Abstract
Background/aims
Self-expandable metal stents (SEMSs) can be used for the palliation of malignant obstruction in the upper gastrointestinal tract. This study assessed the feasibility and efficacy of endoscopically inserted SEMSs for the palliation of malignant obstruction in the stomach and duodenum.
Methods
Between January 2011 and April 2014, 220 patients with gastric or duodenal obstruction due to malignancy underwent endoscopic SEMS insertion at Asan Medical Center. The associations of technical/clinical outcomes and complications with the type of stent and site of obstruction were analyzed.
Results
The 220 patients included 125 men (56.8 %) and 95 women (43.2 %); median patient age was 63 years. Fully covered, partially covered, and uncovered SEMSs were inserted into 16, 77, and 120 patients, respectively. Obstructions were located in the gastric outlet, including the duodenal bulb, in 106 patients, and in the duodenal second and third portions in 114 patients. Technical success was achieved in 213 of 220 patients (96.8 %) and clinical success in 184 of 213 (86.4 %). Clinical success rates were similar to the type of stent, but were significantly greater for gastric outlet (95/104, 91.3 %) than for duodenal (89/109, 81.7 %) obstructions (p = 0.039). Stent migration was observed in 20 patients (9.1 %) and stent obstruction in 51 (23.2 %). Rates of stent migration were significantly higher for fully covered (6/16, 37.5 %) than for partially covered (7/77, 9.1 %) and uncovered (7/120, 5.8 %) SEMSs (p < 0.001) and were significantly higher for gastric outlet (16/104, 15.4 %) than for duodenal (4/109, 1.2 %) obstructions (p = 0.003). Rates of stent obstruction were similar for fully covered (2/16, 12.5 %), partially covered (17/77, 22.1 %), and uncovered (32/120, 26.7 %) SEMSs (p = 0.409) and in patients with gastric outlet (26/104, 25.0 %) and duodenal (25/109, 22.9 %) obstruction (p = 0.724).
Conclusions
SEMS selection for malignant obstruction of the upper gastrointestinal tract depends on the site of obstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastric outlet obstruction (GOO) is a clinical syndrome characterized by epigastric abdominal pain and postprandial vomiting due to mechanical obstruction [1]. Until the late 1970s, benign disease was responsible for most cases of GOO in adults, with malignancy accounting for only 10–39 % [2]. By contrast, in recent decades, 50–80 % of obstructions have been attributable to malignancy [3, 4]. The most frequent causes of malignant GOO are pancreatic cancer and advanced gastric cancer [5].
There have been many changes over time in the treatment of malignant outlet obstruction. Although palliative surgery, including bypass through a gastrojejunostomy, was previously the treatment of choice, significant technical advances in stent development and endoscopic technology have increased the frequency of endoscopic stent insertion. Self-expandable metal stents (SEMSs) can be used in the palliation of patients with malignant gastric or duodenal obstruction and have been shown to restore oral feeding ability [6, 7].
Endoscopic insertion of SEMSs was shown to have technical success rates of 92–100 % and clinical success rates of 75–92 %; complications included perforation, obstruction, migration, and stent fracture [8–13]. The location or quality of the obstruction made the endoscopist choose a fully covered/partially covered/uncovered SEMS [8, 10, 14–16]. Several small studies compared these three stent types at different sites of obstruction, including the gastric outlet and duodenum [15, 17–20]. This study analyzed the feasibility and efficacy of endoscopically inserted SEMSs for the palliation of malignant obstruction according to the type of stent and the site of obstruction.
Methods
Patients
This retrospective study assessed 220 patients who underwent endoscopic SEMS insertion for the management of GOO caused by malignancy between January 2011 and April 2014 at Asan Medical Center, Seoul, Korea. Patients were deemed eligible if (1) they had GOO due to malignancy; (2) the obstruction was located from the distal one-third of the stomach to the second and third portions of the duodenum that could be reached by the endoscope; (3) they had Gastric Outlet Obstruction Scoring System (GOOSS) [21] scores of 0 (no oral intake) to 2 (soft solid diet); and (4) they had Eastern Cooperative Oncology Group (ECOG) performance status of 0–2. Patients with benign strictures in the GI tract or postoperative strictures without cancer recurrence, those who underwent stent insertion for any other reason, including endoscopic retrograde cholangiopancreatography (ERCP) or before gastric surgery, patients who had obstructions at any site other than the gastric outlet and proximal duodenum, and patients with a history of previous SEMS placement were excluded. Patients lost to follow-up within 7 days were also excluded. The flow diagram of the study population is shown in Fig. 1.
All patients provided informed consent to undergo the procedures, and the study protocol was approved by the Institutional Review Board of Asan Medical Center. The study protocol was in complete compliance with the Declaration of Helsinki, as revised in Edinburgh in 2000.
Procedures and follow-up schedule
Malignant GOO was diagnosed by clinical and endoscopic examination. Clinical suspicion was based on changes in the symptoms and signs of nausea, vomiting, reduced oral intake, abdominal discomfort, and/or abdominal distention. SEMSs, including Niti-S stents (Taewoong Medical, Seoul, Korea), Bona stents (Standard Sci-Tech, Seoul, Korea), Hanaro stents (M.I. Tech Co Ltd, Seoul, Korea), Boston stents (Boston Scientific, MA, USA), and S&G stents (S&G Biotech Inc, Seongnam, Korea), were inserted endoscopically. The center diameter of these stents ranged from 18 to 20 mm, and their length ranged from 6 to 14 cm (Fig. 2). The choice of covered, partially covered, or uncovered stent was based on the characteristics of the lesion and the operator’s experience. Stent insertion procedures were performed by five experienced endoscopists (JY Ahn, JH Lee, DH Kim, KD Choi, and HJ Song). Though few number of fully covered stents were used, among of them, five endoscopists had chosen one to eight fully covered stents. Another type of stents was similarly selected to 14–26 cases by each endoscopist. The SEMS was placed across the area of stenosis using the endoscope therapeutic canal over a metal guide under endoscopic guidance, with or without fluoroscopic control. The SEMS was subsequently released, and its position and location were assessed by endoscopy with/without fluoroscopy. Oral intake was started 1 day after SEMS insertion.
Definitions
Outcomes included rates of (1) technical success, (2) clinical success, (3) adverse events, (4) patency, and (5) overall survival. Technical success was defined as successful deployment of the SEMS across the stricture, with patency confirmed by a combination of endoscopy and fluoroscopy. Clinical success was defined as an improvement in obstructive symptoms and oral intake after SEMS placement. The degree of oral intake was assessed using the GOOSS before and 7 days after stent insertion, with scores of 0–3 indicating no oral intake, an exclusively liquid diet, an exclusively soft solid diet, and a full diet, respectively. Performance status was assessed using the ECOG scale, with scores of 0–4 indicating normal activity, symptoms but ambulatory, in bed ≤50 % of the time, in bed >50 % of the time, and completely bedridden, respectively. The length of hospital stay was defined as the time from SEMS placement until hospital discharge or death. Complications were categorized as early (<1 week) or late (>1 week) after SEMS placement. Duration of patency was defined as the time between initial stent placement and the recurrence of obstructive symptoms caused by occlusion or migration of the stent because of tumor ingrowth or overgrowth. Patients were categorized as having peri-pyloric or duodenal obstruction, with peri-pyloric obstruction defined as obstruction of a site in the pylorus or bulb and duodenal obstruction as obstruction of a site on the second and/or third portion of the duodenum. If the patient had no obstructive symptoms, patency duration was regarded as equal to survival time. Survival duration was calculated as the time from SEMS insertion to death or the endpoint of this study, if the patient remained alive.
Statistical analysis
Continuous variables were expressed as mean and SD, and compared using Student’s t tests. Categorical variables were expressed as percentages and differences between groups (by obstruction site) compared using Chi-square tests. Cumulative patency and survival duration were evaluated by the Kaplan–Meier method and compared using log-rank tests. Two-sided p values <0.05 were defined as statistically significant. All statistical analyses were performed using IBM SPSS version 18.0 (SPSS Inc, Chicago, IL, USA).
Results
Baseline characteristics of patients with GOO
The characteristics of the patients are summarized in Table 1. Of the 220 patients, 125 (56.8 %) were male; median patient age was 63 years [interquartile range (IQR) 53.3–70.0 years]. The most frequent causes of obstruction were pancreatic cancer (32.3 %) and gastric cancer (31.8 %). Peri-pyloric obstructions were observed in 106 patients and were due to gastric cancer (n = 68, 64.2 %), cholangiocarcinoma (n = 12, 11.3 %), pancreatic cancer (n = 10, 9.4 %), gallbladder (GB) cancer (n = 6, 5.7 %), duodenal cancer (n = 3, 2.8 %), lymphoma (n = 1, 0.9 %), and metastasis (n = 6, 5.7 %). Duodenal obstructions were observed in 114 patients and were due to pancreatic cancer (n = 61, 53.5 %), cholangiocarcinoma (n = 20, 17.5 %), duodenal cancer (n = 9, 7.9 %), GB cancer (n = 5, 4.4 %), gastric cancer (n = 2, 1.8 %), and metastasis (n = 17, 14.9 %). The mean GOOSS score of all 220 patients before stent insertion was 0.94 ± 0.725, with no difference between patients with peri-pyloric and duodenal obstruction (0.98 ± 0.676 vs. 0.89 ± 0.768, p = 0.378).
Technical and clinical outcomes according to the type of stent and the site of obstruction
Table 2 shows the outcomes of stent insertion. Endoscopic stent placement was technically successful in 213 of 220 patients (96.8 %). Of these 213 patients, 16 (7.5 %), 77 (36.2 %), and 120 (56.3 %) patients underwent insertion of fully covered, partially covered, and uncovered SEMSs, respectively. Median stent width was 20 mm (IQR 20–20 mm), and median stent length was 80 mm (IQR 60–100 mm).
Clinical success rates were similar following the insertion of fully covered, partially covered, and uncovered SEMSs (93.8 vs. 88.3 vs. 84.2 %, respectively, p = 0.476). Technical failures were observed in seven patients and were due to the failure of guide-wire advance in two patients, acute angulation in one, and far distal obstruction site to reach through endoscopy in four. After technical failure, four patients were successfully treated radiologically, two received only supportive care, and one underwent bypass surgery.
Complications according to the type of stent and the site of obstruction
During a median follow-up of 2.8 months (IQR 1.2–5.6 months), stent migration was observed in 20 patients (9.1 %), obstruction in 51 (23.2 %), stent fracture in two (0.9 %), and bile duct obstruction in one (0.5 %) (Table 3). Of the 20 patients with stent migration, six (30 %) underwent a re-intervention, whereas 13 (65 %) received only supportive care. Of the 51 patients who experienced stent obstruction, 25 (49 %) received re-intervention therapy and three (5.9 %) underwent bypass surgery. Both patients with stent fracture received supportive care, and the one patient with bile duct obstruction underwent a re-intervention for bile drainage.
Table 4 shows the sub-analyses of outcomes and complications according to the type of stent and the site of obstruction. Complication rates following SEMS insertion into the peri-pyloric region were lowest for partially covered stents (13/36, 36.1 %), whereas complication rates following insertion into the duodenal region were lowest for uncovered stents (14/63, 22.2 %) (Table 4).
Early complications were observed in ten patients, at a median 5 days. Five of these patients received supportive care, whereas the others underwent endoscopic or radiological re-intervention. Late complications were observed in 64 patients, at a median 67 days. Management included supportive care in 33 patients, re-intervention in 27, and bypass surgery in 4. Patients with early and late complications did not differ significantly in site of obstruction or type of stent.
Outcomes of food intake capacity
Food intake capacity, which was calculated by GOOSS before and after stent placement, is summarized in Table 5. Mean GOOSS was significantly higher after than before stent placement (2.31 ± 0.782 vs. 0.94 ± 0.725, p < 0.001), but clinical success rate did not correlate with baseline GOOSS (Table 5). Mean GOOSS scores were higher after than before placement of fully covered stents (1.77 ± 0.267 vs. 1.03 ± 0.363, p = 0.138) and significantly higher after than before placement of partially covered (1.77 ± 0.102 vs. 0.95 ± 0.123, p < 0.001) and uncovered (1.73 ± 0.073 vs. 1.01 ± 0.094, p < 0.001) SEMSs. Mean GOOSS was significantly higher after than before stent placement in both the peri-pyloric (1.69 ± 0.095 vs. 0.94 ± 0.118, p < 0.001) and duodenal (1.74 ± 0.073 vs. 0.99 ± 0.095, p < 0.001) regions. For stent placement in the peri-pyloric area, mean GOOSS scores were higher after than before placement of fully covered stents (1.77 ± 0.267 vs. 0.94 ± 0.118, p = 0.138) and were significantly higher after than before placement of partially covered (1.77 ± 0.102 vs. 0.95 ± 0.123, p < 0.001) and uncovered (1.73 ± 0.073 vs. 1.01 ± 0.094, p < 0.001) SEMSs.
With GOOSS, the nutritional factor was calculated by albumin level after stent placement. However, there was no significantly difference between pre-stenting albumin level and poststenting albumin level (2.98 ± 0.62 vs. 2.95 ± 0.72, p = 0.492).
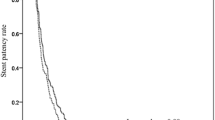
Patency duration and survival
The median stent patency period was 84 days (IQR 34.5–165.5 days), differing significantly in patients with clinical success and failure after stent insertion (141.64 ± 11.56 vs. 62.68 ± 17.43 days, p = 0.009; Fig. 3). However, patency duration was independent of obstruction site (p = 0.819) and stent type (p = 0.474). Median patient survival was 124 days (IQR 55.5–224.0 days), being significantly longer in patients with clinical success than in those with failure after stent insertion (188.35 ± 12.93 vs. 80.89 ± 20.19 days, p = 0.002).
Discussion
Malignant GOO is usually caused by pancreatic cancer, gastric cancer, and other metastatic cancers [3, 22]. Patients with GOO present with epigastric pain, nausea, vomiting, and poor oral intake. Dehydration and malnutrition also occur in these terminally ill patients and may precipitate their hospitalization.
This study showed that the clinical success rate of stent implantation was similar for the three stent types (fully covered, partially covered, and uncovered), but higher in the peri-pyloric than in the duodenal region. However, complication rates differed by stent type. In the peri-pyloric region, the complication rate was lower following placement of partially covered than fully covered and uncovered stents. In the duodenal region, however, complication rates were lower for placement of partially covered and uncovered stents than for placement of fully covered stents. These findings indicate that stent-type selection is dependent on the site of insertion. Covered stents have been associated with high rates of stent migration [23], and uncovered stents have been associated with high rates of stent obstruction [24]. A meta-analysis of the insertion of covered and uncovered stents showed a risk ratio (RR) for technical success rate of 1.00 (95 % confidential interval [CI] 0.98–1.01) and an RR for clinical success of 1.04 (95 % CI 0.98–1.11) [25]. A multicenter randomized trial of uncovered and covered stents showed that both groups had technical success rates of 100 % and comparable clinical success rates (93.5 vs. 87.1 %) [26]. The above-described meta-analysis found that covered stents were associated with a high rate of stent migration and uncovered stents were associated with a high rate of stent obstruction [25]. To overcome the complications of uncovered and covered stents, partially covered stents were developed to minimize the tumor ingrowth observed with uncovered stents and the stent migration observed with covered stents. Although these partially covered stents had technical and clinical success rates of 96.9 and 93.8 %, respectively [19], few studies to date have assessed the efficacy of partially covered stents for malignant GOO [15, 16].
This study compared success and complication rates with each type of stent according to the site of obstruction. In the peri-pyloric region, fully covered, partially covered, and uncovered stents had similar clinical success (100 vs. 94.4 vs. 87.7 %, p = 0.512) and complication (45.5 vs. 36.1 vs. 45.6 %, p = 0.652) rates. Although these three stent types had similar clinical success rates for duodenal lesions (80.0 vs. 82.9 vs. 81.0 %, p = 1.000), complication rates were significantly higher for fully covered (80.0 %) than for partially covered (29.3 %) and uncovered (22.2 %) stents (p = 0.023). Although fully covered stents were used in relatively few patients, partially covered stents may lower rates of overall complications, including migration and obstruction, when used for obstructions in the peri-pyloric region. For obstructions in the duodenal region, partially covered and uncovered stents are equally safe in reducing the risk of bile duct obstruction. As we mentioned previously, these characteristics of stent type and the operator’s preferences about complication occurrence are thought to affect the clinical success among the groups of stent type.
Few previous studies have evaluated stent placement according to the site of obstruction. An assessment of early re-stenosis relative to stenosis site found that obstruction was more frequent at the postoperative anastomosis site than at other duodenal and pyloric area sites [27]. Survival time was significantly longer following stent placement in the duodenum than across the pyloric valve, although the difference was not likely due to obstruction of the stent, because both groups had similar stent patency [28]. Our results, showing that the clinical success rate was higher for stent placement in the peri-pyloric area than in the duodenum, also showed that matching stent type with site of obstruction can reduce complication rates. We also found that the difference in clinical success was related to the main malignant obstruction in patients whom the stent placement was successful. In peri-pyloric region, advanced gastric cancer (68/104, 65.4 %) was the main cause of GOO; by contrast, the main cause of duodenal region was pancreatic cancer (57/104, 52.8 %). We think this difference in location of main tumor might have influenced on the clinical outcomes.
The GOOSS scale was introduced to grade the clinical degree of outlet obstruction, both before and after treatment [21], and stent placement was found to improve GOOSS scores [29, 30]. Similarly, we found that stent placement significantly improved GOOSS score and the ability to eat, but GOOSS scores did not correlate with clinical success. The primary cause of GOO in these patients was advanced gastric cancer. Therefore, these patients could not consume a full or regular diet due to decreased motility in the lower part of the stomach. Limited food intake relative to the median width of the stent (20 mm) and patient food preferences can affect change in GOOSS score after stent insertion.
Stent patency can be influenced by patient characteristics, underlying malignancy, and stent type. Median stent patency duration was reported to range from 9 to 23 weeks [25], with clinical success being the most important factor influencing stent patency [31]. Following clinical success, stent patency time was determined relative to the development of complications, including luminal obstruction of the stent due to tumor ingrowth, stent migration, and stent fracture [8, 9]. Chemotherapy after endoscopic stenting was also found to affect stent patency [8, 24, 32, 33], although palliative chemotherapy was not [25]. In our study, the median stent patency period was 12 weeks, similar to previous studies, and clinical success was associated with the duration of stent patency. However, subgroup analysis showed that stent patency was independent of the site of obstruction and type of stent including fully covered stents. Although chemotherapy may have affected stent patency, this could not be determined due to the retrospective nature of this study.
This study had several limitations associated with its retrospective design and the small number of patients implanted with fully covered stents. Furthermore, there may have been selection bias in choosing patients for the different treatment options, although patients who underwent surgery or previous stent implantation and those who were lost to follow-up were excluded. These findings therefore require confirmation in future prospective randomized studies with proper methodological design to assess the efficacy of endoscopic stent insertion in patients with malignant obstruction of the upper gastrointestinal tract.
In conclusion, the choice of SEMS inserted endoscopically for malignant obstruction of the upper gastrointestinal tract is dependent on the site of obstruction. Migration should be considered when inserting fully covered stents into the peri-pyloric area.
References
Jung GS, Song HY, Kang SG, Huh JD, Park SJ, Koo JY, Cho YD (2000) Malignant gastroduodenal obstructions: treatment by means of a covered expandable metallic stent-initial experience. Radiology 216:758–763
Kreel L, Ellis H (1965) Pyloric stenosis in adults: a clinical and radiological study of 100 consecutive patients. Gut 6:253–261
Chowdhury A, Dhali GK, Banerjee PK (1996) Etiology of gastric outlet obstruction. Am J Gastroenterol 91:1679
Shone DN, Nikoomanesh P, Smith-Meek MM, Bender JS (1995) Malignancy is the most common cause of gastric outlet obstruction in the era of H2 blockers. Am J Gastroenterol 90:1769–1770
Tendler DA (2002) Malignant gastric outlet obstruction: bridging another divide. Am J Gastroenterol 97:4–6
Baron TH (2001) Expandable metal stents for the treatment of cancerous obstruction of the gastrointestinal tract. N Engl J Med 344:1681–1687
Tierney W, Chuttani R, Croffie J, DiSario J, Liu J, Mishkin DS, Shah R, Somogyi L, Petersen BT (2006) Enteral stents. Gastrointest Endosc 63:920–926
Cho YK, Kim SW, Hur WH, Nam KW, Chang JH, Park JM, Lee IS, Choi MG, Chung IS (2010) Clinical outcomes of self-expandable metal stent and prognostic factors for stent patency in gastric outlet obstruction caused by gastric cancer. Dig Dis Sci 55:668–674
Kim JH, Song HY, Shin JH, Choi E, Kim TW, Jung HY, Lee GH, Lee SK, Kim MH, Ryu MH, Kang YK, Kim BS, Yook JH (2007) Metallic stent placement in the palliative treatment of malignant gastroduodenal obstructions: prospective evaluation of results and factors influencing outcome in 213 patients. Gastrointest Endosc 66:256–264
Maetani I, Ukita T, Tada T, Shigoka H, Omuta S, Endo T (2009) Metallic stents for gastric outlet obstruction: reintervention rate is lower with uncovered versus covered stents, despite similar outcomes. Gastrointest Endosc 69:806–812
Mosler P, Mergener KD, Brandabur JJ, Schembre DB, Kozarek RA (2005) Palliation of gastric outlet obstruction and proximal small bowel obstruction with self-expandable metal stents: a single center series. J Clin Gastroenterol 39:124–128
Nassif T, Prat F, Meduri B, Fritsch J, Choury AD, Dumont JL, Auroux J, Desaint B, Boboc B, Ponsot P, Cervoni JP (2003) Endoscopic palliation of malignant gastric outlet obstruction using self-expandable metallic stents: results of a multicenter study. Endoscopy 35:483–489
Phillips MS, Gosain S, Bonatti H, Friel CM, Ellen K, Northup PG, Kahaleh M (2008) Enteral stents for malignancy: a report of 46 consecutive cases over 10 years, with critical review of complications. J Gastrointest Surg 12:2045–2050
Lopes CV, Pesenti C, Bories E, Caillol F, Giovannini M (2008) Self-expandable metallic stents for palliative treatment of digestive cancer. J Clin Gastroenterol 42:991–996
Didden P, Spaander MC, de Ridder R, Berk L, van Tilburg AJ, Leeuwenburgh I, Kuipers EJ, Bruno MJ (2013) Efficacy and safety of a partially covered stent in malignant gastric outlet obstruction: a prospective Western series. Gastrointest Endosc 77:664–668
Oh D, Lee SS, Song TJ, Choi JH, Park DH, Seo DW, Lee SK, Kim MH (2015) Efficacy and safety of a partially covered duodenal stent for malignant gastroduodenal obstruction: a pilot study. Gastrointest Endosc 82:32–36
Chung KH, Lee SH, Park JM, Lee JM, Shin CM, Ahn SH, Park DJ, Kim HH, Ryu JK, Kim YT (2014) Partially covered self-expandable metallic stent for postoperative benign strictures associated with laparoscopy-assisted gastrectomy. Gastric Cancer 19:280–286
Heo J, Jung MK (2014) Safety and efficacy of a partially covered self-expandable metal stent in benign pyloric obstruction. World J Gastroenterol 20:16721–16725
Shi D, Ji F, Bao YS, Liu YP (2014) A multicenter randomized controlled trial of malignant gastric outlet obstruction: tailored partially covered stents (placed fluoroscopically) versus standard uncovered stents (placed endoscopically). Gastroenterol Res Pract 2014:309797
van den Berg MW, Walter D, Vleggaar FP, Siersema PD, Fockens P, van Hooft JE (2014) High proximal migration rate of a partially covered “big cup” duodenal stent in patients with malignant gastric outlet obstruction. Endoscopy 46:158–161
Adler DG, Baron TH (2002) Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol 97:72–78
Lillemoe KD, Pitt HA (1996) Palliation. Surgical and otherwise. Cancer 78:605–614
Bang S, Kim HJ, Park JY, Park YS, Kim MH, Park SW, Lee YC, Song SY (2008) Effectiveness of self-expanding metal stents for malignant antropyloric and duodenal obstruction with a comparison between covered and uncovered stents. Hepatogastroenterology 55:2091–2095
Park CI, Kim JH, Lee YC, Jahng J, Youn YH, Park H, Lee SI (2013) What is the ideal stent as initial intervention for malignant gastric outlet obstruction? Dig Liver Dis 45:33–37
Pan YM, Pan J, Guo LK, Qiu M, Zhang JJ (2014) Covered versus uncovered self-expandable metallic stents for palliation of malignant gastric outlet obstruction: a systematic review and meta-analysis. BMC Gastroenterol 14:170
Maetani I, Mizumoto Y, Shigoka H, Omuta S, Saito M, Tokuhisa J, Morizane T (2014) Placement of a triple-layered covered versus uncovered metallic stent for palliation of malignant gastric outlet obstruction: a multicenter randomized trial. Dig Endosc 26:192–199
Kim GH, Kang DH, Lee DH, Heo J, Song GA, Cho M, Yang US (2004) Which types of stent, uncovered or covered, should be used in gastric outlet obstructions? Scand J Gastroenterol 39:1010–1014
Cheng HT, Lee CS, Lin CH, Cheng CL, Tang JH, Tsou YK, Chang JM, Lee MH, Sung KF, Liu NJ (2012) Treatment of malignant gastric outlet obstruction with metallic stents: assessment of whether gastrointestinal position alters efficacy. J Investig Med 60:1027–1032
Mansoor H, Yusuf MA (2013) Outcomes of endoscopic pyloric stenting in malignant gastric outlet obstruction: a retrospective study. BMC Res Notes 6:280
Piesman M, Kozarek RA, Brandabur JJ, Pleskow DK, Chuttani R, Eysselein VE, Silverman WB, Vargo JJ 2nd, Waxman I, Catalano MF, Baron TH, Parsons WG 3rd, Slivka A, Carr-Locke DL (2009) Improved oral intake after palliative duodenal stenting for malignant obstruction: a prospective multicenter clinical trial. Am J Gastroenterol 104:2404–2411
Canena JM, Lagos AC, Marques IN, Patrocinio SD, Tome MG, Liberato MA, Romao CM, Coutinho AP, Veiga PM, Neves BC, Alem HD, Goncalves JA (2012) Oral intake throughout the patients’ lives after palliative metallic stent placement for malignant gastroduodenal obstruction: a retrospective multicentre study. Eur J Gastroenterol Hepatol 24:747–755
Park JJ, Lee YC, Kim BK, Kim JH, Park JC, Kim YJ, Lee SK, Song SY, Chung JB (2010) Long-term clinical outcomes of self-expanding metal stents for treatment of malignant gastroesophageal junction obstructions and prognostic factors for stent patency: effects of anticancer treatments. Dig Liver Dis 42:436–440
Kim CG, Park SR, Choi IJ, Lee JY, Cho SJ, Park YI, Nam BH, Kim YW (2012) Effect of chemotherapy on the outcome of self-expandable metallic stents in gastric cancer patients with malignant outlet obstruction. Endoscopy 44:807–812
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kyoungwon Jung, Ji Yong Ahn, Hwoon-Yong Jung, Charles J. Cho, Hee Kyong Na, Kee Wook Jung, Jeong Hoon Lee, Do Hoon Kim, Kee Don Choi, Ho June Song, Gin Hyug Lee, and Jin-Ho Kim have no conflicts of interest or financial ties to disclose.
Additional information
Kyoungwon Jung and Ji Yong Ahn have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Jung, K., Ahn, J.Y., Jung, HY. et al. Outcomes of endoscopically inserted self-expandable metal stents in malignancy according to the type of stent and the site of obstruction. Surg Endosc 30, 4001–4010 (2016). https://doi.org/10.1007/s00464-015-4712-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4712-x