Summary
Purpose: We report the first phase I trials of 2-methoxyestradiol (2ME2, Panzem® Capsules, EntreMed, Rockville, MD), alone and in combination with docetaxel, in patients with metastatic breast cancer (MBC).
Patients and methods: In Trial 001, 2ME2 monotherapy was administered orally once (200–1000 mg/d, cohorts 1–5) or twice daily (200–800 mg/q12h, cohorts 6–9) for 28 days followed by a 14-day observation period, continuously thereafter. In Trial 002, docetaxel 35 mg/m2 was administered weekly for four of six weeks for a maximum six cycles; 2ME2 (200–1000 mg/d) was given orally once daily for 28 days followed by a 13-day observation period in cycle one, continuously thereafter. In both trials, responding or stable patients continued 2ME2 until progression.
Results: Trial 001 enrolled 31 patients; there were no objective responses. Trial 002 enrolled 15 patients; ORR was 20% including one CR. There were no Grade IV toxicities; MTD was not reached in either study. When combined with docetaxel, three patients had significant transaminase elevations that returned to normal with continued treatment (in two of three patients). There was significant inter-patient variability and extensive metabolism to 2-methoxyestrone (2ME1). Steady-state AUC and trough concentrations of 2ME2 increased linearly up to 400–600 mg/d; doses above 400–600 mg/d did not increase 2ME2 levels. The target trough concentration (3–25 ng/mL) was not attained. Combined administration did not alter docetaxel or 2ME2 pharmacokinetics.
Conclusion: 2ME2, alone or in combination with docetaxel, was well tolerated in patients with MBC but systemic exposure remained below the expected therapeutic range.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancers must stimulate angiogenesis, the growth of new blood vessels, in order to grow beyond a few millimeters in diameter [1, 2]. Extensive laboratory data suggests that angiogenesis plays an essential role in breast cancer development, invasion and metastasis [3–6]. Clinicopathologic correlations also confirm the central role of angiogenesis. Breast cancer vascularity, quantified by tumor microvessel density, predicts tumor shedding at the time of surgery [7], bone marrow micrometastases [8] recurrence and overall survival [9–11]. This nascent vascular network provides a unique opportunity for therapy.
2ME2 is naturally formed in vivo by the sequential hydroxylation and O-methylation of estradiol at the 2-position. Despite being a natural derivative of estradiol, 2ME2 binds very poorly to the estrogen receptor (0.05% of estradiol binding) [12]. Accordingly, 2ME2 does not exhibit direct estrogenic activity [13–16]. 2ME2 does not sustain the growth of estrogen-dependent breast cancer cell lines and has significant cytotoxic activity independent of estrogen responsiveness at sub- and low micromolar concentrations [17]. 2ME2 is a potent inhibitor of tumor growth in many human tumor xenograft and metastases models [17–19] and exhibits antiangiogenic activity in vitro and in vivo [18–20]. Treatment with 2ME2 in vitro inhibits proliferation of endothelial cells stimulated by either vascular endothelial growth factor (VEGF, 60 ng/mL) or basic fibroblast growth factor (bFGF, 20 ng/mL) and enhances the antiproliferative effect of docetaxel [21].
Altogether, these findings suggest that 2ME2 may provide an alternative or addition to existing therapies for the treatment of breast cancer. We therefore conducted separate phase I trials of 2ME2, alone (Trial 001) and in combination with docetaxel (Trial 002), in patients with metastatic breast cancer.
Patients and methods
Patient eligibility
Trial 001
Women with histologically or cytologically confirmed metastatic breast cancer were eligible if they had received at least two prior regimens (one of which may have been hormonal) for metastatic disease. In addition patients were required to have a Karnofsky performance status ≥80 and adequate renal (creatinine <1.5 mg/dL), hepatic (total bilirubin <1.5 mg/dL; AST and ALT <2.5 times upper limit of normal) and hematologic (WBC >3000/mm3; platelets >100,000/mm3; INR ≤1.2 with normal PTT) function. Patients were excluded if they had any history or radiographic evidence of central nervous system disease; screening brain magnetic resonance image (MR) was required prior to entry. In addition patients may not have had any other primary malignancy within 5 years, major surgical procedure or chemotherapy within 21 days, active infection or clinically significant cardiovascular disease including myocardial infarction or unstable angina within 3 months. Women of reproductive potential were required to use an effective barrier means of contraception throughout the study.
Trial 002
Eligibility criteria were identical to Trial 001 except patients were required to have an Eastern Cooperative Oncology Group (ECOG) Performance Status 0 or 1 and could have received no more than one prior non-taxane containing chemotherapy regimen for advanced disease. Adjuvant taxane use was allowed if the disease-free interval was >12 months.
The Indiana University Institutional Review Board approved both protocols; all patients provided individual written informed consent prior to screening and study entry.
Treatment plan
Trial 001
2ME2 monotherapy was administered orally once (200–1000 mg/d, cohorts 1–5) or twice daily (200–800 mg/q12h, cohorts 6–9) for 28 days followed by a 14-day observation period in cycle one. After cycle one, 2ME2 was given continuously until progression; 28 days defined each subsequent cycle.
Trial 002
Docetaxel 35 mg/m2 was administered weekly for four of six weeks; dexamethasone 4 mg orally every 12 h for 3 doses was initiated 12 h prior to each docetaxel infusion to prevent fluid accumulation. 2ME2 (200–1000 mg/d) was given orally once daily on Days 2–29 followed by a 13-day observation period in cycle one; continuously thereafter (Fig. 1). After a maximum 6 cycles of combined therapy, responding or stable patients continued 2ME2 alone until progression; 28 days defined each subsequent cycle. Docetaxel dose was reduced for hematologic and non-hematologic toxicity.
Docetaxel 35 mg/m2 was administered weekly for four of six weeks. 2ME2 (200–1000 mg/d) was given orally once daily on Days 2–29 followed by a 13-day observation period in cycle one. 2ME2 was administered continuously in all subsequent cycles. After a maximum 6 cycles of combined therapy, responding or stable patients continued 2ME2 alone until progression; 28 days defined each subsequent cycle
Safety and efficacy assessments
In both studies patients were evaluated weekly for the first 4 weeks, then on Days 1 and 15 of all subsequent treatment cycles. Complete blood count, serum chemistries and hormone levels (estrogen, progesterone, testosterone, luteinizing hormone and follicle stimulating hormone) were assessed at each evaluation. Complete blood count was measured prior to each docetaxel infusion in patients enrolled in Trial 002. Docetaxel treatment was interrupted for Grade ≥3 non-hematological or Grade 4 hematological toxicity according to the National Cancer Institute Common Toxicity Criteria, version 2.0. In both studies 2ME2 was discontinued for Grade 3 or greater non-hematological, and Grade 4 hematological toxicity that did not resolve within 14 days; 2ME2 dose was not otherwise adjusted. Disease status was assessed after cycle 1, cycle 2 and every other cycle thereafter.
Pharmacokinetics
Trial 001
Serum for determination of 2ME2 pharmacokinetics was obtained prior to dosing, 30, 60, and 90 min, 2, 4, 8, 12 h after dosing on Days 1 and 28 of cycle 1. Additional samples were obtained 16 and 24 h after dosing in patients in cohorts 1–5. Serum for analysis of 2ME2 and 2ME1 trough concentrations was obtained prior to dosing on Days 8, 15 and 22 of cycle 1 and on Day 1 of all subsequent cycles.
Trial 002
Serum for determination of docetaxel concentration was obtained prior to dosing, at the end of infusion, 30 and 60 min, 2, 4, 6, 8, 12, and 24 h after infusion on Day 1 of cycle 1. Additional samples were obtained immediately after infusion on Days 8, 15 and 22 of cycle 1. 2ME2 was initiated on Day 2 of cycle 1; serum for determination of 2ME2 pharmacokinetics was obtained prior to dosing, 10, 20, 30, 60, and 90 min, 2, 4, 8, and 24 h after dosing. Additional samples were obtained 1 h after dosing on Days 8, 15, 22, and 29 of cycle 1. Detailed pharmacokinetic sampling for both docetaxel and 2ME2 was repeated on Day 22 of cycle 2.
2ME2 pharmacokinetic analyses included area under the curve (AUC), elimination half-life (t 1/2), t max, C max, C min, estimated steady-state concentration (C ss), total clearance (C l), and volume of distribution (V d). Serum concentrations of 2ME2 and 2ME1 were determined using a validated gas chromatographic/mass spectrometric method using trideuterated 2ME2 and 2ME1 as internal standards. Docetaxel pharmacokinetic analyses included total clearance, volume of distribution, and dose-normalized AUC. Serum concentration of docetaxel was determined using a validated high-performance liquid chromatography—mass spectroscopy method using atmospheric pressure chemical ionization. The lower limit of quantitation was 0.5 ng/mL. The assay was linear over the range of 0.5–1000 ng/mL. Intra-day and interday coefficient of variation was less than 10%.
Pharmacodynamics
Blood and urine samples were collected to monitor changes in the concentrations of the angiogenic proteins VEGF (plasma and urine) and bFGF (serum and urine) at baseline, Day 28 of cycle 1, and Day 1 of all subsequent cycles. Serum only was collected for assessment of VCAM-1, MMP-2 and MMP-9. Samples were obtained in a serum separator or standard red top tube and allowed to stand on ice for 30 min, then separated by centrifugation at 3000g for 30 min. Plasma, serum and urine were stored at −20°C in 1 ml aliquots for later analysis; duplicate aliquots were preserved for each patient at each time point. All samples were measured in duplicate using commercially available enzyme linked immunosorbant assays (ELISA, R & D Systems, Minneapolis, MN and Oncogene Research Products, Cambridge, MA). All samples with a coefficient of variation >10% were repeated. The assays have the following limits of detection: VEGF 9 pg/mL, bFGF <1 ng/mL, VCAM-1 <2 ng/mL, MMP-2 <0.37 ng/mL, and MMP-9 <0.156 ng/mL.
Prostate-specific antigen (PSA) is produced by ∼30% of breast cancer and is associated with improved disease-free and overall survival in patients with localized breast cancer [22, 23]. PSA inhibits bFGF- and VEGF-stimulated endothelial proliferation [24] and is cleaved to an angiostatin-like compound by plasminogen suggesting a potential role in regulation of breast cancer angiogenesis [25]. Serum PSA was measured at baseline, Days 1 and 15 of cycle 1 and Day 1 of all subsequent cycles. PSA assays were performed in the CLIA certified laboratories at Indiana University using standard techniques.
Statistical analysis
The primary objective of these phase I trials was to evaluate the safety and tolerability of 2ME2, alone and in combination with docetaxel, in patients with metastatic breast cancer. Dose limiting toxicity (DLT) was defined as any Grade IV hematologic or Grade III non-hematologic toxicity within the first cycle of therapy. Three patients were enrolled into each successive cohort (Trial 001 cohorts 1–5: 200–1000 mg/d, cohorts 6–9: 200–800 mg twice daily; Trial 002: 200–1000 mg/d). If none of the 3 patients in a cohort experienced DLT, accrual to the next cohort commenced. If 2 or more patients experienced DLT, the previous dose level was considered maximum tolerated dose (MTD). If DLT was observed in 1 of 3 patients, 3 additional patients were to be added to that dose level. If no additional DLTs were reported, accrual to the next cohort commenced. If ≥2 of the 6 patients experienced DLT, the previous dose level was considered maximum tolerated dose (MTD).
Secondary endpoints included characterization of 2ME2 pharmacokinetics, impact of 2ME2 on hormone levels, assessment of potential surrogates of response and angiogenesis, and tumor response. A complete response (CR) was defined as the complete disappearance of all clinically detectable disease measured by physical examination and/or radiographic studies for a period of at least 4 weeks. A partial response (PR) was defined as a greater than or equal to a 50% decrease in the sum of the products of the two longest perpendicular diameters of all measurable lesions for a period of at least 4 weeks without an increase greater than 25% in the size of any area known to contain malignant disease and without the appearance of any new areas of malignancy. Progressive disease (PD) was defined as an increase of at least 25% in the size of measurable lesions. Time to treatment failure (TTF) was defined as time from study entry to discontinuation of study therapy for any reason.
Results
Patient populations
Thirty-one patients were enrolled in Trial 001; 15 patients were enrolled in Trial 002. Patient characteristics are shown in Table 1. All patients were evaluable for toxicity. One patient in Trial 001 discontinued treatment without progression prior to the first disease assessment and is not evaluable for response.
Toxicity and treatment delivered
No changes in estradiol, progesterone, testosterone, luteinizing hormone, or follicle stimulating hormone were identified in either study.
Trial 001
2ME2 monotherapy was well tolerated with few patients experiencing Grade 3 or 4 toxicities (Table 2). There was no neutropenia or thrombocytopenia; anemia was limited to patients with extensive prior chemotherapy and/or marrow infiltration. Fatigue was the most commonly reported toxicity; no patient developed increased transaminases or symptoms suggesting significant estrogenic exposure. Non-hematologic toxicity was mild and not clearly associated with dose or duration of 2ME2 therapy. In most cases, toxicity was attributed to the underlying malignancy. Six patients discontinued therapy before completing cycle 1; one patient withdrew consent and five patients experienced rapid disease progression with symptomatic decline. Nine patients received more than 2 cycles of 2ME2 monotherapy (Table 3).
Trial 002
Concurrent docetaxel and 2ME2 was generally well tolerated (Table 2). Transaminase elevations were detected in three patients. Transaminases returned to baseline within 14 days despite continuing 2ME2 and remained normal after resuming a reduced dose (25%) of docetaxel in two patients. Both 2ME2 and docetaxel were held for 14 days in the third patient who had had an allergic reaction to an antibiotic given for an intercurrent illness; grade 3 transaminase elevation recurred despite docetaxel dose reduction prompting discontinuation of protocol therapy. Other toxicities were similar in frequency and severity to those expected from docetaxel monotherapy.
Patients completed a median 5 cycles of combined therapy; 2 patients continued 2ME2 monotherapy for more than one year without progression (Table 3). Eight patients required docetaxel dose reduction; doses were reduced twice in one patient. Reasons for dose reduction included diarrhea (2), hand-foot syndrome (2), increased transaminase (2), peripheral neuropathy (1), neutropenia (1) and pleural effusion (1).
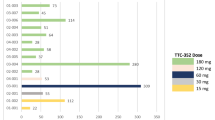
Pharmacokinetics
Pharmacokinetic parameters from Trial 001 are shown in Table 4. There was large interpatient variability with both the daily and every 12 h schedules (data not shown). Terminal half-life was approximately 10 h with daily dosing. No accumulation was detected with daily dosing; slight drug accumulation was detected with every 12 h dosing. 2ME2 concentrations increased with increasing doses through 600 mg/day and 400 mg q12h; no further increase in exposure was obtained with higher doses. 2ME2 is significantly oxidized at the 17 position to 2-methoxyestrone (2ME1). 2ME1 concentrations were approximately 10-fold higher than 2ME2; both 2ME2 and 2ME1 were extensively conjugated to gluronides and sulfates (data not shown).
Docetaxel pharmacokinetic studies were completed in eight patients. 2ME2 did not induce any major alterations in docetaxel clearance, volume of distribution or dose-normalized AUC (Table 5). As in trial 001, there was significant interpatient variability in 2ME2 clearance with extensive metabolism to 2ME1. 2ME2 peak and trough levels were not altered by concurrent docetaxel administration (data not shown).
Pharmacodynamics
Pre-treatment and at least one follow-up sample were available for 22 of 31 patients in Trial 001 and 13 of 15 patients in Trial 002. Plasma VEGF became undetectable in all patients who continued treatment for more than three months in both studies. Baseline serum VCAM-1 was lower in patients with an objective response to combined docetaxel plus 2ME2 than in non-responding patients (372±123 ng/mL vs. 504±221 ng/mL; p < 0.0001); serum VCAM-1 did not correlate with time to progression in patients receiving 2ME2 monotherapy. Urine VEGF, serum MMP-2 and MMP-9 concentrations did not predict time to progression or change consistently with treatment or disease status in either study. Serum and urine bFGF were rarely elevated at baseline; PSA was undetectable in all patients at all timepoints.
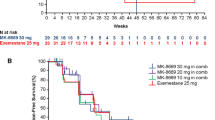
Efficacy
There were no objective responses in Trial 001. One patient who had had four previous chemotherapy regimens experienced a minor response in liver metastases and subsequently progressed after 9 months. Seven patients remained stable for ≥4 months; median time to treatment failure (TTF) was 55 days (range 13–258). Overall response rate in Trial 002 was 20% including one complete response with recalcification of lytic bone lesions; 40% of patients had stable disease. Two patients remained on 2ME2 monotherapy for more than one year without progression. Median TTF was 203 days (range 19–966). There was no obvious correlation between 2ME2 dose and TTF in either study.
Discussion
We report the first phase I study of the naturally occurring antiangiogenic agent 2ME2, alone or in combination with docetaxel. Overall treatment was well tolerated with most toxicities attributed to the underlying malignancy or concurrent docetaxel. Though transient hepatic toxicity has been reported in a minority of men with advanced prostate cancer treated with 2ME2 monotherapy [26], only three patients in our study developed hepatic toxicity—all in combination with docetaxel. The mechanism by which 2ME2 causes or potentiates hepatic toxicity remains unclear. We did not observe any correlation between 2ME2 dose or pharmacokinetic parameters and hepatic toxicity in our patients. Nonetheless, it remains possible that altered 2ME2 metabolism could result in higher systemic exposure to the free drug and its metabolites. Alternatively, patients with a low activity variant of COMT, an enzyme that can revert the metabolism of 2ME2 into 2-hydroxyestradiol, may have higher levels of this metabolite which is known to cause hepatic toxicity in some patients.
As expected based on the preclinical experience, we found no changes in hormone levels in any of our patients but it is important to note that all of our patients were post-menopausal at study entry. Future studies are needed to assess the impact of 2ME2 on hormonal levels in women with intact, functioning ovaries. Similarly, we did not measure sex hormone binding globulin (SHBG), a plasma glycoprotein that binds to certain steroids which was recently shown to increase in hormone refractory prostate cancer patients receiving 2ME2 monotherapy [26].
2ME2 does not directly influence the transcription of any of the angiogenic factors (VEGF, bFGF, VCAM, MMP-2 and MMP-9) we measured [27], thus association with response would be indirect at best. A recent study found significant variability in plasma and urine VEGF levels in the short term in the absence of treatment [28]. Given this variability along with the multiple analyses and modest clinical activity of 2ME2 in our study, the associations we identified can only be viewed as hypotheses to be tested in future studies.
The plasma levels of 2ME2 achieved in our studies were well below that expected for activity based on preclinical models. Nonetheless we saw encouraging signs of activity in some patients. Though there were no objective responses in Trial 001, one patient with liver metastases who had progressed on four prior chemotherapy regimens had a minor response lasting 9 months. While the overall response rate in Trial 002 is similar to that reported in other trials using weekly docetaxel [29–35], the prolonged disease stability experienced by some patients is notable. Two patients continued 2ME2 monotherapy for over a year without progression. One patient with bone metastases had a complete response including recalcification of lytic lesions; she completed 6 cycles of combined therapy and then remained on 2ME2 alone for nearly two and half years before progressing.
In conclusion, 2-methoxyestradiol is well tolerated with evidence of anti-cancer activity in patients with refractory metastatic breast cancer. The maximum tolerated dose was not identified in this study but further dose escalation was abandoned given the pharmacokinetic limitations we encountered. Clearly, improvements in the formulation of 2ME2 to provide greater drug exposure are required. Specifically the oral bioavailability was apparently dissolution-rate limited and resulted in the non-linearity of the pharmacokinetics. Moreover, the extensive conversion to 2ME1 and conjugation resulted in low plasma levels. Reformulation of the drug has improved the bioavailability with increased activity in relevant pharmacokinetic and efficacy models. Phase I evaluation of these new formulations have begun in separate trials at Indiana University and the University of Wisconsin Comprehensive Cancer Center.
References
Folkman J (1990) What is the evidence that tumors are angiogenesis dependent? J Natl Cancer Inst 82:4–6
Gasparini G (1999) Angiogenesis in breast cancer. Role in biology, tumor progression, and prognosis. In: Bowcock A (ed) Breast cancer: Molecular Genetics, Pathogenesis, and Therapeutics. Humana Press Inc, Totowa, NJ, pp 347–371
Brem SS, Gullino PM, Medina D (1977) Angiogenesis: a marker for neoplastic transformation of mammary papillary hyperplasia. Science 195:880–882
Jensen HM, Chen I, DeVault MR et al (1982) Angiogenesis induced by “normal” human breast tissue: a probable marker for precancer. Science 218:293–295
McLeskey SW, Tobias CA, Vezza PR et al (1998) Tumor growth of FGF or VEGF transfected MCF-7 breast carcinoma cells correlates with density of specific microvessels independent of the transfected angiogenic factor. Am J Pathol 153:1993–2006
Weinstat-Saslow DL, Zabrenetzky VS, VanHoutte K et al (1994) Transfection of thrombospondin 1 complementary DNA into a human breast carcinoma cell line reduces primary tumor growth, metastatic potential, and angiogenesis. Cancer Res 54:6504–6511
McCulloch P, Choy A, Martin L (1995) Association between tumour angiogenesis and tumour cell shedding into effluent venous blood during breast cancer surgery [see comments]. Lancet 346:1334–1335
Fox S, Leek R, Bliss J et al (1997) Association of tumor angiogenesis with bone marrow micrometastases in breast cancer patients. J Natl Cancer Inst 89:1044–1049
Weidner N, Semple J, Welch W et al (1991) Tumor angiogenesis and metastasis—correlation in invasive breast cancer. N Engl J Med 324:1–8
Weidner N, Folkman J, Pozza F et al (1992) Tumor angiogenesis: a new significant and independent prognostic indicator in early stage breast carcinoma. J Natl Cancer Inst 84:1875–1887
Hansen S, Grabau D, Sorensen F et al (2000) The prognostic value of angiogenesis by Chalkley counting in a confirmatory study design on 836 breast cancer patients. Clin Cancer Res 6:139–146
Martucci C, Fishman J (1976) Uterine estrogen receptor binding of catecholestrogens and of estetrol (1,3,5(10)-estratriene-3,15a,16a,17b-tetrol). Steroids 27:325–333
Liu D, Bachmann KA (1998) An investigation of the relationship between estrogen, estrogen metabolites and blood cholesterol levels in ovariectomized rats. J Pharmacol Exp Ther 286:561–568
Martucci CP, Fishman J (1979) Impact of continuously administered catechol estrogens on uterine growth and luteinizing hormone secretion. Endocrinology 105:1288–1292
Liehr JG, Fang WF, Sirbasku DA et al (1986) Carcinogenicity of catechol estrogens in Syrian hamsters. J Steroid Biochem 24:353–356
Josefsson E, Tarkowski A (1997) Suppression of type II collagen-induced arthritis by the endogenous estrogen metabolite 2-methoxyestradiol. Arthritis Rheum 40:154–163
Schumacher G, Kataoka M, Roth J et al (1999) Potent antitumor activity of 2-methoxyestradiol in human pancreatic cancer cell lines. Clin Cancer Res 5:493–499
Klauber N, Parangi S, Flynn E et al (1997) Inhibition of angiogenesis and breast cancer in mice by the microtubule inhibitors 2-methoxyestradiol and Taxol. Cancer Res 57:81–86
Fotsis T, Zhang Y, Pepper MS et al (1994) The endogenous oestrogen metabolite 2-methoxyoestradiol inhibits angiogenesis and suppresses tumour growth. Nature 368:237–239
Yue T-L, Wang X, Louden C et al (1997) 2-methoxyestradiol, an endogenous estrogen metabolite, induces apoptosis in endothelial cells and inhibits angiogenesis: possible role for stress-activated protein kinase signaling pathway and fas activation. Molecular Pharmacol 51:951–962
Sweeney CJ, Miller KD, Sissons SE et al (2001) The antiangiogenic property of docetaxel is synergistic with a recombinant humanized monoclonal antibody against vascular endothelial growth factor or 2-Methoxyestradiol but antagonized by endothelial growth factors. Cancer Res 61:3369–3372
Yu H, Levesque MA, Clark GM et al (1998) Prognostic value of prostate-specific antigen for women with breast cancer: a large United States cohort study. Clin Cancer Res 4:1489–1497
Yu H, Levesque MA, Clark GM et al (1999) Enhanced prediction of breast cancer prognosis by evaluating expression of p53 and prostate-specific antigen in combination. Br J Cancer 81:490–495
Fortier AH, Nelson BJ, Grella DK et al (1999) Antiangiogenic activity of prostate-specific antigen. J Natl Cancer Inst 91:1635–1640
Heidtmann HH, Nettelbeck DM, Mingels A et al (1999) Generation of angiostatin-like fragments from plasminogen by prostate- specific antigen. Br J Cancer 81:1269–1273
Sweeney C, Liu G, Yiannoutsos C et al (2005) A phase II multicenter, randomized, double-blind, safety trial assessing the pharmacokinetics, pharmacodynamics, and efficacy of oral 2-methoxyestradiol capsules in hormone-refractory prostate cancer. Clin Cancer Res 11:6625–6633
Mooberry SL (2003) Mechanism of action of 2-methoxyestradiol: new developments. Drug Resist Updat 6:355–361
Miller KD, Trigo JM, Wheeler C et al (2005) A multicenter phase II trial of ZD6474, a vascular endothelial growth factor receptor-2 and epidermal growth factor receptor tyrosine kinase inhibitor, in patients with previously treated metastatic breast cancer. Clin Cancer Res 11:3369–3376
Loeffler T, Droege C, Hausamen T et al (1999) Dose-dense weekly docetaxel in metastatic breast cancer. Breast Cancer Res Treat 57:125
Burstein HJ, Manola J, Younger J et al (2000) Docetaxel administered on a weekly basis for metastatic breast cancer. J Clin Oncol 18:1212–1219
Fornasiero A, Danilel O, Ghiotto C et al (1999) Weekly docetaxel for metastatic breast cancer: A phase II trial. Breast Cancer Res Treat 57:127
Kim Y, Takatsuka Y, Tanigawara Y et al (2000) Weekly docetaxel for patients with recurrent breast cancer: clinical results and pharmacokinetic/pharmacodynamic assessment. Proc Am Soc Clin Oncol 19:113a
Mey U, Kleinschmidt R, Sauerbruch T et al (1999) A phase II trial of weekly docetaxel in patients with advanced metastatic breast cancer - preliminary results. Proc Am Soc Clin Oncol 18:134a
Miranda F, Burris H, Greco F et al (1999) Phase II trial of weekly docetaxel in the treatment of patients who are elderly or medically compromised: A Minnie Pearl Research Network Study. Proc Am Soc Clin Oncol 18:601a
Rittershaus A, Luck H, Scholz U et al (1999) Weekly docetaxel in pretreated patients with metastatic breast cancer. Breast Cancer Res Treat 57:126
Acknowledgments
Supported by the American Cancer Society grant # CRTG-00-199-01-CCE (KDM) a Career Development Award from the American Society of Clinical Oncology (KDM), Breast Cancer Research Foundation (GWS, KDM) and research supported by EntreMed, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
James, J., Murry, D.J., Treston, A.M. et al. Phase I safety, pharmacokinetic and pharmacodynamic studies of 2-methoxyestradiol alone or in combination with docetaxel in patients with locally recurrent or metastatic breast cancer. Invest New Drugs 25, 41–48 (2007). https://doi.org/10.1007/s10637-006-9008-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-006-9008-5