Summary
Background Exon 19 deletion and L858R point mutation in exon 21 of the epidermal growth factor receptor (EGFR) are the most commonly encountered mutations in patients with non-small cell lung cancer (NSCLC) and predict better clinical outcomes following treatment with EGFR-tyrosine kinase inhibitors (TKIs). The inflammatory indicator neutrophil-to-lymphocyte ratio (NLR) in peripheral blood serves as a predictive factor for NSCLC patients treated with chemotherapy. Here, we aimed to evaluate the correlation between NLR and clinical efficacy of EGFR-TKIs in NSCLC patients harboring EGFR mutations. Methods We retrospectively collected information of 205 patients with advanced NSCLC harboring exon 19 deletion or L858R point mutation and receiving gefitinib or erlotinib. The clinical outcomes in the NSCLC patients were evaluated based on NLR level before EGFR-TKI therapy. Results The optimal cut-off value for NLR was 3.55. The response rates in the low-NLR and high-NLR groups were 69.2% and 51.5%, respectively. The median progression-free survival (PFS) in the low-NLR and high-NLR groups were 15.7 months and 6.7 months, respectively. The median overall survival (OS) in the low-NLR and high-NLR groups were 37.6 months and 19.2 months, respectively. The multivariate analysis identified performance status (PS), NLR, stage, and smoking status as independent predictors of PFS. Moreover, the PS and NLR were identified as independent predictors of OS. Conclusions NLR was a significant predictor of clinical efficacy and OS in NSCLC patients harboring EGFR mutations treated with gefitinib or erlotinib.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is amongst the major causes of cancer-related mortality, globally [1]. Non-small cell lung cancer (NSCLC) accounts for approximately 85% of all the lung cancer cases [2]. Targeted therapies are actively being developed for treatment of select patients with NSCLC. Tyrosine kinase inhibitors (TKIs), such as gefitinib and erlotinib, that target the epidermal growth factor receptor (EGFR), are small molecule drugs introduced in the clinics for the treatment of NSCLC patients. NSCLC patients with EGFR mutations who received TKI such as gefitinib, erlotinib, afatinib, and osimertinib had better progression free survival (PFS) and response rates than patients who received chemotherapy using cytotoxic drugs [3,4,5,6,7]. Based on these results, EGFR-TKI has become a standard treatment regimen for patients with advanced NSCLC harboring EGFR mutations. However, 20–30% of NSCLC cases show primary resistance to EGFR-TKIs, despite harboring an activating EGFR mutation [8]. Previously, we have reported the patient’s smoking status as an independent predictor of response and PFS upon treatment with EGFR-TKI therapy [9, 10]. However, other indicators that can elaborate on the response to EGFR-TKI therapy remain largely understudied.
Complete blood count (CBC) is one of the most common laboratory tests performed in the clinics. The absolute counts of neutrophils and lymphocytes reflect the inflammatory response and overall immune status of the patients. Previous studies showed that the peripheral blood prognostic inflammatory markers such as the neutrophil-to-lymphocyte ratio (NLR) associated with patient’s prognosis and treatment outcome [11,12,13,14]. However, there are a limited number of reports about the relationship between these inflammatory markers and the efficacy of EGFR-TKIs in advanced NSCLC patients with EGFR mutations.
Here, we conducted a clinical study to evaluate the potential of NLR obtained from CBCs of patients with advanced NSCLC harboring EGFR mutations in predicting the clinical efficacy of treatment with EGFR-TKIs.
Materials and methods
Patient selection and data collection
For the retrospective analysis, a total of 205 patients with advanced NSCLC who received EGFR-TKIs, including gefitinib and erlotinib, at the Kitasato University Hospital (Kanagawa, Japan) between March 2009 and June 2016, were enrolled. The date cut-off date was March 2019. Patients with histologically or cytologically confirmed NSCLC, stage IV disease, or postoperative recurrence (according to the criteria of the Union for International Cancer Control, version 7), and those not suitable for curative treatment, were assessed for patient selection. Consecutively, patients that met the following inclusion criteria were eligible for the study: (1) measurable target lesions observed in the chest X-ray, computed tomography of the chest and abdomen, or by other imaging modalities [magnetic resonance imaging (MRI) of the head, positron emission tomography (PET), or positron emission tomography/computed tomography (PET/CT)]; and (2) histologically confirmed NSCLC. Furthermore, the patients were categorized according to the smoking history as current smokers (including former smokers who are not categorized former light smokers), former light smokers (defined as patients who had stopped smoking at least 15 years previously, with a total of ≤10 pack-years of smoking), and never smokers (defined as patients who had smoked <100 cigarettes in their lifetime). The CBC was tested before the EGFR-TKI treatment, and NLR was calculated based on the absolute neutrophil and lymphocyte counts. The ethical review board committee of the Kitasato University and its affiliated hospitals approved the present study, which received ethical approval for the use of an opt-out style.
Response assessment
Tumor response was classified on the basis of the Response Evaluation Criteria for Solid Tumors, version 1.1. The disease stage prior to EGFR-TKI therapy and disease progression or recurrence were determined by physical examination, chest X-ray, CT of the chest and abdomen, or by other imaging modalities (e.g., MRI of the head and PET scan).
Statistical analyses
NLR was used to compare patient characteristics with response rates using the Chi-square test. PFS was measured from the date of commencing EGFR-TKI therapy till the date of disease progression, death, or last follow-up. OS was calculated from the date of commencing EGFR-TKI therapy till death from any cause. Survival curves were plotted using the Kaplan-Meier method. Log-rank test was used to assess differences between PFS and OS based on NLR for each patient. Variables (including gender, age, performance status [PS], NLR, EGFR genotype, smoking status, clinical stage prior to EGFR-TKI treatment [Stage IV vs. postoperative recurrence], the presence or absence of brain metastases, type of EGFR-TKI [gefitinib vs. erlotinib]) were entered into a Cox proportional hazards regression model to estimate the hazards ratios for PFS and OS. The receiver operating characteristic (ROC) curves and Youden’s index were utilized to determine the optimal cut-off for NLR. Results with P-values <0.05 were considered statistically significant. All statistical analyses were performed using SPSS software for Windows, version 23.0 (IBM Corp., Armonk, NY, USA).
The statistical significance of differences in the NLR according to the response to EGFR-TKI was determined by the Welch’s t test.
Results
Correlation of NLR with NSCLC patient characteristics
The clinical characteristics of the patients have been listed in Table 1. The patient cohort comprised of 60% women, with 70 years median age, and 65% of good PS. Ninety seven percent of the patients presented with lung adenocarcinoma (198 patients), while others were either pathology unspecified (3%). All patients were confirmed with stage IV disease or postoperative recurrence. The number of Stage IV patients and postoperative recurrences were 154 and 51 of the 205, respectively.
Cut-off values for immunologic parameters
We used PFS longer or shorter than 10 months as the binary variables for ROC curves [15]. Based on the highest Youden index (specificity+sensitivity–1), an optimal cut-off value of 3.55 was chosen for NLR, with an area under the curve (AUC) value of 0.67 [95% confidence interval (CI): 0.59–0.74, P < 0.0001] (Fig. 1). Furthermore, the comparative analysis for categorical variables suggested high NLR levels in stage IV than in recurrence group (P = 0.02, Table 1).
NLR predicts response to EGFR-TKI
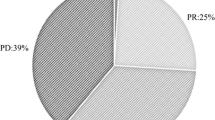
An objective response was achieved in 124 of the 205 patients, indicating a 60.5% overall response rate (95% CI: 53.8–67.2%, Table 2). Furthermore, a statistically significant difference (P = 0.009) was observed upon comparison between the low-NLR group (NLR < 3.55) with 69.2% response rate (95% CI: 60.3–78.1%) than the high-NLR group (NLR ≥3.55) with 51.5% rate (95% CI: 41.8–61.2%). In addition, the mean values of NLR in responders (patients with partial response) and non-responders (patients with stable disease or progressive disease) were 4.8 and 11.3 respectively, indicating a significant difference in the mean NLR between them (P = 0.021, Fig. 2).
Survival analysis of NSCLC patients
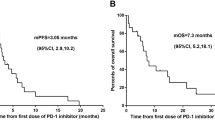
The patients presented with a median 25.2 months follow-up period for the survival analysis. The median PFS and OS of all the patients together were 10.8 months (95% CI: 8.8–12.8 months, Fig. 3a) and 28.0 months (95% CI: 23.5–32.5 months, Fig. 3b), respectively. The median PFS for the low-NLR and high-NLR group was 15.7 months (95% CI: 12.7–18.7 months) and 6.7 months (95% CI: 4.6–8.8 months, Fig. 4a), respectively (P < 0.0001). The median OS for the low-NLR and high-NLR group was 37.6 months (95% CI: 30.3–44.9 months) and 19.2 months (95% CI: 10.6–27.8 months), respectively (P < 0.001, Fig. 4b). The multivariate analyses commonly identified PS, NLR, smoking status, and stage as significant and independent predictors of PFS, as summarized in Table 3. Moreover, the PS and NLR were identified as independent predictors of OS based on the multivariate analyses (Table 4). Additionally, the never or former light smokers/low-NLR group and the smokers/high-NLR group had median PFS of 16.2 months (95% CI: 13.2–19.2 months) and 5.3 months (95% CI: 1.4–9.2 months), respectively (P = 0.0002, Fig. 5).
Discussion
EGFR-TKIs are primary treatment for the advanced stage NSCLC patients with EGFR mutations [3,4,5,6,7,8]. However, a significant percentage of NSCLC patients positive for EGFR mutations show resistance to EGFR-TKIs with short-term PFS. Previously, our study suggested that never-smokers and postoperative recurrence statuses serve as predictors for response to EGFR-TKIs, such as gefitinib and erlotinib, and PFS and OS in patients with NSCLC harboring activating EGFR mutations [9, 10]. Here, low NLRs at baseline were significantly associated with favorable tumor response and better PFS and OS in EGFR-mutant NSCLC patients treated with EGFR-TKIs than in patients with high NLRs. Moreover, our analysis, with a significantly larger patient cohort, is consistent with other studies investigating the correlation between NLR and efficacy of treatment with EGFR-TKI for NSCLC patients with EGFR mutations (Table 5) [15,16,17,18,19,20,21,22]. Furthermore, our NLR cut-off value of 3.55 is in the range reported by others (NLR 2.1–5.0) to predict the clinical efficacy for the treatment of NSCLC patients harboring TKI-sensitive EGFR mutations [15,16,17,18,19,20,21,22].
The utility of NLR as a predictive factor in cancer patients remains relatively understudied. Growing evidences indicate molecular and cellular pathways involving inflammation that contribute to proliferation, angiogenesis, and metastasis of neoplastic cells [23, 24]. Moreover, in patients with mesothelioma, NLR ≥5 correlated with elevated expression of Ki-67 and vascular endothelial growth factor, indicating increased tumor cell proliferation and sustained angiogenesis, than in patients with NLR <5 [25]. Furthermore, the circulating neutrophils release diverse inflammatory cytokines, including tumor necrosis factor-α and interleukin-6, leading to cancer progression [26].
The tumor microenvironment (TME) is involved in tumorigenesis and malignant progression and has a major impact on both the therapeutic response of the tumor and therapeutic effectiveness [27, 28]. Tumor-infiltrating lymphocytes (TILs) are important components of the TME that regulate inflammatory responses and play a pivotal role in eradicating tumor cells [29]. In TME, a significant increase in TIL (CD-8+ T-cells) and decrease in regulatory T-cells have been observed upon administration of EGFR-TKI in a lung cancer mouse model harboring EGFR mutation [30]. Thus, it may be reasonable to argue that treatment with EGFR-TKI is more effective in NSCLC patients positive for EGFR mutations with low NLR than in those with high NLR.
Next, our analysis suggests that NLR can be correlated with the PFS of NSCLC patients, where never or former light smokers showed better survival than the smokers. Furthermore, a combination of pretreatment NLR and smoking status served well as predictors of response to EGFR-TKI. Taken together, the analysis suggests that EGFR-mutant NSCLC patients with high NLR and smoking history show poor survival outcomes when treated only with EGFR-TKI, indicating the necessity of an alternative or combined chemotherapy to provide better response and survival outcome in the patients.
However, our study has certain limitations. First, being a retrospective study, the result cannot be regarded as definitive. Second, we could not exclude the involvement of other conditions, such as infections suffered by patients at the time of blood collection or the administration of steroidal medications that may affect the blood count. Third, we have not studied the correlation between NLR and TME. Fourth, the study does not include patients treated osimertinib as the primary treatment.
In conclusion, our study presents NLR as a significant predictor of clinical efficacy (response and PFS) and OS in NSCLC patients positive for EGFR-mutations and treated with EGFR-TKI including gefitinib and erlotinib. Whether NLR predicts outcome similarly with osimertinib treatment, along with gefitinib and erlotinib, in NSCLC patient’s positive for EGFR-mutations remains to be validated as an immediate follow up to this study.
References
Fitzmaurice C, Allen C, Global Burden of Disease Cancer Collaboration et al (2017) Global, regional, and National Cancer Incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 Cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 3:524–548
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, Cooper D, Gansler T, Lerro C, Fedewa S, Lin C, Leach C, Cannady RS, Cho H, Scoppa S, Hachey M, Kirch R, Jemal A, Ward E (2012) Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin 62:220–241
Bria E, Milella M, Cuppone F, Novello S, Ceribelli A, Vaccaro V, Sperduti I, Gelibter A, Scagliotti GV, Cognetti F, Giannarelli D (2011) Outcome of advanced NSCLC patients harboring sensitizing EGFR mutations randomized to EGFR tyrosine kinase inhibitors or chemotherapy as first-line treatment: a meta analysis. Ann Oncol 22:2277–2285
Petrelli F, Borgonovo K, Cabiddu M, Barni S (2012) Efficacy of EGFR tyrosine kinase inhibitors in patients with EGFR-mutated non–small-cell lung cancer: a meta-analysis of 13 randomized trials. Clin Lung Cancer 13:107–114
Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304:1497–1500
Miyawaki M, Naoki K, Yoda S, Nakayama S, Satomi R, Sato T, Ikemura S, Ohgino K, Ishioka K, Arai D, Namkoong H, Otsuka K, Miyazaki M, Tani T, Kuroda A, Nishino M, Yasuda H, Kawada I, Koh H, Nakamura M, Terashima T, Sakamaki F, Sayama K, Betsuyaku T, Soejima K (2017) Erlotinib as second- or third-line treatment in elderly patients with advanced non-small cell lung cancer: Keio Lung Oncology Group Study 001 (KLOG001). Mol Clin Oncol 6:409–414
Ramalingam SS, Vansteenkiste J, Planchard D, Cho BC, Gray JE, Ohe Y, Zhou C, Reungwetwattana T, Cheng Y, Chewaskulyong B, Shah R, Cobo M, Lee KH, Cheema P, Tiseo M, John T, Lin MC, Imamura F, Kurata T, Todd A, Hodge R, Saggese M, Rukazenkov Y, Soria JC, FLAURA Investigators (2020) Overall survival with Osimertinib in untreated, EGFR-mutated advanced NSCLC. N Engl J Med 382:41–50
Wang J, Wang B, Chu H, Yao Y (2016) Intrinsic resistance to EGFR tyrosine kinase inhibitors in advanced non-small-cell lung cancer with activating EGFR mutations. Onco Targets Ther 9:3711–3726
Igawa S, Sasaki J, Otani S, Ishihara M, Takakura A, Katagiri M, Masuda N (2015) Impact of smoking history on the efficacy of gefitinib in patients with non-small cell lung Cancer harboring activating epidermal growth factor receptor mutations. Oncology 89:275–280
Nishinarita N, Igawa S, Kasajima M, Kusuhara S, Harada S, Okuma Y, Sugita K, Ozawa T, Fukui T, Mitsufuji H, Yokoba M, Katagiri M, Kubota M, Sasaki J, Naoki K (2018) Smoking history as a predictor of epidermal growth factor receptor tyrosine kinase inhibitors in patients with non-small cell lung Cancer harboring EGFR mutations. Oncology 95:109–115
Hirahara N, Matsubara T, Mizota Y, Ishibashi S, Tajima Y (2016) Prognostic value of preoperative inflammatory response biomarkers in patients with esophageal cancer who undergo a curative thoracoscopic esophagectomy. BMC Surg 16:66
Kang KH, Efird JT, Sharma N, Yang M, Dowlati A, Linden P, Machtay M, Biswas T (2017) Prognostic potential of neutrophil-to-lymphocyte ratio and lymphocyte nadir in stage III non-small-cell lung cancer. Future Oncol 13:1405–1414
Guo D, Han A, Jing W, Chen D, Jin F, Li M, Kong L, Yu J (2018) Preoperative to postoperative change in neutrophil-to-lymphocyte ratio predict survival in colorectal cancer patients. Future Oncol 14:1187–1196
Fukui T, Okuma Y, Nakahara Y et al (2019) Activity of nivolumab and utility of neutrophil-to-lymphocyte ratio as a predictive biomarker for advanced non-small-cell lung cancer: a prospective observational study. Clin Lung Cancer 20(3):208–214.e2
Zhang Y, Feng YC, Zhu HG, Xiong TC, Hou YS, Song J, Jiang W, Zhu CJ (2018) The peripheral blood neutrophil-to-lymphocyte ratio is a prognostic predictor for survival of EGFR-mutant nonsmall cell lung cancer patients treated with EGFR-TKIs. Medicine (Baltimore) 97:e11648. https://doi.org/10.1097/MD.0000000000011648
Lin GN, Peng JW, Liu PP, Liu DY, Xiao JJ, Chen XQ (2017) Elevated neutrophil-to-lymphocyte ratio predicts poor outcome in patients with advanced non-small-cell lung cancer receiving first-line gefitinib or erlotinib treatment. Asia Pac J Clin Oncol 13:e189–e194
Meriggi F, Codignola C, Beretta GD, Ceresoli GL, Caprioli A, Scartozzi M, Fraccon AP, Prochilo T, Ogliosi C, Zaniboni A (2017) Significance of neutrophil-to-lymphocyte ratio in Western advanced EGFR-mutated non-small cell lung cancer receiving a targeted therapy. Tumori 103:443–448
Ding PN, Roberts TL, Chua W, Becker TM, Descallar J, Yip PY, Bray V (2017) Clinical outcomes in patients with advanced epidermal growth factor receptor-mutated non-small-cell lung cancer in South Western Sydney local Health District. Intern Med J 47:1405–1411
Minami S, Ogata Y, Ihara S, Yamamoto S, Komuta K (2017) Neutrophil-to-lymphocyte ratio predicts overall survival of advanced non-small cell lung cancer harboring mutant epidermal growth factor receptor. World J Oncol 8:180–187
Phan TT, Ho TT, Nguyen HT, Nguyen HT, Tran TB, Nguyen ST (2018) The prognostic impact of neutrophil to lymphocyte ratio in advanced non-small cell lung cancer patients treated with EGFR TKI. Int J Gen Med 11:423–430
Aguiar-Bujanda D, Dueñas-Comino A, Saura-Grau S et al (2018) Neutrophil to lymphocyte ratio as a prognostic factor in European patients with epidermal growth factor receptor-mutant non-small cell lung cancer treated with tyrosine kinase inhibitors. Oncol Res Treat 41:755–760
Deng C, Zhang N, Wang Y, Jiang S, Lu M, Huang Y, Ma J, Hu C, Hou T (2019) High systemic immune-inflammation index predicts poor prognosis in advanced lung adenocarcinoma patients treated with EGFR-TKIs. Medicine (Baltimore) 98:e16875. https://doi.org/10.1097/MD.0000000000016875
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 30:1073–1081
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454:436–444
Pinato DJ, Mauri FA, Ramakrishnan R, Wahab L, Lloyd T, Sharma R (2012) Inflammation-based prognostic indices in malignant pleural mesothelioma. J Thorac Oncol 7:587–594
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Klemm F, Joyce JA (2015) Microenvironmental regulation of therapeutic response in cancer. Trends Cell Biol 25:198–213
Aerts JG, Hegmans JP (2013) Tumor-specific cytotoxic T cells are crucial for efficacy of immunomodulatory antibodies in patients with lung cancer. Cancer Res 73:2381–2388
Sharma P, Allison JP (2015) The future of immune checkpoint therapy. Science 348:56–61
Jia Y, Li X, Jiang T, Zhao S, Zhao C, Zhang L, Liu X, Shi J, Qiao M, Luo J, Liu S, Han R, Su C, Ren S, Zhou C (2019) EGFR-targeted therapy alters the tumor microenvironment in EGFR-driven lung tumors: implications for combination therapies. Int J Cancer 145:1432–1444
Acknowledgements
We would like to thank the patients and their families for the participation. We also thank the staff members of the Department of Respiratory Medicine, Kitasato University School of Medicine, for their suggestions and assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ono, T., Igawa, S., Kurahayashi, S. et al. Impact of neutrophil-to-lymphocyte ratio in patients with EGFR-mutant NSCLC treated with tyrosine kinase inhibitors. Invest New Drugs 38, 885–893 (2020). https://doi.org/10.1007/s10637-020-00919-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-020-00919-0