Abstract
Background
Previously, we reported that microRNA-181b (miR-181b) activates hepatic stellate cells partly through the phosphatase and tensin homolog deleted on chromosome 10 (PTEN)/Akt pathway.
Aims
The main objective of this study was to ascertain whether serum miR-181b expression is correlated with that of liver hepatitis B virus (HBV) DNA and disease progression in chronic hepatitis B (CHB) patients.
Methods
Serum miR-181b and liver HBV DNA levels were quantified in 64 CHB patients with real-time PCR. Liver fibrosis and necroinflammation were graded according to the Ishak scoring system.
Results
Serum miR-181b levels were evaluated in the CHB group, compared with healthy controls. Expression in patients with HBsAg (+) was higher than that in patients with HBsAg (−). Notably, serum miR-181b and liver HBV DNA levels were significantly correlated (P < 0.05). Serum miR-181 levels were higher in patients with serum HBV DNA > 103 IU/ml (P = 0.017), histologic activity index (HAI) >8 (P = 0.001) and fibrosis score >4 (P < 0.0001). Liver HBV DNA levels were higher in patients with abnormal alanine aminotransferase (ALT) values (P = 0.004), serum HBV DNA levels > 103 IU/ml (P = 0.034) and fibrosis score >4 (P = 0.006). Using multivariate logistic regression analysis, serum miR-181b was identified as an independent predictor of disease progression (OR 4.172, 95 % CI 1.838–9.473, P = 0.009 for HAI >8; OR 5.387, 95 % CI 2.067–14.036, P = 0.001 for fibrosis score >4).
Conclusions
Serum miR-181b is correlated with liver and serum HBV DNA levels as well as disease progression in CHB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic hepatitis B virus (HBV) affects 350–400 million patients worldwide and is one of the major etiological factors for the development of cirrhosis and hepatocellular carcinoma (HCC) [1, 2]. The HBV DNA level has been identified as one of the risk factors of cirrhosis and HCC for chronic hepatitis B (CHB) patients [3]. In China, HBV infection is a predominant etiological factor of liver disease, whereby ~7.8 % of the population are HBV carriers [4]. China is additionally one of the areas with the highest prevalence of HCC due to the significant number of chronic HBV carriers [5]. CHB poses a serious health burden, leading to increased healthcare costs and other socioeconomic problems. Liver biopsy has been reported to be valuable in the assessment of HBV-induced liver injury severity and monitoring of CHB progression [6]. However, due to the invasive procedure and possible complications, such as bleeding and sampling error, this technique is not commonly used in CHB patients. Therefore, the identification of potential effective non-invasive markers of CHB progression is critical.
MicroRNAs (miRNAs) are small non-coding RNAs (18–24 nucleotides long) that modulate gene expression by binding to the 3′-untranslated region of target mRNAs [7]. MiRNAs are involved in several physiological processes, including cellular differentiation, apoptosis and proliferation [8], and play vital roles in pathogenesis, diagnosis and therapeutic aspects of viral infection [9, 10]. Increasing evidence has shown that miRNAs act as HSC regulators and play diverse roles in hepatic fibrosis [11]. Moreover, cell-free miRNAs circulate in the blood and are detectable in serum and plasma in a sufficiently stable form to serve as biomarkers [12–15]. The miRNA levels in serum and plasma are strongly correlated, indicating that both serum and plasma may be employed for the analysis of these blood-based biomarkers [14]. Altered levels of serum/plasma miRNAs are associated with numerous diseases, including cancer and liver disease [16–18]. Thus, circulating miRNAs have significant potential as non-invasive markers for human liver fibrosis.
Previously, Wang et al. [11] reported that miR-181b, but not miR-181a, promotes hepatic stellate cell proliferation by targeting p27, and is elevated in serum of cirrhosis patients. Our group further demonstrated that miR-181b activates hepatic stellate cells (HSCs), at least in part, via the phosphatase and tensin homolog deleted on chromosome 10 (PTEN)/Akt pathway [19]. Overexpression of miR-181b resulted in enhanced cell proliferation, and expression of ECM proteins and α-SMA in HSCs. However, the issue of whether serum miR-181b expression is associated with HBV replication and CHB disease progression remains to be established. In the present study, we investigated the serum levels of miR-181b and its possible correlation with serum HBV DNA and progression of liver fibrosis in CHB patients.
Materials and Methods
Study Subjects
Serum samples were obtained from patients attending the First Affiliated Hospital of Wenzhou Medical University in Wenzhou and the Second Yinzhou Hospital in Ningbo from 2007 to 2012 (Table 1). The study included 72 healthy controls (with normal liver biochemistry, no history of liver disease or alcohol abuse, and no viral hepatitis) and 72 patients with CHB. Patients with CHB who were naïve to nucleos(t)ide analogues and interferon therapy were included. All patients were hepatitis B surface antigen (HBsAg)-positive for at least 6 months. Exclusion criteria were: (1) patients aged less than 16 years, (2) co-infection with human immunodeficiency virus (HIV), (3) coexistence of liver injury caused by other etiologies, including hepatitis C virus (HCV) infection, drug intake, alcohol consumption and auto-immune hepatitis, (4) severe systematic diseases, and (5) pregnancy and lactation [20]. Eight patients were excluded owing to coagulation disorders. Overall, 64 patients underwent liver biopsy. Demographic and clinical information were obtained, and blood samples collected from all patients on the day of diagnostic liver biopsy. Diagnosis of HCC was based on histopathological assessment [21].
Ethics Statement
Informed consent for the use of blood samples was obtained from all participants. The project was approved by the Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University. All procedures were performed in accordance with the current international guidelines, standards on human experimentation of the Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University, and the Helsinki Declaration of 1975, revised in 1983.
Liver Histology
Liver biopsy was performed using a 16-gauge Menghini needle. Each liver biopsy case was advised by physicians in care, and liver specimens at least in 2.0 cm in length obtained. Samples were fixed in formalin, embedded in paraffin, and stained with hematoxylin-eosin. Results were reviewed by experienced hepatopathologists. In addition, at least 8–10 portal tracts in samples are required to admit patients. Histological activity index (HAI) and fibrosis stages (F0 = no fibrosis to F6 = cirrhosis) were assessed according to the Ishak scoring system [22].
Blood Samples Processing
All blood samples were centrifuged at 3400g for 7 min at room temperature within 4 h of acquisition. Sera were transferred into Eppendorf tubes and additionally centrifuged at 12,000g for 10 min at 4 °C to remove the remaining cells. Serum samples were stored at −80 °C pending RNA extraction.
Detection of miR-181b with Real-Time Quantitative RT-PCR
Total RNA was extracted with the miRNeasy Mini Kit (Qiagen, Carlsbad, CA, USA), according to the manufacturer’s instructions for liquid samples. For removing DNA contaminants in total RNA, DNase treatment (Qiagen) was performed. The final elution volume was 20 μl. Prior to the reverse transcription reaction, serum RNA preparations were quantified using NanoDrop 1000 (Nanodrop, Wilmingtion, DE, USA). Reverse transcription was performed in a 20 μl reaction volume using the TaqMan MicroRNA Reverse Transcription kit (Applied Biosystems, Foster City, CA, USA). For cDNA synthesis, reaction mixtures were sequentially incubated at 16 °C for 30 min, 42 °C for 30 min, and 85 °C for 5 min. miR-181b was quantified in triplicate via qRT-PCR using the TaqMan MicroRNA Assay Kit (Applied Biosystems). According to the standard TaqMan MicroRNA assay protocol, real-time PCR was performed on an ABI 7500 Real-Time PCR system (Applied Biosystems) under the following conditions: 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 60 s. Each PCR mixture (20 μl) included the reverse transcription products, TaqMan 2X Universal PCR Master Mix without UNG Amperase, miRNA-specific TaqMan probes, and primers supplied by Applied Biosystems. The cycle threshold (Ct) is defined as the number of cycles required for the fluorescent signal to cross the threshold in qPCR. Ct values were calculated with SDS 2.0.1 software (Applied Biosystems). The formula 2−ΔCt was used to calculate the miRNA levels in serum, where ΔCt = mean (Ct of internal references) − Ct of target miRNA. The relative expression levels of miR-181b were calculated and normalized to miR-16 (Applied Biosystems) using the comparative ΔCt method and the Eq. 2−ΔCt, as described previously [23].
Liver HBV DNA and Serum Hepatitis Markers Analysis
Liver tissues from biopsies were homogenized with TissueLyser (Qiagen, Hilden, Germany) for 30 s at 30 Hz, and DNA extracted using microspin columns (QIAamp DNA kit; Qiagen). DNA was analyzed for HBV genome levels with real-time PCR in a Light Cycler 1.5 (Roche Diagnostics, Branchburg, NJ, USA). An external standard curve was generated to quantify HBV genome levels using a PCR product cloned with the TA cloning system as standard (Invitrogen, Carlsbad, CA, USA), with 8 μl appropriately diluted plasmid used to generate the standard curve. HBV DNA was normalized to β-globin as a positive control, which is ubiquitously detected in all human cells [24]. Data are indicated as the number of IU/cells. Each value represents mean ± SD of three experiments.
For all CHB patients, HBsAg, HBeAg, and antibodies against HBsAg (anti-HBs), HBeAg (anti-HBe) and hepatitis B core antigen (anti-HBc) were determined using the Roche Modular E170 Immunoassay Analyzer (Roche, Basel, Switzerland). Serum HBV DNA was quantified with the artus HBV QS-RGQ Kit (Qiagen) using a lower detection limit of 10.2 IU/ml.
Statistical Analysis
Statistical analyses were performed with SPSS 13.0 (IBM, Armonk, NY, USA). Continuous variables were summarized as mean and standard deviation, and categorical variables as absolute and relative frequencies. Differences were evaluated using the Wilcoxon signed-rank test, and categorical variables compared with the Chi square test using the exact procedures, where required. Correlation coefficients (r) were calculated using Spearman’s rank correlation. Odds ratios with 95 % confidence intervals (CI) were estimated with a logistic regression model for evaluating the relationships among age, serum miR-181b, serum HBV DNA, HAI and fibrosis. Data were considered significant at P < 0.05.
Results
A total of 136 subjects were recruited, including 72 healthy controls and 64 CHB patients. Patient characteristics are shown in Table 1. We observed no significant differences in age between healthy controls and patients with CHB (P = 0.746). Sex distribution (male:female) was 43:29 in healthy controls and 37:27 in CHB patients (P = 0.821, χ 2 test).
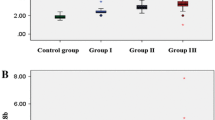
Serum miR-181b in CHB patients was detected at a mean concentration of 2.688 ± 1.097 (Table 1). To ascertain its potential as a novel biomarker of CHB, serum miR-181b levels were detected in both CHB patients (n = 64) and healthy controls (n = 72). qRT-PCR analysis revealed higher serum miR-181b levels in CHB patients (median and range 2.550, 0.820–5.810), compared to healthy controls (0.920, 0.450–1.720; P < 0.0001, Fig. 1a). Liver HBV DNA was detected in CHB patients at a mean concentration of 2.282 ± 4.499 (Table 1). All CHB patients were divided into two subgroups according to HBeAg status. To determine the association between serum miR-181b and HBV replication, serum miR-181b levels were analyzed in HBeAg+ and HBeAg− groups. The serum miR-181b level in the HBeAg + group (median and range 2.905, 0.820–5.810) was significantly higher than that in the HBeAg- group (2.315, 0.870–4.700; P < 0.0001; Fig. 1b). CHB patients were additionally divided into two subgroups according to mean liver HBV DNA concentration. Our results showed that serum miR-181b levels in patients with liver HBV DNA ≤2.282 IU/cell (median and range 2.295, 0.820–5.300) are lower than those in patients with liver HBV DNA ≥2.282 IU/cell (3.570, 2.600–5.810; P < 0.0001; Fig. 1c). Furthermore, serum miR-181b and liver HBV DNA levels were correlated (r = 0.595, P < 0.05; Fig. 1d).
Serum miR-181b levels in CHB patients and correlation with liver HBV DNA levels. a Serum miR-181b levels in healthy controls (n = 72) and patients with CHB (n = 64). b Serum miR-181b levels in CHB patients from HBsAg (+) or HBsAg (−) groups. c Serum miR-181b levels in CHB patients with liver HBV DNA ≤ 2.282 or > 2.282. Vertical lines indicate the range, and horizontal boundaries of the boxes represent the first and third quartiles. *P < 0.0001. d Correlation between serum miR-181b and liver HBV DNA levels in patients with CHB. Significance was calculated according to Spearman correlation. P and r values are shown
Serum miR-181b and liver HBV DNA levels were analyzed according to patient age, sex, alanine aminotransferase (ALT) values, HBV DNA serum levels, HAI and fibrosis scores. In univariate analysis, no association was found between serum miR-181b level and sex, age or ALT values. Notably, serum miR-181b levels were significantly increased in patients with HBV DNA serum levels >103 IU/ml [median 2.770 (1.890–4.700) vs. 2.210 (0.820–5.810), P = 0.017], HAI >8 [median 3.450 (1.890–5.810) vs. 2.420 (0.820–4.700), P = 0.001] and fibrosis scores >4 [median 3.320 (1.890–5.810) vs 2.220 (0.820–4.700), P < 0.0001] (Table 2). In terms of liver HBV DNA, no association was evident with age, sex or HAI (Table 2). However, liver HBV DNA levels were significantly increased in patients with abnormal ALT values [median 2.485 (0.002–20.540) vs. 0.113 (0.006–2.140) (0.820–5.810), P = 0.004], HBV DNA serum level >103 IU/ml [median 0.716 (0.014–20.540) vs. 0.135 (0.002–2.310), P = 0.034] and fibrosis score >4 [median 1.100 (0.006–14.870) vs. 0.098 (0.002–20.540), P = 0.006] (Table 2).
To further confirm the association between serum miR-181b and histological lesions (HAI and fibrosis scores) and avoid possible confounding effects of other factors, such as age and liver HBV DNA levels, multivariate logistic regression analysis was performed. Serum miR-181b was identified as an independent predictor of HAI >8 (OR 4.172, 95 % CI 1.838–9.473, P = 0.009) and of a fibrosis score >4 (OR 5.387, 95 % CI 2.067–14.036, P = 0.001) (Table 3). Increasing HAI or fibrosis scores were accompanied by a progressive increase in the mean serum miR-181b level (Fig. 2a, b). Similarly, we observed a progressive increase in the prevalence of patients with liver HBV DNA >2.282 IU/cell or serum miR-181b level >2.688, reflecting increased HAI (Fig. 2c) and fibrosis scores (Fig. 2d).
Discussion
Considerable research attention has focused on the identification of novel serum miRNAs for diagnosis of diseases, in view of their noninvasive nature [25–27]. The discovery of serum miRNA in peripheral blood has provided a novel approach for noninvasive clinical diagnosis. Zhang et al. [28] evaluated circulating miR-122 in plasma of patients and animal models with viral-, alcohol-, and chemical-induced liver diseases, and suggested its potential as a liver injury biomarker for diagnosis and monitoring of disease. Another recent study showed that serum miR-29 is correlated with disease progression in CHB patients [20], supporting the potential of serum miRNAs as markers for disease progression.
Recent studies have identified cellular and viral miRNAs as a new class of regulators in viral pathogenesis [29]. Chronic HBV infection is a known major etiological factor for HCC development [1]. HBV gene expression and replication may be affected by several miRNAs that bind directly to viral transcripts, such as miR-151-5p [30, 31], miR-125-5p [31], miR-199-3p and miR-210 [32]. For example, Liu et al. [33] reported that hsa-miR-125-5p is increased at least 3-fold in the HBV-producing cell line, HepG2.2.15, compared with the parent cell line, HepG2. Potenza and colleagues previously reported that overexpression of miR-125-5p in cultured PLC/PRF/5 induces significant reduction in HBsAg, whereas inhibition of miR-125-5p triggers HBsAg expression [31]. Further studies confirmed that liver miR-125-5p activity in HBV-infected tissues is correlated with HBV replication and disease progression [24]. However, since it is difficult to obtain liver tissue, liver miRNAs do not effectively serve as potential biomarkers for CHB patients. On the other hand, blood-derived microRNAs are easily accessible and can be utilized as novel markers for assessment of disease severity. In patients with chronic viral hepatitis, elevated levels of microRNAs, such as miR-122, have been reported [34]. In the current study, we observed miR-181b expression in the serum of all enrolled patients.
We focused on miR-181b owing to its pro-fibrosis ability [19], as well as the earlier finding that serum levels may be a potential diagnostic biomarker for cirrhosis [11].
In the current study, serum miR-181b levels were determined in CHB patients according to several bioclinical and histological parameters. Compared with healthy controls, serum miR-181b was increased in CHB patients, supporting its utility as a biomarker of CHB. Further analysis of the correlation between serum miR-181b levels and viral replication revealed that serum miR-181b is increased in patients with HBeAg+ and HBV DNA levels higher than 2.282, suggesting that liver exposure to HBV induces serum miR-181b. Serum miR-181b was significantly correlated with serum and liver HBV DNA levels (Fig. 1d; Table 2). However, the issue of whether miR-181b is capable of inhibiting HBV replication requires further investigation. Additionally, serum miR-181b level was associated with HAI score >8 and fibrosis score >4, highlighting its potential as an independent predictor of moderate and severe CHB disease. This may be explained by the fact that higher serum miR-181b levels are induced at higher levels of HBV DNA, which is often associated with more severe liver disease [35]. These results are in accordance with our previous in vitro findings [19], suggesting that miR181b acts as pro-fibrosis miRNA in liver.
Our results support the development of serum miR-181b as a marker for disease progression in CHB patients. However, the current study has a number of limitations. The sample size was relatively small. In addition, the relationship between serum miR-181b and immune status of patients was not examined. For example, subjects were not divided into inactive carriers, low replicative HBe antigen-negative elevated ALT, high replicative HBe antigen-negative normal ALT, high replicative HBe antigen-negative elevated ALT, and HBe antigen-positive hepatitis groups for analysis [34]. Studies with larger sample sizes are warranted to validate the efficacy of this marker and determine the relationship between serum miR-181b and patient immune status.
In summary, serum 181b levels are elevated in CHB patients and correlated with HBV replication and disease progression, highlighting the potential utility of this microRNA as a marker of CHB.
References
Dienstag JL. Hepatitis B virus infection. N Engl J Med. 2008;359:1486–1500.
McMahon BJ Epidemiology and natural history of hepatitis B. Seminars in Liver Disease. 2005;25:3–8.
Chen CJ, Yang HI, Su J, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. J Am Med Assoc. 2006;295:65–73.
Liu X, Wan X, Li Z, Lin C, Zhan Y, Lu X. Golgi protein 73(GP73), a useful serum marker in liver diseases. Clin Chem Lab Med CCLM/FESCC. 2011;49:1311–1316.
Li L, Guo Z, Wang J, Mao Y. Gao Q Serum miR-18a: a potential marker for hepatitis B virus-related hepatocellular carcinoma screening. Dig Dis Sci. 2012;57:2910–2916.
Degertekin B. Lok AS Indications for therapy in hepatitis B. Hepatology. 2009;49:S129–S137.
Bartel DP. MicroRNAs genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–297.
Croce CM, Calin GA. miRNAs, cancer, and stem cell division. Cell. 2005;122:6–7.
Esquela-Kerscher A, Slack FJ. Oncomirs—microRNAs with a role in cancer. Nat Rev Cancer. 2006;6:259–269.
Kloosterman WP, Plasterk RH. The diverse functions of microRNAs in animal development and disease. Dev Cell. 2006;11:441–450.
Wang B, Li W, Guo K, Xiao Y, Wang Y, Fan J. miR-181b promotes hepatic stellate cells proliferation by targeting p27 and is elevated in the serum of cirrhosis patients. Biochem Biophys Res Commun.. 2012;421:4–8.
Chen X, Ba Y, Ma L, et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 2008;18:997–1006.
Fang C, Zhu DX, Dong HJ, et al. Serum microRNAs are promising novel biomarkers for diffuse large B cell lymphoma. Ann Hematol. 2012;91:553–559.
Gilad S, Meiri E, Yogev Y, et al. Serum microRNAs are promising novel biomarkers. PLoS ONE. 2008;3:e3148.
Mitchell PS, Parkin RK, Kroh EM, et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci USA. 2008;105:10513–10518.
Bihrer V, Friedrich-Rust M, Kronenberger B, et al. Serum miR-122 as a biomarker of necroinflammation in patients with chronic hepatitis C virus infection. Am J Gastroenterol. 2011;106:1663–1669.
Qi P, Cheng SQ, Wang H, Li N, Chen YF, Gao CF. Serum microRNAs as biomarkers for hepatocellular carcinoma in Chinese patients with chronic hepatitis B virus infection. PLoS ONE. 2011;6:e28486.
Xu J, Wu C, Che X, et al. Circulating microRNAs, miR-21, miR-122, and miR-223, in patients with hepatocellular carcinoma or chronic hepatitis. Mol Carcinog. 2011;50:136–142.
Zheng J, Wu C, Xu Z, et al. Hepatic stellate cell is activated by microRNA-181b via PTEN/Akt pathway. Mol Cell Biochem. 2015;398:1–9.
Huang C, Zheng JM, Cheng Q, et al. Serum microRNA-29 levels correlate with disease progression in patients with chronic hepatitis B virus infection. J Dig Dis. 2014;15:614–621.
2004 guidelines for surgical treatment of primary hepatocellular carcinoma. Zhonghua gan zang bing za zhi = Zhonghua ganzangbing zazhi = Chinese J Hepatol. 2005;13:329–330.
Ishak K, Baptista A, Bianchi L, et al. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22:696–699.
Yao J, Liang L, Huang S, et al. MicroRNA-30d promotes tumor invasion and metastasis by targeting Galphai2 in hepatocellular carcinoma. Hepatology. 2010;51:846–856.
Coppola N, Potenza N, Pisaturo M, et al. Liver microRNA hsa-miR-125a-5p in HBV chronic infection: correlation with HBV replication and disease progression. PLoS ONE. 2013;8:e65336.
Ozer J, Ratner M, Shaw M, Bailey W, Schomaker S. The current state of serum biomarkers of hepatotoxicity. Toxicology. 2008;245:194–205.
Amacher DE, Adler R, Herath A, Townsend RR. Use of proteomic methods to identify serum biomarkers associated with rat liver toxicity or hypertrophy. Clin Chem. 2005;51:1796–1803.
Ebert MP, Korc M, Malfertheiner P, Rocken C. Advances, challenges, and limitations in serum-proteome-based cancer diagnosis. J Proteome Res. 2006;5:19–25.
Zhang Y, Jia Y, Zheng R, et al. Plasma microRNA-122 as a biomarker for viral-, alcohol-, and chemical-related hepatic diseases. Clin Chem. 2010;56:1830–1838.
Russo A, Potenza N. Antiviral effects of human microRNAs and conservation of their target sites. FEBS Lett. 2011;585:2551–2555.
Park SO, Kumar M, Gupta S. TGF-beta and iron differently alter HBV replication in human hepatocytes through TGF-beta/BMP signaling and cellular microRNA expression. PLoS ONE. 2012;7:e39276.
Potenza N, Papa U, Mosca N, Zerbini F, Nobile V, Russo A. Human microRNA hsa-miR-125a-5p interferes with expression of hepatitis B virus surface antigen. Nucleic Acids Res. 2011;39:5157–5163.
Zhang GL, Li YX, Zheng SQ, Liu M, Li X, Tang H. Suppression of hepatitis B virus replication by microRNA-199a-3p and microRNA-210. Antiviral Res. 2010;88:169–175.
Liu Y, Zhao JJ, Wang CM, et al. Altered expression profiles of microRNAs in a stable hepatitis B virus-expressing cell line. Chin Med J. 2009;122:10–14.
Waidmann O, Bihrer V, Pleli T, et al. Serum microRNA-122 levels in different groups of patients with chronic hepatitis B virus infection. J Viral Hepatitis. 2012;19:e58–e65.
Iloeje UH, Yang HI, Su J, Jen CL, You SL, Chen CJ. Predicting cirrhosis risk based on the level of circulating hepatitis B viral load. Gastroenterology. 2006;130:678–686.
Acknowledgments
The project was supported by National Natural Science Foundation of China (81000176/H0317, 81100292/H0317), Zhejiang Provincial Natural Science Foundation of China (Y2090326, Y2110634) and Wang Bao-En Liver Fibrosis Foundation (Nos. 20100002, 20120127).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Yu, F., Zhou, G., Li, G. et al. Serum miR-181b Is Correlated with Hepatitis B Virus Replication and Disease Progression in Chronic Hepatitis B Patients. Dig Dis Sci 60, 2346–2352 (2015). https://doi.org/10.1007/s10620-015-3649-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3649-1