Abstract
Irritable bowel syndrome (IBS) is an extremely common and often very debilitating chronic functional gastrointestinal disorder. Despite its prevalence, significant associated healthcare costs, and quality-of-life issues for affected individuals, our understanding of its etiology remained limited. However, it is now evident that microbial factors play key roles in IBS pathophysiology. Acute gastroenteritis following exposure to pathogens can precipitate the development of IBS, and studies have demonstrated changes in the gut microbiome in IBS patients. These changes may explain some of the symptoms of IBS, including visceral hypersensitivity, as gut microbes exert effects on the host immune system and gut barrier function, as well as the brain–gut axis. Microbial differences also appear to underlie the two main functional categories of IBS: diarrhea-predominant IBS (IBS-D) is associated with small intestinal bacterial overgrowth, which can be diagnosed by a positive hydrogen breath test, and constipation-predominant IBS (IBS-C) is associated with increased levels of methanogenic archaea, which can be diagnosed by a positive methane breath test. Mechanistically, the pathogens that cause gastroenteritis and trigger subsequent IBS development produce a common toxin, cytolethal distending toxin B (CdtB), and antibodies raised against CdtB cross-react with the cytoskeletal protein vinculin and impair gut motility, facilitating bacterial overgrowth. In contrast, methane gas slows intestinal contractility, which may facilitate the development of constipation. While antibiotics and dietary manipulations have been used to relieve IBS symptoms, with varying success, elucidating the specific mechanisms by which gut microbes exert their effects on the host may allow the development of targeted treatments that may successfully treat the underlying causes of IBS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Mark Pimentel

Anthony Lembo
Introduction
Irritable bowel syndrome (IBS) is a chronic functional gastrointestinal disorder characterized by abdominal pain and altered bowel habits, either diarrhea (IBS-D), constipation (IBS-C), or altering between diarrhea and constipation (IBS-M). Approximately 13% of the world’s population suffers from IBS symptoms [1], which results in increased consultations, diagnostic procedures, and surgeries. IBS is also associated with increased medication consumption, reduced quality of life, and high rates of absenteeism from work and school, and the costs of IBS in the USA alone have been estimated at over $30 billion [2].
Despite the prevalence and burden of IBS, its pathobiology has remained elusive. Early studies focused on gastrointestinal motor disturbances including changes in intestinal transit and abnormal contractions [3]. Subsequent studies found that many IBS patients experience pain from rectal balloon distention at lower thresholds than healthy controls (i.e., visceral hypersensitivity). Increasing evidence over the past decade suggests that the microbiome may contribute significantly to these findings in IBS. Early recognition that IBS frequently develops after an episode of infectious gastroenteritis led investigators to explore the role of bacteria in the pathophysiology of IBS. Uncovering this role requires the understanding of two parallel paths of research into post-infectious IBS and intestinal dysbiosis, which later merge into a single hypothesis (Fig. 1).
Post-infectious IBS
Prevalence
Reports of post-infectious IBS are not new, although until recently these descriptions were sporadic. In the 1960s, Chaudhary and Truelove described what was then known as “irritable colon syndrome” following infectious gastroenteritis [4]. In 1994, McKendrick and Read reported the development of IBS following two outbreaks of Salmonella in the UK [5]. Subsequently, multiple infectious gastrointestinal outbreaks have been studied, with the incidence of post-infectious IBS ranging from 3.7 to 36% and lasting up to 6 and 8 years after the acute illness [6]. In addition to typical acute gastroenteritis pathogens, even more exotic pathogens are being linked to IBS as well, such as spirochetes [7].
A recent meta-analysis of 45 studies that prospectively followed infectious outbreaks found that the pooled incidence of IBS was 10.1% at 3 or more months after acute gastroenteritis and 14.5% at more than 12 months after acute gastroenteritis [6]. The risk of IBS was 4.2-fold higher in patients who had acute gastroenteritis in the past 12 months than in those who did not [6]. Several factors increased the likelihood of developing IBS (Table 1). Notably, the severity of acute gastroenteritis and female sex were strong predictors. Although the reasons for the higher prevalence of IBS in women remain unproven, a recent genome-wide association study (GWAS) by Bonfiglio et al. found an association between variants at the locus 9q31.2 and the risk of IBS in women, a region previously associated with conditions and traits influenced by sex hormones [8].
Psychological Factors
Although IBS is frequently associated with stress and anxiety [9], it has been unclear to what extent these contribute to the development of IBS, or vice versa. Evidence from studies in animal models, e.g., the Citrobacter rodentium mouse model [10], indicates stress may affect the gut microbiota, increase gut motility [11], and augment the risk of developing post-infectious symptoms. Recently, a study of deployed US military personnel found that, despite significant psychological stress in combat zones, acute gastroenteritis during deployment rather than stress was the most important risk factor for IBS development [12]. Furthermore, recent evidence indicates that in approximately two-thirds of IBS cases, psychological distress develops after the onset of gastrointestinal symptoms [13].
Post-infectious IBS Changes the Microbiome
Following the emerging data that linked IBS to acute gastroenteritis, animal models were developed. These included the above-described Citrobacter rodentium mouse model [10], as well as the Trichinella spiralis mouse model that has been used to study smooth muscle hypercontractility following parasite infection [14]. While these models have provided valuable insights, neither Citrobacter nor Trichinella are common causes of human acute gastroenteritis or post-infectious IBS in the USA. In another model, Sprague–Dawley rats were infected with Campylobacter jejuni [15], one of the most common causes of bacterial gastroenteritis in the USA. After recovery from the initial acute infection, most animals developed altered stool form, increased rectal lymphocytes [15], reduced deep muscular plexus interstitial cells of Cajal, and small intestinal bacterial overgrowth [16]. These findings mirrored findings in humans with post-infectious IBS [17]. Interestingly, small intestinal bacterial overgrowth in humans can result from reductions in migrating motor complexes [18] for which the deep muscular plexus interstitial cells of Cajal are the pacemaker cells.
This new animal model was an important tool to study the development of IBS following acute gastroenteritis. Since C. difficile, C. jejuni, Salmonella, Escherichia coli, and Shigella can all cause IBS [6], identifying a common factor became an important goal. One commonality was the production of cytolethal distending toxin (Cdt). Pokkunuri et al. showed that animals infected with a genetically modified C. jejuni lacking CdtB had fewer symptoms (i.e., altered bowel habits) and less inflammation (i.e., rectal lymphocytes [17]) compared to animals exposed to wild-type C. jejuni [19]. These results suggested the CdtB toxin was required for the development of IBS-like phenotypes.
Subsequent studies found that antibodies to CdtB cross-react with vinculin [20], an intracellular cytoskeletal protein that is an important component of cell adhesion and plays a key role in neuronal cell motility and contractility [21], particularly in the gastrointestinal tract. Data suggest that exposure to CdtB leads to autoimmunity to vinculin [20], supporting an earlier hypothesis that autoimmunity may play a role in functional gastrointestinal disorders [22].
The clinical significance of these discoveries is highlighted by the finding that anti-CdtB and anti-vinculin antibodies occur more commonly in IBS-D as compared to other conditions that cause diarrhea, including inflammatory bowel disease (IBD) and celiac disease [23]. When both antibodies are positive, an IBS-D diagnosis can be reached more confidently [23]. However, sensitivity remained low at approximately 50%, likely due to the heterogeneous nature of IBS-D pathophysiology. The utility of these antibodies in diagnosing IBS has been validated in several independent studies performed in European [24], Latin American [25], and US military [26] populations.
Antibiotics
Studies have also suggested that prior antibiotics are a risk factor for IBS. In a case-controlled study, antibiotic use in the previous year was associated with a three-fold increased risk of developing IBS [27]. In another case-controlled study, 83% of patients with new-onset functional GI symptoms reported antibiotic use with an odds ratio of 1.95 (95% CI: 1.2–3.0, p = 0.005) [28].
Role of Intestinal Dysbiosis in IBS
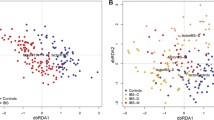
The concept that the intestinal microbiome was associated with human disease led investigators to study whether alterations in the microbiome could be identified in IBS, and whether these contributed to, or were the result of, the IBS development. Numerous studies have been performed using varying techniques (quantitative PCR (qPCR), 16S rRNA denaturing gradient gel electrophoresis (DGGE), phylogenetic microarrays, and 16S rRNA gene sequencing) and sample types (fecal samples, duodenal mucosa brush samples, duodenal aspirates, and colonic/rectal mucosal biopsy samples) (Table 2). Moreover, some compared IBS subjects to healthy controls, while others examined specific IBS subtypes. Comparing these studies, several [29,30,31,32,33,34], but not all [35], identified lower microbial diversity or richness in IBS subjects versus healthy controls. At the phylum level, some found an increase in Firmicutes-to-Bacteroidetes ratio in IBS subjects, including Rajilic-Stojanovic et al. who also found decreased Bifidobacterium [36] and Jeffery et al. who also found increased Actinobacteria in IBS samples [31]. In contrast, Ng et al. found increased Bacteroidetes abundance and decreased Actinobacteria abundance in IBS subjects versus healthy controls, with probiotic treatment reducing the genus Bacteroides to levels similar to controls [32]. A recent meta-analysis of stool qPCR studies identified consistent findings of lower levels of Lactobacillus, Bifidobacterium, and Faecalibacterium prausnitzii in IBS subjects [37]. Using a machine learning procedure, a recent study identified a microbial profile in patients with severe IBS characterized by decreased microbial richness, lower levels of exhaled methane, and a Bacteroides-enriched enterotype [38].
One of the stronger links between IBS and the intestinal microbiota is the finding that the transfer of stool from IBS-D patients to animals induces changes similar to those in IBS, including altered intestinal motility, innate immune-activation and increased intestinal permeability, and visceral hypersensitivity [39]. IBS patients also appear to have increased expression of intestinal Toll-like receptors (TLRs) [40, 41], which are important mediators of intestinal immune response to gut microbes—specifically, TLR4 is implicated in recognition of bacterial lipopolysaccharide (LPS) and TLR5 is implicated in flagellin recognition [42]. Pike et al. suggested that differences in host immune responses may predict the likelihood of developing IBS, with or without antecedent acute gastroenteritis, and concluded that combining cytokine profiles with microbiome-directed antibodies might provide optimal results [26]. They also found a strong association between anti-vinculin antibody levels and development of post-Campylobacter IBS [26].
Small Intestinal Bacterial Overgrowth and IBS
Many, but not all, studies have reported a greater prevalence of small intestinal bacterial overgrowth in IBS versus controls based on either glucose or lactulose breath testing [43]. Meta-analyses revealed that breath testing is abnormal in IBS subjects more often than in healthy controls (pooled OR 3.45 (95% CI 0.9–12.7) or 4.7 (95% CI 1.7–12.95)), depending on the criteria used to define a positive test [43]. In comparison, only a handful of studies used small bowel cultures to determine the presence of small intestinal bacterial overgrowth. Posserud et al. showed that coliforms were much more common in duodenal aspirates from IBS subjects versus healthy controls [44]. However, using older definitions of small intestinal bacterial overgrowth (> 105 cfu/mL), these differences were not significant. Another study found small intestinal bacterial overgrowth was far more predominant in IBS patients than in non-IBS patients undergoing endoscopy for other reasons [45]. QPCR and deep sequencing of small bowel aspirates from IBS subjects and controls confirmed these findings [33].
Recent data suggest that elevated methane gas production, generated predominantly by archaeal species, can influence intestinal motor activity and leads to intestinal slowing and constipation [46, 47]. In humans, the predominant archaeon and methane producer is Methanobrevibacter smithii [48]. In a double-blind, randomized, placebo-controlled trial [49], a combination of rifaximin and neomycin could be used to eradicate methane on breath test in up to 85% of subjects, resulting in significant improvements in gastrointestinal symptoms including constipation severity, straining, and bloating [49]. A recent consensus now considers methane (as a surrogate for excess intestinal colonization with methanogens) as important in the assessment of constipation and IBS-C [50].
Brain–Gut–Microbiome Axis
The brain–gut axis has been widely described as important to the understanding of IBS [3]. IBS is associated with alterations in gut motility, gut barrier function, immune regulation, and visceral hypersensitivity, all of which can be affected by the gut microbiome [42, 51, 52]. For example, increased serum levels of bacterial LPS and anti-flagellin antibodies have been demonstrated in IBS-D subjects, indicating impaired gut barrier function and resultant bacterial translocation to the circulation [53], which in turn leads to immune responses and inflammation. Interestingly, this increase in serum anti-flagellin antibodies correlated with patient anxiety scores [53], underscoring the central link between gut and brain. The reductions in bifidobacteria identified in some IBS studies [35, 36] have also been associated with impaired gut barrier function (possibly mediated through TLRs [40, 41] and/or tight junction proteins). Altered signaling by muscle-residing macrophages and secretion of cytokines, both of which may be influenced by the gut microbiota, have also been suggested to affect inflammatory responses and gut motility, possibly via effects on the interstitial cells of Cajal [54] that again are mediated by TLR signaling [55]. Lastly, serotonin (produced by intestinal enterochromaffin cells) and histamine (produced by mast cells in the mucosa) have been shown to affect inflammation and intestinal barrier integrity [56], and serotonin has also been implicated in visceral hypersensitivity. Gut microbiota appear to modulate serotonin production [57], suggesting another potential mechanism by which gut microbes may affect the gut–brain axis and potentially contribute to IBS symptoms.
Recently, it has become apparent that beyond their interaction with the gut, microbes can influence the brains of their hosts including links to psychological symptoms [58]. For example, colonization of germ-free mice with microbiota from IBS-D patients with anxiety resulted in anxiety-like behavior in those mice but not in mice colonized with microbiota from IBS-D patients without anxiety or with healthy controls [59]. In a recent human study, changes in the microbiome of IBS patients appeared to determine patterns of brain activation [60]. These findings help to integrate the seemingly disparate brain–gut axis and microbial theories of IBS.
Treating the Microbiome in IBS
Given the mounting evidence that microbes have a role in IBS, research has examined many avenues of microbial manipulation including antibiotics, probiotics, and dietary changes.
Antibiotics
The growing role of the microbiome in IBS became the basis for trials using antibiotic approaches to treat IBS. Most studies have used poorly absorbed antibiotics, neomycin or rifaximin in particular, to elicit this effect. Another study showed that norfloxacin was successful in relieving IBS symptoms, including small intestinal bacterial overgrowth [61]. In some ways, the success of antibiotics to treat IBS may represent the strongest argument for the role of bacteria in IBS.
Neomycin was one of the first antibiotics to be studied systematically for IBS. In a randomized double-blind placebo-controlled trial of 111 IBS patients fulfilling standard diagnostic criteria comparing neomycin to placebo, neomycin resulted in a 35% improvement in composite scores of IBS symptoms, compared with only 11% for placebo (p < 0.05) [62]. Although neomycin alone was somewhat effective in treating IBS, it is used less often due to side effects.
Rifaximin is a non-systemic antibiotic for which a number of mechanisms of action have been proposed, including potential anti-inflammatory actions, and is the most comprehensively studied antibiotic explored in the treatment of IBS-D. In two identically designed phase III trials, a single 2-week treatment with rifaximin 550 mg three times daily in patients with non-constipated IBS resulted in significantly more patients reporting adequate relief of IBS (p = 0.01) and bloating (p = 0.005) [63]. Improvement in symptoms persisted for up to 10 weeks following cessation of treatment [63]. In a more recent phase III trial to assess the safety and efficacy of repeat rifaximin treatment, 692 IBS-D patients who initially responded to rifaximin and then relapsed were randomized to double-blind rifaximin or placebo for 14 days. More patients were found to respond to retreatment with rifaximin than placebo (38.1% vs. 31.5%) [64].
A meta-analysis of clinical trials found rifaximin to be more efficacious than placebo for global IBS symptom improvement (OR = 1.57; 95% CI = 1.22, 2.01; therapeutic gain = 9.8%; number needed to treat (NNT = 10.2), with mild heterogeneity (p = 0.25, I(2) = 26%) [65]. Importantly, rifaximin appears to have an acceptable side-effect profile with no difference in overall adverse events between the antibiotic and placebo groups. While the mechanism of rifaximin is not entirely determined, a rodent model revealed that rifaximin reduces bacterial levels in the small intestine, particularly the duodenum, but has lesser and more transient effects on colonic microbes, with stool coliform counts recovering within 3 days of cessation of treatment [66]. Due to its safety, rifaximin was approved by the FDA for the treatment of IBS-D.
Probiotics
Probiotics are widely available and may benefit patients with IBS through mechanisms that include modifying gut bacterial communities, mucosal immune function, mucosal barrier function, function of neuroendocrine cells, and fermentation [67]. Though clinical trials have evaluated the efficacy of probiotics in IBS patients, most suffer from serious methodological flaws. A recent meta-analysis that included 15 controlled trials concluded that probiotics reduce pain and symptom severity scores with a relative risk ratio for adequate improvement of IBS of 2.14 (95% CI: 1.08–4.26; p = 0.03) [68]. Despite this observed improvement, the optimal strain, dose, formulation, and duration of therapy have not yet been determined.
In probably the most notable study using probiotics to treat IBS, Bifidobacter infantis 35624 led to significant improvements in abdominal pain/discomfort, bloating/distention, and/or bowel movement difficulty compared with placebo (p < 0.05) in a randomized, blinded placebo-controlled trial conducted in IBS patients [69]. Few studies have evaluated the effects of probiotics specifically in subtypes of IBS, although a recent placebo-controlled trial evaluated a probiotic combination of three lactobacilli, three bifidobacteria, and Streptococcus thermophiles for 8 weeks in 50 patients with IBS-D. A significantly greater percentage of patients receiving the probiotic combination reported adequate relief of IBS compared to placebo (48% vs. 12%, p = 0.01 reporting adequate relief for > 50% of weeks). Stool consistency also improved significantly with probiotics versus placebo [70].
Effects of Diets for IBS on the Microbiome
The low-FODMAP (fermentable oligo-, di-, and monosaccharides and polyols) diet has gained the most attention in recent years in part on the basis that it restricts consumption of food that promotes microbial fermentation in the gut. The main dietary sources of FODMAPs include dairy, wheat and other grains, many fruits and vegetables, and artificial sweeteners. Accumulating evidence from retrospective and prospective controlled trials suggests dietary FODMAP restriction is associated with reduced fermentation and significant symptom improvement in a subset of IBS sufferers [71]. Restriction of both fructose and fructans appears necessary to achieve the full clinical benefits [72]. In a randomized sham-controlled single-blind crossover trial among IBS patients who had not previously tried dietary manipulation, participants reported a significant reduction in overall gastrointestinal symptom scores compared to those on a standard Australian diet (22.8 vs., 44.9; range 0–100, p < 0.001) [71]. Patients of all IBS subtypes had greater satisfaction with stool consistency while on the low-FODMAP diet, but IBS-D (n = 10) was the only subtype with improvement in altered fecal frequency [71]. A recent meta-analysis that included six clinical trials found that IBS patients administered a low-FODMAP diet had significant reduction in abdominal pain, bloating, and diarrhea [73]. Long-term follow-up (i.e., > 4 weeks) is lacking.
One challenge with the low-FODMAP diet is long-term use. Response to full FODMAP restriction is usually assessed after 4–6 weeks. Responders then engage in a structured reintroduction of FODMAP-containing foods, which allows the individual to tailor their diets. The complexity of the low-FODMAP diet and the need for a structured food reintroduction phase emphasize the critical role of a properly trained dietician in the IBS care team [74]. More importantly, a recent study indicated that a low-FODMAP diet can reduce stool microbiome diversity [75], a finding usually attributed to an “unhealthy” microbiome. Thus, long-term treatment with of low FODMAP requires further study.
Fecal Microbiota Transplantation
Fecal transplantation has been an exciting area of therapeutics, with most benefit seen in recurring C. difficile colitis. A recent Norwegian study found that when stool from healthy individuals was transplanted into IBS-D patients during colonoscopy, clinically meaningful improvement in symptoms (defined as a decrease in the IBS-SSS score of > 75 points) occurred in 65% (36 out 75) of patients at 3 months compared with 43% (12 out 28) of patients receiving their own stool. Patients had better results if they received frozen rather than fresh fecal microbiota transplantation [76]. However, another recent study found that while fecal transplantation did alter the gut microbiome in IBS subjects, those receiving placebo reported greater symptom relief than those receiving fecal transplantation [77]. The level of current interest in this subject is evidenced by three recently presented abstracts. On balance, results are not promising, but these data await scrutiny after peer-reviewed publication. These variable results illustrate that further data are needed before considering this approach in clinical practice.
Conclusions
There is ever-growing evidence supporting the role of microbes in the pathophysiology of IBS (Table 3). It is clear from an immense body of literature that exposure to a pathogen can be an important initiating event in the development of IBS, leading to a series of downstream events that may culminate in a change in gut colonization in IBS patients (Fig. 1). These data form the basis of a new microbial hypothesis in the pathogenesis of IBS. To date, antibiotics and diet have been first-generation attempts to correct microbial perturbations and provide relief from IBS symptoms. The evolving story of the microbiome has opened up the potential for new treatments for IBS, which target the underlying cause rather than focusing only on symptom remediation. The hope is that the future of IBS research will reduce suffering, cut costs, and avoid unnecessary testing. In addition, further research is needed to explore potential means of preventing IBS. While these include protecting against acute gastroenteritis through good hygiene, using precautions when traveling, and facilitating good water, sanitation and hygiene practices even after natural disasters, also important is identifying ways to prevent the progression to IBS, including chemoprophylaxis possibly in combination with screening for additional risk factors such as predictive cytokine and antibody panels. This review supports the concept that IBS is, at least in some patients, a microbiome-associated condition with promising therapies in the future based on a growing understanding of the disorder.
Key Messages
-
Post-infectious IBS following acute gastroenteritis is triggered by the development of antibodies to the bacterial toxin CdtB which, through molecular mimicry, leads to the development of autoimmunity to the host protein vinculin.
-
Anti-CdtB and anti-vinculin antibodies are useful in diagnosing IBS-D and distinguishing it from other causes of diarrhea such as IBD and celiac disease.
-
The gut microbiome is altered in IBS subjects. Specific findings include lower levels of Lactobacillus, Bifidobacterium, and Faecalibacterium prausnitzii in IBS.
-
Small intestinal bacterial overgrowth (SIBO) is associated with IBS-D, whereas increased levels of methanogenic archaea, specifically Methanobrevibacter smithii, are associated with IBS-C.
-
Alterations in the gut microbiome may lead to impaired gut barrier function, which in turn may affect the brain–gut axis and potentially contribute to IBS symptoms.
-
A low-FODMAP diet may result in improvements in abdominal pain, bloating, and diarrhea in IBS-D patients, but longer-term follow-up studies are needed to determine the effects on gut microbiome composition and diversity.
References
Choung RS, Locke GR 3rd. Epidemiology of IBS. Gastroenterol Clin N Am. 2011;40:1–10.
The Burden of Gasterointestinal Diseases. Bethesda, MD: American Gastroenterological Association; 2001.
Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131.
Chaudhary NA, Truelove SC. The irritable colon syndrome. A study of the clinical features, predisposing causes, and prognosis in 130 cases. Q J Med. 1962;31:307–322.
McKendrick MW, Read NW. Irritable bowel syndrome–post salmonella infection. J Infect. 1994;29:1–3.
Klem F, Wadhwa A, Prokop LJ, et al. Prevalence, risk factors, and outcomes of irritable bowel syndrome after infectious enteritis: a systematic review and meta-analysis. Gastroenterology. 2017;152:1042–1054.e1.
Goodsall TM, Talley NJ, Rassam L, et al. Unique pathology of colonic spirochaetosis characterised by mucosal eosinophilia is linked to diarrhoea and IBS. Gut. 2017;66:978.
Bonfiglio F, Zheng T, Garcia-Etxebarria K, et al. Female-specific association between variants on chromosome 9 and self-reported diagnosis of irritable bowel syndrome. Gastroenterology. 2018;155:168–179.
Sibelli A, Chalder T, Everitt H, Workman P, Windgassen S, Moss-Morris R. A systematic review with meta-analysis of the role of anxiety and depression in irritable bowel syndrome onset. Psychol Med. 2016;46:3065–3080.
Spreadbury I, Ochoa-Cortes F, Ibeakanma C, Martin N, Hurlbut D, Vanner SJ. Concurrent psychological stress and infectious colitis is key to sustaining enhanced peripheral sensory signaling. Neurogastroenterol Motil. 2015;27:347–355.
Murakami T, Kamada K, Mizushima K, et al. Changes in intestinal motility and gut microbiota composition in a rat stress model. Digestion. 2017;95:55–60.
Porter CK, Gloor K, Cash BD, Riddle MS. Risk of functional gastrointestinal disorders in U.S. military following self-reported diarrhea and vomiting during deployment. Dig Dis Sci. 2011;56:3262–3269. https://doi.org/10.1007/s10620-011-1762-3.
Koloski NA, Jones M, Talley NJ. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment Pharmacol Ther. 2016;44:592–600.
Akiho H, Deng Y, Blennerhassett P, Kanbayashi H, Collins SM. Mechanisms underlying the maintenance of muscle hypercontractility in a model of postinfective gut dysfunction. Gastroenterology. 2005;129:131–141.
Pimentel M, Chatterjee S, Chang C, et al. A new rat model links two contemporary theories in irritable bowel syndrome. Dig Dis Sci. 2008;53:982–989. https://doi.org/10.1007/s10620-007-9977-z.
Jee SR, Morales W, Low K, et al. ICC density predicts bacterial overgrowth in a rat model of post-infectious IBS. World J Gastroenterol. 2010;16:3680–3686.
Spiller RC, Jenkins D, Thornley JP, et al. Increased rectal mucosal enteroendocrine cells, T lymphocytes, and increased gut permeability following acute Campylobacter enteritis and in post-dysenteric irritable bowel syndrome. Gut. 2000;47:804–811.
Pimentel M, Soffer EE, Chow EJ, Kong Y, Lin HC. Lower frequency of MMC is found in IBS subjects with abnormal lactulose breath test, suggesting bacterial overgrowth. Dig Dis Sci. 2002;47:2639–2643. https://doi.org/10.1023/A:1021039032413.
Pokkunuri V, Pimentel M, Morales W, et al. Role of cytolethal distending toxin in altered stool form and bowel phenotypes in a rat model of post-infectious irritable bowel syndrome. J Neurogastroenterol Motil. 2012;18:434–442.
Pimentel M, Morales W, Pokkunuri V, et al. Autoimmunity links vinculin to the pathophysiology of chronic functional bowel changes following campylobacter jejuni infection in a rat model. Dig Dis Sci. 2015;60:1195–1205. https://doi.org/10.1007/s10620-014-3435-5.
Shen K, Tolbert CE, Guilluy C, et al. The vinculin C-terminal hairpin mediates F-actin bundle formation, focal adhesion, and cell mechanical properties. J Biol Chem. 2011;286:45103–45115.
Ford AC, Talley NJ, Walker MM, Jones MP. Increased prevalence of autoimmune diseases in functional gastrointestinal disorders: case-control study of 23471 primary care patients. Aliment Pharmacol Ther. 2014;40:827–834.
Pimentel M, Morales W, Rezaie A, et al. Development and validation of a biomarker for diarrhea-predominant irritable bowel syndrome in human subjects. PLoS One. 2015;10:e0126438.
Chira A, Dumitrascu DL. Serum biomarkers for irritable bowel syndrome. Clujul Med. 2015;88:258–264.
Schmulson M, Balbuena R, Corona de Law C. Clinical experience with the use of anti-CdtB and anti-vinculin antibodies in patients with diarrhea in Mexico. Rev Gastroenterol Mex. 2016;81:236–239.
Pike BL, Paden KA, Alcala AN, et al. Immunological biomarkers in postinfectious irritable bowel syndrome. J Travel Med. 2015;22:242–250.
Maxwell PR, Rink E, Kumar D, Mendall MA. Antibiotics increase functional abdominal symptoms. Am J Gastroenterol. 2002;97:104.
Paula H, Grover M, Halder SL, et al. Non-enteric infections, antibiotic use, and risk of development of functional gastrointestinal disorders. Neurogastroenterol Motil. 2015;27:1580–1586.
Codling C, O’Mahony L, Shanahan F, Quigley EM, Marchesi JR. A molecular analysis of fecal and mucosal bacterial communities in irritable bowel syndrome. Dig Dis Sci. 2010;55:392–397. https://doi.org/10.1007/s10620-009-0934-x.
Carroll IM, Ringel-Kulka T, Siddle JP, Ringel Y. Alterations in composition and diversity of the intestinal microbiota in patients with diarrhea-predominant irritable bowel syndrome. Neurogastroenterol Motil. 2012;24:521–530, e248.
Jeffery IB, O’Toole PW, Ohman L, et al. An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut. 2012;61:997–1006.
Ng SC, Lam EF, Lam TT, et al. Effect of probiotic bacteria on the intestinal microbiota in irritable bowel syndrome. J Gastroenterol Hepatol. 2013;28:1624–1631.
Giamarellos-Bourboulis E, Tang J, Pyleris E, et al. Molecular assessment of differences in the duodenal microbiome in subjects with irritable bowel syndrome. Scand J Gastroenterol. 2015;50:1076–1087.
Maharshak N, Ringel Y, Katibian D, et al. Fecal and mucosa-associated intestinal microbiota in patients with diarrhea-predominant irritable bowel syndrome. Dig Dis Sci. 2018;63:1890–1899. https://doi.org/10.1007/s10620-018-5086-4.
Ponnusamy K, Choi JN, Kim J, Lee SY, Lee CH. Microbial community and metabolomic comparison of irritable bowel syndrome faeces. J Med Microbiol. 2011;60:817–827.
Rajilic-Stojanovic M, Biagi E, Heilig HG, et al. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology. 2011;141:1792–1801.
Liu HN, Wu H, Chen YZ, Chen YJ, Shen XZ, Liu TT. Altered molecular signature of intestinal microbiota in irritable bowel syndrome patients compared with healthy controls: a systematic review and meta-analysis. Dig Liver Dis. 2017;49:331–337.
Tap J, Derrien M, Tornblom H, et al. Identification of an intestinal microbiota signature associated with severity of irritable bowel syndrome. Gastroenterology. 2017;152:111–123 e8.
Crouzet L, Gaultier E, Del’Homme C, et al. The hypersensitivity to colonic distension of IBS patients can be transferred to rats through their fecal microbiota. Neurogastroenterol Motil. 2013;25:e272–e282.
Brint EK, MacSharry J, Fanning A, Shanahan F, Quigley EM. Differential expression of toll-like receptors in patients with irritable bowel syndrome. Am J Gastroenterol. 2011;106:329–336.
McKernan DP, Gaszner G, Quigley EM, Cryan JF, Dinan TG. Altered peripheral toll-like receptor responses in the irritable bowel syndrome. Aliment Pharmacol Ther. 2011;33:1045–1052.
Ringel Y. The gut microbiome in irritable bowel syndrome and other functional bowel disorders. Gastroenterol Clin N Am. 2017;46:91–101.
Shah ED, Basseri RJ, Chong K, Pimentel M. Abnormal breath testing in IBS: a meta-analysis. Dig Dis Sci. 2010;55:2441–2449. https://doi.org/10.1007/s10620-010-1276-4.
Posserud I, Stotzer PO, Bjornsson ES, Abrahamsson H, Simren M. Small intestinal bacterial overgrowth in patients with irritable bowel syndrome. Gut. 2007;56:802–808.
Pyleris E, Giamarellos-Bourboulis EJ, Tzivras D, Koussoulas V, Barbatzas C, Pimentel M. The prevalence of overgrowth by aerobic bacteria in the small intestine by small bowel culture: relationship with irritable bowel syndrome. Dig Dis Sci. 2012;57:1321–1329. https://doi.org/10.1007/s10620-012-2033-7.
Kunkel D, Basseri RJ, Makhani MD, Chong K, Chang C, Pimentel M. Methane on breath testing is associated with constipation: a systematic review and meta-analysis. Dig Dis Sci. 2011;56:1612–1618. https://doi.org/10.1007/s10620-011-1590-5.
Pimentel M, Lin HC, Enayati P, et al. Methane, a gas produced by enteric bacteria, slows intestinal transit and augments small intestinal contractile activity. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1089–G1095.
Miller TL, Wolin MJ. Enumeration of Methanobrevibacter smithii in human feces. Arch Microbiol. 1982;131:14–18.
Pimentel M, Chang C, Chua KS, et al. Antibiotic treatment of constipation-predominant irritable bowel syndrome. Dig Dis Sci. 2014;59:1278–1285. https://doi.org/10.1007/s10620-014-3157-8.
Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: the North American consensus. Am J Gastroenterol. 2017;112:775–784.
Raskov H, Burcharth J, Pommergaard HC, Rosenberg J. Irritable bowel syndrome, the microbiota and the gut–brain axis. Gut Microbes. 2016;7:365–383.
Bhattarai Y, Muniz Pedrogo DA, Kashyap PC. Irritable bowel syndrome: a gut microbiota-related disorder? Am J Physiol Gastrointest Liver Physiol. 2017;312:G52–G62.
Dlugosz A, Nowak P, D’Amato M, et al. Increased serum levels of lipopolysaccharide and antiflagellin antibodies in patients with diarrhea-predominant irritable bowel syndrome. Neurogastroenterol Motil. 2015;27:1747–1754.
Mikkelsen HB. Interstitial cells of Cajal, macrophages and mast cells in the gut musculature: morphology, distribution, spatial and possible functional interactions. J Cell Mol Med. 2010;14:818–832.
Anitha M, Vijay-Kumar M, Sitaraman SV, Gewirtz AT, Srinivasan S. Gut microbial products regulate murine gastrointestinal motility via toll-like receptor 4 signaling. Gastroenterology. 2012;143:1006–1016.e4.
Wouters MM, Vicario M, Santos J. The role of mast cells in functional GI disorders. Gut. 2016;65:155–168.
Yano JM, Yu K, Donaldson GP, et al. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 2015;161:264–276.
Foster JA, Rinaman L, Cryan JF. Stress and the gut–brain axis: regulation by the microbiome. Neurobiol Stress. 2017;7:124–136.
De Palma G, Lynch MDJ, Lu J, et al. Transplantation of fecal microbiota from patients with irritable bowel syndrome alters gut function and behavior in recipient mice. Sci Transl Med. 2017;9:eaaf6397.
Labus JS, Hollister EB, Jacobs J, et al. Differences in gut microbial composition correlate with regional brain volumes in irritable bowel syndrome. Microbiome. 2017;5:49.
Ghoshal UC, Srivastava D, Misra A, Ghoshal U. A proof-of-concept study showing antibiotics to be more effective in irritable bowel syndrome with than without small-intestinal bacterial overgrowth: a randomized, double-blind, placebo-controlled trial. Eur J Gastroenterol Hepatol. 2016;28:281–289.
Pimentel M, Chow EJ, Lin HC. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome. A double-blind, randomized, placebo-controlled study. Am J Gastroenterol. 2003;98:412–419.
Pimentel M, Lembo A, Chey WD, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22–32.
Lembo A, Pimentel M, Rao SS, et al. Repeat treatment with rifaximin is safe and effective in patients with diarrhea-predominant irritable bowel syndrome. Gastroenterology. 2016;151:1113–1121.
Menees SB, Maneerattannaporn M, Kim HM, Chey WD. The efficacy and safety of rifaximin for the irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2012;107:28–35.
Kim MS, Morales W, Hani AA, et al. The effect of rifaximin on gut flora and Staphylococcus resistance. Dig Dis Sci. 2013;58:1676–1682. https://doi.org/10.1007/s10620-013-2675-0.
Borowiec AM, Fedorak RN. The role of probiotics in management of irritable bowel syndrome. Curr Gastroenterol Rep. 2007;9:393–400.
Didari T, Mozaffari S, Nikfar S, Abdollahi M. Effectiveness of probiotics in irritable bowel syndrome: updated systematic review with meta-analysis. World J Gastroenterol. 2015;21:3072–3084.
O’Mahony L, McCarthy J, Kelly P, et al. Lactobacillus and bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology. 2005;128:541–551.
Ki Cha B, Mun Jung S, Hwan Choi C, et al. The effect of a multispecies probiotic mixture on the symptoms and fecal microbiota in diarrhea-dominant irritable bowel syndrome: a randomized, double-blind, placebo-controlled trial. J Clin Gastroenterol. 2012;46:220–227.
Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;146:67–75.e5.
Shepherd SJ, Parker FC, Muir JG, Gibson PR. Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence. Clin Gastroenterol Hepatol. 2008;6:765–771.
Altobelli E, Del Negro V, Angeletti PM, Latella G. Low-FODMAP diet improves irritable bowel syndrome symptoms: a meta-analysis. Nutrients. 2017;9:940.
Eswaran SL, Chey WD, Han-Markey T, Ball S, Jackson K. A randomized controlled trial comparing the low FODMAP diet vs modified NICE guidelines in US adults with IBS-D. Am J Gastroenterol. 2016;111:1824–1832.
Hill P, Muir JG, Gibson PR. Controversies and recent developments of the low-FODMAP diet. Gastroenterol Hepatol NY. 2017;13:36–45.
Johnsen PH, Hilpüsch F, Cavanagh JP, et al. Faecal microbiota transplantation versus placebo for moderate-to-severe irritable bowel syndrome: a double-blind, randomised, placebo-controlled, parallel-group, single-centre trial. Lancet Gastroenterol Hepatol. 2018;3:17–24.
Halkjaer SI, Christensen AH, Lo BZS, et al. Faecal microbiota transplantation alters gut microbiota in patients with irritable bowel syndrome: results from a randomised, double-blind placebo-controlled study. Gut. 2018;67:2107–2115.
Kerckhoffs AP, Samsom M, van der Rest ME, et al. Lower Bifidobacteria counts in both duodenal mucosa-associated and fecal microbiota in irritable bowel syndrome patients. World J Gastroenterol. 2009;15:2887–2892.
Kerckhoffs AP, Ben-Amor K, Samsom M, et al. Molecular analysis of faecal and duodenal samples reveals significantly higher prevalence and numbers of Pseudomonas aeruginosa in irritable bowel syndrome. J Med Microbiol. 2011;60:236–245.
Rangel I, Sundin J, Fuentes S, et al. The relationship between faecal-associated and mucosal-associated microbiota in irritable bowel syndrome patients and healthy subjects. Aliment Pharmacol Ther 2015;42:1211–1221.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MP is a consultant for and has received grant support from Salix Pharmaceuticals. MP also consults for US Medical and Shire. MP has equity in and consults for Gemelli Biotech, Naia Pharmaceuticals, and Synthetic Biologics. Cedars-Sinai has licensing agreements with Bausch Health, Naia Pharmaceuticals, Synthetic Biologics and Gemelli Biotech. AL has served on the advisory boards for Allergen, Salix Pharmaceuticals, Valeant Pharmaceuticals, Alkermes, Arena, Aoen Biopharma, Takeda, Bioamerica and Ironwood Pharmaceuticals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pimentel, M., Lembo, A. Microbiome and Its Role in Irritable Bowel Syndrome. Dig Dis Sci 65, 829–839 (2020). https://doi.org/10.1007/s10620-020-06109-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06109-5