele can be used interchangeably. Most babies (70–90%) with spina bifida either have hydrocephalus at birth or develop it soon after [4].
Agent Orange is composed of approximately equal proportions by weight of two defoliants: n-butyl esters of 2,4-dichlophenoacetic acid (2,4-D) and 2,4,5-trichlorophenoxyacetic acid (2,4,5-T). Dioxin is a synthetic contaminant of the 2,4,5-T. In animal studies, dioxin was found more toxic than the active ingredients of the herbicides used in Vietnam [3]. Specific concern about AO with its contaminant-dioxin and spina bifida was raised by Erickson et al. [5] in the early 1980s when the US Centre for Disease Control (CDC) birth defects study was re-analyzed using the Exposure Opportunity Index (EOI) based upon interview data. This study found that the risk of spina bifida was significantly associated with the estimated levels of AO exposure, while the association with other birth defects was insignificant. Furthermore, US Vietnam veterans in this study with a higher EOI were at greater risk of fathering a baby with spina bifida. Following this study, the CDC Vietnam experience study [6] and the Ranch Hand Study [7] also found an elevated risk for fathering spina bifida among US veterans who were exposed to AO. Based on these three studies, the US Institute of Medicine (IOM) reviewed biannually the health effects of AO and concluded that there is “suggestive” evidence that the risk of spina bifida is increased in the offspring of US soldiers who were exposed to AO during the US war in Vietnam [3].
In an attempt to address the potential link between AO and human birth defects, Ngo et al. (2006) performed a systematic review and meta-analysis pooling data from 22 studies (both published and unpublished) of US, Australian, and Vietnamese veterans, and sprayed civilians. This meta-analysis found that those exposed, or thought to be exposed to AO, were almost twice as likely to have a child with birth defects as were unexposed people. The authors, however, noted that a particular teratogen or mutagen may cause specific type(s) of defects; thus there is a possibility that since not all birth defects are related to AO exposure, the inclusion of all types of defects in an overall estimate of RR can result in dilution of RRs for those that are related. Moreover, the specific birth defects have been reported in the context of studies of congenital anomalies of all types, or a wide range of reproductive outcomes. Therefore, the studies lacked statistical power for the purpose of analyzing associations between Agent Orange and a particular category of birth defects. To address this shortcoming, the aim of this study was to undertake a meta-analysis to determine the association between paternal AO exposure and the risk of spina bifida in the offspring.
Spina bifida has been chosen because this birth defect has been consistently defined and frequently reported in studies of the association of AO with birth defects. Furthermore, the evidence concerning a potential link between AO exposure and spina bifida was primarily based on the IOM’s qualitative review of three published studies in the US [5, 7, 8] without an overall estimate of the association. This meta-analysis combines data from US, Australia, and Vietnam thus increasing statistical power which permits a more reliable estimate of risk over individual studies.
Methods
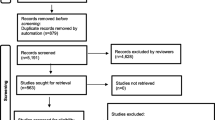
The methods, including data sources, eligible criteria for selecting studies, review procedure, and statistical methods are more fully described elsewhere [9]. We used multiple search strategies including: (1) a literature search of electronic databases (Medline from 1966 to Dec 2008) and Embase (1974 to Dec 2008) using the exploded terms: ‘AO’ and ‘Vietnam’ in conjunction with one of following terms: ‘birth defects’, ‘congenital malformations’, ‘congenital anomalies’, ‘adverse reproductive effects’, and ‘adverse developmental effects’, “spina bifida”, “neural tube defects”, and “meningomyelocoele”; (2) a review of relevant conference proceedings or published meeting abstracts, and relevant articles from the bibliography of all retrieved publications; (3) and by contacting researchers in the field and The National Committee for Investigation of the Consequences of the Chemical Used in the Vietnam War (the 10–80 Committee).
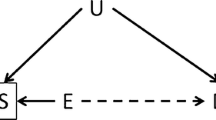
The screening of potentially eligible studies was undertaken through two sequential steps. First, studies of the association between AO and birth defects were located through reviewing the titles and abstracts, using the following inclusion criteria: (1) published and unpublished studies providing RR or OR on the association between AO exposure and birth defects or providing data that permit the calculation of these; (2) meta-analysis of the relevant studies; (3) international veteran studies that compared the incidence of birth defects among children of ex-service men involved in the Vietnam War with other ex-service man or general populations. Second, data on each specific category of birth defects including spina bifida were extracted, where available, and the numbers were entered into two by two tables. For the present meta-analysis, studies were included if they reported an OR or RR and 95% CI of an association between AO exposure and spina bifida, or data that allowed for calculation of these. When one group of a study has no event of spina bifida (i.e., containing a zero cell in the 2 × 2 table), 0.5 was added to each cell of the two by two table to estimate the RR [10].
Occupational and environmental studies of dioxin exposure and birth defects in other non-military situations were not considered. This is because these studies are limited by the fact that the exposures were minimal, the context of exposure varied greatly, the number of people exposed was small, and length of the time exposed was short, making the evidence far from conclusive. When a study had duplicate publications, only the most inclusive publication was used.
Each study was classified as a cohort study, case–control study, or cross-sectional study. Studies were further allocated into individual or aggregate studies according to the assessment of exposure assigned to groups, or measured in individuals. In addition, all studies that met eligibility criteria were assessed by the following characteristics: location of studies (Vietnam vs. other countries), the time when studies were carried out, levels of exposure, sample size and sampling methods, the source of exposure and outcome data, the types of parental exposure (mother, father or both), measurement and strength of association, and potential confounding and bias.
Pooling of data was performed using both fixed-and random-effects models [11, 12], weighting each study by a measure of its precision as the inverse of the estimated variance [13]. When there is no detectable heterogeneity, the two estimates coincide. In the results section, while random-effects estimates are reported as the primary analysis, fixed effects estimates are also provided for comparison.
Heterogeneity of effects across studies was assessed by the Cochran’s Q statistic [13] and was deemed significant when P < 0.05. In addition, the coefficient of inconsistency (I 2) as described by Higgins and Thompson [14] was also computed to assess the heterogeneity. I 2 is an estimate of the proportion of total variation in study estimates that is due to heterogeneity. To examine the possibility that publication bias may have affected the results, a funnel plot of the natural logarithm of OR or RR as the inverse of the variance of the studies was constructed, and the regression test for small study effects [15] was used for quantitative assessment of publication bias and funnel plot asymmetry. The data on ORs or RRs and 95% CI were entered into the STATA statistical package version 8.0 to perform these calculations. We used the META command to calculate a summary RR and 95% CI, and heterogeneity statistics, and the META-BIAS command to conduct the Egger test [10].
Results
Seven studies, involving 330 cases and 134,884 non-affected children were identified as eligible for the present meta-analysis (Tables 1, 2). No meta-analyses relevant to this topic were identified. Four studies were conducted in the US [5–7, 16], one in Australia [17], and two in northern Vietnam [18, 19]. Three non-Vietnamese studies were included in the IOM report, as noted earlier. Three studies [16, 18, 19] have not been published in any peer-reviewed journal. Although we did not restrict our inclusion criteria to studies with fathers exposed, none of the seven studies involved sprayed civilians (including men and women) or ex-service women, so only ex-service men were included in the present meta-analysis. Funnel plots revealed a symmetrical distribution with no evidence of publication bias (Egger’s test: intercept = 0.03; P = 0.96) (Fig. 1) for all studies, as well as for published studies only (Egger’s test: intercept = 1.00, P = 0.6).
There were three case–control studies with a total of 80 spina bifida cases, three retrospective cohort studies reporting on 12,875 infants or children of exposed fathers and 103,220 infants or children of unexposed fathers, and one cross-sectional study involving 213 children of exposed fathers and 210 children of unexposed fathers (Table 3). In the cohort study of US Ranch Hand veterans [7], four cases of spina bifida were recorded among Ranch Hand veterans, while none were observed among children of control veterans.
The pooled RR of seven studies was 2.02 (95% CI: 1.48–2.74) by both fixed-and random-effects models (Table 3; Fig. 2). The heterogeneity Q statistic is 5.30 (P = 0.51) and the coefficient of inconsistency (I 2) is 0.00, indicating no statistical evidence for heterogeneity. The overall association between AO exposure and spina bifida was statistically significant for the case–control studies (OR: 2.25, 95% CI: 1.31–3.86) and the cross sectional study (RR = 1.97, 95% CI: 1.31–2.96), but not for the cohort studies (RR: 2.11; 95% CI: 0.78–5.73), although the point estimate was similar. The magnitude of association was slightly higher in non-Vietnamese veterans (RR: 2.22, 95% CI: 1.38–3.56) than in North Vietnamese veterans (RR: 1.92; 95% CI: 1.29–2.86), although 95% CI overlapped.
It was noted that one Vietnamese study [19] differed methodologically from other studies. This particular study was cross-sectional and designed to specifically examine spina bifida occulta associated with paternal AO exposure. It provided more than two-thirds of the number of spina bifida cases and captured more than 50% of the total weight of effect (Fig. 2). When this study was removed from the meta-analysis the pooled RR increased slightly to 2.09, and remained statistically significant, with a corresponding confidence interval of (1.31–3.32). Thus, the overall risk estimate was not directionally affected by a single study with a methodological difference and which contributed the largest number of cases.
Discussion
Results of this meta-analysis combining data from seven studies show that paternal exposure to AO is associated with a twofold increase in the risk of spina bifida in their children. By pooling data from more than 100,000 population, with 330 cases of spina bifida, the present meta-analysis has stronger statistical power than individual studies to estimate the overall strength of the association with AO. There is no statistical evidence for heterogeneity across different studies suggesting that they measured the same underlying risk and that pooling the data is appropriate. Furthermore, there is no statistical evidence indicating a deficit of smaller negative studies minimizing the possibility of publication bias affecting the summary RR. By providing a quantitative estimation of risk, the results complement findings from a previous qualitative review by IOM that the risk of spina bifida, as a specific birth defect, appeared to be elevated with paternal AO exposure [3].
As noted in the previous meta-analysis [9], the inclusion of all types of defects in an overall estimate of RR can result in dilution of RRs for those that are related. However, the present meta-analysis found that the magnitude of the association between AO and spina bifida to be similar to that when all types of birth defects were considered (RR = 1.95; 95% CI: 1.59–2.39) [9]. Compared to the previous meta-analysis, none of the seven studies involved sprayed civilians, including exposed men and women who experienced a higher level of exposure [9]. The absence of a group with a higher level of exposure and maternal exposure in the present meta-analysis could explain the lack of increase in observed effects when the outcome is focused on spina bifida.
Studies of AO exposure and the risk of spina bifida have been criticized for their methodological limitations, including small sample size, possible exposure misclassification, limited validation of self-reported birth defects (for Vietnamese studies), differential ascertainment of cases, and lack of adjustment for confounding. Moreover, the studies in this review included a range of study designs, populations, methods of ascertainment of outcome, levels of exposure, and timing of exposure assessment. The homogeneity of observed associations, therefore, should be interpreted with caution. The consistency in findings across studies might be due to a shared bias or unmeasured confounding. However, we can think of no reason for a uniform bias or confounding to move OR/RR in all studies in the same direction. It is also of note that the two studies [7, 16] that measured individual serum dioxin concentration to determine exposure status produced higher risk estimates than the studies where exposure was assigned collectively or indirectly through EOI to war veterans. Given that studies without biological measures of exposure are subject to exposure misclassification because not all veterans who involved in the war were exposed to AO [3], this difference suggests that exposure misclassification may have diluted the effect of AO in the study as a whole.
Misclassification and under-ascertainment of birth defects were unlikely in non-Vietnamese studies that obtained birth defects from hospital records or birth defects registries, but may have occurred in the two Vietnamese studies where a registry was non-existent. The possibility of misclassification of spina bifida, however, was minimal because the two Vietnamese studies included live children where spina bifida was confirmed by physician examination and/or radiography. However, the largest Vietnamese study [18] reported only one case of spina bifida in the exposed (0.04 per 1,000 births) and 6 in the unexposed (0.06 per 1,000 births) which is lower than the prevalence of spina bifida in the general population, as noted earlier (i.e., 0.2–3 per 1,000 total births). This study, including only live children, may suffer from under-reporting bias as children with spina bifida are subject to excess mortality [1]. Differential under-reporting may result because exposed Vietnamese children with spina bifida are more likely to die unreported, or milder cases (e.g., closed without hydrocephalus) go undetected due to the poor access to health services during the post-war period where a diagnosis and treatment of spina bifida could have been made. If the differential in case ascertainment is great enough, it could alter the direction of the exposures estimated effect. Severe under-reporting could lead to the appearance of a protective effect for this group. Therefore, the lower summary RR from studies of Vietnamese veterans who experienced a higher level of exposure to AO [9] is unsurprising.
Confounding is a major threat to observational studies. Inadequate maternal intake of folic acid and diabetes mellitus type 1 in pregnant women are established risk factors for spina bifida. Furthermore, maternal overweight and obesity were found to increase the risk of spina bifida [20]. Low social economic class as measured by parental occupation (e.g., agricultural) and education, has been found to be associated with and increased risk for having an offspring with neural tube defects (NTD) in some studies [1]. In this meta-analysis, the possibility that confounding is responsible for the observed association is minimal for several reasons. Firstly, the findings are consistent across studies in different times, places, and exposed populations, by different investigators, with different research designs. Secondly, the studies were statistically homogenous, lending further credibility for the observed association. Thirdly, the lower elevated risk experienced by North Vietnamese veterans demonstrated that factors associated with the occurrence of spina bifida that were more likely to occur in Vietnam as the consequence of the war, such as poor parental nutritional status, maternal folate deficiency, or maternal infection and fever during pregnancy, was unlikely to explain the observed association. And finally, the statistically significant relative risk of more than two reduces the likelihood of significant confounding producing the result.
AO was one among multiple herbicides sprayed over South Vietnam during the war; others were picloram, and cacodylic acid [21]. Concerns have been raised about non-dioxin contaminants of herbicides, but far too little is known about their distribution and concentration in the formulations used in Vietnam to permit conclusions concerning their impact [21]. However, there is evidence that picloram causes male-mediated birth defects, including persistent histologic effects in testes of animals. High, maternally toxic doses of cacodylic acid are feototoxic and teratogenic in rats and mice [3]. Therefore, there is a possibility that the occurrence of spina bifida could be also attributed to exposure to other herbicides than AO.
The combination of studies with a range of quality in a meta-analysis has been a concern. Vietnamese studies appeared weak under some methodological criteria relative to the non-Vietnamese studies, such as exposure assessment based on ecological measure and lack of adjustment for confounding variables. As originally proposed by Glass [22, 23] and confirmed by our previous meta-analyses [9], the quality of the study does not appear to directionally affect the result. The risk estimate is statistically significant regardless of whether Vietnamese studies were included or excluded.
Although there were too few studies to perform sub-group meta-analysis according to the level of AO exposure, there is some indication of a dose–response relationship in the studies reviewed here. Among non-Vietnamese studies, the study of Ranch Hand veterans [7] who directly conducted AO spraying, produced a higher risk of spina bifida associated with paternal exposure to AO than studies of non-Ranch Hand veterans [5, 6, 16, 17]. Our observation is well supported by Erickson et al. [5] who reported that the estimated risks for spina bifida were higher for sub-groups of veterans with a greater AO Exposure Opportunity Index. Similarly, Knafl and Schwartz (2001) analyzed reproductive outcome data from the Air Force Health Study by [24] and found that spina bifida was among three malformations (anomalies of ear, face, and neck; spina bifida; and anencephaly) of 28 defect types examined for which adjusted estimated odds ratios increased with the increase in the observed serum dioxin levels [25].
The outcome under investigation is important for assessment of risk, given the heterogeneity in clinical presentation of spina bifida. Unfortunately, types of spina bifida or co-occurrence of spina bifida with other defects were not specified in all studies reviewed, except for the study by Hung et al. [19] that indicated to focus on spina bifida occulta. Furthermore, data on anencephaly—another common form of neural tube defect (NTD) was too limited to subject to statistical analyses, with 2 out of 5 non-Vietnamese studies reporting no anencephaly cases among the unexposed and a small number of cases in the exposed [6, 7]. Also, as infants born with anencephaly often die soon after birth, Vietnamese studies using parental self-report that was then verified by physician’s examination of live children for ascertainment of birth defect outcomes may not ascertain this type of NTD. The non-inclusion of anencephaly constitutes under-enumeration bias for NTD and would move the OR/RR towards 1, under-estimating the effect of Agent Orange.
Concerning the timing of exposure, most studies were carried out almost 10 years or longer after the time of exposure. Although 2 non-Vietnamese veteran studies [7, 16] measured serum dioxin levels to determine exposure status, they were collected and analyzed 10 or 20 years after the time of conception. Furthermore, when studies were arranged in the order of length of time since exposure, no consistent pattern of increase or decrease of RR or OR were found. For example, three studies of US and Australian veterans [5, 6, 17] that ascertained birth defects in three overlapping periods (i.e., 1965–1987; 1968–1980; 1966–1979) provided estimates of relative risk of 1.70 (95% CI: 0.6–5.0), 2.7 (95% CI: 1.2–6.2), and 1.04 (95% CI: 0.35–2.31), respectively. Thus, it is impossible to address the extent to which latency of follow-up after exposure affects the magnitude of the AO-spina bifida association.
The paternal-mediated mechanism in which dioxin can cause human birth defects is not fully established. It has been suggested that the lack of an established biological mechanism that explains the statistical association may reflect the gap in existing scientific knowledge and thus does not rule out a possible causal relationship between Agent Orange and spina bifida [26]. Furthermore, the detrimental effect of dioxin in causing congenital malformations has been documented in animal studies in which dioxin was shown to act as either a teratogen or mutagen [27–32]. In humans, paternal exposure to dioxin can impact on gene expression through activating the aryl hydrocarbon receptor (AHR)/aryl hydrocarbon receptor nuclear translocator (ARNT) complex in spermatogenesis, resulting in NTDs [33]. The wide and abundant distribution of AHR and ARNT in the human testis makes it amongst most sensitive organs to dioxin’s effects, and thus explains how dioxins can interfere directly with human spermatogenesis and fertility [34].
In summary, this meta-analysis provides more evidence to support the IOM’s conclusion concerning the potential link between paternal exposure to AO and the risk of spina bifida in the offspring. The data are consistent with six out of seven studies showing the same direction of risk. Despite the fact that Vietnamese studies were of low quality, the overall risk estimate were not directionally changed by the inclusion and exclusion of studies with methodological deficiencies. Consistent findings across studies suggest that the observed association is hard to explain by chance. Limitations of Vietnamese studies, coupled with limited knowledge concerning biological mechanisms that could explain the observed statistical association, provide justification for more biological and epidemiological studies to further elucidate the association between AO and spina bifida.
Future epidemiological studies should be conducted in heavily sprayed regions in Vietnam where dioxin concentrations in the environment remain high [35] with inclusion of biological measures of AO exposure to avoid exposure misclassification. Future studies also need to incorporate measures of folate intake to adjust for this potential confounder or effect modifier. Before a large and well-designed study can be conducted, support for children with spina bifida in AO affected populations, implementation of dioxin mitigation strategies and folate fortification for women at child bearing ages to prevent further occurrence of spina bifida in AO affected regions in Vietnam are urgently needed.
Abbreviations
- AO:
-
Agent Orange
- CDC:
-
Centers for disease control and prevention
- CI:
-
Confidence interval
- EOI:
-
Exposure opportunity index
- OR:
-
Odds ratio
- RR:
-
Relative risk
References
Mitchell LE, Adzick NS, Melchionne J, Pasquariello PS, Sutton LN, Whitehead AS. Spina bifida. Lancet. 2004;364:1885–95.
Northrup H, Volcik KA. Spina bifida and other neural tube defects. Curr Probl Pediatr. 2000;30:313–32.
Institute of Medicine. Veterans and Agent Orange—update. Washington DC: National Academy Press; 2003.
Barker E, Saulino M, Caristo AM. Spina bifida. RN. 2002;65:33–8.
Erickson JD, Mulinare J, McClain PW, et al. Vietnam veterans’ risks for fathering babies with birth defects. JAMA. 1984;252:903–12.
Centers for Disease Control. Health status of Vietnam veterans. III. Reproductive outcomes and child health. The Centers for Disease Control Vietnam Experience Study. JAMA. 1988;259:2715–9.
Wolfe WH, Michalek JE, Miner JC, et al. Paternal serum dioxin and reproductive outcomes among veterans of Operation Ranch Hand. Epidemiology. 1995;6:17–22.
Centers for Disease Control and Prevention. Vietnam veterans’ risks for fathering babies with birth defects. MMWR. 1984;33:457–9.
Ngo AD, Taylor R, Roberts CL, Nguyen TV. Association between Agent Orange and birth defects: systematic review and meta-analysis [see comment]. Int J Epidemiol. 2006;35:1220–30.
Stern J, Braburn MJ, Egger M, Smith GD, Altman DG. Meta-analysis in StataTM. In: Altman DG, editor. Systematic reviews in health care, meta-analysis in context. London: BMJ; 2001. p. 357.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1995;22:719–48.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control ClinTrials. 1986;7:177–88.
Pettiti D, editor. Meta analysis, decision analysis and cost effectiveness analysis. New York: Oxford University Press; 1999.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Egger M, Davey SG, Schneider M, Minder CE. Bias in metaanalysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
del Junco DJ, Sweeney AM, Papke O. Paternal blood dioxin, CYP1A1 and nural tube defects in children of Vietnam Veterans. Houston: Texas A & M Health Science Center; 2006.
Donovan JW, MacLennan R, Adena M. Vietnam service and the risk of congenital anomalies. A case-control study. Med J Aus. 1984;140:394–7.
Can N, Xiem NT, Hong TT, Tong NK, Duong DB. An epidemiological survey of pregnancies in the North of Vietnam. In: Proceedings of the first international conference of Agent Orange/dioxin. 1983. Hanoi.
Hung TM, Cuc PTK, Cau HD. Spina Bifida investigated by Spinal X-ray among children of veterans exposed to defoliant in the war in consequences of chemicals used in Vietnam war 1961–1971. Hanoi: 10–80 Committee; 2000. p. 50–9.
Stothard KJ, Tennant PW, Bell R, Rankin J. Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis. JAMA. 2009;301:636–50.
Institute of Medicine. Veterans and Agent Orange—update. Washington DC: National Academy Press; 2004.
Glass GV. Primary, secondary, and meta-analysis of research. Educ Res. 1976;5:3–8.
Glass CV. Integrating findings: the meta-analysis of research. Rev Res Educ. 1978;5:351–79.
Wolfe WH, Michalek JE, Miner JC, Rahe AJ. An epidemiologic investigation of health effects in air force personnel following exposure to herbicides. Armstrong: Epidemiology Research Division; 1992.
Knafl KJ, Schwartz, LS. Assessment of evidence for an impact of dioxin exposure on birth defects occurrence in offspring of Ranch Hand study participants. In: Third international conference of Agent Orange/dioxin. Hanoi; 2001.
Hatch MC, Stein ZA. Agent Orange and risks to reproduction: the limits of epidemiology. Teratog Carcinog Mutagen. 1987;7:423–4.
Theobald HM, Peterson RE. Developmental and reproductive toxicity of dioxins and other ah receptor agonists. In: Schecter A, editor. Dioxin and health. New York: Plenum Press; 1984. p. 319–32.
Giri AK. Mutagenic and genotoxic effects of 2, 3, 7, 8- tetrachlorodibenzo-p-dioxin, a review. Mutat Res. 1986;168:241–8.
Couture LA, Harris MW. Characterization of the peak period of sensitivity for the induction of hydronephrosis in C57BL/6N mice following exposure to 2, 3, 7, 8-tetrachlorodibenzo-p-dioxin. Fundam Appl Toxicol. 1990;15:142–50.
Nessel CS, Gallo MA, Lippmann M. Dioxins and related compounds. In: Lippmann M, editor. Environmental toxicants. New York: Van Nostrand Reinhold; 1992.
DeVito MJ, Birnbaum LS. Dioxins: model chemicals for assessing receptor-mediated toxicity. Toxicology. 1995;102:115–23.
Bryant PL, Reid LM, Schmid JE, Buckalew AR, Abbott BD. Effects of 2, 3, 7, 8-tetrachlorodibenzo-p-dioxin (TCDD) on fetal mouse urinary tract epithelium in vitro. Toxicology. 2001;162:34.
Hansen DA. Parental environment exposures and gene expression during spermatogenesis: research review to research framework. Birth Defects Res Part C. 2008;84:155–63.
Schultz R, Suominen J, Varre T. Expression of aryl hydrocarbon receptor and aryl hydrocarbon receptor nuclear transporter messenger ribonucleic acids and proteins in rat and human testis. Endocrinology. 2003;144:767–76.
Dwernychuk LW, Cau HD, Hatfield CT. Dioxin reservoirs in southern Viet Nam—a legacy of Agent Orange. Chemosphere. 2002;47:117–37.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ngo, A.D., Taylor, R. & Roberts, C.L. Paternal exposure to Agent Orange and spina bifida: a meta-analysis. Eur J Epidemiol 25, 37–44 (2010). https://doi.org/10.1007/s10654-009-9401-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-009-9401-4