Abstract
The diversity of probiotic products makes choosing an appropriate probiotic challenging. One unanswered question is whether single-strain probiotics are more effective than multi-strain mixtures. The aim of this review is to account for both disease and strain specificity to determine whether single strains or multiple strains are equivalent or more effective. This literature review of randomized controlled trials from 1973 to 2019 was used to compare the pooled efficacy of trials with a single strain versus the probiotic mixture with same matched strain within the same type of disease indication. A total of 65 RCTs were included (41 with single strains, 22 multi-strain mixtures and 2 comparing single strain to mixture arms) for eight different disease indications (N = 10,863). Only three strains (L. rhamnosus GG, L. helveticus R52 and B. lactis Bb12) had corresponding trials with matching mixtures. Use of L. rhamnosus GG only was significantly more protective for necrotizing enterocolitis compared to two mixtures also containing different strains of B. lactis. The mixture of L. rhamnosus GG and B. lactis Bb12 was significantly more effective than L. rhamnosus GG alone for the eradication of H. pylori. In most cases, single strains were equivalent to mixtures. Choice of an appropriate probiotic should be based, not on the number of strains in the product, rather based on evidence-based trials of efficacy. In most cases, multi-strain mixtures were not significantly more effective than single-strain probiotics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Probiotics are a well-studied mode of therapy but not everything is known about how they work and when they are most effective. In addition, regulatory requirements differ by country as probiotics may be available as dietary supplements (not requiring efficacy trials) or as medications (requiring efficacy and safety trials). The choice of when to use specific probiotics is an evolving field. Recent publications have demonstrated both strain and disease specificity for both the prevention and treatment of various diseases [1, 2]. Linking specific probiotic strains based on randomized controlled trials to specific disease indications has become easier due to published practical guidelines, but some recurrent questions are asked by patients and physicians.
One basic question is whether single-strain probiotics or multi-strain probiotic mixtures are better or equivalent for efficacy. Although many single-strain probiotics have evidence-based efficacy, it has been postulated since the intestinal microbiome is complex and contains > 400 species, the use of multiple strains might be more beneficial to restore the microbiome after dysbiosis has occurred. Advantages of multi-strain mixtures may include synergistic effects of different strains in the mixture (increased adhesion, increased pathogen inhibition) [3, 4]. Different strains may also have different mechanisms of actions and thus provide a wider coverage [5, 6]. For example, B.longum W11 increases the production of T-helper cells, whereas B. longum NCIMB8809 does not [5]. A disadvantage of multi-strain mixtures may be reduced efficacy due to antagonistic intra-strain inhibition by different probiotic strains [7]. Fredua-Agyeman et al. [8] tested the four individual strains found in a multi-strain mixture (L.plantarum 30173, L. rhamnosus 30174, L. acidophilus 30175, Enterococcus faecium 30176, ‘Symprove®’). Two of the four single strains (L. plantarum 30173 and L. rhamnosus 30174) showed antagonism against the other two strains in the mixture, while no inhibition was found by the other two strains. Another study did not find any intra-strain antagonism between the four strains in a mixture of two lactobacilli strains and two bifidobacterial strains [9].
Two reviews of the literature failed to reach a strong conclusion on this issue citing the lack of studies using the same strains comparing single strain versus multi-strain mixtures as the major reason [10, 11]. Several meta-analyses also attempted to determine whether single strain or multi-strain mixtures are more effective, with most analyses not finding a significant difference, but these meta-analyses pooled different strains of probiotics into either single strain or multiple strain groups and did not account for strain specificity, thus the issue remains unresolved [12,13,14].
The aim of this paper is to compare the efficacy of single-strained probiotics to corresponding multi-strained mixtures that include at least one identical single strain, while controlling for disease and strain specificities.
Materials and Methods
As few randomized controlled trials directly compare a single strain to another study arm with a mixture of additional strains, an alternative analytic approach was used. The analysis comprised four steps: (1) literature search of randomized controlled efficacy trials (RCTs) using probiotics, (2) matching of trials within the same disease indication linking single-strain probiotic trials to those with a probiotic mixture containing the identical single strain, (3) pooling outcomes measures from the matched trials using meta-analysis and (4) comparing the pooled efficacy of trials with a single strain versus the probiotic mixture with same matched strain.
Literature Search
Standard Preferred Reporting Items for Systematic reviews and Meta-analysis (PRISMA) guidelines were used for this review (Supplemental Table 1) [15]. PubMed, Google Scholar and NIH registry of clinical trials (www.clinicaltrials.gov) were searched from database inception to December 2019, unrestricted by language or year of publication. Search strategy was as follows: (“probiotics” [MeSH Terms] OR “probiotics” [All Fields]) AND “randomized controlled trials” [MeSH Terms] OR “randomized controlled trials” [All Fields] AND “controlled trials”). Additional searches were done using search terms: bacillus or bifidobacterium or escherichia or enterococcus or lactobacillus or saccharomyces or probiotic mixtures or VSL#3. Secondary searches of grey literature included reference lists, authors, reviews, meeting abstracts websites and clinicaltrials.gov for unpublished trials. A recursive search was also performed, using the bibliographies of all obtained articles. There were no language restrictions. In addition, an open-access database of randomized controlled trials of probiotics was utilized [1] and data were drawn from previously published meta-analyses [16,17,18,19,20,21,22,23].
Inclusion and Exclusion Criteria
Inclusion criteria included randomized, controlled clinical trials with adult or pediatric patients testing probiotics fulfilling the standard definition (must be living microbe, of adequate dose and having efficacy for a health effect) [24].As the efficacy of probiotics is disease and strain-specific, as well as mode-specific (prevention or treatment) [25], inclusion of studies into this review was limited to probiotics that had efficacy trials with at least one trial using a single strain and at least one RCT of a multi-strain mixture containing at least one matching single strain. Single-strain probiotics that have not been incorporated into multi-strain mixtures were not included. Multi-strain mixtures that had no corresponding efficacy trials from at least one single strain in the mixture were also excluded. Most trials provided genus and species for probiotics being tested, but if no strain designation could be determined, a search of the product’s website, communication with authors or other manufacturing data were sought to determine the strain designation. As taxonomic classifications of bacteria may shift with updated recommendations, the most current strain designation was assigned to historical taxonomy when appropriate [25]. If no stain designation could be determined, these were excluded. Other exclusion criteria included non-human studies, early phase 1 or 2 safety or mechanism of action studies, no control group, probiotic not well described, reviews and duplicate reports. Cross-over trials were excluded due to the potential for effect carry-over after short wash-out periods used in these trials.
Statistical Methods
Meta-analyses were conducted separately for each type and mode (prevention or treatment) of disease indication; then, sub-groups of single probiotic strains that had at least one RCT with a sub-group of mixtures containing the matched single strain as one of the strain components were used. Statistical analysis and generation of forest plots of pooled summary estimates was performed using Stata software version 16 (Stata Corporation, College Station, Texas) with meta-analysis modules [26].Differences in mean daily doses and duration were tested using Student’s t test [26]. Publication bias was assessed using the Egger’s test [26]. Heterogeneity was evaluated using I2 statistic (which indicates the proportion of total variability attributed to heterogeneity) [27]. If significant heterogeneity was found (I2 > 50%), a random effects model was employed, otherwise fixed-effects models were used. Summary estimates were based on the pooled data from RCTs using the same type (species) of probiotic and sharing a common outcome measure. Dichotomous outcomes were assessed using relative risks (RR) and 95% confidence intervals (CI) and continuous outcomes were assessing using standard mean difference (SMD) and 95% CI using standard methods [15]. Risk of bias was assessed using standard methods, but as inclusion was restricted to RCTs, all included studies had low risk of bias [27].
The efficacy of a single-strain probiotic was compared to matched multi-strained mixtures with the single-strain component and was assessed using tests of interactions from ratios of relative risks (RRR) and 95% confidence intervals (CI) using Z-scores [28] or meta-regression was used for standardized mean differences [26]. Data on patient characteristics, probiotic dose, duration data and individual study quality assessment have been previously published and were not included in this systematic review.
Results
Literature Review
A total of 2644 abstracts were initially reviewed (Supplemental Figure 1) and 1751 non-RCT studies were excluded. Of the 893 probiotic trials, 549/893 (62%) used single-strain probiotics and 344 (38%) trials used multi-strained probiotic mixtures. From the literature review, there were 259 different types of probiotic products tested in RCTs, among which 109 were single-strain probiotics. The four most common single-strain probiotics included Saccharomyces boulardii CNCM I-745 (109 RCTs), L. rhamnosus GG (99 RCTs), L. reuteri DSM17938 (22 RCTs) and Bifidobacterium animalis lactis Bb12 (18 RCTs). Of the 150 types of multi-strained probiotic mixtures, the three most common mixtures included Lacidofil® (L.helveticus R52 and L. rhamnosus R11, 24 RCTs), VSL#3® (Bifido. breve DSM24732, Bifido. longum DSM24736, Bifido. infantis DSM24737, L. acidophilus DSM24735, L. plantarum DSM24730, L. paracasei DSM24733, L. delbruckiisubsp. bulgaricus DSM24734, Strept. thermophilus DSM24731, 20 RCTs) and a two-strain mixture (L. acidophilus La5 and B. lactis Bb12,16 RCTs).
However, most multi-strained mixtures (140/150, 93%) did not have trials with a corresponding identical single strain, but ten different multi-strained mixtures had ≥ 1 matching RCT with at least one single strain contained in the mixture (a total of 24 RCTs). Some of the common types of probiotics (L. reuteri DSM17938, L. acidophilus, L. plantarum 299v and S.boulardii CNCM I-745) could not be matched with any mixtures that contained the same single-strain type and were excluded. Similarly, the most common multi-strain mixtures did not have corresponding trials with any of the single strains contained in the mixture and were thus excluded. Only three single-strained probiotics (Bifidobacterium lactis Bb12, Lactobacillus rhamnosus GG, Lactobacillus helveticus R52) had RCTs with matching multi-strained mixtures within the same disease indication.
Of the 893 RCTs, 51 of the 59 disease indications could not be included, as there were no matching RCTs with a single strain and mixtures with the corresponding strain within the same disease indication, leaving eight disease indications (total of 81 RCTs). Within the eight disease indications, an additional 16 RCTs were excluded as they did not share common outcome measures with the other RCTs within the same disease indication. For example, the most common outcome measure for IBS was number of ‘Responders’ (IBS symptom resolution), but one RCT only measured change in quality of life scores and, as a consequence, was excluded. The eight disease indications included treatment of atopic dermatitis/eczema, prevention of atopic dermatitis/allergy, prevention of antibiotic-associated diarrhea (AAD), eradication of H. pylori, treatment of irritable bowel syndrome (IBS), prevention of necrotizing enterocolitis (NEC), maintenance of neonatal general wellness and prevention of upper respiratory tract infections (URTI).
A total of 65 RCTs from the eight disease indications were included (41 single-strain trials, 22 multi-strain mixtures and two RCTs comparing the same single strain to a matched multi-strain mixture), including a total N = 10,863 patients [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93]. The probiotic interventions were found to vary by dose (ranging from 108 to 1011/day), duration given (ranging from 1 week to 1 year) and country (Supplementary Table 2). Six RCTs provided two different disease indication outcomes (prevention of AAD and eradication of H. pylori), as shown in Supplementary Table 3 [34, 35, 37, 39, 41, 44]. Only two studies included a study arm with a single strain directly comparing a matching mixture in another study arm [29, 30].
Disease-Specific Meta-Analyses
The first step in assessing probiotic efficacy required RCTs to be grouped first by disease indication, then by strain-specific sub-groups with single strains and matching multi-strained mixture subgroups (Supplementary Tables 2–3). The second step compared the pooled estimates (RR or SMD) of single strains to those of the different mixtures (Table 1) to determine whether they were quantitatively different.
Prevention of Antibiotic-Associated Diarrhea (AAD)
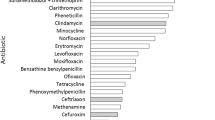
As shown in Fig. 1 and in Supplementary Table 3, 22 eligible RCTs were found for the prevention of AAD [31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52]. Trials with two single strains (L. rhamnosus GG or L.helveticus R52) had matching trials using one of the two strains in their mixtures. The pooled estimate from 10 RCTs using L. rhamnosus GG alone (RR = 0.48, 95% CI 0.27, 0.86) indicated a significant protective efficacy for the prevention of AAD by this single strain. When another strain (B. lactis Bb12) was added, the two-strained mixture was also significantly protective (RR = 0.22, 95% CI 0.12, 0.39). Another mixture containing L. rhamnosus GG, B. lactis Bb12 and L. acidophilus La5 was also found to significantly reduce AAD (RR = 0.17, 95% CI 0.05, 0.64), while a four-strain mixture was not effective (RR = 2.1, 95% CI 0.42, 10.3). The mean daily dose in the ten trials using L. rhamnosus GG alone (4 ± 6 × 1010/d) was similar to dose of L. rhamnosus GG in mixtures from the four trials (9 ± 8 × 1010/d, p = 0.4). The duration of probiotic (1–2 weeks) was also similar for single- and multi-strained mixtures, p = 0.2 (Supplemental Table 2). Eight RCTs were found using L. helveticus R52, with one study finding a significant reduction in AAD when the strain was used by itself (RR = 0.20, 95% CI 0.05, 0.83). Six RCTs with a two-strain mixture of L. helveticus R52 and L. rhamnosus R11 were also protective (RR = 0.44, 95% CI 0.24, 0.79). However, when two additional strains were added to the mixture (B. longum R175 and S. cerevisiae boulardii CNCM I-1079), the efficacy was not significant (RR = 0.29, 95% CI 0.03, 2.69). The mean daily dose in the one trial using L. helveticus R52 alone (2 × 109/d) was higher compared to doses of L. helveticus R52 when in mixtures in six trials (5 ± 7 × 108/d), as only 5% of the mixture was composed of L. helveticus R52. The duration of probiotic (1–4 weeks) was also similar for single- and multi-strained mixtures (Supplemental Table 2). As shown in Table 1, none of the five mixtures were significantly more effective than use of the single probiotic strains (L. rhamnosus GG or L. helveticus R52) used alone. There was no significant publication bias (Egger p = 0.23).
Forest plot of 22 probiotic randomized controlled trials for prevention of antibiotic-associated diarrhea. B bifidobacterium, L. lactobacillus, RR relative risk, 95% CI 95% confidence interval. Strain designations: BlBb12, B. animalis spp. lactis Bb12; BbBb99, B. breve Bb99 (DSM 13692); Bl175, B. longum R175; L. helveticus R52; LrGG, L. rhamnosus GG (ATCC 53103); LrR11, L. rhamnosus R11; Profreud, Propionibacterium freudenrechii ssp. shermanii JS (DSM7076); Sc1079, S. cerevisiae CNCM I-1079
Treatment of Atopic Dermatitis/Eczema
Seven RCTs were found using L. rhamnosus GG alone or as a mixture (L. rhamnosus GG, L. rhamnosus LC705, B. breve Bb99 and Propionibacterium freudenreichii shermanii JC) [29, 53,54,55,56,57].The mean daily dose in the six trials using L. rhamnosus GG alone (2 ± 1 × 1010/d) was similar to the one treatment arm that included L. rhamnosus GG in the mixture (1 × 1010/d). Neither the duration of probiotic given nor the country was significantly different for single versus mixtures (Supplemental Table 2). Pooled outcome data (Supplemental Figure 2) found neither the use of the single L. rhamnosus GG strain (RR = 0.18, 95% CI − 0.24, 0.59) nor the four-strain mixture (RR = 0.23, 95% CI − 0.09, 0.55) was significantly effective for the treatment of atopic dermatitis (t = − 0.08, p = 0.94 from meta-regression models). There was no significant publication bias (Egger’s p = 0.79).
Prevention of Atopic Dermatitis/Allergy
Seven RCTs were found using L. rhamnosus GG alone (4 RCTs) or included into a multi-strain mixture (3 RCTs) with varying results (Supplementary Table 3) [58,59,60,61,62,63,64]. The mean daily dose in the four trials using L. rhamnosus GG alone was similar (2 ± 0.5 × 1010/d, p = 0.1) to the mean dose used in three trials that included L. rhamnosus GG in their mixture (4 ± 2x 1010/d). The duration of probiotic (mean 4 months) was similar in both single- and multi-strained mixtures (Supplemental Table 2). Meta-analysis (Supplemental Figure 3) found L. rhamnosus GG by itself did not significantly reduce atopic dermatitis or pollen allergy (RR = 0.90, 95% CI 0.58, 1.39). Two mixtures were able to significantly reduce the incidence of atopic dermatitis: L. rhamnosus GG, L. rhamnosus LC705, B. breve Bb99, Prop. Freudenreichii shermanii JC (RR = 0.70, 95% CI 0.51, 0.96) and L. rhamnosus GG, L. acidophilus La5 and B. lactis Bb12 (RR = 0.62, 95% CI 0.46, 0.82). However, neither mixtures were significantly more protective compared to the single probiotic strain (Table 1). There was no significant publication bias (Egger p = 0.14).
Eradication of H. pylori
Probiotics have been added to standard eradication treatments in an effort to either increase compliance (which may indirectly improve cure rates) or as a direct mechanism to clear the pathogen, as some probiotics interfere with the attachment of H. pylori [19, 20]. Six RCTs were found using L. rhamnosus alone (4 RCT) or a two-strain mixture (L. rhamnosus GG, B. lactis Bb12) and a four-strain mixture (L. rhamnosus GG, L. rhamnosus LC705, B. breve Bb99 and Prop. Freudenreichii shermanii JC) [34, 35, 37, 39, 41, 44]. No significant efficacy was found for the single strain alone (RR = 1.02, 95% CI 0.90, 1.15) or the four-strain mixture (RR = 1.15, 95% CI 0.91, 1.47), but the two-strain mixture had a significant cure rate for H. pylori (RR = 1.20, 95% CI 1.11, 1.30), as shown in Fig. 2. The mean daily dose in the four trials using L. rhamnosus GG alone (7 ± 4 × 109/d) was similar to the dose of L. rhamnosus GG in mixtures in two trials (4 ± 4 × 109/d, p = 0.5). The duration of probiotic (1–4 weeks) was also similar for single- and multi-strained mixtures (Supplemental Table 2). The mixture containing L. rhamnosus GG and B. lactis Bb12 was significantly better than the single strain of L. rhamnosus GG alone (RRR = 0.85, 95% CI 0.73, 0.98). There was significant publication bias found for this indication (Egger p = 0.01).
Forest plot of probiotic randomized controlled trials for eradication of H. pylori. Outcome is eradication rate. Strain designations of mixtures: BlBb12, B. animalis spp. lactis Bb12; BbBb99, B. breve Bb99 (DSM 13692); Lr705, L. rhamnosus LC705 (DSM 7061); LrGG, L. rhamnosus GG (ATCC 53103); Profreud, Propionibacterium freudenrechii ssp. shermanii JS
Treatment of IBS
Four RCTs were found using L. rhamnosus GG alone (3 RCTs) and one trial with four strains (L. rhamnosus GG, L. rhamnosus LC705, B. breve Bb99 and Prop. Freudenreichii shermanii JC) [65,66,67,68]. The mean daily dose in the three trials using L. rhamnosus GG alone (9 ± 1 × 109/d) was similar to the one trial that included L. rhamnosus GG in their mixture (9 × 109/d). The duration of probiotic (4–8 weeks) was shorter for the three single-strain trials compared to the one multi-strained mixture (duration 24 weeks), as shown in Supplemental Table 2. A meta-analysis (Supplemental Figure 4) found the single strain of L. rhamnosus GG did not significantly increase the responder rate for IBS (RR = 1.28, 95% CI 0.65, 2.54), but the four-strain mixture did significantly increase the responder rate (RR = 1.78, 95 CI 1.19, 2.65). However, the mixture was not significantly increased over the single strain (RRR = 0.72, 95% CI 0.32, 1.58), perhaps due to the low number of RCTs using the mixture (only one trial). There was no significant publication bias (Egger p = 0.37).
Prevention of NEC
Ten RCTs were found using either B. lactis Bb12 alone (3 RCTs) or L. rhamnosus GG alone (4 RCTs) and four two-strain mixtures (1 RCT each): B. lactis Bb12 and B. longum Bb536 or L. rhamnosus GG and B. lactis Bb12 or L. rhamnosus GG and B. lactis Bb536 or L. rhamnosus GG and B. lactis HN19 [30, 69,70,71,72,73,74,75,76,77]. The mean daily dose in the three trials using B. lactis Bb12 alone (5.3 ± 4.5 × 109/d, p = 0.4) was similar to the two trials (2 × 109/day) when in mixtures. In contrast, the mean dose in the four trials using L. rhamnosus GG alone was significantly higher (6 ± 0 × 109/d) than the mean dose of L. rhamnosus GG when used in mixtures (3 ± 1 × 108/d, p < 0.001). The duration of probiotic (mean of 5 ± 1 weeks for both groups) was also similar for single- and multi-strained mixtures (Supplemental Table 2). A meta-analysis (Supplemental Figure 5) found the only significant efficacy was found for L. rhamnosus GG alone (RR = 0.17, 95% CI 0.07, 0.41). L. rhamnosus GG alone was also significantly more effective than the mixture of L. rhamnosus GG and B. lactis Bb12 (RRR = 0.22, 95% CI 0.08, 0.60) and the mixture of L. rhamnosus GG and B. longum Bb536 (RRR = 0.08, 95% CI 0.01, 0.98), as shown in Table 1. There was no significant publication bias (Egger p = 0.86).
Maintenance of Neonatal General Health
Six RCTs were found for assessing use of probiotics for neonatal health with the common outcome of increase in body weight while on probiotics [78,79,80,81,82,83]. Most were done using B. lactis Bb12 alone (5 RCTs) and one trial used a mixture of B. lactis Bb12 with L. rhamnosus CNCM I-3724. The mean daily dose in the five trials using B. lactis Bb12 alone (1 ± 2 × 109/d) was similar to the one trial that included B. lactis Bb12 in the mixture (1 × 109/d). The duration of probiotic for single strains varied from 4–12 months, while the mixture was only given for 2 months (Supplemental Table 2). While the single strain by itself did not result in a significant gain in body weight, the mixture resulted in mild increase (RR = 0.44, 95% CI 0.10, 0.78), (Supplemental Figure 6). The mixture was not significantly better than the single strain alone (t = 1.86, p = 0.20 from meta-regression models), as shown in Table 1. There was no significant publication bias (Egger p = 0.63).
Prevention of URTI
Ten RCTs were found for the prevention of respiratory tract infections, either as a single strain (B. lactis Bb12, 1 RCT or L. rhamnosus GG, 6 RCTs) or a mixture of the two strains (3 RCTs) [84,85,86,87,88,89,90,91,92,93]. The mean daily dose in the six trials using L. rhamnosus GG alone (2 ± 4 × 109/d, p = 0.3) or the one trial using B. lactis Bb12 alone (1 × 109/d) was similar to the three trials that included L. rhamnosus GG or B. lactis Bb12 in their mixture (3 ± 3 × 109/d each strain). The duration of probiotic varied widely, with single strains given for a shorter mean duration (11 ± 12 weeks) were compared to 26.4 ± 19.2 weeks for the mixtures, but the difference was not significant (p = 0.2). Only B. lactis Bb12 alone showed significant efficacy (RR = 0.69, 95% CI 0.53, 0.89), while L. rhamnosus GG alone did not (RR = 0.75, 95% CI 0.53, 1.07) (Supplemental Figure 7). The combination of the two strains together did not show an increase in efficacy (Table 1) despite being given for longer times. The mixture was not significantly different from either single strain alone: B. lactis Bb12 (RRR = 1.36, 95% CI 0.99, 1.86) or L. rhamnosus GG alone (RRR = 1.25, 95% CI 0.85, 1.85). There was no significant publication bias (Egger p = 0.69).
Discussion
This study demonstrated, at least for the limited number of strains that could be evaluated, when disease and strain specificity is accounted for, the efficacy of probiotics is typically not more effective for multiple strains compared to single strains. Only two trials directly compared a single-strain probiotic group to a study arm using a mixture with additional strains, but neither study found a significant difference between the single strain and the mixtures [29, 30]. Lacking more direct comparison trials, pooling trials within the same strain types was productive. A single strain (L. rhamnosus GG) was found more effective than two mixtures containing additional strains for the prevention of necrotizing enterocolitis. A two-strain mixture of L. rhamnosus GG and B. lactis Bb12 was more effective than either strain alone for the eradication of H. pylori when used as an adjunct to antibiotic treatments. In all other comparisons, there was no increased efficacy found when additional probiotic strains were added to an effective single probiotic strain.
With recent publications demonstrating strain and disease specificity observed in clinical trials of efficacy [1], the importance of only comparing the same strains to each other has become apparent. Other studies concluding multi-strained probiotic mixtures were more effective than single-strained probiotics based on their conclusions on biased data, in that the group of multi-strained probiotics was often different types of mixtures. Chang et al. [14] reported ‘multiple strain probiotics’ appeared to be more effective than single strains for the prevention of NEC and mortality, but of the 11 trials pooled into one group of ‘multi-strained’ probiotics, there were actually 10 different types of mixtures of varying efficacies. Several other studies have combined different types of mixtures and pooled different types of single strains into groups and either concluded there was no significant difference between single- and multi-strain probiotics [12, 13, 94]. Chapman et al. [95] reviewed probiotic literature and reported mixtures were more effective in 12/16 (75%) of the studies (including in vitro studies, animal models and RCTs). However, only two studies were RCTs with clinical outcomes and neither study defined the strain(s) of probiotics used. Ouwehand et al. [11] reviewed over 60 RCTs and compared all single-strained probiotics against multi-strain mixtures within 39 different disease indications. Both this extensive review [11] and a short review [10] were unable to come to a conclusion due to the paucity of trials with matching single strain and multi-strain mixtures. None of these reviews quantitatively compared single probiotic strains with matched multi-strain mixtures.
The different efficacies of probiotic strains may be due to varying mechanisms of actions possessed by different strains and if they are given singly or in combination with other strains. A clear advantage of a single strain was only found for Lactobacillus rhamnosus GG (ATCC 53103) for the prevention of necrotizing enterocolitis. Mileti et al. [6] studied three strains of lactobacilli (including L. rhamnosus GG) and reported differing abilities to produce cytokines by strain. In our study, addition of B. lactis Bb12 to L. rhamnosus GG did not result in a synergistic effect for seven of the different disease indications. In only one case was the mixture of L. rhamnosus GG and B. lactis Bb12 more effective than either of the single strains given alone (for the eradication of H. pylori). A basis for this synergistic effect may be due to the doubling of the adhesion of B. lactis Bb12 when combined with L. rhamnosus GG [3]. Few strains had evidence from trials for a single strain linked with trials of additional strains. However, in the case of L. helveticus R52, the single strain significantly prevented AAD, but the addition of another strain (L. rhamnosus R11) did not significantly improve this efficacy, which might reinforce the efficacy to the R52 strain. Interestingly, when two additional strains were added (B. longum I-175 and S. cerevisiae I-1079), this 4-strain mixture was no longer significantly protective of AAD. An explanation for this lack of protective effect might be the observed reduction in cytokine production in this four-strain mixture compared to cytokine levels when the single strains were tested independently [96].
There are several strengths of this review. This is the first study directly linking the efficacy of single-strained probiotics to a multi-strain mixture containing the same strain and comparing efficacy within the same type and mode (prevention or treatment) of disease. Unlike previous reviews that qualitatively compared the efficacy of single strain and multi-strain mixtures, we used quantitative tests to determine whether there is a significant difference between these types of probiotics. We extensively reviewed a large number of trials (n = 65 RCTs) over eight different types of diseases.
There are several limitations of this review. Although the research on probiotics has been done in a variety of disease indications when determining whether singlestrains or multiple strains are more effective, the lack of RCTs using the same strains for single strain versus multi-strain mixtures limited the types of probiotics we could analyze. Many of the most commonly used probiotics could not be included in this analysis due to a lack of trials using the same single strain and trials with the identical strain in multi-strain mixtures. For example, one of the more commonly researched probiotic, S. boulardii CNCM I-745, could not be assessed, as all mixtures either used another strain (S. cerevisiae CNCM I-1079) or did not provide the strain of Saccharomyces used. Another limitation was the lack of strain designations in many single strain or multi-strain mixtures. In addition, not all strains used in multi-strained mixtures had corresponding trials with each individual strain of probiotic. Another limitation was the lack of common outcome measures used for the same type of disease (most notable, IBS outcomes ranged from change in symptom scores, to quality of life measures or frequency of abdominal pain/gas). In most cases, the potential for synergistic or antagonistic effects in multi-strained mixtures could not be evaluated, as most single strains in mixtures have not been tested independently. The variety of daily doses and duration of probiotics given varied, even within disease indications and, in general, daily doses or duration were not significantly different. In one case, the significant efficacy for the single strain of L. rhamnosus GG compared to mixtures in the prevention of NEC might have been due to the significantly higher dose used in the single-strain trials. Other confounding factors, such as differences in dietary patterns in different countries, study population characteristics (age, race, etc.) were not analyzed in this review.
The choice of an appropriate probiotic product for patients continues to be a clinical challenge, and as not all probiotics are equally effective or cost-effective, the decision must be based on available scientific evidence. Future trials should compare similar doses and durations of single strains of probiotics with multi-strain mixtures containing the identical single strain within the same disease indication. Adding a previously untested probiotic strain to a mixture should carefully consider interactions between the strains, doses and durations given and how an increase in efficacy is documented. Each single strain should be tested independently with clearly defined parameters (study population, daily dose and duration of probiotic given, disease outcome measures) and then a mixture made from the previously studied single strains (at the same dose) can be tested for any increased efficacy. In addition, other important considerations, such as cost-effectiveness, frequency of side effects and impact on the normal microbiome need exploration, as this information was not found in most of the included trials in this review. More studies comparing the same strains given singly versus given in a mixture within the same disease indication are needed to clearly determine whether single strains or mixtures are more effective. This study shows that, in most cases, it is not just the number of strains used to prevent or treat specific diseases that predicts efficacy, rather it is the choice of which strain that is the most important factor impacting efficacy.
References
Sniffen JC, McFarland LV, Evans CT, et al. Choosing an appropriate probiotic product for your patient: an evidence-based practical guide. Including S1. Dataset. McFarland dataset for probiotic trials. PLOS ONE. 2018;13:e0209205.
Szajewska H. Pooling data on different probiotics is not appropriate to assess the efficacy of probiotics. Eur J Pediatr. 2014;173:975.
Ouwehand AC, Isolauri E, Kirjavainen PV, et al. The mucus binding of Bifidobacterium lactis Bb12 is enhanced in the presence of Lactobacillus GG and Lact. delbrueckii subsp. bulgaricus. Lett Appl Microbiol. 2000;30:10–13.
Timmerman HM, Koning CJ, Mulder L, et al. Monostrain, multistrain and multispecies probiotics-a comparison of functionality and efficacy. Int J Food Microbiol. 2004;96:219–233.
Medina M, Izquierdo E, Ennahar S, et al. Differential immunomodulatory properties of Bifidobacterium longum strains: relevance to probiotic selection and clinical applications. Clin Exp Immunol. 2007;150:531–538.
Mileti E, Matteoli G, Iliev ID, et al. Comparison of the immunomodulatory properties of three probiotic strains of Lactobacilli using complex culture systems: prediction for in vivo efficacy. PLoS ONE. 2009;4:e7056.
Chapman CMC, Gibson GR, Rowland I. In vitro evaluation of single- and multi-strain probiotics: inter-species inhibition between probiotic strains, and inhibition of pathogens. Anaerobe. 2012;18:405–413.
Fredua-Agyeman M, Stapleton P, Basit AW, et al. Microcalorimetric evaluation of a multi-strain probiotic: interspecies inhibition between probiotic strains. J Funct Foods. 2017;36:356–361.
Forssten SD, Ouwehand AC. Simulating colonic survival of probiotics in single-strain products compared to multi-strain products. Microb Ecol Health Dis. 2017;28:1378061.
Korada SK, Yarla NS, Mishra V, et al. Single probiotic versus multiple probiotics—a debate on current scenario for alleviating health benefits. Curr Pharm Des. 2018;24:4150–4153.
Ouwehand AC, Invernici MM, Furlaneto FAC, et al. Effectiveness of multistrain versus single-strain probiotics: current status and recommendations for the future. J Clin Gastroenterol. 2018;52:S35–S40.
Goldenberg JZ, Lytvyn L, Steurich J, et al. Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database Syst Rev. 2015;4:CD004827.
Johnston BC, Ma SS, Goldenberg JZ, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea: a systematic review and meta-analysis. Ann Intern Med. 2012;157:878–888.
Chang HY, Chen JH, Chang JH, et al. Multiple strains probiotics appear to be the most effective probiotics in the prevention of necrotizing enterocolitis and mortality: an updated meta-analysis. PLoS ONE. 2017;12:e0171579.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
McFarland LV, Elmer GW, McFarland M. Meta-analysis of probiotics for the prevention and treatment of acute pediatric diarrhea. Int J Probiot Prebiot. 2006;1:63–76.
McFarland LV, Dublin S. Meta-analysis of probiotics for the treatment of irritable bowel syndrome. World J Gastroenterol. 2008;14:2650–2661.
McFarland LV, Goh S. Preventing pediatric antibiotic-associated diarrhea and Clostridium difficile infections with probiotics: a meta-analysis. World J Meta-Anal. 2013;1:102–120.
McFarland LV, Malfertheiner P, Huang Y, et al. Meta-analysis of single strain probiotics for the eradication of Helicobacter pylori and prevention of adverse events. World J Meta-Anal. 2015;3:97–117.
McFarland LV, Huang Y, Wang L, et al. Systematic review and meta-analysis: multi-strain probiotics as adjunct therapy for Helicobacter pylori eradication and prevention of adverse events. United Euro J Gastroenterol. 2016;4:546–561.
Feng JR, Wang F, Qiu X, et al. Efficacy and safety of probiotics supplemented triple therapy for eradication of Helicobacter pyloriin children: a systematic review and network meta-analysis. Euro J Clin Pharm. 2017;73:1199–1208.
Agamennone V, Krul CAM, Rijkers G, et al. A practical guide for probiotics applied to the case of antibiotic-associated diarrhea in The Netherlands. BMC Gastroenterol. 2018;18:103.
McFarland LV, Goh S. Are probiotics and prebiotics effective in the prevention of travellers’ diarrhea: a systematic review and meta-analysis. Trav Med Infect Dis. 2019;27:11–19.
Hill C, Guarner F, Reid G, et al. Expert consensus document: the International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11:506–514.
McFarland LV, Evans CT, Goldstein EJC. Strain-specificity and disease-specificity of probiotic efficacy: a systematic review and meta-analysis. Front Med. 2018;5:1–14.
Palmer TM, Sterne JAC, eds. Meta-analysis in Stata: an updated collection from the Stata Journal. 2nd ed. College Station: Stata Press; 2016.
Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane-handbook.org.
Altman DG, Bland JM. Statistics notes interaction revisited: the difference between two estimates. BMJ. 2003;326:219.
Viljanen M, Savilahti E, Haahtela T, et al. Probiotics in the treatment of atopic eczema/dermatitis syndrome in infants: a double-blind placebo-controlled trial. Allergy. 2005;60:494–500.
Hays S, Jacquot A, Gauthier H, et al. Probiotics and growth in preterm infants: a randomized controlled trial, PREMAPRO study. Clin Nutr. 2016;35:802–811. https://doi.org/10.1016/j.clnu.2015.06.
Vaisanen ML, Leskinen M, Siitonen A, et al. Occurrence of diarrhea in children receiving oral antibiotics with or without probiotic supplementation with Lactobacillus GG. Microbiol Ecol Health Dis. 1998;10:199–200.
Vanderhoof JA, Whitney DB, Antonson DL, et al. Lactobacillus GG in the prevention of antibiotic-associated diarrhea in children. J Pediatr. 1999;135:564–568.
Arvola T, Laiho K, Torkkeli S, et al. Prophylactic Lactobacillus GG reduces antibiotic-associated diarrhea in children with respiratory infections: a randomized study. Pediatrics. 1999;104:e64.
Armuzzi A, Cremonini F, Ojetti V, et al. Effect of Lactobacillus GG supplementation on antibiotic-associated gastrointestinal side effects during Helicobacter pylori eradication therapy: a pilot study. Digestion. 2001;63:1–7.
Armuzzi A, Cremonini F, Bartolozzi F, et al. The effect of oral administration of Lactobacillus GG on antibiotic-associated gastrointestinal side-effects during Helicobacter pylori eradication therapy. Aliment Pharmacol Ther. 2001;15:163–169.
Thomas MR, Litin SC, Osmon DR, et al. Lack of effect of Lactobacillus GG on antibiotic-associated diarrhea: a randomized, placebo-controlled trial. Mayo Clin Proc. 2001;76:883–889.
Cremonini F, Di Caro S, Covino M, et al. Effect of different probiotic preparations on anti-helicobacter pylori therapy-related side effects: a parallel group, triple blind, placebo-controlled study. Am J Gastroenterol. 2002;97:2744–2749.
Miller M, Florencio S, Eastmond J, et al. Results of 2 prospective randomized studies of Lactobacillus GG to prevent C. difficile infection in hospitalized adults receiving antibiotics. Intersci Conf Antimicrobial Agents Chemother. 2008;48:578–579.
Szajewska H, Albrecht P, Topczewska-Cabanek A. Randomized, double-blind, placebo-controlled trial: effect of lactobacillus GG supplementation on Helicobacter pylori eradication rates and side effects during treatment in children. J Pediatr Gastroenterol Nutr. 2009;48:431–436.
Padilla-Ruiz M, Fernández Aguiar ME, Arce Nuñez M, et al. Lactobacillus rhamnosus GG supplementation to reduce side-effects of anti-Helicobacter pylori treatment. Rev Gastroenterol Peru. 2013;33:121–130.
Hauser G, Salkic N, Vukelic K, et al. Probiotics for standard triple Helicobacter pylori eradication: a randomized, double-blind, placebo-controlled trial. Medicine (Baltimore). 2015;94:e685.
Wenus C, Goll R, Loken EB, et al. Prevention of antibiotic-associated diarrhoea by a fermented probiotic milk drink. Eur J Clin Nutr. 2008;62:299–301.
Fox MJ, Ahuja KD, Robertson IK, et al. Can probiotic yogurt prevent diarrhoea in children on antibiotics? A double-blind, randomised, placebo-controlled study. BMJ Open. 2015;5:e006474.
Myllyluoma E, Veijola L, Ahlroos T, et al. Probiotic supplementation improves tolerance to Helicobacter pylori eradication therapy—a placebo-controlled, double-blind randomized pilot study. Aliment Pharmacol Ther. 2005;21:1263–1272.
Ivanko O, Radutnaya E. Lactobacillus acidophilus reduces frequency of diarrhoea caused by toxins Clostridium difficile A + B in children treated by antibiotics. Zaporozhye Med Period. 2005;2:21–23.
Marushko Y, Shef G. Current status of antibiotics-associated bowel disorders issue in children. Perinatol Paediatr. 2007;4:65–68.
Gnaytenko O, Lychkovska O, Kulachkovska Y, et al. Antibiotic-associated diarrhoea as a complication of anti-helicobacter therapy in children. Pract Med. 2009;5:76–83.
Aryayev M, Kononenko N. Prevention of antibiotic-associated diarrhoea in patients with cystic fibrosis. Odessa Med J. 2009;4:78.
Song H, Kim J, Jung S, et al. Effect of probiotic Lactobacillus (Lacidofil® Cap) for the prevention of antibiotic-associated diarrhoea: a prospective, randomised double-blind multicenter study. J Korean Med Sci. 2010;25:1784–1791.
Liskovich V, Naumov I, Ganchar E, et al. Efficiency of Lacidofil-WM for prevention of vaginal dysbiosis and antibiotics-associated diarrhoea in puerperas after caesarean operation. Health. 2010;1:63–66.
Evans M, Salewski RP, Christman MC, et al. Effectiveness of Lactobacillus helveticus and Lactobacillus rhamnosus for the management of antibiotic-associated diarrhoea in healthy adults: a randomised, double-blind, placebo-controlled trial. Br J Nutr. 2016;116:94–103.
Grgov S, Tasić T, Radovanović-Dinić B, et al. Can probiotics improve efficiency and safety profile of triple Helicobacter pylori eradication therapy? A prospective randomized study. Vojnosanit Pregl. 2016;73:1044–1049.
Majamaa H, Isolauri E. Probiotics: a novel approach in the management of food allergy. J Allergy Clin Immunol. 1997;99:179–185.
Isolauri E, Arvola T, Sütas Y, Moilanen E, Salminen S. Probiotics in the management of atopic eczema. Clin Exp Allergy. 2000;30:1604–1610.
Kirjavainen PV, Salminen SJ, Isolauri E. Probiotic bacteria in the management of atopic disease: underscoring the importance of viability. J Pediatr Gastroenterol Nutr. 2003;36:223–227.
Fölster-Holst R, Müller F, Schnopp N, et al. Prospective, randomized controlled trial on Lactobacillus rhamnosus in infants with moderate to severe atopic dermatitis. Br J Dermatol. 2006;155:1256–1261.
Grüber C, Keil T, Kulig M, et al. History of respiratory infections in the first 12 yr among children from a birth cohort. Pediatr Allergy Immunol. 2007;62:1270–1276.
Kalliomaki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E. Probiotics in primary prevention of atopic disease: a randomized placebo-controlled trial. Lancet. 2001;357:1076–1079.
Helin T, Haahtela S, Haahtela T. No effect of oral treatment with an intestinal bacterial strain, Lactobacillus rhamnosus (ATCC 53103), on birch-pollen allergy: a placebo-controlled double-blind study. Allergy. 2002;57:243–246. https://doi.org/10.1034/j.1398-9995.2002.1s3299.x.
Kopp MV, Hennemuth I, Heinzmann A, Urbanek R. Randomized, double-blind, placebo-controlled trial of probiotics for primary prevention: no clinical effects of Lactobacillus GG supplementation. Pediatrics. 2008;121:e850–e856.
Cabana MD, McKean M, Caughey AB, et al. Early probiotic supplementation for eczema and asthma prevention: a randomized controlled trial. Pediatrics. 2017;140:e20163000. https://doi.org/10.1542/peds.2016-3000.
Kukkonen K, Savilahti E, Haahtela T, et al. Probiotics and prebiotic galacto-oligosaccharides in the prevention of allergic diseases: a randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol. 2007;119:192–198.
Simpson MR, Dotterud CK, Storrø O, Johnsen R, Øien T. Perinatal probiotic supplementation in the prevention of allergy related disease: 6 year follow up of a randomised controlled trial. BMC Dermatol. 2015;15:13. https://doi.org/10.1186/s12895-015-0030-1.
Dotterud CK, Storrø O, Johnsen R, Oien T. Probiotics in pregnant women to prevent allergic disease: a randomized, double-blind trial. Br J Dermatol. 2010;163:616–623. https://doi.org/10.1111/j.1365-2133.2010.09889.x.
Bausserman M, Michail S. The use of Lactobacillus GG in irritable bowel syndrome in children: a double-blind randomized control trial. J Pediatr. 2005;147:197–201. https://doi.org/10.1016/j.jpeds.2005.05.015.
Gawrońska A, Dziechciarz P, Horvath A, Szajewska H. A randomized double-blind placebo-controlled trial of Lactobacillus GG for abdominal pain disorders in children. Aliment Pharmacol Ther. 2007;25:177–184. https://doi.org/10.1111/j.1365-2036.2006.03175.x.
Francavilla R, Miniello V, Magistà AM, et al. A randomized controlled trial of Lactobacillus GG in children with functional abdominal pain. Pediatrics. 2010;126:e1445–e1452. https://doi.org/10.1542/peds.2010-0467.
Kajander K, Hatakka K, Poussa T, Farkkila M, Korpela R. A probiotic mixture alleviates symptoms in irritable bowel syndrome patients: a controlled 6 month intervention. Aliment Pharmacol Ther. 2005;22:387–394.
Mohan R, Koebnick C, Schildt J, et al. Effects of Bifidobacterium lactis Bb12 supplementation on intestinal microbiota of preterm infants: a double-blind, placebo-controlled, randomized study. J Clin Microbiol. 2006;44:4025–4031.
Mihatsch WA, Vossbeck S, Eikmanns B, Hoegel J, Pohlandt F. Effect of Bifidobacterium lactis on the incidence of nosocomial infections in very-low-birth-weight infants: a randomized controlled trial. Neonatology. 2010;98:156–163. https://doi.org/10.1159/000280291.
Lambæk ID, Fonnest G, Gormsen M, Brok J, Greisen G. Probiotics to prevent necrotising enterocolitis in very preterm infants. Dan Med J. 2016;63:A5203.
Dani C, Biadaioli R, Bertini G, Martelli E, Rubaltelli FF. Probiotics feeding in prevention of urinary tract infection, bacterial sepsis and necrotizing enterocolitis in preterm infants. A prospective double-blind study. Biol Neonate. 2002;82:103–108.
Manzoni P, Mostert M, Leonessa ML, et al. Oral supplementation with Lactobacillus casei subspecies rhamnosus prevents enteric colonization by Candida species in preterm neonates: a randomized study. Clin Infect Dis. 2006;42:1735–1742. https://doi.org/10.1086/504324.
Manzoni P, Rinaldi M, Cattani S, et al. Bovine lactoferrin supplementation for prevention of late-onset sepsis in very low-birth-weight neonates: a randomized trial. JAMA. 2009;302:1421–1428. https://doi.org/10.1001/jama.2009.1403.
Manzoni P, Meyer M, Stolfi I, et al. Bovine lactoferrin supplementation for prevention of necrotizing enterocolitis in very-low-birth-weight neonates: a randomized clinical trial. Early Hum Dev. 2014;90:S60–S65. https://doi.org/10.1016/S0378-3782(14)70020-9.
Rougé C, Piloquet H, Butel MJ, et al. Oral supplementation with probiotics in very-low-birth-weight preterm infants: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr. 2009;89:1828–1835. https://doi.org/10.3945/ajcn.2008.26919.
Van Niekerk E, Nel DG, Blaauw R, Kirsten GF. Probiotics reduce necrotizing enterocolitis severity in HIV-exposed premature infants. J Trop Pediatr. 2015;61:155–164. https://doi.org/10.1093/tropej/fmv004.
Ziegler EE, Jeter JM, Drulis JM, et al. Formula with reduced content of improved, partially hydrolyzed protein and probiotics: infant growth and health. Monatsschrift Kinderheilkunde. 2003;151:S65–S71.
Barclay D, Giammanco A, Carrie-Fassler AL, et al. Growth and tolerance of whey-based starter infant formula with enhanced protein efficiency and containing pro-, pre- or synbiotics: a randomized controlled trial in term infants. J Pediatr Gastroenterol Nutr. 2003;37:388.
Urban MF, Bolton KD, Mokhachane M, et al. Growth of infants born to HIV-infected women when fed a biologically acidified starter formula with and without probiotics. S Afr J Clin Nut. 2008;21:28–32.
Gibson RA, Barclay D, Marshall H, et al. Safety of supplementing infant formula with long- chain polyunsaturated fatty acids and Bifidobacterium lactis in term infants: a randomised controlled trial. Br J Nutr. 2009;101:1706–1713. https://doi.org/10.1017/S0007114508084080.
Cooper P, Bolton KD, Velaphi S, et al. Early benefits of a starter formula enriched in prebiotics and probiotics on the gut microbiota of healthy infants born to HIV+ mothers: a randomized double-blind controlled trial. Clin Med Insights Pediatr. 2017;10:119–130. https://doi.org/10.4137/CMPed.S40134.
Mantaring J, Benyacoub J, Destura R, et al. Effect of maternal supplement beverage with and without probiotics during pregnancy and lactation on maternal and infant health: a randomized controlled trial in the Philippines. BMC Pregnancy Childbirth. 2018;18:193. https://doi.org/10.1186/s12884-018-1828-8.
Taipale T, Pienihäkkinen K, Isolauri E, et al. Bifidobacterium animalis subsp. lactis BB-12 in reducing the risk of infections in infancy. Br J Nutr. 2011;105:409–416. https://doi.org/10.1017/s0007114510003685.
Hatakka K, Savilahti E, Pönkä A, et al. Effect of long term consumption of probiotic milk on infections in children attending day care centres: double blind, randomised trial. BMJ. 2001;322:1327.
Honeycutt TC, El Khashab M, Wardrop RM 3rd, et al. Probiotic administration and the incidence of nosocomialinfection in pediatric intensive care: a randomized placebo-controlled trial. Pediatr Crit Care Med. 2007;8:452–458. https://doi.org/10.1097/01.PCC.0000282176.41134.E6.
Hojsak I, Snovak N, Abdović S, et al. Lactobacillus GG in the prevention of gastrointestinal and respiratory tract infections in children who attend day care centers: a randomized, double-blind, placebo-controlled trial. Clin Nutr. 2010;29:312–316. https://doi.org/10.1016/j.clnu.2009.09.008.
Morrow LE, Kollef MH, Casale TB. Probiotic prophylaxis of ventilator-associated pneumonia: a blinded, randomized, controlled trial. Am J Respir Crit Care Med. 2010;182:1058–1064. https://doi.org/10.1164/rccm.200912-1853OC.
Kumpu M, Kekkonen RA, Korpela R, et al. Effect of live and inactivated Lactobacillus rhamnosus GG on experimentally induced rhinovirus colds: randomised, double blind, placebo-controlled pilot trial. Benef Microbes. 2015;6:631–639. https://doi.org/10.3920/bm2014.0164.
Luoto R, Ruuskanen O, Waris M, Kalliomäki M, Salminen S, Isolauri E. Prebiotic and probiotic supplementation prevents rhinovirus infections in preterm infants: a randomized, placebo-controlled trial. Allergy Clin Immunol. 2014;133:405–413. https://doi.org/10.1016/j.jaci.2013.08.020.
Rautava S, Salminen S, Isolauri E. Specific probiotics in reducing the risk of acute infections in infancy—a randomised, double-blind, placebo-controlled study. Br J Nutr. 2009;101:1722–1726. https://doi.org/10.1017/S0007114508116282.
Smith TJ, Rigassio-Radler D, Denmark R, Haley T, Touger-Decker R. Effect of Lactobacillusrhamnosus LGG® and Bifidobacterium animalis ssp. lactis BB-12® on health-related quality of life in college students affected by upper respiratory infections. Br J Nutr. 2013;109:1999–2007. https://doi.org/10.1017/s0007114512004138.
Lehtoranta L, Kalima K, He L, et al. Specific probiotics and virological findings in symptomatic conscripts attending military service in Finland. J Clin Virol. 2014;60:276–281. https://doi.org/10.1016/j.jcv.2014.03.021.
Chapman CMC, Gibson GR, Rowland I. Effects of single- and multi-strain probiotics on biofilm formation and in vitro adhesion to bladder cells by urinary tract pathogens. Anaerobe. 2014;27:71–76.
Chapman C, Gibson GR, Rowland I. Health benefits of probiotics: are mixtures more effective single strains? Euro J Nutr. 2011;50:1–17.
Bisson JF, Hidalgo S, Rozan P, et al. Preventive effects of different probiotic formulations on travelers’ diarrhea model in Wistar rats: preventive effects of probiotics on TD. Dig Dis Sci.. 2010;55:911–919. https://doi.org/10.1007/s10620-009-0822-4.
Funding
This study was unfunded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LVM is on the Scientific Advisory Board and paid consultant for Bio-K+ (Canada) and on the Microbiome Advisory Board and paid consultant for Biocodex (France) but owns no stock or equity in either company.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McFarland, L.V. Efficacy of Single-Strain Probiotics Versus Multi-Strain Mixtures: Systematic Review of Strain and Disease Specificity. Dig Dis Sci 66, 694–704 (2021). https://doi.org/10.1007/s10620-020-06244-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06244-z