Summary
The continual increase in mortality rates and number of cancer cases is a matter of serious concern in developing countries. The incorporation of natural products into classical cancer treatment approaches is a promising direction. The mechanisms of A549 and HeLa cancer cell death induction by ethanolic extracts of propolis samples from Phayao, Chiang Mai, and Nan provinces in northern Thailand were investigated in this study. The propolis extract from Chiang Mai showed the highest antioxidant activity and the greatest total phenolic content. The propolis extract from Nan also exhibited the highest total flavonoid content. The proliferation of A549 and HeLa cells grown in the presence of the propolis extracts was suppressed in a dose- and time-dependent manner. Moreover, treatment of both cancer cells with the propolis extracts showed DNA fragmentation and significantly increased the number of the apoptotic cells. On A549 cells, the extrinsic and intrinsic pathways of caspase enzymes were activated by the propolis extracts from Phayao and Chiang Mai. In the case of the propolis extract from Nan, the mechanisms involved apoptosis on the A549 cells were caspase-independent pathway. The extrinsic pathway of the caspase enzyme was triggered by all of the propolis extracts on HeLa cells. Finally, oral administration of the propolis granule produced from the propolis extract from Nan resulted in extended survival of tumour-bearing mice. Therefore, propolis extracts from the northern region of Thailand demonstrated pharmacological properties, both antioxidant and anticancer activities. From these findings, it is evident that propolis extracts can be considered as a naturally obtained agent extremely useful in cancer treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is among the diseases that are widely found in developing countries. Radiotherapy and chemotherapy are normally used to treat cancer. However, these treatments often have severe side effects on patients such as damage to skin and intestinal epithelium and suppression of the immune system. The finding of natural substances which have an effect on an apoptotic induction, and an inhibition of cyclin-dependent kinase, telomerase, and poly (ADP-ribose) polymerase or PARP, has been studied [1]. Apoptosis, or programmed cell death, is subject to clearance of abnormal cells without the inflammatory response [2]. Several proteins are associated with the apoptosis mechanism, including members of the caspase and Bcl-2 families [3]. Caspase enzymes are grouped according to their function. The caspase-3, 6, 7, 8 and 9 are involved in apoptosis and the caspase-1, 4, 5 and 12 are also involved in inflammation [4]. The caspase enzyme is generally present as an inactive zymogen. After activation, the zymogen or procaspase is cleaved into two small and two large subunits with two active sites per molecule [3]. Members of the Bcl-2 protein family are important molecules that can confer induction or inhibition of apoptosis. The Bcl-2 proteins are classified into two groups (anti-apoptotic and pro-apoptotic) according to their function [5]. The apoptosis pathway is divided into extrinsic and intrinsic pathways. In the extrinsic pathway, the tumour necrosis factor (TNF) is bound to the TNF receptor. The intracellular domain of TNF recruits the adaptor protein and forms complexes to initiate the activation of procaspase-8. The intrinsic pathway cytochrome C and other proteins are released from the damaged mitochondria and activate caspase-9. The active caspase-8 and caspase-9 also activate procaspase-3, which results in cell death by the cleavage of cellular protein and DNA [6].
Propolis is the resinous substance obtained from bees. It is generally used as a sealant for unwanted open spaces in the hive and as a protective substance against parasites and microbes [7]. It is composed of several chemical compositions which have pharmacological properties including antioxidant property, antimicrobial activity, anticancer activity, and immunostimulant activity [8]. Studies on the biological activity of propolis are of interest for developing novel pharmaceutical products for use as alternative medicine in the treatment of cancer. Many studies have reported on the efficacy of propolis to inhibit the growth of many types of cancer cells [9–11]. Two main bioactive compounds, cardanol and cardol, which were identified in propolis from Nan, Thailand exerted antiproliferation and cytotoxicity among duet carcinoma (BT474), undifferentiated lung (Chaco), liver hepatoblastoma (Hep-G2), gastric carcinoma (KATO-III) and colon adenocarcinoma (SW620) cancers. However, other potent compound or the synergistic interaction of the propolis compound might involve in the antiproliferative and cytotoxic properties [12]. Moreover, the anticancer activity of propolis obtained from Northern Thailand, including its molecular mechanism on the suppression of cancer cells has not been reported. Therefore, propolis was collected from different sources in Northern Thailand and the biological properties of 70 % ethanolic extracts of propolis (EEP) that dissolved in dimethyl sulfoxide (DMSO) were investigated for their antioxidant activity and some mechanisms of cancer cell growth inhibition.
Materials and methods
Propolis extraction
Propolis samples from the northern region of Thailand were obtained from bee keepers in Phayao, Chiang Mai, and Nan provinces. All propolis samples were extracted using the modified method [13]. One hundred grams of the propolis samples was cut into small pieces and frozen at −80 °C overnight. The propolis was then blended and macerated with 70 % ethanol for 72 hours in the dark. The suspension was filtered through Whatman filter No.1. The filtrate was frozen for the removal of the wax. Then, the ethanol was removed and the filtrate was made into a concentrate in a rotary evaporator. After evaporation, the filtrate was lyophilized to obtain the propolis extract. The ethanolic extract of propolis (EEP) was dissolved in dimethyl sulfoxide (DMSO) before use for the study.
Determination of antioxidant activity
The antioxidant activity of the EEP was evaluated using the 2,2-diphenyl-1-picrylhydrazyl (DPPH) method. The EEP was mixed with 0.1 mM DPPH (Sigma-Aldrich, MO, USA). The absorbance of solution was measured at a wavelength of 517 nm after 20 minutes of incubation at room temperature. The antioxidant activity was calculated and compared to Gallic acid (Sigma-Aldrich, MO, USA) which was considered as the antioxidant standard. The antioxidant activity of the propolis extract is represented as milligram Gallic acid equivalent per gram extract (mg GAE/g extract) [14].
Determination of total phenolic compounds
The total phenolic content of the EEP was determined by Folin–Ciocalteu assay. The EEP was mixed with 50 % Folin–Ciocalteu reagent (Merck, NY, USA) for 5 minutes. 5 % Sodium carbonate, was added, and it was further incubated for 1 hour. The absorbance of the reaction was measured at wavelength 725 nm. The total phenolic compound content was calculated from the Gallic acid standard curve. The total phenolic content of the propolis extract was presented as milligram Gallic acid equivalent per gram extract (mg GAE/g extract) [14].
Determination of total flavonoid compounds
The total flavonoid content of the EEP was determined. The EEP was mixed with 10 % aluminium chloride and 1 M potassium acetate. After incubation at room temperature for 30 minutes, the absorbance of the reaction was measured at a wavelength of 415 nm. The total flavonoid content was calculated from the Quercetin (Merck, NY, USA) standard curve. The total flavonoid content of the propolis extract was presented as milligram Quercetin equivalent per gram of extract (mg QAE/g extract) [14].
Cultivation of cancer cells
Human lung adenocarcinoma epithelial cell line (A549) was kindly provided by Dr. Khanittha Punturee of The Division of Clinical Chemistry, Department of Medical Technology, Faculty of Associated Medical Sciences, Chiang Mai University. Human cervical adenocarcinoma cell line (HeLa) was kindly provided by Prof. Dr. André M. Lieber, University of Washington, Seattle, Washington, USA. A549 and HeLa cells were cultured in Dulbecco’s Modified Eagle Medium (DMEM) (Gibco, CA, USA) supplemented with 10 % heat-inactivated fetal bovine serum (Hyclone, UK), penicillin (100 units/mL), and streptomycin (100 μg/mL) (Gibco, CA, USA) at 37 °C in a 5 % CO2 incubator. Prior to the experiment, the cells were harvested using 0.05 % trypsin-EDTA (Gibco, CA, USA) solution and washed with sterile PBS. The cells were then resuspended, stained with trypan blue exclusion test and counted with a haemocytometer to adjust to a desired cell number.
Detection of cytotoxic effect of EEP on cancer cells using MTT assay
The antiproliferative activity of the propolis extract was determined using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay [15]. Briefly, the cells (5 × 103 cells) were seeded on a 96-well tissue culture plate (Corning Incorporated, NY, USA) at 37 °C in a humidified atmosphere of 5 % CO2. The cells were allowed to adhere for 24 hours, and the EEP was added to the cells. DMSO, 0.6 % was also used as a vehicle control. The cells were maintained in a humidified atmosphere of 5 % CO2 at 37 °C for 24, 48, and 72 hours. Subsequently, MTT solution (2 mg/mL), 15 μL (Bio Basic INC., Canada), was added. Finally, the blue formazan crystal was dissolved with 200 μL of DMSO. Absorbance values at wavelengths of 540 nm and 630 nm were measured. The percentage of cell proliferation was calculated by comparing it to that of the cell control.
Detection of DNA fragmentation of cancer cells after treatment with EEP
DNA fragmentation of the cancer cells was observed after incubation with the EEP. Cancer cells (1 × 106 cells) were seeded on a 24-well tissue culture plate at 37 °C in a humidified atmosphere of 5 % CO2 for 24 hours. Then, the cells were washed with sterile PBS and treated with the EEP at 37 °C in a humidified atmosphere of 5 % CO2 for 48 hours. DMSO, 0.6 % was also used as a vehicle control. The cells were extracted with a lysis solution containing 10 mM Tris pH 7.4, 100 mM NaCl, 25 mM EDTA, 1 % SDS, and 10 mg/mL proteinase K solution (AMRESCO, OH, USA), and further incubated at 45 °C for 90 minutes. Next, RNaseA (10 mg/mL) (AMRESCO, OH, USA), 2 μL, was added, and the cells were placed at room temperature for 60 minutes. The fragmented DNA was obtained and separated on 2 % agarose gel in a 0.5X TBE buffer [16]. The gel was photographed under gel documentation (Syngene, MD, USA).
Determination of procaspase-3, procaspase-9, and Bcl-2 protein expressions in cancer cells after treatment with EEP using SDS-PAGE and Western blotting
Cancer cells (1 × 106 cells) were placed on a 6-well tissue culture plate and allowed to attach at 37 °C in a humidified atmosphere of 5 % CO2 incubator overnight. The cells were treated with the EEP for 48 hours. DMSO, 0.6 % was used as a vehicle control. Then, the apoptotic proteins of the treated cells were extracted using a RIPA buffer with 1X of protease inhibitor cocktail (Roche, Switzerland). The protein concentration was measured using the Bio-Rad Protein Assay Dye Reagent Concentrate (Bio-Rad, CA, USA). Sixty micrograms of protein were loaded on 4–20 % of the Mini-PROTEAN TGX™ Precast Gels (Bio-Rad, CA, USA). The separated protein on the polyacrylamide gel was transferred into the nitrocellulose membrane by Western blotting. The membrane was probed with anti-procaspase-3, anti-procaspase-9, and anti-Bcl-2 (Bio Legend, CA, USA), overnight. The membrane was then probed with anti-mouse conjugated with horseradish peroxidase. After 1 hour of incubation, 1 mL of a detection reagent, Amersham ECL Prime Western Blotting Detection Reagent (GE Healthcare Life Sciences, PA, USA), was added on the membrane and incubated at room temperature for 3–5 minutes before exposure to an X-ray film.
Determination of apoptosis induction by EEP on cancer cells using flow cytometer
The cancer cells (5 × 104 cells) were seeded on a 24-well tissue culture plate and incubated in a humidified atmosphere of 5 % CO2 at 37 °C for 24 hours. The EEP was then added to the cells and the cells were maintained in a humidified atmosphere of 5 % CO2 at 37 °C for 48 hours. After incubation, the cells were harvested and stained with AnnexinV-FITC and 7-amino-actinomycin D (7-ADD) according to the manufacturer’s instruction (Bio Legend, CA, USA). The stained cells were counted and grouped using a flow cytometer (Becton Dickinson, NJ, USA). The apoptotic index of the cells was calculated as follows [17].
The caspase enzymes were studied using 25 μM of a pan-caspase inhibitor (z-VAD-fmk), caspase-3 inhibitor (z-DEVD-fmk), caspase-8 inhibitor (z-IETD-fmk), and caspase-9 inhibitor (z-LEHD-fmk) [18, 19]. After seeding the cells, the cells were pre-incubated with these caspase inhibitors in a humidified atmosphere of 5 % CO2 at 37 °C for 2 hours, and the cells were consequently treated with the EEP for 48 hours. The treated cells were stained with AnnexinV-FITC and 7-ADD, and the apoptotic indices were calculated.
Determination of orally administered propolis granules on tumor growth
The propolis granules were produced from the EEP. Twenty-five milligrams of EEP was mixed with lactose as a binder. The mixture was ground and dried at 50 °C overnight for reduction of the moisture. The dried propolis granules were obtained. The tumour suppression activity of propolis granules was determined on tumour bearing mice. All procedures about animal testing were performed according to the Institutional Animal Care and Use Committee (IACUC), Office of Animal Welfare, University of Washington (Approved protocol No. 3108-01). This approved protocol covered all procedure such as the animal care, route of exposure and euthanasia method throughout the experiments. The local allowance of animal use was also authorized according to the Animal Ethics Committees, Department of Biology, Faculty of Science, Chiang Mai University (Approved protocol No. 001/14).
The female CB-17 SCID mice were maintained under specific pathogen free (SPF) controlled humidity and temperature. The HeLa cells (5 × 105 cells) were selected to resuspend in matrigel coating in DMEM (Becton Dickinson, NJ, USA) and were injected subcutaneously on the right mammary fat pad once. After the tumour volume reached 100–200 mm3, the control and treatment mice were orally fed sterile PBS and the propolis granule at 24 mg/mouse every other day until the tumour volume reached the cut-off (1 × 103 mm3). The tumour size was measured by caliper every other day and the tumour volume was calculated using the formula: length x (width)2 [20]. When the tumour volume reached the cut-off (1 × 103 mm3), the mice were sacrificed and the tumour nodules were collected. Histopathological study by haematoxylin & eosin (H&E) and TUNEL staining were performed [21].
Statistical analysis
All the experiments were performed as three independent experiments. All the data is represented as mean ± SD. The independent sample t-test and the ANOVA analysis were used to analyse and compare between the treatment group and the control group. A Kaplan-Meier survival fraction was used to compare the percentage of survival mice between the treatment and control groups.
Results
Physical appearance of the propolis samples
All the northern Thai propolis samples were dark brown in colour and sticky. The solution after extraction was light to dark yellow, and the sticky extracts were observed to be light to dark brown after evaporation and lyophilization. The percentage yields of the propolis extracts were calculated from the weight of the dried extract × 100 and divided by the weight of the original propolis sample. The results showed that the percentage yields of the propolis extracts from the Phayao, Chiang Mai, and Nan provinces were 18.08, 11.46, and 22.64, respectively.
Antioxidant activity, total phenolic and flavonoid compound content of the EEP
The antioxidant activity of the EEP demonstrated that the EEP from Chiang Mai had the highest antioxidant activity, at 7.98 ± 0.63 mg GAE/g extract, and a total phenolic compound content of 34.82 ± 1.55 mg GAE/g extract, compared to the EEP from other sources. However, the EEP from Nan showed the highest total flavonoid compound content of 25.05 ± 2.57 mg QAE/g extract. The results are shown in Table 1.
Cytotoxicity of the EEP on A549 and HeLa cells
In order to assess the cytotoxicity of the EEP on cancer cells, proliferation of A549 and HeLa cells was continuously observed after treatment with various concentrations of the EEP for 24, 48, and 72 hours. Proliferation of the A549 and HeLa cells was suppressed by the EEP in a dose-dependent and time-dependent manner. The A549 cell viability in the presence of the EEP from Phayao ranged from 1.10 ± 0.93 to 138.45 ± 8.44 %. The A549 cell viability after treatment with the EEP from Chiang Mai was between 0.74 ± 0.33 and 134.44 ± 7.84 %. After the treatment of the cells with the EEP from Nan, the cell viability was in the range of 0.42 ± 0.08 to 108.13 ± 9.36 %. HeLa cell viability in the presence of the EEP from Phayao ranged from 0.79 ± 0.44 to 90.62 ± 3.34 %. After the treatment of the HeLa cells with the EEP from Chiang Mai and Nan, the cell viability was found to range from 0.92 ± 0.53 to 110.94 ± 2.65 % and from 0.35 ± 0.25 to 91.55 ± 1.18 %, respectively (Fig. 1). The 50 % inhibitory concentration (IC50) of the EEP was calculated for comparing the toxicities of the EEP from different sources after treatment on both the cancer cells.
The cytotoxicity of the EEP on A549 and HeLa cells after treatment with the EEP. The cells were treated with EEP for 24 hours, 48 hours, and 72 hours. Control and vehicle control cells were also treated with DMEM and 0.6 % DMSO, respectively. The cell viability was measured using the MTT assay and calculated to compare with the control cells. The data is expressed as mean ± SD. a The EEP from Phayao, b The EEP from Chiang Mai, and c The EEP from Nan
On the A549 cells, the lowest IC50 value of the EEP was observed after the treatment of the cells with the EEP from Nan for 72 hours (Table 2). However, the highest IC50 value of the EEP was also found on the incubation of the cells with the EEP from Chiang Mai for 24 hours. Similar, consistent results were found in the case of HeLa cells as well. Upon taking into consideration the IC50 values obtained in the two cancer cells, the IC50 values of all of the EEP on HeLa cells were lower than the IC50 values of all of the propolis extracts on the A549 cells. Thus, it can be concluded that i) the EEP from Nan is the most potent propolis in suppressing cancer cells proliferation and ii) HeLa cells are more sensitive to all of the EEP than A549 cells.
Alteration in cancer cell morphology after treatment with the EEP
To study cancer cell morphology after incubation with the EEP, both the cancer cells were cultured in the presence of various concentrations of the EEP and evaluated under an inverted microscope. In the presence of the EEP, there was a change from adherent and epithelial cells to round and small cells. Eighty percent of the cells floated in the medium which is indicative of dead cells after treatment with the highest concentration of the EEP (Fig. 2).
Morphology of the A549 and HeLa cells after incubation with the EEP from different sources for 48 hours. The cell morphology was observed and photographed under an inverted microscope at a final magnifying power of × 100. a Control, b vehicle control, c-f the EEP from Phayao at concentrations of 0.03125 mg/ml, 0.0625 mg/ml, 0.125 mg/ml, and 0.25 mg/ml, g-j the EEP from Chiang Mai at concentrations of 0.0625 mg/ml, 0.125 mg/ml, 0.25 mg/ml, and 0.5 mg/ml, and k-n the EEP from Nan at concentrations of 0.03125 mg/ml, 0.0625 mg/ml, 0.125 mg/ml, and 0.25 mg/ml
Induction of DNA fragmentation in cancer cells by the EEP
Detection of DNA fragmentation which is indicative of the late apoptosis in the A549 and HeLa cancer cell lines after treatment with the EEP from different sources are shown in Fig. 3. A549 cells were treated with the EEP from Phayao at concentrations of 0.125 mg/mL and 0.25 mg/mL, the EEP from Chiang Mai at a concentration of 0.5 mg/mL, and the EEP from Nan at concentrations of 0.125 mg/mL and 0.25 mg/mL for 48 hours; this treatment induced visible DNA fragmentation, compared to the control and the vehicle control. For HeLa cells, the EEP from Phayao at concentrations of 0.125 mg/mL and 0.25 mg/mL, the EEP from Chiang Mai at concentrations of 0.25 mg/mL and 0.5 mg/mL, and the EEP from Nan at concentrations of 0.125 mg/mL and 0.25 mg/mL induced DNA fragmentation (Fig. 3).
Expression of apoptotic proteins after treatment of cancer cells with the EEP
To investigate the apoptotic protein expression in the cancer cells after treatment with the EEP, the apoptotic proteins procaspase-3, procaspase-9, and Bcl-2 were chosen for the study. The EEP from Phayao and Nan at a concentration of 0.125 mg/mL and from Chiang Mai at a concentration of 0.25 mg/mL were used to investigate this effect. Incubation of A549 cells with the EEP from Nan showed the lowest procaspase-3 level, followed by the EEP from Chiang Mai. The procaspase-9 level was found to have reduced in the A549 cells with the EEP from both Phayao and Chiang Mai. However, evidence for the same was not found in the case of A549 cells which were treated with the EEP from Nan. At the same time, none of EEP was observed to suppress Bcl-2 protein in A549 cells. Incubation of HeLa cells with all of the EEP demonstrated complete reduction in the procaspase-3 level. However, the EEP was not found to suppress the procaspase-9 and the Bcl-2 protein in HeLa cells (Fig. 4).
Induction of apoptosis in cancer cells by the EEP
To evaluate the mechanism of the EEP induced cell death, cells were detected by staining them with two fluorescent dyes (AnnexinV-FITC and 7-ADD) after treatment with the EEP for 48 hours. The stained cells were counted using a flow cytometer and grouped into viable cells, early and late apoptotic cells, as well as necrotic cells according to the fluorescent staining pattern. The viable cells were not stained with both fluorescent dyes. The early apoptotic cells were merely stained with annexinV-FITC. The late apoptotic cells were also stained with both fluorescent dyes. In addition, the necrotic cells were merely stained with 7-ADD.
The results demonstrated that the EEP could induce early and late apoptotic cell death in a dose-dependent manner. In A549 cells, control and the vehicle control cells showed 2.58 ± 0.28 % and 3.05 ± 0.16 % of early apoptotic cells, respectively. The percentages of late apoptotic cells of the control and the vehicle control were 2.11 ± 0.09 % and 2.86 ± 0.34 %, respectively. After the treatment with the EEP, a dose-dependent increase in the early and the late apoptotic cells was found on both cancer cell lines that were incubated with the EEP. In the A549 cells, the highest percentage of the early and late apoptotic cells was clearly found on the cells which were incubated with the EEP from Phayao at a concentration of 0.125 mg/mL by 41.25 ± 0.07 % and 27.00 ± 1.27 %, respectively. After exposure of A549 cells treated with the EEP from Chiang Mai at concentration of 0.25 mg/mL, the highest percentages of the early and the late apoptotic cells were observed by 20.55 ± 1.62 and 18.00 ± 0.57 %, respectively. In addition, the highest percentages of the early and the late apoptotic cells were 46.6 ± 0.71 and 20.7 ± 0.28 %, respectively in the presence of the cells with the EEP from Nan at a concentration of 0.125 mg/mL (Fig. 5). Similarly, the control and the vehicle control of the HeLa cells showed the percentages of early apoptosis to be 14.30 ± 1.98 % and 14.60 ± 1.70 %, respectively. The percentages of the late apoptotic cells of the control and the vehicle control were 5.20 ± 0.75 % and 5.09 ± 0.35 %, respectively. The highest percentage of the early apoptotic cells was found in the presence of the EEP from Phayao at a concentration of 0.0625 mg/mL by 37.8 ± 2.97 %. After the incubation of the HeLa cells with the EEP from Chiang Mai at a concentration of 0.25 mg/ml, the highest percentage of the early and late apoptotic cells was also observed by 36.85 ± 1.78 and 18.35 ± 2.76 %, respectively. Additionally, the HeLa cells that were incubated with the EEP from Nan at a concentration of 0.125 mg/mL showed the highest percentages of the early and the late apoptotic cells to be in the value of 32.3 ± 1.98 and 41.6 ± 7.92 %, respectively (Fig. 5).
The apoptosis induction on the A549 and HeLa cells after treatment with the EEP for 48 hours. The treated cells were stained with Annexin V-FITC and 7-ADD. The stained cells were grouped and counted using a flow cytometer. The data is presented as mean ± SD. The observations with; a The EEP from Phayao, b The EEP from Chiang Mai, and c The EEP from Nan
The apoptotic rate on the A549 and the HeLa cancer cells after treatment with the EEP was determined by the apoptotic index (AI) [17]. The AI was calculated to compare the rate of apoptotic cell induction on the control and the EEP-treated cells. The AI was calculated from the proportion of annexinV-stained apoptotic cells, in the total cell population in the sample. The AI of the A549 cells which were treated with the EEP was observed to have increased in a dose-dependent manner. Significant increase in the AI was observed after the treatment of the cells with the EEP from Phayao at concentrations of 0.0625 mg/mL and 0.125 mg/mL with AI of 0.0686 ± 0.0057 and 0.6827 ± 0.0118, respectively. Moreover, a significant increase in the AI was found on the cells treated with the EEP from Chiang Mai at concentration of 0.25 mg/ml when compared to 0.6 % DMSO treated cells (vehicle control), at an AI of 0.1192 ± 0.0052. A significant increase in the AI was also found after the treatment of the cells with the EEP from Nan at a concentration of 0.125 mg/mL, at an AI of 0.4755 ± 0.0333 (Fig. 6).
The apoptotic index of the A549 and HeLa cells after incubation with the EEP for 48 hours. The cells were harvested for fluorescent staining. After analyzing using a flow cytometer, the apoptotic index was calculated and expressed as mean ± SD. *Statistically significance between in AI of EEP-treated cells compared to control cells (p ≤ 0.05)
With regard to HeLa cells, the AI of the HeLa cells which were treated with the EEP was observed to have increased in a dose-dependent manner. A significant increase in the AI was observed after the treatment of cells with the EEP from Phayao at concentrations of 0.0625 mg/mL and 0.125 mg/mL with AI of 0.6331 ± 0.0161 and 0.5307 ± 0.0046, respectively. Treatment with the EEP from Chiang Mai at a concentration of 0.25 mg/mL produced a significant increase in the AI, by 0.5522 ± 0.0103. Additionally, a significant increase in the AI was observed after the treatment of the cells with the EEP from Nan at concentrations of 0.0625 mg/mL and 0.125 mg/mL with AI of 0.4717 ± 0.0095 and 0.7394 ± 0.0595, respectively (Fig. 6).
Based on a comparison of the potencies to induce apoptosis on both cancer cells, the concentration of 0.125 mg/mL of the EEP from different sources was considered. Incubation of the A549 cells with the EEP from Phayao showed the highest potency to induce apoptosis, with the AI of 0.6827 ± 0.0118. In addition, the EEP from Nan also showed the highest potency to induce apoptosis on HeLa cells, with the AI of 0.7394 ± 0.0595. However, the EEP from Chiang Mai showed the lowest potency to induce apoptosis on both cancer cells (Fig. 6). From these results, it is evident that the EEP from Phayao and Nan showed the highest potency to induce apoptotic cell death on A549 and HeLa cells. In contrast, the EEP from Chiang Mai showed the lowest potency to induce apoptosis. These results were consistent with the cytotoxicity of EEP on both cancer cells.
The EEP-induced apoptosis through activation of caspase enzyme
To investigate whether caspase enzymes were implicated in cancer cell apoptosis in the presence of propolis, an irreversible pan-caspase inhibitor (z-VAD-fmk) was used to inhibit the apoptosis. Pre-treatment the A549 cells using z-VAD-fmk showed significant decreases in an AI, by 0.0491 ± 0.008 and 0.0574 ± 0.0020, in cells treated with EEP from Phayao and Chiang Mai compared to the cells that were treated with EEP only. In contrast, the AI of the cells after incubation with or without z-VAD-fmk and the EEP from Nan were not found to be different. A significant reduction in the AI was observed upon pre-incubation of the HeLa cells with z-VAD-fmk and the EEP from all sources, when compared to the treatment with EEP only (Fig. 7a). Therefore, it can be inferred that the EEP triggered the apoptotic cell death in both the A549 and the HeLa cancer cells through the caspase enzyme, except in the case of the EEP from Nan. We conclude that the EEP from Nan might induce apoptosis in A549 cells via a caspase-independent pathway.
The apoptotic index of the A549 and HeLa cells, which were pre-incubated with; a 25 μM of z-VAD-fmk, and b 25 μM each of z-DEVD-fmk (caspase-3 inhibitor), z-IETD-fmk (caspase-8 inhibitor) and z-LEHD-fmk (caspase-9 inhibitor) for 2 hours following treatment with the EEP from different sources for 48 hours. #Statistically significance between AI of EEP-treated cells compared to control cells (p ≤ 0.05). *Statistically significance between in AI of the cells that were treated with the caspase inhibitor and EEP compared to the treatment with EEP only (p ≤ 0.05)
To assess which members of caspase enzymes were involved in the apoptosis induction by EEP, specific inhibitors for specific caspases were used. Cancer cells were pre-incubated with 25 μM each of z-DEVD-fmk (caspase-3 inhibitor), z-IETD-fmk (caspase-8 inhibitor) and z-LEHD-fmk (caspase-9 inhibitor). The AI of the A549 cells pre-incubated in the presence of caspase-3, caspase-8, and caspase-9 inhibitors and subsequently treated with the EEP from Phayao were 0.0612 ± 0.0006, 0.0430 ± 0.0030, and 0.0535 ± 0.0001, respectively. The AI of the A549 cells when pre-incubated with the caspase-8 or the caspase-9 inhibitor, and the EEP from Phayao, were found to be significantly lower than the AI of the cells that were treated with the EEP from Phayao only. Interestingly, a statistically significant reduction in an AI of the A549 cells after treatment with the EEP from Chiang Mai was observed when the cells were pre-treated with the caspase-3, caspase-8, and caspase-9 inhibitors, with an AI of 0.0567 ± 0.0005, 0.0699 ± 0.0003, and 0.0592 ± 0.0030, respectively. However, no statistic reduction was observed in an AI on treatment with the EEP from Nan (Fig. 7b). The results from the evaluation of the caspase enzymes on the HeLa cells demonstrated that an AI of the HeLa cells in the presence of the EEP from Phayao with the caspase-3 and the caspase-8 inhibitors were 0.1099 ± 0.0047 and 0.1061 ± 0.0034, respectively. There was a significant decrease in these AI, compared to the EEP-treated cell control. Similarly, a significant reduction in an AI of the HeLa cells was observed after treatment with the EEP from Chiang Mai on pre-treatment of the cells with caspase-8 inhibitors compared to the EEP-treated cell control. Pre-incubation of the HeLa cells with the EEP from Nan and the caspase-3 inhibitor (AI = 0.1784 ± 0.0008) or the caspase-8 inhibitor (AI = 0.1031 ± 0.0136) was found to have caused significant reduction in the apoptotic index, compared to the EEP-treated cell control (Fig. 7b). From these results, it is evident that EEP-induced apoptosis was mostly mediated through caspase activation. The EEP from Phayao and Chiang Mai caused apoptosis through both extrinsic and intrinsic pathways. In the case of the EEP from Nan, the mechanisms involved on apoptosis in the A549 cells were caspase-independent pathway, while, the caspase-dependent apoptosis in extrinsic pathway was found in the HeLa cells.
Improvement of survival time on tumour-bearing mice by propolis granule
According to cytotoxicity test of EEP on cancer cells, the EEP from Nan province, Thailand showed the most potent activity to suppress cancer cells proliferation. Moreover, HeLa cells were sensitive to the EEP more than A549 cells. Therefore, the effect of propolis granules produced from propolis extract from Nan province on the survival time of tumour-bearing mice that were subcutaneously injected with the HeLa cells was determined. The result found that the percentage of survival mice after treatment with the propolis granules was significantly higher than control mice. After euthanizing the treated mice, the tumour nodules of mice were stained with H&E and TUNEL assay. The tumour tissues contained many of the cancer cells which were stained with H&E. Although, the TUNEL positive cells on tumour tissue in propolis-treated mice were not found. The result is shown on Fig. 8.
The percentage of survival mice, which were treated with propolis granule (blue line) at 24 mg/mouse every other day by oral gavage was analyzed by Kaplan-Meier survival fraction. The tumor volume was measured and the percentage of survival mice was calculated. The tumor sections of mice in control, propolis granule, and positive control (H2O2) were stained with H&E and TUNEL
Discussion
The mechanism of Thai propolis of suppressing A549 and HeLa cancer cells was evaluated for the very first time in this study. After extraction, it was observed that the EEP from Nan showed the highest percentage of yield, followed by the EEP from Phayao and that from Chiang Mai. The harvesting season and the bee species might have had an influence on the extraction yield of the propolis extract [22, 23]. Moreover, the use of different solvents to extract the propolis also affected the percentage yield after extraction. The aqueous extract of propolis showed a percentage yield that was lower than that of the ethanolic extract. This is because the polarity index of water is higher than that of ethanol. The more polar solvents such as water merely liberate only the polar compounds in propolis. In contrast, solvents with intermediate polarity such as ethanol liberate both polar and non-polar compounds in propolis [24]. In addition, flavonoids which are found in propolis in abundance are readily extracted by solvents like alcoholic solutions [25].
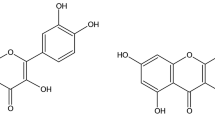
We demonstrated that the EEP from Chiang Mai exhibited the highest antioxidant activity and total phenolic compound content. The EEP from Nan showed the highest total flavonoid compound content. Previously consistent results reported that the highest DPPH and reducing power activity was found in propolis from Chiang Mai, followed by propolis from Chiang Rai, Lamphun, and Nan. Propolis from Chiang Mai showed different amounts of eight major compounds. Chrysin was predominated in this propolis followed by galangin, quercetin, kaempferol, rutin, myricetin, apigenin and pinocembrine. In contrast, two major compounds such as kaemferol and galangin were present in propolis from Nan [26]. Propolis from Nan has also been reported to contain the highest amount of flavonoid compounds, for example rubin, quercetin, and naringenin, which also exerted antioxidant activity [27]. In addition, other reports discovered that the propolis from Chiang Mai composed of new phenyl allyl flavanone ((7″S)-8-[1-(4′-hydroxy-3′-methoxyphenyl)prop-2-en-1-yl]-(2S)- pinocembrin (1), (E)-cinnamyl-(E)-cinnamylidenate) and other compounds belonging to flavonoids and phenolic ester such as (E)-cinnamyl-(E)-p-methoxycinnamate, phenethyl caffeate, (2S)-pinocembrin and chrysin [28]. A sugars and sugar derivatives, triterpenes and phenolic lipids in high amounts were detected in propolis from the northern region of Thailand (Chiang Rai, Lamphun, Nan, Phayao and Phrae). Nevertheless, the highest amounts of the triterpenes compound were found in propolis from Nan. The most active compound in Phayao propolis was found to be several triterpenes and phenolic acid (cardols, cardanols, and anacardic acids). These compounds in Phayao propolis may be originated from Mangifera indica [29].
In our study, cancer cell growth was suppressed by the EEP in a dose- and time-dependent manner. A comparison of the IC50 values of the EEP with regard to suppressing cancer cell growth showed that the EEP from Nan had the highest toxicity on both A549 and HeLa cells. However, the EEP from Chiang Mai showed the lowest toxicity on both the cancer cell lines. Additionally, all of the EEP showed toxicity and sensitivity more to HeLa cells than to A549 cells. According to a previous report, they demonstrated the toxicity of chrysin, which was isolated from Chiang Mai propolis, on TRAIL-resistant HeLa cells that was higher than the toxicity on A549 cells [30]. Moreover, we found that the EEP from Nan showed the highest total flavonoid compound content and gave the highest cytotoxicity on both cancer cells. Several researches have demonstrated that toxicity on cancer cells is positively correlated with the presence of flavonoid compounds such as quercetin, caffeic acid, and clerodane diterpenoid [31]. Previous reports demonstrated the toxicity of flavonoid, the main constituent in propolis, depended on its structure. The increasing of the hydroxyl group might decrease the cytotoxicity of flavonoid in colorectal carcinoma cells [32].
Our experiment illustrated that both A549 and HeLa cancer cells, after treatment with the EEP at concentrations that induce late apoptosis, respond strongly with DNA fragmentation within those cells. This was because the DNA cleavage process occurred after the activation of the caspase cascade and the cell death. Similarly, it has been reported that the ethanolic extract of propolis from Turkey was able to induce the phenotype of apoptosis in the breast cancer cell line by increasing the number of TUNEL positive cells [33]. Incubation of both A549 and HeLa cells with EEP resulted in an increase in the number of the apoptotic cells in a dose-dependent manner. The EEP from Phayao had the highest potency to induce apoptosis on the A549 cells. In contrast, the EEP from Nan had the highest potency to trigger apoptosis on the HeLa cells. The potency of propolis for inducing apoptosis may be associated with the antioxidant activity. The lower antioxidant activity was found in the EEP from Phayao and Nan and resulted in an increase of intracellular oxidative stress. Furthermore, the production of reactive oxygen species from the reaction between intracellular transition ion and flavonoid compound also triggered apoptosis [34–36]. Activation of caspase enzymes played an important role in apoptosis. We confirmed that the caspase enzymes were implicated in the cancer cell apoptosis by the EEP. A significant decrease was observed from an AI upon the treatment of both A549 and HeLa cells with all of the EEP. Previous studies have shown that co-incubation of nymphaeol-A and z-VAD-fmk showed complete inhibition of nymphaeol-A-induced apoptosis [37]. Additionally, co-treatment between chrysin and z-VAD-fmk demonstrated that the activation of caspase enzymes, especially caspase-8 and caspase-3, was inhibited [38].
Moreover, our data indicated that the induction of apoptosis in A549 cells by EEP from Nan involved caspase-independent pathways because there was no evidence of a decrease in an AI after pre-treatment with z-VAD-fmk. Proteins such as apoptosis-inducing factor (AIF) and endonuclease G (EndoG) might also have been involved in the caspase-independent pathway. The AIF is a flavin adenine dinucleotide-containing protein, and it activates chromatin condensation and large-scale DNA degradation [39]. Furthermore, the EndoG, was released from the damaged mitochondria and translocated to the nucleus. It cooperates with exonucleases and DNase to generate internucleosomal DNA fragments [40].
These investigations indicated that caspase-3, caspase-8, and caspase-9 were implicated with the apoptosis-induction of the EEP. The distinct activation of the caspase enzyme might have resulted from the chemical constitution of the EEP. Flavonoid is found to be the dominant compound in propolis and it has been reported to be involved in apoptosis induction which ultimately affects cellular response [41]. Treatment of human colon cancer cells using cinnamic acid derivatives found in propolis induces apoptosis through both extrinsic and intrinsic pathways by the up-regulation of active caspase-8, caspase-9, and FADD [42]. Whilst, HeLa cells apoptosis through both extrinsic and intrinsic pathways was activated by genistein, it found that the genistein-induced apoptosis on HeLa cells was blocked in the presence of z-VAD-fmk, z-IETD-fmk, z-DEVD-fmk and z-LEHD-fmk [43].
The expressions of procaspase-3, procaspase-9, and Bcl-2 on EEP-treated cells were investigated. A reduction of procaspase-3 and procaspase-9 levels was found in propolis-treated A549 cells, while a reduction of procaspase-3 level was observed in propolis-treated HeLa cells only. However, the EEP from Nan had a procaspase-9 level similar to those of the control. This is in accordance with the findings in the case of the A549 cells, where the cells did not show any significant reduction in the number of apoptotic cells after the incubation of the cells with this EEP and the pan-caspase inhibitor. However, the procaspase-3 expression on the A549 cells treated with the EEP from Nan was partially suppressed because the AIF was an alternative molecule used to activate caspase-3 and EndoG without the activation of caspase-9 or cytochrome c [44]. A decrease in the levels of procaspase-8, Bid, and procaspase-3 were found after treatment of the human melanoma cells with Taiwanese propolis [11, 45]. Similarly, the ethanolic extract of propolis from Turkey could induce the phenotype of apoptosis in breast cancer cell lines by increasing the caspase-6, caspase-8, and caspase-9 activities [33]. According to previous finding, cardanol, that was isolated from dichloromethane extract of propolis from Nan, Thailand, showed the induction of cell cycle arrest and apoptosis in BT-474 cells. The G/S phase in cell cycle was arrested by the up-regulation of the cell cycle gene p21 through ERK, JNK and p38 phosphorylations. In addition, the up-regulation of apoptotic genes such as the DR5 and Bcl-2 genes in extrinsic and intrinsic pathways of the apoptosis process was also found in these cells [46].
Therefore, the cancer cell apoptosis was induced after incubation cancer cells with all of the EEPs. The EEP from Nan showed the highest toxicity on HeLa cells when compared to other sources. Likewise, HeLa cells were more sensitive to this EEP than A549 cells. Consequently, the propolis granules produced from the EEP of Nan were evaluated on the suppression of HeLa cell proliferation in tumour-bearing mice. We demonstrated that the extended lifespan of mice that were given propolis granule, was significant. Other studies demonstrated the consistent results on the extended survival time of mice after administration with propolis or its components [21, 47]. Moreover, the combination between propolis and chemotherapy significantly reduced tumor progression and side effects induced by the chemotherapeutic agents alone [48–50].
Conclusion
This current study demonstrated that propolis from Northern region of Thailand exhibited the biological activities of antioxidant activity and anticancer activity. The mechanism of propolis inducing cancer cell apoptosis was involved in caspase-dependent and –independent pathway depending on its source and cell lines (Fig. 9). On A549 cells, the extrinsic and intrinsic pathways of caspase enzymes were activated by the propolis extracts from Phayao and Chiang Mai. In contrast, the A549 cells that were incubated with propolis from Nan involved caspase-independent pathway. The extrinsic pathway of caspase enzyme was only triggered by all of propolis extracts on HeLa cells. All of these finding suggested that propolis should be developed as a natural supplementary product or combined with synthetic chemotherapy drugs for use in treatment as an alternative medicine to suppress cancer cells.
References
Sonnenschein C, Soto AM (2013) The aging of the 2000 and 2011 Hallmarks of Cancer reviews: a critique. J Biosci 38:651–663. doi:10.1038/nature12213
Elmore S (2007) Apoptosis: a review of programmed cell death. Toxicol Pathol 35:495–516. doi:10.1080/01926230701320337
Reed JC (2000) Mechanisms of apoptosis. Am J Pathol 157:1415–1430. doi:10.1016/S0002-9440(10)64779-7
McIlwain DR, Berger T, Mak TW (2013) Caspase functions in cell death and disease. Cold Spring Harb Perspect Biol 5:a008656. doi:10.1101/cshperspect.a008656
Tsujimoto Y (1998) Role of Bcl-2 family proteins in apoptosis: apoptosomes or mitochondria? Genes Cells 3:697–707. doi:10.1046/j.1365-2443.1998.00223.x
Wong RSY (2011) Apoptosis in cancer: from pathogenesis to treatment. J Exp Clin Cancer Res 30:1–14. doi:10.1186/1756-9966-30-87
Bankova VS, de Castro SL, Marcucci MC (2000) Propolis: recent advances in chemistry and plant origin. Apidologie 31:3–15. doi:10.1051/apido:2000102
Wagh VD (2013) Propolis: a wonder bees product and its pharmacological potentials. Adv Pharmacol Sci 2013:1–11. doi:10.1155/2013/308249
Khacha-ananda S, Tragoolpua K, Chantawannakul P, Tragoolpua Y (2013) Antioxidant and anti-cancer cell proliferation activity of propolis extracts from two extraction methods. Asian Pac J Cancer Prev 14:6991–6995. doi:10.7314/APJCP.2013.14.11.6991
Patel S (2016) Emerging adjuvant therapy for cancer: propolis and its constituents. J Diet Suppl 13:245–268. doi:10.3109/19390211.2015.1008614
Chen C-N, Wu C-L, Lin J-K (2007) Apoptosis of human melanoma cells induced by the novel compounds propolin A and propolin B from Taiwenese propolis. Cancer Lett 245:218–231. doi:10.1016/j.canlet.2006.01.016
Teerasripreecha D, Phuwapraisirisan P, Puthong S et al (2012) In vitro antiproliferative/cytotoxic activity on cancer cell lines of a cardanol and a cardol enriched from Thai Apis mellifera propolis. BMC Complement Altern Med 12:27. doi:10.1186/1472-6882-12-27
Trusheva B, Trunkova D, Bankova V (2007) Different extraction methods of biologically active components from propolis: a preliminary study. Chem Cent J 1:13. doi:10.1186/1752-153X-1-13
Ghasemi K, Ghasemi Y, Ebrahimzadeh MA (2009) Antioxidant activity, phenol and flavonoid contents of 13 citrus species peels and tissues. Pak J Pharm Sci 22:277–281
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63. doi:10.1016/0022-1759(83)90303-4
Zhu N, Wang Z (1997) An assay for DNA fragmentation in apoptosis without phenol/chloroform extraction and ethanol precipitation. Anal Biochem 246:155–158. doi:10.1006/abio.1997.2018
Prieto A, Díaz D, Barcenilla H et al (2002) Apoptotic rate: a new indicator for the quantification of the incidence of apoptosis in cell cultures. Cytometry 48:185–193. doi:10.1002/cyto.10132
He F, Wang Q, Zheng X-L et al (2012) Wogonin potentiates cisplatin-induced cancer cell apoptosis through accumulation of intracellular reactive oxygen species. Oncol Rep 28:601–605. doi:10.3892/or.2012.1841
Lan Y, Liu X, Zhang R et al (2013) Lithium enhances TRAIL-induced apoptosis in human lung carcinoma A549 cells. Biometals 26:241–254. doi:10.1007/s10534-012-9607-x
Tuve S, Liu Y, Tragoolpua K et al (2009) In situ adenovirus vaccination engages T effector cells against cancer. Vaccine 27:4225–4239. doi:10.1016/j.vaccine.2009.03.074
Sulaiman GM, Ad’hiah AH, Al-Sammarrae KW et al (2012) Assessing the anti-tumour properties of Iraqi propolis in vitro and in vivo. Food Chem Toxicol 50:1632–1641. doi:10.1016/j.fct.2012.01.022
Kujumgiev A, Tsvetkova I, Serkedjieva Y et al (1999) Antibacterial, antifungal and antiviral activity of propolis of different geographic origin. J Ethnopharmacol 64:235–240. doi:10.1016/S0378-8741(98)00131-7
Paviani L, Sacoda P, Saito E, Cabral F (2011) Extraction techniques of red and green propolis: extraction yield of phenolic compounds. Proc 11th Int Congr Eng Food, Greece, 22–26 May 2011
Biscaia D, Ferreira SRS (2009) Propolis extracts obtained by low pressure methods and supercritical fluid extraction. J Supercrit Fluids 51:17–23. doi:10.1016/j.supflu.2009.07.011
Park YK, Ikegaki M (2014) Preparation of water and ethanolic extracts of propolis and evaluation of the preparations. Biosci Biotechnol Biochem 62:2230–2232. doi:10.1271/bbb.62.2230
Chen L (2011) Extraction and antioxidant properties of propolis from China, Korea and Northern Thailand. Dissertation. Chulalongkorn University
Siripatrawan U, Vitchayakitti W, Sanguandeekul R (2013) Antioxidant and antimicrobial properties of Thai propolis extracted using ethanol aqueous solution. Int J Food Sci Technol 48:22–27. doi:10.1111/j.1365-2621.2012.03152.x
Athikomkulchai S, Awale S, Ruangrungsi N et al (2013) Chemical constituents of Thai propolis. Fitoterapia 88:96–100. doi:10.1016/j.fitote.2013.04.008
Sanpa S, Popova M, Tunkasiri T, et al (2016) Chemical profiles and antimicrobial activities of Thai propolis collected from Apis mellifera. Chiang Mai J Sci (Paper In Press)
Lirdprapamongkol K, Sakurai H, Abdelhamed S et al (2013) Chrysin overcomes TRAIL resistance of cancer cells through Mcl-1 downregulation by inhibiting STAT3 phosphorylation. Int J Oncol 43:329–337. doi:10.3892/ijo.2013.1926
Kimoto T, Aga M, Hino K et al (2011) Apoptosis of human leukemia cells induced by Artepillin C, an active ingredient of Brazilian propolis. Anticancer Res 21:221–228
Shen S-C, Ko CH, Tseng S-W et al (2004) Structurally related antitumor effects of flavanones in vitro and in vivo: involvement of caspase 3 activation, p21 gene expression, and reactive oxygen species production. Toxicol Appl Pharmacol 197:84–95. doi:10.1016/j.taap.2004.02.002
Seda Vatansever H, Sorkun K, Ismet Deliloğlu Gurhan S et al (2010) Propolis from Turkey induces apoptosis through activating caspases in human breast carcinoma cell lines. Acta Histochem 112:546–556. doi:10.1016/j.acthis.2009.06.001
Dreher D, Junod AF (1996) Role of oxygen free radicals in cancer development. Eur J Cancer 32A:30–38. doi:10.1016/0959-8049(95)00531-5
Khan HY, Zubair H, Ullah MF et al (2012) A prooxidant mechanism for the anticancer and chemopreventive properties of plant polyphenols. Curr Drug Targets 13:1738–1749. doi:10.2174/138945012804545560
Tsai Y-C, Wang Y-H, Liou C-C et al (2012) Induction of oxidative DNA damage by flavonoids of propolis: its mechanism and implication about antioxidant capacity. Chem Res Toxicol 25:191–196. doi:10.1021/tx200418k
Tsuchiya I, Hosoya T, Ushida M et al (2013) Nymphaeol-A isolated from Okinawan propolis suppresses angiogenesis and induces caspase-dependent apoptosis via inactivation of survival signals. Evidence-Based Complement Altern Med 2013:1–9. doi:10.1155/2013/826245
Li X, Wang J-N, Huang J-M et al (2011) Chrysin promotes tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL) induced apoptosis in human cancer cell lines. Toxicol In Vitro 25:630–635. doi:10.1016/j.tiv.2010.12.013
Sevrioukova IF (2011) Apoptosis-inducing factor: structure, function, and redox regulation. Antioxid Redox Signal 14:2545–2579. doi:10.1089/ars.2010.3445
Li LY, Luo X, Wang X (2001) Endonuclease G is an apoptotic DNase when released from mitochondria. Nature 412:95–99. doi:10.1038/35083620
Williams RJ, Spencer JPE, Rice-Evans C (2004) Flavonoids: antioxidants or signalling molecules? Free Radic Biol Med 36:838–849. doi:10.1016/j.freeradbiomed.2004.01.001
Kumazaki M, Shinohara H, Taniguchi K et al (2014) Propolis cinnamic acid derivatives induce apoptosis through both extrinsic and intrinsic apoptosis signaling pathways and modulate of miRNA expression. Phytomedicine 21:1070–1077. doi:10.1016/j.phymed.2014.04.006
Kim S-H, Kim S-H, Lee S-C, Song Y-S (2009) Involvement of both extrinsic and intrinsic apoptotic pathways in apoptosis induced by genistein in human cervical cancer cells. Ann N Y Acad Sci 1171:196–201. doi:10.1111/j.1749-6632.2009.04902.x
Waterhouse NJ, Green DR (1999) Mitochondria and apoptosis: HQ or high-security prison? J Clin Immunol 19:378–387. doi:10.1023/A:1020550716138
Chen C-N, Wu C-L, Lin J-K (2004) Propolin C from propolis induces apoptosis through activating caspases, bid and cytochrome c release in human melanoma cells. Biochem Pharmacol 67:53–66. doi:10.1016/j.bcp.2003.07.020
Buahorm S, Puthong S, Palaga T et al (2015) Cardanol isolated from Thai Apis mellifera propolis induces cell cycle arrest and apoptosis of BT-474 breast cancer cells via p21 upregulation. DARU J Pharm Sci 23:55–65. doi:10.1186/s40199-015-0138-1
Novak EM, Silva MS, Marcucci MC et al (2014) Antitumoural activity of Brazilian red propolis fraction enriched with xanthochymol and formononetin: An in vitro and in vivo study. J Funct Foods 11:91–102. doi:10.1016/j.jff.2014.09.008
Lisičić D, Benković V, Ðikić D et al (2014) Addition of propolis to irinotecan therapy prolongs survival in ehrlich ascites tumor-bearing mice. Cancer Biother Radiopharm 29:62–69. doi:10.1089/cbr.2013.1535
Rizk SM, Zaki HF, Mina MAM (2014) Propolis attenuates doxorubicin-induced testicular toxicity in rats. Food Chem Toxicol 67:176–186. doi:10.1016/j.fct.2014.02.031
Singla S, Kumar NR, Kaur J (2014) In vivo studies on the protective effect of propolis on doxorubicin-induced toxicity in liver of male rats. Toxicol Int 21:191–195. doi:10.4103/0971-6580.139808
Acknowledgments
We would like to thank the Research and Researcher for Industry (RRi) of The Thailand Research Fund (Grant No. PHD56I0018), Bee Product Industry Co., Ltd. and the National Research Council of Thailand (NRCT) for the financial support. We also would like to thank Prof. Dr. André M. Lieber, University of Washington, Seattle Washington, USA for kindly suggestion, providing the cervical carcinoma cell lines (HeLa), advice on flow cytometry and animal studies. We also thank Dr. Khanittha Punturee of Division of Clinical Chemistry, Department of Medical Technology, Faculty of Associated Medical Sciences, Chiang Mai University for kindly provided lung carcinoma cell lines (A549). We would like to thank Chiang Mai University Press and Mr. Matthew Hawkins, Department of English, Faculty of Humanity and Language Institute, Chiang Mai University for proof reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors; SK, KT, PC and YT declare that they have no conflict of interest.
Funding
The work was supported by Research and Researcher for Industry (RRi) of The Thailand Research Fund (Grant No. PHD56I0018) and the National Research Council of Thailand (NRCT).
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures about animal testing were performed according to the Animal Ethics Committees, Department of Biology, Faculty of Science, Chiang Mai University (Approved protocol No. 001/14) and the Institutional Animal Care and Use Committee (IACUC), Office of Animal Welfare, University of Washington (Approved protocol No. 3108-01).
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Khacha-ananda, S., Tragoolpua, K., Chantawannakul, P. et al. Propolis extracts from the northern region of Thailand suppress cancer cell growth through induction of apoptosis pathways. Invest New Drugs 34, 707–722 (2016). https://doi.org/10.1007/s10637-016-0392-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-016-0392-1