Summary
Purpose This phase I trial was designed to determine the recommended phase II dose(s) of everolimus (RAD001) with temozolomide (TMZ) in patients with glioblastoma (GBM). Patients receiving enzyme-inducing antiepileptic drugs (EIAEDs) and those not receiving EIAEDs (NEIAEDs) were studied separately. Patients and Methods Enrollment was restricted to patients with proven GBM, either newly diagnosed or at first progression. Temozolomide was administered at a starting dose of 150 mg/m2/day for 5 days every 28 days, and everolimus was administered continuously at a starting dose of 2.5 mg orally on a daily schedule starting on day 2 of cycle 1 in 28-day cycles. Results Thirteen patients receiving EIAEDs and 19 not receiving EIAEDs were enrolled and received 83 and 116 cycles respectively. Everolimus 10 mg daily plus TMZ 150 mg/m2/day for 5 days was declared the recommended phase II dose for the NEIAEDs cohort. In the EIAEDs group, doses were well tolerated without DLTs, and pharmacokinetic parameters indicated decreased everolimus exposure. Temozolomide pharmacokinetic parameters were unaffected by EIAEDs or everolimus. In the subset of 28 patients with measurable disease, 3 had partial responses (all NEIAEDs) and 16 had stable disease. Conclusion A dosage of 10 mg everolimus daily with TMZ 150 mg/m2/day for five consecutive days every 28 days in patients is the recommended dose for this regimen. Everolimus clearance is increased by EIAEDs, and patients receiving EIAEDs should be switched to NEIAEDs before starting this regimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) is the most common primary brain tumor in adults. Following maximal feasible surgical resection, most patients with GBM receive radiotherapy with concurrent and adjuvant temozolomide chemotherapy as primary treatment [1]. Although this recent advance has improved prognosis for many patients [2], more effective initial treatments for this intractable disease are needed.
A majority of patients with GBM have altered PTEN gene-suppression activity, usually as a consequence of gene deletion [3–5]. This molecular aberration leads to enhanced and dysregulated activity of the phosphotidylinositol 3-kinase (PI3K)/Akt pathway. Increased activity of this signaling cascade leads to activation of the mammalian target of rapamycin (mTOR), a critical step for cell-cycle progression. Considerable evidence implicates inactivation of the PTEN gene and subsequent activation of the PI3K/Akt/mTOR signaling pathway in gliomas, including an association with poor prognosis and a target for therapy in preclinical studies [6–8].
Although a phase I trial of rapamycin in recurrent GBM demonstrated in vivo evidence of mTOR inhibition and subsequent reduction of tumor cell proliferation [9], phase II trials using its analogue temsirolimus (CCI-779) have been disappointing [10, 11]. Similar disappointing outcomes have been noted in phase I/II trials combining mTOR inhibitors with other targeted therapies such as sorafenib and gefitinib in recurrent GBM [12, 13]. Despite this, mTOR inhibitors remain of interest in GBM as part of first-line therapy, a setting of greatest promise for changing the outcome of this disease.
Everolimus is one such mTOR inhibitor that has documented in vitro activity in GBM cell lines, and in vitro analysis of the effects of combining rapamycin analogues with standard cytotoxic chemotherapies such as nitrosoureas has demonstrated no antagonism but rather additive or synergistic activity [14]. Clinical studies evaluating everolimus (RAD001) in patients with a variety of solid tumors have established an effective monotherapy dose of 10 mg daily or 50–70 mg weekly [15–19]. Efficacy has been observed at these doses in a variety of tumors, and the US FDA has recently approved everolimus for advanced renal cell carcinoma [20].
This study was designed to determine the recommended phase II doses of everolimus with temozolomide in patients with GBM receiving temozolomide in the adjuvant setting or at first progression. Because everolimus is a substrate for the cytochrome P450 isoenzyme 3A4, patients receiving or not receiving enzyme-inducing anti-epileptic drugs (EIAEDs) were enrolled separately [21, 22].
Patients and methods
Patient population
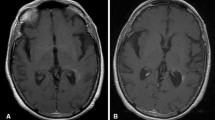
Entry was restricted to adults (≥18 years old) with a histologically confirmed GBM, either newly diagnosed or at first progression. Newly diagnosed patients required initial treatment with radiotherapy and concurrent TMZ. For these patients, study enrollment occurred before the first adjuvant cycle of temozolomide and everolimus was initiated with the first cycle of adjuvant treatment. Prophylaxis against Pneumocystis jerovici was not mandatory for newly-diagnosed patients, and only one patient received trimethoprim/sulfamethoxazole while on study treatment. Patients with progressive GBM required radiographic progression following radiotherapy. For patients with progressive disease, one prior chemotherapy regimen administered in the adjuvant setting was permitted. Prior TMZ was permitted provided last exposure was at least 4 months before study entry. Treatment with radiotherapy was mandatory and was to be completed at least 12 weeks prior to enrollment. Patients with progressive GBM also were required to have bidimensionally measurable disease by MR or CT imaging.
Baseline MR/CT scans were performed in all patients within 21 days prior to registration. Patients receiving corticosteroids required stable doses for at least 14 days prior to study enrolment. All patients were to have an ECOG performance status ≤2, an estimated life expectancy of at least 12 weeks and acceptable bone marrow and organ function. The protocol and informed consent were reviewed and approved by the local institutional ethics review boards of each participating centre and all patients provided signed informed consent before enrollment.
Treatment plan
Patients receiving EIAEDs were studied separately from those not receiving EIAEDs.. Everolimus was supplied by the NCIC CTG Investigational New Drug program under an agreement with Novartis Pharmaceuticals. The dose escalation schedule of everolimus and TMZ is outlined in Table 1. In cycle 1 only, everolimus was initiated on day 2 of the cycle while TMZ was initiated on day 1, so as to evaluate TMZ PK alone and in combination with everolimus. Dose escalation was planned in groups of three patients, with an additional three patients to be added at the first indication of a dose limiting toxicity (DLT). Toxicities were graded according to the Common Terminology Criteria for Adverse Events, Version 3.0 (http://ctep.cancer.gov/reporting/ctc.html). No new patients were to be entered at an escalated dose level until at least three patients had completed one treatment cycle at the previous level without evidence of DLT. DLTs were defined as any grade 4 thrombocytopenia or thrombocytopenic bleeding, grade 4 neutropenia for ≥7 days or grade ≥3 febrile neutropenia, grade ≥3 microbiologically documented infection with grade ≥3 neutropenia, grade ≥3 nonhematologic toxicity or grade ≥2 clinically relevant neurotoxicity or cardiotoxicity, failure to administer full doses of everolimus for ≥7 days due to toxicity, or a delay of ≥2 weeks in starting cycle 2 for reasons of toxicities. If 1/3 patients in a cohort experienced a DLT, an additional three patients were enrolled at the same dose level for a total of six patients. Maximum administered dose (MAD) was defined as at least 2/3 or 2/6 patients in a cohort experiencing a DLT. The next lower dose would be declared the recommended phase II dose (RP2D) for expansion, and an additional six patients would be enrolled at that dose level.
If clinically indicated, intermediate dose levels other than the levels specified in Table 1 were permitted. Additionally, if patients in the NEIAEDs cohort accrued more quickly, and tolerated a given dose level without DLTs, patients in the EIAEDs arm could skip that dose level given the likelihood that they could tolerate higher dose levels than NEIAEDs patients.
Patient evaluation
Pretreatment evaluation included a complete history and physical examination including neurologic assessment. Clinical evaluations were repeated before the start of every 4-week cycle. Complete blood counts were performed weekly for cycles 1 and 2, and on days 1 and 15 for subsequent cycles. Biochemistry was performed on days 1 and 15 of all cycles. Magnetic resonance (MR) imaging or computed tomography (CT) was obtained at baseline, and at the end of every other cycle. Enhancing tumor was assessed for radiographic response, and responses were determined by the Macdonald criteria [23]. All responses (CR and PR) required confirmation by repeat imaging between 4 and 6 weeks from the time at which response criteria were met. A designation of stable radiographic disease required at least one assessment satisfying criteria for SD a minimum of 8 weeks post study entry. Response duration was measured from the time measurement criteria are first met until disease progression. Stable disease duration was measured from the start of therapy until disease progression.
Pharmacokinetics (PK)
Pharmacokinetics of TMZ and RAD were performed during the first cycle only and patients were instructed to take RAD and TMZ in the morning on an empty stomach. Anticonvulsants were administered according to instructions of treating physicians and the schedule was not altered for PK studies.
Sample collection
For TMZ PK, whole blood was collected in EDTA-containing tubes on day 1, cycle 1 at each of the following times: baseline (before ingestion) and at 0.25, 0.5, 1, 2, 4 and 6 h after administration. To study possible interaction with everolimus, TMZ PK samples were also collected on day 5, cycle 1 using an identical schedule. Everolimus PK with TMZ co-administration was evaluated on day 5, cycle 1 at each of the following times: baseline (before ingestion) and at 1, 2, 4, 6 and 24 h after administration. To determine everolimus PK in the absence of TMZ, blood was collected at identical times on day 15, cycle 1.
Following collection, whole blood for TMZ PK was centrifuged at 4°C for 15 min at 3,000 rpm. A 2.0 mL plasma sample was transferred to a plastic tube containing 8.5% phosphoric acid, vortexed and stored at a minimum of −20°C until analysis. For everolimus PK, whole blood was collected into a tube containing EDTA before 2.5 mL was transferred to a polypropylene tube for storage at a minimum of −20°C until analysis. Whole blood was selected for everolimus analysis because of the preferential distribution of this drug into red blood cells and its limited storage stability in plasma.
Measurement of temozolomide levels
Temozolomide concentrations were determined by validated methods previously described and with a high-performance liquid chromatograph coupled with a triple quadrupole mass spectrometer [24]. The lower limit of quantitation was 25.0 ng/mL.
Measurement of everolimus levels
Whole-blood concentration of everolimus was determined by liquid chromatography-mass spectrometry with lower limits of quantification of 0.3 ng/ml. PK for everolimus were derived by standard non-compartmental analysis methods using WinNonlin, Version 5 (Pharsight Corporation, CA).
Translational studies
Paraffin-embedded tumor tissue was obtained from all patients for PTEN immunohistochemistry. Expression levels were assessed semi-quantitatively by evaluating the relative staining intensity (0, absent, 1, weak, 2, moderate and 3, strong) and the percent tumor cells stained (0, no staining, 1, ≤10% staining, 2, 11–50% staining, and 3, ≥51% staining). The final expression level for each tumor was represented by the sum of grades of staining intensity and extent, and the median for all specimens was used to dichotomize high and low expressing tumors. Two independent pathologists performed assessments of all specimens.
Statistical considerations
The primary endpoint of this study was to determine the MAD and establish a recommended dose of everolimus when given in combination with standard dose temozolomide in patients with GBM receiving and not receiving EIAEDs, and to characterize the toxicities and pharmacokinetics of this combination. Pharmacokinetic variables are reported as mean values ± SD. Radiographic responses were summarized.
Results
Patient characteristics
Thirty-two patients were enrolled in this study, 19 in the NEIAED arm and 13 in the EIAED arm. One patient in the NEIAED group was deemed ineligible (diagnosis of another cancer within 5 years of study entry), but is included in all tables except response. Patient characteristics are summarized in Table 2.
Recommended phase II dose (RP2D) and adverse events –NEIAED cohort
In the NEIAED cohort, toxicities were encountered at dose level 2, the first dose level where temozolomide was administered at a full dose of 200 mg/m2/day with everolimus at 2.5 mg/day. Although no DLTs were observed at this level, three of four patients required a delay in the start of cycle 2 because of myelosuppression, and two of three patients had the dose of temozolomide reduced to 150 mg/m2/day for cycle 2. This experience suggested that for patients in the NEIAED arm, a dosage of temozolomide at 200 mg/m2/day could not easily be combined with everolimus, so temozolomide dosing was fixed at subsequent dose levels to 150 mg/m2/day while escalating everolimus as planned.
The RP2D in the NEIAED cohort was 10 mg/day everolimus with temozolomide 150 mg/m2/day. Eight patients were enrolled at this level, and none had DLTs. This was declared the recommended dose for the combination on the basis that full single-agent doses of everolimus were given and that PK data were comparable to those obtained for the recommended dose of 10 mg/day for everolimus.
As shown in Table 3, common adverse effects included mild fatigue, flushing, pruritus, rash, mucositis, nausea and vomiting, headache and cough. Myelosuppression at this dose level was mild: two patients had grade 3 thrombocytopenia, two had grade 3 lymphopenia and two had grade 2 granulocytopenia. Although pneumonitis is sometimes seen with mTOR inhibitors, only 4 patients in the NEIAED cohort had pneumonitis: three grade 1 and one grade 2.
One patient enrolled in the NEIAED cohort at dose level 1 experienced grade 2 supraventricular arrhythmia (sinus tachycardia) and grade 3 left ventricular systolic dysfunction during cycle 3 and was removed from protocol therapy.
Recommended phase II dose (RP2D) and adverse events –EIAED cohort
Accrual in the EIAED cohort was slower than in the NEIAED, and toxicities encountered by these patients are listed in Table 3. One patient in the EIAED group was treated at dose level 1, and this patient experienced no DLTs. Dose level 2 enrolled six patients because one patient experienced a protocol defined DLT of grade 4 thrombocytopenia and cycle 2 delay exceeding 2 weeks due to grade 2 thrombocytopenia. The three additional patients enrolled to this level did not experience DLTs, and further dose escalations were undertaken as per protocol guidelines. Two patients in the EIAED arm were enrolled in the protocol defined third dose level, and no DLTs were observed. At this point in the trial, the recommended dose for NEIAED patients was established, and all subsequent EIAED patients were enrolled at this dose level to determine safety and PK. Four EIAED patients were enrolled at a dose level of temozolomide 150 mg/m2/day with everolimus 10 mg/day because one withdrew and was thereafter replaced. At this dose level no DLTs were experienced and escalation halted despite the MAD not having been reached. Because PK data suggested more rapid clearance of everolimus in this cohort, a recommendation was made that patients receiving EIAEDs should switch to NEIAEDs before starting this regimen. There were no SAEs or grade III or greater non-hematologic toxicities reported in the EIAED cohort.
Pharmacokinetic results
Pharmacokinetic data are available from 13 patients in the NEIAED cohort and ten in the EIAED cohort, and are summarized in Supplementary Tables 1 and 2. Temozolomide PK on days one and five were similar for all 150 mg/m2/day dose levels and all 200 mg/m2/day dose levels in NEIAED and EIAED cohorts respectively, being unaffected by the presence of EIAEDs and increasing doses of everolimus (Supplementary Figures 1 and 2). Moreover, the observed temozolomide PK were similar to those expected from single agent temozolomide based on historical data [25, 26].
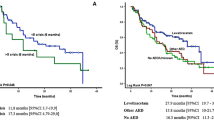
In patients enrolled in the NEIAED cohort, the whole blood exposure of everolimus increased with dose. Everolimus PK were comparable when administered alone (cycle 1 day 15) and in combination with TMZ (cycle 1 day 5), in patients belonging to the NEIAED cohort. There was no evidence of influence of TMZ on everolimus pharmacokinetics at the three dose levels of 2.5 mg, 5 mg and 10 mg everolimus investigated in this study.
In patients in the EIAED cohort, there were fewer patients at each dose level with evaluable PK samples. At dose level 2 (n = 6), AUC was 105.67 ± 35.83 ng.h/mL at cycle 1 day 5, which was nearly 50% lower than corresponding exposure of 243 ± 142.52 ng.h/mL at cycle 1 day 5 observed in the NEIAED cohort (Fig. 1). Similarly on cycle 1 day 15, AUC was 86.83 ± 45.16 ng.h/mL in EIAED cohort, while AUC was 171.50 ± 150.61 in NEIAED cohort (Fig. 2). These data suggest that concomitant administration of EIAEDs with everolimus, leads to decreased everolimus exposure.
Response data
Seventeen of 19 patients in the NEIAED cohort were evaluable for radiographic response. Of these, three PRs of 7.8 months median duration (range, 6.4–7.8 months) and 9 SDs (range, 2.7–11.5 months) were observed. No CRs were documented, and five patients were removed from protocol therapy due to PD. All PRs occurred in newly diagnosed patients and are of uncertain significance given the confounding influence of radiotherapy. The response rate for all evaluable patients in the NEIAED cohort was 17.6% (95% CI: 3.8, 43.4%).
Eleven of 13 patients in the EIAED cohort were evaluable for radiographic response. No responses were observed, seven patients had SD of median duration 38.3 months (range, 3.1–38.3 months) and four were removed from study for PD.
Translational studies
PTEN analysis by immunohistochemistry of the original formalin-fixed and paraffin-embedded glioblastoma surgical sample was undertaken in 32 cases. Results were inconclusive with no apparent differences in response and survival between patients with PTEN intact and deleted tumors .
Discussion
This trial has demonstrated that the mTOR inhibitor everolimus can be administered safely at a daily dosage of 10 mg in combination with temozolomide at 150 mg/m2/day for five consecutive days in a 28-day cycle in patients not receiving EIAEDs, and is the recommended phase II dosage of this combination. At this dosage, the majority of adverse effects were grades 1 and 2 and consistent with known adverse effect profiles of mTOR inhibitors and of temozolomide when these agents are administered as monotherapy. Notably, no new toxicities were encountered as a consequence of this combination therapy, and no cases of opportunistic infections were documented.
An objective of this study was the evaluation of pharmacokinetic endpoints. In the NEIAED group, there did not appear to be any appreciable impact of temozolomide administration on everolimus pharmacokinetic parameters, and results are comparable to those seen with single agent everolimus in phase I studies [19]. Moreover our data provided reassurance that everolimus did not affect temozolomide exposure as the observed temozolomide PK in both EIAED and NEIAED cohorts were similar to that expected from single agent temozolomide based on historical data. However, everolimus is metabolized through the CYP3A4/5 hepatic enzymes, and the use of EIAEDs appears to lead to enhanced everolimus metabolism, resulting in diminished overall exposure.
Although the manufacturer recommended schedule for everolimus is a daily one, both weekly and daily oral doses have been evaluated in phase I trials [19, 27]. Based on the clinical safety profile and tumor pharmacodynamic studies, these studies recommended a dosing of everolimus at either 10 mg/day or 50–70 mg/week. As expected, the maximum serum steady-state concentration and area under the curve at steady state are increased in the weekly as compared to daily regimen. In this trial, a daily regimen was selected because the daily regimen results in more profound and sustained inhibition of the mTor pathway, an observation that may possibly be related to much lower everolimus trough concentrations in the weekly as compared to daily schedule.
Most patients in both cohorts experienced disease stabilization of various durations. Three partial responses in the NEIAED cohort were documented, and these responses were restricted to patients with newly-diagnosed GBM. However, radiographic responses cannot be assessed reliably in this study because the considerable treatment effect of irradiation and the absence of tumor MGMT promotor hypermethylation data make interpretation of radiographic response and survival outcomes impossible.
PTEN expression by immunohistochemistry of archival tumor specimens revealed no relationship between tumor PTEN status and response. These results are consistent with observations of others who have examined the impact of PTEN expression on response to mTOR inhibitors [9, 28].
This study is the first to evaluate everolimus with temozolomide in patients with GBM. Previous single agent studies of mTOR inhibitors in recurrent GBM given alone or in combination with targeted agents have been disappointing [10–13, 29]. Explanations for the absence of activity reported to date in studies involving mTOR inhibitors in recurrent GBM have included redundancy of signaling pathways, mutation of mTOR and associated binding proteins and alteration of the downstream effectors of mTOR including preferential inhibition of TOR complex 1 resulting in aberrant paradoxical upregulation of AKT via increased mTOR complex 2 activation [30, 31].
The study has determined a phase II dose of everolimus and TMZ for GBM patients receiving adjuvant treatment without EIAEDs,. Everolimus cannot easily be combined with the recommended maximal dose of temozolomide when administered as a 5-day regimen because of unacceptable myelosuppression. However the recommended daily monotherapy dose of everolimus can be combined with temozolomide at 150 mg/m2/day when given as a 5-day regimen, and at this dose temozolomide is expected to have adequate antitumor activity. Everolimus has demonstrable anticancer activity, has been incorporated into the treatment of renal cell carcinoma and neuroendocrine tumors and is being studied as part of combination therapy for several cancers [18]. These encouraging developments suggest that further evaluation of agents such as everolimus for the treatment of central nervous tumors should continue. With preclinical evidence for synergy between radiotherapy and mTOR inhibitors [32], a phase I trial evaluating the safety of radiotherapy, temozolomide and everolimus in patients with newly diagnosed disease could lay the foundations for a larger randomized trial comparing radiotherapy and temozolomide with and without everolimus in patients with newly diagnosed GBM.
References
Stupp R, Hegi ME, Gilbert MR, Chakravarti A (2007) Chemoradiotherapy in malignant glioma: standard of care and future directions. J Clin Oncol 25:4127–4136
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466
Ohgaki H, Kleihues P (2007) Genetic pathways to primary and secondary glioblastoma. Am J Pathol 170:1445–1453
Louis DN (2006) Molecular pathology of malignant gliomas. Annu Rev Pathol 1:97–117
Duerr EM, Rollbrocker B, Hayashi Y et al (1998) PTEN mutations in gliomas and glioneuronal tumors. Oncogene 16:2259–2264
Rich JN, Hans C, Jones B et al (2005) Gene expression profiling and genetic markers in glioblastoma survival. Cancer Res 65:4051–4058
Smith JS, Tachibana I, Passe SM et al (2001) PTEN mutation, EGFR amplification, and outcome in patients with anaplastic astrocytoma and glioblastoma multiforme. J Natl Canc Inst 93:1246–1256
Chakravarti A, Zhai G, Suzuki Y et al (2004) The prognostic significance of phosphatidylinositol 3-kinase pathway activation in human gliomas. J Clin Oncol 22:1926–1933
Cloughesy TF, Yoshimoto K, Nghiemphu P et al (2008) Antitumor activity of rapamycin in a phase I trial for patients with recurrent PTEN-deficient glioblastoma. PLoS Med 5:e8
Galanis E, Buckner JC, Maurer MJ et al (2005) Phase II trial of temsirolimus (CCI-779) in recurrent glioblastoma multiforme: a North Central Cancer Treatment Group Study. J Clin Oncol 23:5294–5304
Chang SM, Wen P, Cloughesy T et al (2005) Phase II study of CCI-779 in patients with recurrent glioblastoma multiforme. Investig New Drugs 23:357–361
Kreisl TN, Lassman AB, Mischel PS et al (2009) A pilot study of everolimus and gefitinib in the treatment of recurrent glioblastoma (GBM). J Neurooncol 92:99–105
Wen PY, Cloughesy T, Kuhn J et al (2009) Phase I/II study of sorafenib and temsirolimus for patients with recurrent glioblastoma (GBM) (NABTC 05–02). J Clin Oncol 27:15S
Tanaka K, Sasayama T, Mizukawa K et al (2007) Specific mTOR inhibitor rapamycin enhances cytotoxicity induced by alkylating agent 1-(4-amino-2-methyl-5-pyrimidinyl)methyl-3-(2-chloroethyl)-3-nitrosourea (ACNU) in human U251 malignant glioma cells. J Neurooncol 84:233–244
Motzer RJ, Escudier B, Oudard S et al (2008) Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. Lancet 372:449–456
Dancey J (2010) mTOR signaling and drug development in cancer. Nat Rev Clin Oncol 7:209–219
Atkins MB, Yasothan U, Kirkpatrick P (2009) Everolimus. Nat Rev Drug Discov 8:535–536
Chan HY, Grossman AB, Bukowski RM (2010) Everolimus in the treatment of renal cell carcinoma and neuroendocrine tumors. Adv Ther 27:495–511
O'Donnell A, Faivre S, Burris HA 3rd et al (2008) Phase I pharmacokinetic and pharmacodynamic study of the oral mammalian target of rapamycin inhibitor everolimus in patients with advanced solid tumors. J Clin Oncol 26:1588–1595
Sun M, Lughezzani G, Perrotte P, Karakiewicz PI (2010) Treatment of metastatic renal cell carcinoma. Nat Rev Urol 7:327–338
Kuhn JG, Chang SM, Wen PY et al (2007) Pharmacokinetic and tumor distribution characteristics of temsirolimus in patients with recurrent malignant glioma. Clin Cancer Res 13:7401–7406
Boni J, Leister C, Burns J et al (2007) Pharmacokinetic profile of temsirolimus with concomitant administration of cytochrome p450-inducing medications. J Clin Pharmacol 47:1430–1439
Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8:1277–1280
Meany HJ, Warren KE, Fox E et al (2009) Pharmacokinetics of temozolomide administered in combination with O6-benzylguanine in children and adolescents with refractory solid tumors. Canc Chemother Pharmacol 65:137–142
Dhodapkar M, Rubin J, Reid JM et al (1997) Phase I trial of temozolomide (NSC 362856) in patients with advanced cancer. Clin Cancer Res 3:1093–1100
Newlands ES, Blackledge GR, Slack JA et al (1992) Phase I trial of temozolomide (CCRG 81045: M&B 39831: NSC 362856). Br J Cancer 65:287–291
Tabernero J, Rojo F, Calvo E et al (2008) Dose- and schedule-dependent inhibition of the mammalian target of rapamycin pathway with everolimus: a phase I tumor pharmacodynamic study in patients with advanced solid tumors. J Clin Oncol 26:1603–1610
Yang L, Clarke MJ, Carlson BL et al (2008) PTEN loss does not predict for response to RAD001 (everolimus) in a glioblastoma orthotopic xenograft test panel. Clin Cancer Res 14:3993–4001
Reardon DA, Desjardins A, Vredenburgh JJ et al (2010) Phase 2 trial of erlotinib plus sirolimus in adults with recurrent glioblastoma. J Neurooncol 96:219–230
Gulati N, Karsy M, Albert L et al (2009) Involvement of mTORC1 and mTORC2 in regulation of glioblastoma multiforme growth and motility. Int J Oncol 35:731–740
Akhavan D, Cloughesy TF, Mischel PS (2010) mTOR signaling in glioblastoma: lessons learned from bench to bedside. Neuro Oncol 12:882–889
Eshleman JS, Carlson BL, Mladek AC et al (2002) Inhibition of the mammalian target of rapamycin sensitizes U87 xenografts to fractionated radiation therapy. Cancer Res 62:7291–7297
Funding
Financial support was provided by Novartis, Inc. to NCIC CTG for the conduct of this trial
Conflicts of Interest
Dr. Urva is an employee of Novartis, Inc. and owns stock in the company. On behalf of the NCIC CTG Dr. Eisenhauer received funding from Novartis, Inc. for the conduct of this trial
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
Pharmacokinetic Variables of Temozolomide in NEIAED and EIAED Patients (DOC 48 kb)
Supplementary Table 2
Pharmacokinetic Variables of Everolimus in NEIAED and EIAED Patients (DOC 42 kb)
Supplementary Figure 1
Mean TMZ AUCinf in plasma at Day 1 in EIAED and NEIAED cohorts by dose level. (JPEG 2056 kb)
Supplementary Figure 2
Mean TMZ AUCinf in plasma at Day 5 in EIAED and NEIAED cohorts by dose level. (JPEG 2056 kb)
Rights and permissions
About this article
Cite this article
Mason, W.P., MacNeil, M., Kavan, P. et al. A phase I study of temozolomide and everolimus (RAD001) in patients with newly diagnosed and progressive glioblastoma either receiving or not receiving enzyme-inducing anticonvulsants: an NCIC CTG study. Invest New Drugs 30, 2344–2351 (2012). https://doi.org/10.1007/s10637-011-9775-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-011-9775-5