Abstract
Purpose
TTC-352 is a selective human estrogen receptor (ER) partial agonist developed for treatment of hormone-refractory ER + breast cancer.
Methods
This was an accelerated dose escalation study with the primary endpoint of maximum tolerated dose that evaluated five dose levels of TTC-352 in breast cancer progressing after at least two lines of hormonal therapy including one in combination with a CDK4/6 inhibitor. The secondary objectives were to determine treatment tolerability, pharmacokinetics of TTC-352, best response, progression-free survival (PFS), and PKCα expression in tumors.
Results
The study enrolled 15 patients. No dose-limiting toxicity was observed. Patients experienced the following grade 3 toxicities: asymptomatic pulmonary embolism, diarrhea, aspartate transaminase elevation, and myalgia, and one grade 4 toxicity of gamma glutamyltransferase elevation. Pharmacokinetic half-life was 7.6–14.3 h. The intra- and inter-individual variability for AUC0-∞ hampered assessment of the relationship between dose and AUC0-∞. Median PFS was 58 days (95% CI = 28,112). Higher PKCα expression in tumor stroma was associated with a trend toward longer PFS.
Conclusions
TTC-352 demonstrates safety and early clinical evidence of antitumor activity against heavily pretreated hormone-refractory breast cancer. Based upon TTC-352 plasma concentrations and tolerability, the 180 mg twice a day is recommended for further testing.
(ClinicalTrials.gov Identifier: NCT03201913)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Though there has been an increase in the number of patients diagnosed with breast cancer over the past several years, overall outcomes have improved for several reasons, including more effective therapies. However, more than 40,000 patients in the USA die from breast cancer annually. Approximately two-thirds of breast tumors are estrogen receptor positive (ER +) and the use of endocrine therapy has improved outcome for patients with all stages of ER + disease. Unfortunately, endocrine resistance, both de novo and acquired, results in disease recurrence and progression. The addition of CDK 4/6 inhibition to endocrine therapy has led to dramatic improvements in progression-free survival for patients with metastatic hormone receptor positive breast cancer treated in the first-line setting and are now standard of care [1]. Despite the efficacy of endocrine therapy, and the new combinations of AIs and SERD with CDK4/6 inhibitor therapies, all patients with metastatic disease will develop resistance to endocrine therapy ultimately leaving cytotoxic chemotherapy as the only option [2, 3]. Thus, the development of therapeutic alternatives for patients with ER + endocrine-resistant breast cancer is of critical importance. One drug class that has shown efficacy in the tamoxifen and AI-resistant setting is the novel selective estrogen mimics (SEMs) [4].
TTC-352 [3-(4-fluorophenyl)-2-(4-hydroxyphenoxy)benzo[b]thiophen-6-ol] is one of a subset of SEMs, which acts as a selective human ER partial agonist (ShERPA) in ER + cell lines [5]. It is argued and supported by animal studies that a ShERPA that mimics the effects of 17b-estradiol (E2) in endocrine-resistant breast cancer cells and tumors, but is a partial agonist in contrast to the full agonists, E2 and diethylstilbestrol (DES), will have an improved side effect profile. Specifically, ShERPAs did not support the growth of ER + , hormone-dependent cell lines that normally require E2 for growth; nor did they result in significant uterine growth as E2 did in these models [5]. Given these observations, TTC-352 was advanced to drug development for clinical study in patients with endocrine-resistant breast cancer.
Protein kinase C alpha (PKCα) is a member of the serine/threonine kinases and has a role in the transduction of signals for cell proliferation and differentiation [6]. Tumors that develop acquired endocrine resistance, retain ER and show elevated PKCα expression associated with resistance to endocrine therapy [7, 8]. We have previously shown that increased PKCα expression in ER + breast cancer cell lines with acquired resistance to tamoxifen and AI, correlates with growth inhibition and apoptosis in response to E2 [9, 10]. Growth of multiple MCF-7-derived tamoxifen-resistant tumor cell lines was inhibited by E2, and E2 caused complete regression of xenograft tumors [4], which suggested that PKCα may be predictive of benefit from therapeutic intervention by estrogenic compounds.
The primary objective of this study was to determine the maximum tolerated dose (MTD) for TTC-352 in patients with breast cancer progressing on at least two endocrine therapies including in combination with CDK4/6 inhibitor. The secondary objectives were to evaluate treatment tolerability, to establish the pharmacokinetic profile of TTC-352, to assess best response to treatment, and determine progression-free survival (PFS). An exploratory objective was to evaluate PKCα expression in tumors and correlate it with duration of PFS.
Methods
Patients
Enrolled patients had ER + (defined per ASCO-CAP guidelines) metastatic breast cancer and received and experienced disease progression on at least two lines of endocrine therapy, with one that included a CDK4/6 inhibitor, and for which no effective standard therapy other than chemotherapy was available. Patients with HER2-positive cancer where eligible. Main eligibility criteria were as follows: (a) Eastern Cooperative Oncology Group (ECOG) performance status of ≤ 1; (b) No impending visceral crisis that requires chemotherapy; (c) No uncontrolled or symptomatic CNS metastases (d) Adequate hepatic, renal, and hematologic functions; and (e) measurable or evaluable disease. The complete list of inclusion and exclusion criteria can be found in the study protocol in Supplementary Material.
The institutional review board at all participating centers approved the study protocol. All patients provided informed consent before study interventions were initiated.
Treatment plan
TTC-352 was administered as an oral capsule, twice a day. Patients received sequential 28-day cycles of treatment until disease progression, unacceptable toxicity, patient refusal to continue treatment, any other reason to discontinue, or study completion/termination. TTC-352 was supplied in 15 and 60 mg capsules by TTC Oncology, LLC (Edina, MN, USA).
Study design
A total of five incremental dose levels (15, 30, 60, 120, 180 mg twice a day) were planned. The lower level of tested TTC-352 dose range was determined by results of severely toxic rate (10) in rats (the most sensitive species to TTC -352) being 30 mg/kg. The highest tested dose level of TTC-352 exceeded threefold a level where antitumor activity was observed in two tamoxifen-resistant xenograft models. Cycle was defined as 28 days. Rapid escalation (cohort size of 1 patient) continued until a patient experienced toxicity grade 2 (excluding alopecia or diarrhea), after which enrollment proceeded with cohorts of 3 patients.
A dose-limiting toxicity (DLT) was defined as one of the following probably or possibly related to study medication events occurring during the first cycle: (a) Grade 4 thrombocytopenia of any duration or grade 3 thrombocytopenia with clinically significant bleeding; (b) Grade 3 or greater neutropenia with fever of any duration; (c) Grade 3 or greater clinical non-hematological toxicity (excluding ≥ grade 3 nausea, vomiting, or diarrhea without maximal medical intervention and/or prophylaxis); (d) a pause in treatment of more than 3 weeks after the first 28-day cycle of treatment, due to inadequate recovery of any hematologic toxicity considered related, probably related or possibly related to study medication (adequate hematologic toxicity recovery is defined as a total neutrophil count > 1000/mm3 or platelets > 100,000/mm3); (e) inadequate recovery of any non-hematologic toxicity considered related, probably related or possibly related to study medication (adequate non-hematologic toxicity recovery is defined as improvement to ≤ grade 1, unless the patient entered the study with a grade 2 baseline), disease-related toxicity or a grade 2 baseline neuropathy.
The MTD was defined as the dose associated with DLT in less than or equal to 33% of patients. Once MTD was determined, the MTD dose cohort was expanded to enroll a cohort of 10 patients to assure safety. Treatment was continued until disease progression, unacceptable toxicity, or patient refusal.
Evaluation of toxicity and response
The US National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE version 4.03) [11] were used to evaluate symptoms and toxicity assessment on day 1 of each treatment cycle. Appropriate imaging scans, including CT scans, MRI and bone scans, were performed at the time of study enrollment and every 8 weeks from treatment cycle to assess disease status. Standard clinical measures were used to assess malignancy response including RECIST v1.1 in patients with measurable disease [12]. Secondary efficacy endpoints included best response (complete response, partial response, or stable disease) and PFS and OS measured from time of first administration of drug.
Pharmacokinetics
Pharmacokinetics were established for each dose level. The pharmacokinetic profile of TTC-352 was assessed under fasting conditions after the first dose on Day 1 of cycle 1 and after morning administration of the last dose of cycle 1 on Day 28 with evening doses skipped on these days. Blood samples for analysis of TTC-352 plasma concentrations were collected prior to and 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 10, 12, 24 and 28 (day 28 only) hours following oral administration of TTC-352 on days 1 and 28 of cycle 1. Plasma was assayed for TTC-352 utilizing a validated LC/MS–MS method. The lower limit of quantitation was 0.1 ng/ml. The TTC-352 plasma concentration–time data was analyzed by non-compartmental methods (Phoenix WinNonLin® version 8.1, Certara, L.P., Princeton, NJ).
PKCα expression evaluation
PKCα expression level in archived tumor biopsies was determined by immunohistochemistry (IHC) at the University of Illinois at Chicago in the laboratory of Dr Elizabeth L. Wiley. IHC analysis was performed on 5 μM sections of formalin-fixed paraffin embedded tissue with the Ventana Benchmark automated staining platform using the iView DAB detection kit according to company protocol using CC1 Standard antigen retrieval. The PKCα antibody (rabbit polyclonal, Santa Cruz Biotechnology, sc-208) was previously validated [13, 14] and used at a dilution of 1:200 and incubated at 37 °C for 30 min. Frequency and intensity of PKCα staining of all tumor cells on each slide were scored on a scale of 0 to 4 without the assessor’s knowledge of clinical patient data. Frequency of positive staining in less than 1% of tumor cells was scored as 0, 1%–10% as 1, 11% to-35% as 2, 36%–70% as 3, and over 70% as 4. A composite score is also reported based on the Allred scoring system which is a sum of the frequency and intensity scores yielding numerical values from 0 to 8 [15].
Statistical analyses
Descriptive statistics were used to describe response rates. PFS curves were estimated using the Kaplan–Meier method. Chi-square tests were used for testing association between PKCα expression and PFS. All statistical tests were 2-sided tests, controlling for Type I error probability of 0.05.
Results
Patient characteristics
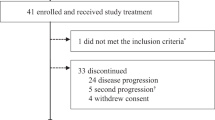
Fifteen patients were enrolled in the trial between January 30, 2018 and June 9, 2019. All patients were females, with median age of 62 (range: 40–77), had ER + metastatic breast cancer, and all had received multiple lines of prior therapy (median 9, range; 2–15) for metastatic disease. One patient had HER2 positive disease. All patients received prior CDK inhibitor therapy and all, but one, had received cytotoxic chemotherapy for metastatic disease. Two-thirds of patients had received prior therapy with a mTOR inhibitor. Prior therapies are listed in Table 1.
Dose escalation
There were 2 patients at the first dose level (15 mg twice a day), because the first patient withdrew from the study at Day 22 of the first cycle due to progression of breast cancer metastasis in liver. Therefore, this patient was replaced. In the following dose levels (Table 1), there was one patient per dose. Since in the highest dose level tested of 180 mg twice a day, there was no DLT and MTD was not reached, this cohort was expanded to enroll 10 patients. A total of 47 treatment cycles were administered during the trial. No DLT was observed at dose level 1, 2, 3, 4 or 5.
Toxicity
Table 2 shows toxicities possibly or probably related to TTC-352. Most common grade 1 and 2 toxicities seen in more than one patient were: diarrhea (87%), hot flashes (27%), abdominal pain (27%), nausea (20%), fatigue (20%), headache (20%), maculopapular rash (20%), dizziness (13%), peripheral neuropathy (13%), vaginal discharge (20%), breast pain (13%), arthralgia (13%),vomiting (13%), QT prolongation (13%), anemia (13%), uterine hemorrhage (13%), and blurred vision (13%). There were four grade 3 toxicities: one of asymptomatic pulmonary embolism, one of diarrhea, one of aspartate transaminase elevation, and one episode of myalgia. There was one grade 4 toxicity of gamma glutamyltransferase elevation. No treatment-related deaths occurred.
Pharmacokinetics
Pharmacokinetics of TTC-352 were examined in 15 patients following administration of a single-oral dose on Day 1 and 12 patients following TTC-352 twice daily for 28 days. Subjects received either 15 mg, 30 mg, 60 mg, 120 mg, or 180 mg twice a day. The day 28 plasma concentration data from two subjects, 02–002 and 03–006, were not included in the pharmacokinetic analysis. Both subjects experienced adverse events at the 180 mg dose, and, as a result, their TTC-352 doses were lowered from 180 to 150 mg on day 28.
Maximum plasma concentrations (Cmax) typically occurred within 5 h after oral administration. The terminal elimination half-life (t1/2-λz) ranged from 7.23 to 10.23 h in the 15 mg—120 mg groups on day 1, 8.84 to 14.31 h in the 180 mg group on day 1, 9.38 to 20.45 h in the 15 mg – 120 mg groups on day 28 and 4.53 to 20.35 h in the 180 mg group on day 28. Dose and single- versus multiple-dose administration had minimal influence on Tmax and t1/2-λz. Oral clearance (CL/F) in the ≤ 60 mg dose group was lower than in the 120 and 180 mg groups on days 1 (medians: 6505 mL/min vs 11,246 mL/min, respectively) and 28 (median: 2766 mL/min vs. 9333 mL/min, respectively). The CL/F on days 1 and 28 were comparable across dose groups.
TTC-352 Cmax in the 180 mg dose cohort ranged from 4.62 to 65.47 ng/mL on day 1 and 25.78 to 93.17 ng/mL on day 28. Area under the plasma concentration–time curve from time 0 to 12 h post-dose (AUC0-12) ranged from 35.8 to 272.4 ng-h/ml on day 1 and 154.9 to 975.7 ng-h/mL on day 28. Similar variability occurred at the lower doses. Assessment of dose proportionality was hampered by the small number of patients at the lower doses, and large inter-patient variability in Cmax, AUC0-12 and area under the plasma concentration–time curve from time 0 to infinity (AUC0-∞).
Prediction by t1/2-λz of accumulation of TTC-352 plasma concentrations with multiple dosing from day 1 to day 28 underestimated the actual extent of accumulation by approximately two-fold, 1.57 versus 2.64 (day 12 to day 1 AUC0-12 ratio). The underestimation of accumulation of TTC-352 plasma concentrations likely represents the failure of t1/2-λz to reflect the influence of absorption or enterohepatic recirculation on the functional half-life of TTC-352.
The pharmacokinetics of orally administered TTC-352 at doses of 15 to 180 mg was characterized by high intra- and inter-individual variability.
Efficacy
Progression of disease was a cause of study treatment discontinuation in 13 (87%) patients. One patient withdrew from the study because of increase in tumor biomarkers (CA 15–3 and CA 27–29), and the other because of gamma glutamyltransferase elevation. Of 15 enrolled, 3 patients were unevaluable for radiologic response due to the following: removed due to toxicity prior to starting cycle 3 (N = 1), clinical progression during cycle 1 (N = 1), clinical progression during cycle 2 (N = 1). The percentage change according to RECIST criteria from baseline was evaluated at the time of best response. There were no complete or partial responses. There were six patients with stable disease, four at 180 mg twice a day dose. Of the 12 evaluable patients, 4 patients had stable disease at 4 months (33%), and 2 patients at 6 months (16% clinical benefit rate (CBR)). Median PFS time was 58 days (95% CI = 28,112). Figure 1 shows duration of therapy for each patient. Figure 2A shows Kaplan–Meier PFS curve for all patients.
PKCα expression evaluation
Table 3 shows PKCα expression in archival tumor tissue. There was no tissue available in two patients, and in one patient tissue was inadequate for analysis. Expression of PKCα in tumor cells did not correlate with PFS (HR 1.179, 95% CI = 0.772, 1.802), p-value = 0.446), whereas expression of PKCα in tumor stroma had a trend towards weak association with better outcome (HR 0.442, 95% CI = 0.164, 1197), p-value = 0.1082) (Fig. 2b).
Discussion
We conducted the first in-human phase 1 study of a novel ShERPA, TTC-352, in patients with ER + metastatic breast cancer previously treated with at least two prior hormonal therapies, one of which was given in combination with a CDK4/6 inhibitor.
The approval of cyclin-dependent kinase CDK4/6 inhibitors in combination with AIs or the SERD, fulvestrant, has transformed the treatment of hormone receptor (HR)-positive, HER2 negative metastatic breast cancer. Pivotal studies of the three approved CDK4/6 inhibitors in combination with an AI or fulvestrant support combination therapy as the preferred therapeutic approach for most patients HR positive, HER2-negative metastatic breast cancer dramatically improving PFS by approximately 50% and improving overall survival in several trials. After disease progression on CDK4/6 inhibition, at present, there are no studies supporting continuation of CDK4/6 inhibitor therapy [16], though this approach is being evaluated in ongoing clinical trials. Following endocrine therapy and CDK inhibition, options for further therapy include mTOR inhibition, or PI3-kinase inhibition in tumors with PI3-kinase mutations, or chemotherapy, but therapeutic resistance ultimately occurs with resultant disease progression [17]. Therefore, with the goal of improving survival while maintaining quality of life, there is a critical need for new therapies for endocrine-resistant metastatic breast cancer.
Although clinical trials have supported the re-emergence of E2 as a possible treatment strategy for patients with endocrine-resistant breast cancer [18], this therapy is associated with the potential for serious side effects such as an increased risk of endometrial cancer and thromboembolic events, which has deterred the clinical community from adopting it as a treatment strategy. Prior to the introduction of tamoxifen, high-dose estrogen (HDE) and DES were used to treat metastatic breast cancer in the 1960s and 1970s [19]. Randomized trials compared tamoxifen to HDE/DES and found similar or slightly inferior efficacy, but better tolerability with tamoxifen [20, 21]. More recently, the preclinical evidence for the switch from E2 promoting growth in breast epithelial cells to causing growth inhibition was observed in both cell lines and xenograft models and is often described as the cyclical response to estradiol [22]. This laboratory observation was later validated coincidentally in the Women’s Health Initiative study reporting that women treated with conjugated equine estrogens (CEE) post-hysterectomy had reduced risk of breast cancer incidence and mortality [23]. Later, Ellis et al. addressed the tolerability issue by comparing low-dose estrogen versus HDE in patients with resistance to AIs and discovered that the lower dose provided a similar clinical benefit as HDE but with fewer side effects [18]. Another report by Zucchini et al. showed similar clinical benefit with low-dose E2 valerate [24]. A recent review of clinical data suggests that HDE should be considered a valuable alternative to chemotherapy in selected patients [25].
The premise for development of a ShERPA is to preserve the antitumoral activity of E2, but with less toxicity due to partial agonist activity [5]. TTC-352 was selected for its activity in tamoxifen-resistant cell lines and efficacy in inducing tumor regression, comparable to E2, in PKCα- overexpressing and other tamoxifen-resistant xenografts. While endometrial thickening was seen in estradiol-treated animals, none was seen in TTC-352-treated animals [4, 5].
In this first in-human clinical trial with TTC-352, no DLT was observed, and only 4 events of grade 3 toxicity were observed: asymptomatic pulmonary embolus discovered incidentally on restaging computed tomography, diarrhea, increase in aspartate transaminase level, myalgia, and one grade 4 toxicity of gamma glutamyltransferase elevation (7% each). This is in contrast to the known toxicity of E2, which is associated with nausea and vomiting, hyponatremia, pleural effusions, pain, serious infections, and thromboembolism [18]. In summary, TTC-352 use was associated with mild toxicity and compared favorably to that of E2, making it an attractive agent for further use in endocrine-resistant ER + breast cancer.
Pharmacokinetics of TTC-352 demonstrated variability and multiple peaking of TTC-352 plasma concentrations across dose cohorts following single and multiple doses. Enterohepatic recycling of TTC-352 may explain the large variability in TTC-352 pharmacokinetics, multiple peaking, and failure of t1/2-λz to predict accumulation and fluctuation of plasma concentrations with multiple dosing [26,27,28].
Therapy following hormonal therapy and CDK inhibition failure has limited benefit in the majority of patients. Analysis of outcomes of subsequent therapies after progression following palbociclib or to palbociclib and endocrine therapy in the randomized TREnd trial revealed that overall time-to-treatment failure (TTF) was only 3.8 months (95% CI = 3.5, 4.8). In addition, TTF was similar in patients receiving subsequent hormonal therapy (3.7 months (95% CI = 2.8, 4.8)) or chemotherapy (4.6 months (95% CI = 3.5, 5.8)) [29]. In this context preliminary data from our phase 1 study with median PFS of 58 days across all dose levels in more heavily treated patients than in the TREnd study is encouraging. Especially intriguing is the fact that there were two patients in our study with disease control of more than 6 months (280 and 309 days). Both patients had more than 3 lines of prior therapy, including prior SERD and chemotherapy. One patient had received prior tamoxifen, anastrozole, letrozole with palbociclib, exemestane and everolimus, and multiple chemotherapy regimens. The second patient had prior therapy with tamoxifen, letrozole with everolimus, fulvestrant with palbociclib, fulvestrant with capecitabine, fulvestrant with abemaciclib, megestrol acetate, anastrozole, exemestane, then several lines of chemotherapy with vinorelbine, then paclitaxel, and a single agent capecitabine. Both women had performance status of 0, one of them had breast cancer with mutation in the ESR1 gene (D538G) and bone metastases only disease (Table 4). Tumor genomic testing was not mandated and results where available are presented in Table 4.
Activation of PKCα is associated with endocrine-resistance and tumor aggressiveness in the clinic [7, 8]. Tonetti et al. found that lack of responsiveness to tamoxifen was associated with upregulation of PKCα signaling [4, 10, 13, 30]. TTC-352 was designed to induce an inhibitory effect in PKCα-expressing breast cancer models [3, 4]. Therefore, we hypothesized that expression of PKCα in tumor tissue would be predictive of benefit from TTC-352. We collected archived diagnostic breast cancer tissue from patients participating in this study and correlated PKCα with PFS. Although the study sample was small (only 11 tissue samples were available and adequate for analysis), expression of PKCα in tumor stroma appeared to be associated with a longer PFS. While stromal expression of PKCα was unexpected based on our preclinical findings, PKCβ expression was reported in the tumor microenvironment in a breast cancer cohort suggesting linkage to tumorigenesis [31]. Further, there is evidence of stromal PKCα expression in the Human Protein Atlas https://www.proteinatlas.org/ [32]. Given the small size of the study sample, it is necessary to further examine PKCα expression and localization in future studies to determine whether this biomarker can guide patient selection for TTC-352 therapy.
Conclusions
In summary, this phase 1 trial established the dose of TTC-352 for future testing in phase 2 studies. TTC-352 has a favorable toxicity profile and an encouraging signal of efficacy in breast cancer refractory to at least two prior hormonal therapies and CDK4/6 inhibitor. Next steps include defining the role of PKC-α expression in tumor stroma as a predictive biomarker and validation of its efficacy in a phase 2 clinical trial in patients with ER + breast cancer who have been less heavily pretreated.
Data availability
For the data supporting the presented results please contact the corresponding author. Supplementary information is available at the British Journal of Cancer’s website.
Abbreviations
- AI:
-
Aromatase inhibitors
- CEE:
-
Conjugated equine estrogens
- Cmax :
-
Maximum plasma concentration
- CTCAE:
-
Cancer Institute Common Terminology Criteria for Adverse Events
- DES:
-
Diethylstilbestrol
- DLT:
-
Dose-limiting toxicity
- E2:
-
17β-Estradiol
- ECOG:
-
Eastern Cooperative Oncology Group
- ER:
-
Estrogen receptor
- ER + :
-
Estrogen receptor positive
- HER2-:
-
Human epidermal growth factor receptor 2 negative
- HDE:
-
High-dose estrogens
- IHC:
-
Immunohistochemistry
- MTD:
-
Maximum tolerated dose
- PFS:
-
Progression-free survival
- PI3K:
-
Phosphoinositide-3-kinase
- PKCα:
-
Protein kinase C alpha SEMs
- SEMs:
-
Selective estrogen mimics
- ShERPA:
-
Selective human ER partial agonist
- SRERD:
-
Selective estrogen receptor downregulator
- t1/2-λz :
-
Terminal half-life
- TTF:
-
Time-to-treatment failure
References
Messina C, Cattrini C, Buzzatti G, Cerbone L, Zanardi E, Messina M, Boccardo F (2018) CDK4/6 inhibitors in advanced hormone receptor-positive/HER2-negative breast cancer: a systematic review and meta-analysis of randomized trials. Breast Cancer Res Treat 172(1):9–21
Li J, Wang Z, Shao Z (2019) Fulvestrant in the treatment of hormone receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer: A review. Cancer Med 8(5):1943–1957
Iorfida M, Mazza M, Munzone E (2020) Fulvestrant in Combination with CDK4/6 Inhibitors for HER2- Metastatic Breast Cancers: Current Perspectives. Breast Cancer (Dove Med Press) 12:45–56
Molloy ME, White BE, Gherezghiher T, Michalsen BT, Xiong R, Patel H, Zhao H, Maximov PY, Jordan VC, Thatcher GR et al (2014) Novel selective estrogen mimics for the treatment of tamoxifen-resistant breast cancer. Mol Cancer Ther 13(11):2515–2526
Xiong R, Patel HK, Gutgesell LM, Zhao J, Delgado-Rivera L, Pham TND, Zhao H, Carlson K, Martin T, Katzenellenbogen JA et al (2016) Selective Human Estrogen Receptor Partial Agonists (ShERPAs) for Tamoxifen-Resistant Breast Cancer. J Med Chem 59(1):219–237
Mackay HJ, Twelves CJ (2003) Protein kinase C: a target for anticancer drugs? Endocr Relat Cancer 10(3):389–396
Assender JW, Gee JM, Lewis I, Ellis IO, Robertson JF, Nicholson RI (2007) Protein kinase C isoform expression as a predictor of disease outcome on endocrine therapy in breast cancer. J Clin Pathol 60(11):1216–1221
Lonne GK, Cornmark L, Zahirovic IO, Landberg G, Jirstrom K, Larsson C (2010) PKCalpha expression is a marker for breast cancer aggressiveness. Mol Cancer 9:76
Yao K, Lee ES, Bentrem DJ, England G, Schafer JI, O'Regan RM, Jordan VC (2000) Antitumor action of physiological estradiol on tamoxifen-stimulated breast tumors grown in athymic mice. Clin Cancer Res 6(5):2028–2036
Chisamore MJ, Ahmed Y, Bentrem DJ, Jordan VC, Tonetti DA (2001) Novel antitumor effect of estradiol in athymic mice injected with a T47D breast cancer cell line overexpressing protein kinase Calpha. Clin Cancer Res 7(10):3156–3165
Services USDoHaH: Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0 https://www.evsncinihgov/ftp1/CTCAE/CTCAE_403 June 14, 2010.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247
Tonetti DA, Morrow M, Kidwai N, Gupta A, Badve S (2003) Elevated protein kinase C alpha expression may be predictive of tamoxifen treatment failure. Br J Cancer 88(9):1400–1402
Tonetti DA, Gao W, Escarzaga D, Walters K, Szafran A, Coon JS (2012) PKCalpha and ERbeta Are Associated with Triple-Negative Breast Cancers in African American and Caucasian Patients. Int J Breast Cancer 2012:740353
Allred DC, Clark GM, Elledge R, Fuqua SA, Brown RW, Chamness GC, Osborne CK, McGuire WL (1993) Association of p53 protein expression with tumor cell proliferation rate and clinical outcome in node-negative breast cancer. J Natl Cancer Inst 85(3):200–206
Spring LM, Wander SA, Andre F, Moy B, Turner NC, Bardia A (2020) Cyclin-dependent kinase 4 and 6 inhibitors for hormone receptor-positive breast cancer: past, present, and future. Lancet 395(10226):817–827
Costa C, Wang Y, Ly A, Hosono Y, Murchie E, Walmsley CS, Huynh T, Healy C, Peterson R, Yanase S et al (2020) PTEN Loss Mediates Clinical Cross-Resistance to CDK4/6 and PI3Kalpha Inhibitors in Breast Cancer. Cancer Discov 10(1):72–85
Ellis MJ, Gao F, Dehdashti F, Jeffe DB, Marcom PK, Carey LA, Dickler MN, Silverman P, Fleming GF, Kommareddy A et al (2009) Lower-dose vs high-dose oral estradiol therapy of hormone receptor-positive, aromatase inhibitor-resistant advanced breast cancer: a phase 2 randomized study. JAMA 302(7):774–780
Ingle JN (2002) Estrogen as therapy for breast cancer. Breast Cancer Res 4(4):133–136
Peethambaram PP, Ingle JN, Suman VJ, Hartmann LC, Loprinzi CL (1999) Randomized trial of diethylstilbestrol vs. tamoxifen in postmenopausal women with metastatic breast cancer. An updated analysis. Breast Cancer Res Treat 54(2):117–122
Matelski H, Greene R, Huberman M, Lokich J, Zipoli T (1985) Randomized trial of estrogen vs tamoxifen therapy for advanced breast cancer. Am J Clin Oncol 8(2):128–133
Jordan VC (2015) The new biology of estrogen-induced apoptosis applied to treat and prevent breast cancer. Endocr Relat Cancer 22(1):R1–31
Chlebowski RT, Aragaki AK, Anderson GL (2015) Menopausal Hormone Therapy Influence on Breast Cancer Outcomes in the Women's Health Initiative. J Natl Compr Canc Netw 13(7):917–924
Zucchini G, Armstrong AC, Wardley AM, Wilson G, Misra V, Seif M, Ryder WD, Cope J, Blowers E, Howell A et al (2015) A phase II trial of low-dose estradiol in postmenopausal women with advanced breast cancer and acquired resistance to aromatase inhibition. Eur J Cancer 51(18):2725–2731
Coelingh Bennink HJ, Verhoeven C, Dutman AE, Thijssen J (2017) The use of high-dose estrogens for the treatment of breast cancer. Maturitas 95:11–23
Roberts MS, Magnusson BM, Burczynski FJ, Weiss M (2002) Enterohepatic circulation: physiological, pharmacokinetic and clinical implications. Clin Pharmacokinet 41(10):751–790
Davies NM, Takemoto JK, Brocks DR, Yanez JA (2010) Multiple peaking phenomena in pharmacokinetic disposition. Clin Pharmacokinet 49(6):351–377
Ogungbenro K, Pertinez H, Aarons L (2015) Empirical and semi-mechanistic modelling of double-peaked pharmacokinetic profile phenomenon due to gastric emptying. AAPS J 17(1):227–236
Rossi L, Biagioni C, McCartney A, Migliaccio I, Curigliano G, Sanna G, Moretti E, Minisini AM, Cinieri S, Tondini C et al (2019) Clinical outcomes after palbociclib with or without endocrine therapy in postmenopausal women with hormone receptor positive and HER2-negative metastatic breast cancer enrolled in the TREnd trial. Breast Cancer Res 21(1):71
Lin X, Yu Y, Zhao H, Zhang Y, Manela J, Tonetti DA (2006) Overexpression of PKCalpha is required to impart estradiol inhibition and tamoxifen-resistance in a T47D human breast cancer tumor model. Carcinogenesis 27(8):1538–1546
Wallace JA, Pitarresi JR, Sharma N, Palettas M, Cuitino MC, Sizemore ST, Yu L, Sanderlin A, Rosol TJ, Mehta KD et al (2014) Protein kinase C Beta in the tumor microenvironment promotes mammary tumorigenesis. Front Oncol 4:87
Ponten F, Jirstrom K, Uhlen M (2008) The Human Protein Atlas–a tool for pathology. J Pathol 216(4):387–393
Acknowledgements
We are thankful to James P. Zacny, PhD for his editorial support with the clinical protocol and manuscript.
Funding
We acknowledge funding from TTC Oncology, LLC, and the Engdahl Family Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
AZD serves as Chief Medical Officer and obtained honoraria from TTC Oncology and Vanquish Oncology. AZD has received honoraria for consulting work from EMD Serono. AZD has equity in TTC Oncology, IGF Oncology, Squarex, and Martell Diagnostic Laboratories. AZD reports research funding to institutions from Merck, and Eli Lilly. DAT and GRJT have equity in TTC Oncology. RPV has received honoraria from TTC Oncology. RMO serves as an advisor for Lilly, PUMA, Novartis, Genomic Health and Biotheranostics and receives grant support from PUMA, Novartis, Seattle Genetics, and Eisai. All other authors declare no competing interests.
Ethical approval
This clinical trial was approved by the Institutional Review Board at the participating institutions. It was conducted in accordance with the Declaration of Helsinki.
Informed consent
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dudek, A.Z., Liu, L.C., Fischer, J.H. et al. Phase 1 study of TTC-352 in patients with metastatic breast cancer progressing on endocrine and CDK4/6 inhibitor therapy. Breast Cancer Res Treat 183, 617–627 (2020). https://doi.org/10.1007/s10549-020-05787-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05787-z