Abstract
Background and Aims
Self-expandable metallic stent insertion has been a mainstream treatment for relieving the obstructive symptoms of malignant gastric outlet obstruction (MGOO), a late-stage complication of gastrointestinal malignancies. This study aims to investigate the predictive value of stent expansion rates in clinical outcomes in patients with MGOO.
Methods
Eighty-seven patients with inoperable MGOO receiving metallic stents were reviewed retrospectively from April 2010 to December 2014. Clinical outcomes, predictors of stent patency, and survival were analyzed.
Results
The technical and clinical success rates were 100 and 94.3%, respectively. The median stent patency time was 114 days (range 13–570 days). The median survival time was 133 days (range 13–1145 days). Stent dysfunctions occurred in 28 patients (32.2%), with restenosis accounting for the majority (82%). The stent expansion rate ≥75% at Day 1 predicted the stent patency [hazard ratio (HR) 0.12, P = 0.04]. However, it did not correlate with survival. Non-gastric cancer origins (HR 2.41, P = 0.002) and peritoneal carcinomatosis (HR 2.54, P = 0.001) correlated with poor survival. However, post-stent chemotherapy (HR 0.55, P = 0.03) was related to better outcome. The comparison of clinical outcomes of first and second stent insertions showed no significant difference in the stent expansion rate either at Day 0 and Day 1 (P = 0.97 and P = 0.57).
Conclusions
Self-expandable metallic stent insertion is a safe and effective treatment for relieving the obstructive symptoms. The stent expansion rate ≥75% at Day 1 is a novel stent-related predictor of stent patency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant gastric outlet obstruction (MGOO) is a late complication of gastrointestinal malignancies, causing nausea, vomiting, poor appetite, and a decrease in the quality of life. MGOO has historically been treated by gastrojejunostomy as a palliative method; however, self-expandable metallic stent (SEMS) insertion has recently been introduced as another palliative treatment. Several studies have investigated the comparison between SEMS and gastrojejunostomy. SEMS has several advantages over gastrojejunostomy, including early time to oral intake, rapid symptom relief, less morbidity and mortality, shorter length in hospital stays and decreased costs [1–4]. Three randomized controlled studies have further confirmed the advantages of SEMS. Fiori et al. [5] found that the endoscopic stenting had shorter operation time, restoration of oral intake and length of hospitalization compared with gastroenterostomy. Jeurnink et al. [6] reported that there were better short-term outcomes of earlier food intake and lower total costs for stent placement. Mehta et al. [7] demonstrated that stent placement offered advantages of less pain scores, shorter hospital stay and improvement in physical health at 1 month objectively compared with gastrojejunostomy. In addition, most patients suffering from gastric outlet obstruction have limited life expectancies and multiple comorbidities and are not suitable for surgery; thus, SEMS insertion, as a minimally invasive procedure, becomes the mainstream management in MGOO.
Several studies have attempted to find out the prognostic predictors of the resumption of oral intake after stent insertion and stent patency time. Peritoneal carcinomatosis, ascites, and poor performance status were predictors of poor clinical success [8–10]. We have identified the GOOSS 3-point at Day 7 as a novel predictor of stent patency in our previous report [11]; however, all of these known predictors originated from diseases themselves or patients’ conditions which might be judged subjectively. Interestingly, Hori et al. [12] reported that the stent underexpansion <30% on the procedure day is a predictor of poor oral intake. This is the first study to find stent-related prognostic factors of oral intake. We aim to further extend the ideas to identify the cut-off values of stent expansion rates and find the relationship between stent expansion rates and clinical outcomes in our patients.
Methods
Patients
Eighty-seven consecutive patients with inoperable intraabdominal malignancies causing MGOO receiving metallic stent placement at Taipei Veterans General Hospital were recruited retrospectively from April 2010 to December 2014. These patients were referred for the obstructive symptoms and did not receive metallic stent insertion before. After stent insertions, the patients receiving chemotherapy or radiotherapy were followed up when they came back for chemotherapy or radiotherapy. For patients not receiving chemotherapy or radiotherapy, they were suggested to be followed up at day 7 and day 30 after stent deployment, then once every two weeks or when they were symptomatic. All included patients were followed up to death or till March 2015. This study was approved by Institutional Review Board of Taipei Veterans General Hospital. Informed consent was obtained from all individual participants included in the study.
Stent Placement
A computed tomography scan and upper gastrointestinal (UGI) endoscopy were performed to evaluate the site and the length of stricture several days before the stent placement. Then, patients received the nasogastric tube insertion for drainage to minimize the risk of aspiration and to improve gastric emptying during the procedure.
All metallic stents were deployed by UGI endoscopes with wide-caliber working channels (GIF-2T240 or GIF-2TQ260M; Olympus, Tokyo, Japan) under fluoroscopic guidance as we previously described [11].
Briefly, we advanced the endoscope to the stricture site. A guide wire (Hydra Jagwire, Boston Scientific Corporation, USA) was introduced into the working channel of the scope 15–20 cm beyond the stricture site. Then, the length and location of the stricture were identified by injecting water-soluble contrast. The length of stent was determined by the stricture length with an additional 2–3 cm on each side to ensure adequate margins after placement. The uncovered stents, either WallFlex Single-use Duodenal Stent (Boston Scientific Corporation, USA) or Bonastent Pyloric/Duodenal (Standard SCI.Tech Inc, South Korea), were then deployed with fluoroscopic guidance. Abdominal plain films were taken immediately after the stent deployment and were suggested to be followed up on the next day to observe the extent of stent expansion. If recurrences of obstructive symptoms occurred during the follow-up period, a UGI endoscopy and a computed tomography scan were performed to evaluate the cause of obstruction. The second metallic stents were then inserted in some patients to relieve obstructive symptoms via the stent-in-stent technique.
Evaluation of the Degrees of Gastric Outlet Obstruction
The degrees of obstruction were evaluated by the Gastric Outlet Obstruction Scoring System (GOOSS) [13]. The system scores are based on the competence of diet intake, arrayed in a 4-point scale: 0 for no intake, 1 for liquid diet only, 2 for soft diet and 3 for regular diet.
Definitions
Technical success was defined as proper stent locations crossing the stricture site and adequate stent expansions. Clinical success was assumed to be the resolution of obstructive symptoms and improvement of at least 1 point on the GOOSS scores at Day 7.
Procedure-related adverse events were classified as minor and major events. The minor events were defined as not life-threatening events including abdominal pain, nausea, and vomiting. The major events were life-threatening events, including aspiration pneumonia, sepsis, bleeding, or perforation.
Stent patency time was defined as the period between stent insertion and stent restenosis. Apart from the restenosis, the death or till March 2015 were also the censors of stent patency.
Stent dysfunctions were defined as recurrences of obstructive symptoms and failures of resuming oral intake. They were classified as restenosis, migration or fracture by fluoroscopic images or UGI endoscopy findings.
The stent expansion rate was defined as the minimal diameter at stricture site of the body divided by the maximum diameter of stent body and multiplied by 100% on the procedure day and the next day if plain films were taken as our suggestion. We also collected the stent expansion rate at Day 7 and Day 30 if plain films were available for any reasons. All stent diameters were measured by two gastroenterologists who were blind to the patients’ clinical data using the smart-iris system (Informer Technologies, Inc., version 1.3.0.10). Then, we calculated the average of two measurements to determine the final diameter. In order to avoid the bias during measurement of stent diameters under different fluorescence imaging sources and settings, the measured minimal diameter of body at stricture site divided by the measured diameter of end then multiplied by the maximal diameter of end as the actual minimal diameter of body. We used the actual minimal diameter of body divided by the maximal diameter of body multiplied by 100% to get the stent expansion rate (Fig. 1).
The schematic estimation of stent expansion rate. The minimal diameter of stent body (mB) at stricture site and diameter of stent end (mE) were measured, then, the ratio kappa (κ), defined by mE/ME (ME, maximal diameter of end on full expansion of stent; 27 mm for WallFlex stent and 25 mm for Bonastent) for correction was obtained. The value of mB was divided by kappa to get aB (actual minimal diameter of stent body). Finally, the value of aB was divided by the value of MB (maximal diameter of body on full expansion of stent; 22 mm for WallFlex stent and 20 mm for Bonastent) times 100% to get stent expansion rate
Data Collection
All data were obtained from patients’ medical records including radiologic reports, procedure reports, and blood biochemistry exams. The collected data included the baseline characteristics, the Eastern Cooperative Oncology Group (ECOG) status, cancer origins, cancer stages, albumin values, receiving chemotherapy/radiotherapy or not, GOOSS values, adverse events, stent patency time, survival time, and the diameters of stent expansion.
Statistic Analysis
The continuous variables are presented as mean ± standard deviation (SD) or number (percentage). The stent patency time and survival time were expressed as median (range). The stent expansion rates at Day 0, Day 1, Day 7, and Day 30 were compared by paired-t test. The univariate analysis of stent patency and survival were analyzed by the Kaplan–Meier analysis and compared by the log-rank test. Variables with P values <0.05 in the univariate analysis were evaluated subsequently by the multivariate analysis. The multivariate analysis was analyzed by the Cox regression model. Significance is defined only at a P value <0.05. The clinical outcome between first and second stent insertion was compared by the paired-t test. The selection for cut-off values of the stent expansion rate and the change of expansion rate was determined by the Youden index of the Area under Receiver Operating Characteristic Curve (AUROC) analysis. The optimal values were about 50% of stent expansion at Day 0 and 75% at Day 1. The AUROC values were 0.627 at Day 0 (P = 0.098, confidence interval (CI) 0.497–0.758) and 0.671 at Day 1 (P = 0.026, CI 0.549–0.796). Thus, 75% stent expansion at Day 1 was selected for the subsequent analyses so as to avoid the statistic interference. All the statistical analyses were conducted by Statistical Package for the Social Sciences (IBM Corporation, Armonk, NY).
Results
Patients’ Demographic Characteristics
The patients’ baseline characteristics are shown in Table 1. Seventy-seven patients died during the followed up period. The other ten patients were followed up till March 2015. The mean age of our study group was 71.1 years old with 58 males (66.7%). Fifty-four patients (62.1%) had advanced performance status (ECOG ≥ 2). The main etiologies of MGOO were gastric cancer (67.8%), followed by cholangiocarcinoma (18.4%) and then pancreatic cancer (12.6%). These patients were inoperable with 73 patients (83.9%) already at Stage IV. Most obstruction sites were at the pylorus (48.3%). Peritoneal carcinomatosis was detected in 38 patients (43.7%). Among these recruited patients, 53 patients (60.9%) failed to resume any oral intake.
Clinical Outcomes
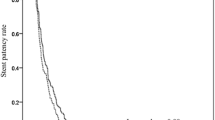
The clinical outcomes are summarized in Table 2. Technical success was achieved in all patients (100%). Clinical success was attained in 82 patients (94.3%). The mean GOOSS values improved from 0.41 (before stent placement) to 2.34 (after stent placement at Day 7, P < 0.001). The median stent patency time of the first stent was 114 days (range 13–570 days). The median survival time was 133 days (range 13–1145 days). The stent patency time and survival time are shown in Figs. 2 and 3, respectively. Stent dysfunctions were observed in 28 patients (32.2%) with 23 patients suffering from restenosis.
Procedure-related adverse events occurring in our study are listed in Table 2. Three major adverse events happened in the follow-up period. Two patients (2.8%) suffered from aspiration pneumonia after stent placement. One recovered after medical treatment and was discharged one week later. However, the other patient died of respiratory failure three days later because of no further resuscitation requested by the patient. One patient developed sepsis after stent placement and recovered after antibiotic treatment. The minor adverse events in our study consisted of abdominal pain, nausea, and vomiting. All patients were treated medically and improved after several days.
Stent Expansion
The mean diameter of stent expansion was 8.7 ± 3.4 mm at Day 0 immediately after stent insertion and 13.8 ± 3.6 mm at Day 1. The mean stent expansion rate was 41.8 ± 16.9% at Day 0 and 66.1 ± 17.7% at Day 1. The change of stent expansion rate from Day 0 to Day 1 was 24.5 ± 12.2%. During the follow-up period, the mean stent expansion rate was 76.6 ± 12.6% in 35 patients at Day 7 and 81.2 ± 11.3% in 36 patients at Day 30 (Fig. 4). The subgroup analysis of the stent expansion rate with different brands was performed. The expansion rate at Day 0 was 36.1 ± 13.0% for WallFlex stent and 46.9 ± 18.4% for Bonastent. The expansion rate at Day 1 was 62.3 ± 14.6% for WallFlex stent and 69.1 ± 19.4% for Bonastent. The Bonastent significantly expanded more rapidly than the WallFlex stent initially (P = 0.002). However, the difference did not exist at Day 1 (P = 0.09).
Predictive Factors for Stent Restenosis
In the univariate analysis, the GOOSS 3-point at Day 7 and the stent expansion ≥75% at Day 1 were predictive factors of stent patency. However, in the multivariate analysis, only the stent expansion ≥75% at Day 1 was the independent protective factor of stent patency (Table 3; Fig. 5).
Predictive Factors for Survival
In the univariate analysis, the advanced ECOG status, non-gastric cancer origin, stage IV status, no post-stent chemotherapy, peritoneal carcinomatosis, and a GOOSS score <3 points at Day 7 were poor prognostic factors. However, in the multivariate analysis, only tumor origin, post-stent chemotherapy, and peritoneal carcinomatosis were significantly associated with survival (Table 4).
Comparison of Clinical Outcomes Between First and Second Stent Insertion
Fifteen of 87 patients suffered from the recurrence of obstruction and received the second metallic stent insertion for symptom reliefs. The causes of recurrence of obstruction included stent fractures in two patients and restenosis in the other 13 patients. The median survival time after the second stent placement was 70 days (range 8–281 days). The comparison of clinical outcomes in the first and second stent placement is shown in Table 5. Although the stent expansion rates between the first and second stents were similar, the patency time, albumin levels, GOOSS values at Day 7 and Day 30 were significantly reduced after the second stent insertion while comparing those of the first stent insertion.
Discussion
In this study, stent expansion rate ≥75% at Day 1 is found to be a novel predictive factor of stent patency. This is the first study to find an objective stent-related parameter to predict stent patency. We can carefully monitor and follow the patients with poor stent expansion rate at Day 1.
Because of the importance of SEMS insertion in MGOO, some studies have aimed to find out the predictors of stent patency or poor oral intake to guide treatment. We previously identified the GOOSS 3-point at Day 7 as a novel predictor for stent patency [11]. Kim et al. [14] found palliative chemotherapy correlated with stent patency but carcinoembryonic antigen (CEA) levels were in contrast. Canena et al. [15] found the obstruction level at duodenum was associated with stent patency. Carcinomatosis, ascites, and poor performance status were correlated with poor predictive factors of food intake [8–10]. However, most of the above predictors were disease-related or had to use scoring systems which still needed to be judged subjectively. We anticipated identifying other more objective and stent-related predictive factors of stent patency. Recently, Hori et al. [12] reported the stent under expansion on the procedure day predicted poor oral intake. Thus, we further extended the idea to find out whether the stent expansion rate on the procedure day as well as the following day could predict stent patency. Interestingly, stent expansion rate ≥75% at Day 1 was found to be novel predictive factor for stent patency in the univariate analysis. Even compared with the GOOSS 3-point at Day 7 in the multivariate analysis, the stent expansion rate ≥75% at Day 1 was still the only independent predictor for stent patency.
We also found the extent of stent expansion gradually increased in the first month. Although no maximal extent of stent expansion could be attained during the 1 month follow-up, the trend of stent expansions seemed to be stabilized. We only analyzed the stent expansion rates at Day 0 and Day 1 to predict stent patency, because many patients did not receive abdominal plain film exams at Day 7 and Day 30. Tumor ingrowth might occur during the follow-up period because of uncovered stents insertions in these patients. In this situation, the extent of stent expansion could not represent the actual stent luminal patency.
The rates of stent expansion differed in the two brands of stents. The Bonastent expanded more rapidly than the WallFlex stent at Day 0 but the difference disappeared at Day 1. Even though the difference in speed of stent expansion existed at Day 0, the stent brands still did not correlate with stent patency in this study.
Few previous studies have demonstrated that the second stent insertion could effectively and safely relieve the stent dysfunctions, such as restenosis, migration, and even fractures [10, 16, 17]. However, the information of the clinical outcomes from the second stent insertions was limited. Sato et al. [10] reported the comparable results between first and second stent placements in clinical success, median stent patency, and tolerable oral intake to death or study terminations after second stent placement. In our study, we further analyzed the 15 patients receiving the second stent insertion for the recurrent obstruction. In contrast to Sato’s report, we found this to be statistically significant in decreasing stent patency time, GOOSS values at Day 7 and Day 30 in patients receiving the second stent insertion. These findings might be attributed to the development of multiple strictures in distal gastrointestinal tracts or peritoneal carcinomatosis. In fact, 10 of the 15 patients had obvious evidence of peritoneal seeding by CT scans on the second stent insertion. As disease progressed, some patients refused to receive further image exams or UGI endoscopy because of terminal stages. Thus, the real patient numbers with peritoneal carcinomatosis might be higher than the estimated numbers. This could be also the reason for decreased patency time after the second stent insertion. Interestingly, the expansion rate of the second stent insertion at Day 0 and Day 1 could attain the similar extents as those of the first stent. This possibly implies the second stent could still attain the similar expansion effect as the first stent. However, the long-term clinical efficacy might be poor in these patients with terminal stages.
In this study, we predicted stent patency by the extent of uncovered stent expansions. However, the true capacity of oral intake must be determined by the intraluminal space of stent. In patients with uncovered stent insertion, some tumor parts would squeeze into the wire cells of the stents and caused a relatively smaller diameter of intraluminal space than the stent diameter. As time goes by, the tumor might progress and cause in-stent restenosis although the adequate expansion appearance of stents was still noted in abdominal plain film. Thus, the predictability of the uncovered metallic stent expansions should be in few days after the stent insertion. That might be one of our limitations because of the placement of uncovered stents. Further studies regarding the predictive values of covered metallic stent expansion rates in clinical outcomes of patients with MGOO are anticipated. Besides, the findings are based on the plain films taken after stent placement. Thus, we could not pick up the high risks patients for stent restenosis before the placement of stent. Thus, we do not know whether these patients would be more suitable for palliative gastrojejunostomy instead of the placement of metallic stents. Additionally, we could not analyze the roles of the axial and radial forces of these metallic stents on stent patency and stent expansion rate because of unavailability of this information due to commercial secrets. Further studies to elucidate the contributing factors determining the stent expansion rate before stent deployment are important. Moreover, for the patients with high risks of stent restenosis, further studies to investigate whether balloon dilatations in these patients can help to lengthen the stent patency time are anticipated. However, with this study, we can find out the patients with high risk of stent restenosis at Day 1 and plan to closely monitor these patients. If recurrent obstructions occur, they can receive the insertion of the second stent earlier, which may reduce the incidence of complications like aspiration pneumonia and prolonged poor nutrition. Our study is retrospective and the number of cases is relatively small, future prospective studies are still required to validate the new predictor.
In conclusion, stent expansion rate ≥75% at Day 1 could predict stent patency in patients with MGOO. The study findings are based on the previously taken plain films using a retrospective study. We should closely follow-up patients with poor stent expansion rate at Day 1. After inserting the second metallic stent, the extent of stent expansion at Day 0 and Day 1 still attained the similar extents as those of the first stent. However, the clinical efficacy of the second stent decreased compared to the first one.
Abbreviations
- SEMS:
-
Self-expandable metallic stent
- MGOO:
-
Malignant gastric outlet obstruction
- GOOSS:
-
Gastric outlet obstruction scoring system
- ECOG:
-
Eastern Cooperative Oncology Group
- UGI:
-
Upper gastrointestinal
- CT:
-
Chemotherapy
- RT:
-
Radiotherapy
- SD:
-
Standard deviation
- HR:
-
Hazard ratio
References
Del Piano M, Ballare M, Montino F, et al. Endoscopy or surgery for malignant GI outlet obstruction? Gastrointest Endosc. 2005;61:421–426.
Espinel J, Sanz O, Vivas S, et al. Malignant gastrointestinal obstruction: endoscopic stenting versus surgical palliation. Surg Endosc. 2006;20:1083–1087.
Roy A, Kim M, Christein J, Varadarajulu S. Stenting versus gastrojejunostomy for management of malignant gastric outlet obstruction: comparison of clinical outcomes and costs. Surg Endosc. 2012;26:3114–3119.
Hosono S, Ohtani H, Arimoto Y, Kanamiya Y. Endoscopic stenting versus surgical gastroenterostomy for palliation of malignant gastroduodenal obstruction: a meta-analysis. J Gastroenterol. 2007;42:283–290.
Fiori E, Lamazza A, Volpino P, et al. Palliative management of malignant antro-pyloric strictures. Gastroenterostomy vs. endoscopic stenting. A randomized prospective trial. Anticancer Res. 2004;24:269–271.
Jeurnink SM, Steyerberg EW, van Hooft JE, et al. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc. 2010;71:490–499.
Mehta S, Hindmarsh A, Cheong E, et al. Prospective randomized trial of laparoscopic gastrojejunostomy versus duodenal stenting for malignant gastric outflow obstruction. Surg Endosc. 2006;20:239–242.
Jeon HH, Park CH, Park JC, et al. Carcinomatosis matters: clinical outcomes and prognostic factors for clinical success of stent placement in malignant gastric outlet obstruction. Surg Endosc. 2014;28:988–995.
Sasaki T, Isayama H, Nakai Y, et al. Predictive factors of solid food intake in patients with malignant gastric outlet obstruction receiving self-expandable metallic stents for palliation. Dig Endosc. 2012;24:226–230.
Sato T, Hara K, Mizuno N, et al. Gastroduodenal stenting with Niti-S stent: long-term benefits and additional stent intervention. Dig Endosc. 2015;27:121–129.
Ye BW, Lee KC, Hsieh YC, et al. Self-expandable metallic stent placement in malignant gastric outlet obstruction: a comparison between 2 brands of stents. Medicine. 2015;94:e1208.
Hori Y, Naitoh I, Ban T et al. Stent underexpansion on the procedure day is a predictive factor for poor oral intake after metallic stenting for gastric outlet obstruction. J Gastroenterol Hepatol. 2015;30:1246–1251.
Piesman M, Kozarek RA, Brandabur JJ, et al. Improved oral intake after palliative duodenal stenting for malignant obstruction: a prospective multicenter clinical trial. Am J Gastroenterol. 2009;104:2404–2411.
Kim SH, Chun HJ, Yoo IK, et al. Predictors of the patency of self-expandable metallic stents in malignant gastroduodenal obstruction. World J Gastroenterol WJG. 2015;21:9134–9141.
Canena JM, Lagos AC, Marques IN, et al. Oral intake throughout the patients’ lives after palliative metallic stent placement for malignant gastroduodenal obstruction: a retrospective multicentre study. Eur J Gastroenterol Hepatol. 2012;24:747–755.
Kim CG, Choi IJ, Lee JY, et al. Outcomes of second self-expandable metallic stent insertion for malignant gastric outlet obstruction. Surg Endosc. 2014;28:281–288.
Sasaki T, Isayama H, Nakai Y, et al. Clinical outcomes of secondary gastroduodenal self-expandable metallic stent placement by stent-in-stent technique for malignant gastric outlet obstruction. Dig Endosc. 2015;27:37–43.
Acknowledgments
We thank Mr. Liao Dong-Ming for his excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by Institutional Review Board of Taipei Veterans General Hospital. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ye, BW., Chou, CK., Hsieh, YC. et al. Metallic Stent Expansion Rate at Day One Predicts Stent Patency in Patients with Gastric Outlet Obstruction. Dig Dis Sci 62, 1286–1294 (2017). https://doi.org/10.1007/s10620-017-4534-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4534-x