Abstract
Background
Alcohol intake is closely related to colorectal cancer, which remains inconsistent with studies on the relation between alcohol consumption and risk of colorectal serrated polyp (SP) which was proven to have potential of developing into malignant serrated neoplasm.
Aim
A meta-analysis investigating the association between alcohol intake and colorectal SP with the dose–response of alcohol intake was conducted.
Methods
The literature search was performed on PubMed to identify pertinent articles presenting results for at least three categories of alcohol consumption dated up to October 2014. Summarized relative risks (RRs) with 95 % confidence intervals (CIs) were estimated using random or fixed effects models based on statistical heterogeneity.
Results
A total of ten observational studies were identified in this meta-analysis. All drinkers were associated with 24 % increased risk of colorectal SP compared with non-/occasional drinkers. In particular, the light alcohol intake was not related to an increased risk of colorectal SP (RR 1.05, 95 % CI 0.93–1.18), whereas the RRs were 1.19 (95 % CI 1.02–1.40) for moderate alcohol intake and 1.60 (95 % CI 1.35–1.91) for heavy alcohol intake. The risks were consistent in further dose–response analysis. Meanwhile, subgroup analyses demonstrated that patients in America had more increased risk of SP with respect to those in Europe and Asia. In terms of subtype of colorectal SP, alcohol consumption had a greater influence on SSA than HP.
Conclusions
This is the first meta-analysis that demonstrated the relationship between moderate and heavy alcohol consumption and increasing risks of colorectal SP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer has been rapidly increasing since 1975 and is now the third most common cancer worldwide, which has an impact on approximately 1.23 million people [1, 2]. Many studies suggest that most colorectal cancers originate from precursor benign polyps [3, 4]. Besides the well-known colorectal adenomas (CRAs) which may cause tumorigenesis via the traditional adenoma-carcinoma pathway, the World Health Organization recently defined a new group of polyps called serrated polyps.
Serrated polyps (SPs), generally considered as “hyperplastic polyps” in the past, have been now classified into hyperplastic polyp (HP), sessile serrated adenoma (SSA), and traditional serrated adenoma (TSA) [5]. These polyps show different colonoscopic appearances, histology, and molecular alteration, and risk of progression to CRC. HPs are the most common category and account for 75–95 % of total SPs, while SSAs take up less than a quarter. TSAs are the rarest kind, comprising only approximate 1 % of SPs [6–11].
Rosty et al. [5] found that 30 % of CRC developed via the serrated neoplasia pathway, which was characterized by the mutation of the BRAF oncogene and development of CpG island methylator phenotype (CIMP). It is likely that different risk factors act at each step of the serrated pathway and exacerbate the SP into CRC. SPs (including HPs) share a number of common risk factors with conventional adenomas and carcinomas, such as cigarette smoking and overeating [12–14]. Some studies demonstrate smoking is an independent risk factor for developing SPs via DNA hypermethylation and even has greater association with colorectal SP than CRA [15]. However, some epidemiologic evidence suggested that serrated polyps may have many different risk factors. For instance, aging was thought to be a strong risk factor of traditional adenomas [16], yet not many studies find any prominent relationship between age and risk for serrated (or hyperplastic) polyps [17–19].
In some studies, alcohol consumption was regarded as one of the most important risk factors in the development of SPs (including HPs), as shown by Martinez et al. [20] (>9.4 g/day vs. non-drinkers: RR 2.01, 95 % CI 1.05, 3.91). However, the mechanism by which alcohol increased the risk of colorectal SPs or HPs is not yet clearly known. Alcohol may not be a direct-acting carcinogen, but the various compounds including phenols, higher alcohols, aldehydes and nitrosamines in different types of drinking may be involved in the serrated pathway [21]. Nevertheless, not many studies have proven that alcohol intake is a serious risk factor for SPs. [18]. Meanwhile, the relative risks may vary due to different dose of alcohol consumption.
Therefore, the relationship between alcohol intake and colorectal SPs of different categories is still under debate, and no comprehensive meta-analysis is conducted. Thus, this systematic review with meta-analysis is to estimate the summarized relative risk of colorectal SPs associated with alcohol intake in different categories as well as with the dose–response analysis.
Methods
Data Sources and Searches
A comprehensive, computerized literature search was carried out on PubMed from the beginning of indexing to October 2014, following the Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) guidelines [22]. Two independent investigators (Y.M. Wang and J.Z. Zhu) used the terms (colorectal OR colorectum OR colon OR rectum OR bowel) AND (polyps OR adenoma OR adenomatous) AND (ethanol OR alcohol OR drink) to search for relevant studies. Abstracts or unpublished reports were not considered for inclusion in the meta-analysis.
Study Selection
Two authors (Y.M. Wang, K.F. Zhu) independently accessed all the potentially eligible studies retrieved according to prespecified selection criteria. Discrepancies between the two reviewers were decided by another author (J.Z. Zhu). Studies were included if they met the following criteria: (1) published as an original article using a case–control, cohort or cross-sectional design; (2) reported relative risk (RR) estimates with corresponding 95 % CIs for at least three categories of alcohol intake levels (including a category of nonalcohol intake or occasional alcohol intake) and the risk of colorectal SP. Studies were excluded if the cases had both colorectal SP and adenoma. Besides, neither the nonpeer-reviewed articles, experimental animal studies nor the mechanistic studies were included.
Data Abstraction and Study Quality Assessment
Two authors (Q.Y. Zhou and K.F. Zhu) independently extracted data from the included full-text citations. The following information was abstracted: study design (case–control, cohort, or cross-sectional study), the first author’s last name, country of origin, gender, age of cases, site of SPs, publication year, number of cases and controls with the definition for each level of alcohol consumption, race/ethnicity, examination method (endoscopy or/and CT) and case ascertainment.
Two authors (J.Z. Zhu and K.F. Zhu) independently assessed the methodological quality of every included study according to the Newcastle–Ottawa Scale (NOS) [22, 23]. The NOS contains nine items (1 point for each) for the observational studies: selection (4 items), comparability (2 items), and exposure/outcome assessment (3 items). A study with no less than 7 points was regarded as high quality and a study with insufficient information was considered to be of low quality.
Statistical Methods
Different studies used different ways to calculate the alcohol consumption. Thus, the alcohol consumption was converted into grams of ethanol per day using the following equations: 1 mL = 0.8 g and 1 drink = 11.0 g. Nondrinkers or occasional drinkers were defined as the reference category. The standard deviation, quartiles, mean, and median of the lower boundaries of heavy dose of the selected studies were calculated to set up the boundary of light, moderate and heavy doses. The upper boundary of light dose was set according to the first quartile of the lower boundaries of heavy doses of all included studies. And the upper boundary of moderate dose was set by the difference of the maximum and standard deviation of the lower boundaries of heavy doses of the studies. Therefore, the alcohol consumption categories were defined using the following values: light (≤8 g/day), moderate (8–36 g/day), and heavy (≥36 g/day).
Abstracted data from the included studies were entered into Stata Statistical Software (version 12.0; StataCorp LP, College Station, TX, USA). Fixed or random effects models were used to calculate the summarized relative risks of colorectal SPs with 95 % CIs. Forest plots were made for any, light, moderate, and heavy versus non-/occasional alcohol consumption. Heterogeneity across studies was assessed with the chi-square statistic, with P < 0.10 considered significant, and with the I² test [24]. An I² value greater than 50 % was regarded as substantial heterogeneity. Furthermore, the sources of heterogeneity were investigated by subgroup analyses and meta-regression analyses according to study design, race, geographic location, subtype of SPs, and published year. Additionally, sensitivity analysis was carried out to estimate the influence of each individual study on the summary estimates by conducting the random effects meta-analysis again after omitting one of the included studies in each turn. Publication bias was assessed using the Egger linear regression test [25], the Begger–Mazumdar test and visual inspection of funnel plots. Potential publication bias would be adjusted by trim-and-fill method if applicable (P < 0.05).
A dose–response analysis was conducted using both linear and nonlinear random effects models on the natural logarithm of the RR. This method is able to explain the correlation between reported risks estimates within one study, heterogeneity between the studies and nonlinear dose–risk association. Linear random effect models and ten second-order fractional polynomial random effects models were tested to find out the best-fitting model. Finally, the best-fitting model that had the lowest Akaike’s information criterion was selected as the final dose–risk relation model. The statistics of the chosen model showed that the model was appropriate [26, 27].
Results
Literature Search
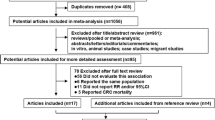
Figure 1 shows the study selection details in the meta-analysis. A total of 467 citations were identified, of which 250 citations were excluded due to irrelevant topics after screening of the titles and abstracts. A total of 207 of the remaining articles were excluded for various reasons after evaluating the full texts. Finally, ten articles (7 case–control studies [12, 18–20, 28–30], 2 cross-sectional studies [31, 32], and 1 cohort study [13]) were included in this meta-analysis.
Study Characteristics
A total of ten studies concerning alcohol consumption and colorectal SP incidence were published between 1995 and 2014. All studies inquired about the alcohol intake of the participants, whether they ever had symptoms, and the histological diagnosis of the colorectal polyps after undergoing the examination of colonoscopy or sigmoidoscopy. Among the ten qualified studies, seven were conducted in the United States, two in Europe, and one study in Asia, as shown in Table 1. In addition, eight studies reported RRs for both colon and rectum SPs, while two did for distal colon and rectum. In terms of subtype of the SPs, only two recent articles summarized the data [30, 32], from which we can only abstract the RRs of HPs and SSAs. Due to the limited data, the analysis of the gender and the size of polyps cannot be performed.
In General
Meta-analysis of the ten studies in a random-effects model showed that alcohol intake was associated with a 24 % increased risk of colorectal SP (RR 1.24; 95 % CI 1.07–1.44). There heterogeneity existed among studies (P < 0.001; I² = 70.2 %), so subgroup meta-analyses and meta-regression were used to explore the sources of heterogeneity. Moreover, RRs of different levels of alcohol drinkers were as follows: light drinkers, 1.05 (95 % CI 0.93–1.18); moderate drinkers, 1.19 (95 % CI 1.02–1.40); heavy drinkers, 1.60 (95 % CI 1.35–1.91) (Fig. 2; Table 2).
Pooled risk estimates for colorectal SP incidence for all drinkers versus non-/occasional drinkers, light drinkers versus non-/occasional drinkers, moderate drinkers versus non-/occasional drinkers and heavy drinkers versus non-/occasional drinkers, with respect to types of study (cohort, case–control and cross-sectional studies)
Type of the Studies
In the stratified analysis by study type, the summary RRs of colorectal SP were 1.24 (95 % CI 1.02–1.52) in case–control studies, 1.16 (95 % CI 0.94–1.42) in cross-sectional studies and 1.41 (95 % CI 1.10–1.80) in the cohort study, comparing all drinkers and non-/occasional drinkers (Fig. 2; Table 2).
Geographical Region
In terms of different regions, the pooled estimate showed a significant increased risk of colorectal SP in the United States [RR 1.29 (95 % CI 1.06–1.57)] when compared to the non-/occasional alcohol intake controls, but with a substantial heterogeneity between trials. However, there was no statistical difference between all drinkers and non-/occasional drinkers in Europe [RR = 1.12 (95 % CI 0.90–1.41)] and those in Asia [RR = 1.16 (95 % CI 0.88–1.52)]. Yet, further analysis suggested that heavy alcohol consumption was associated with a significant increased risk of colorectal SP in Europe [1.70 (95 % CI 1.15–2.51)] but not in Asia [1.43 (95 % CI 0.90–2.25)] (Fig. 3; Table 2).
Pooled risk estimates for colorectal SP incidence for all drinkers versus non-/occasional drinkers, light drinkers versus non-/occasional drinkers, moderate drinkers versus non-/occasional drinkers and heavy drinkers versus non-/occasional drinkers, with respect to geographical region of studies (USA, Europe and Asia)
Subgroup of SP
Only data from the two recent studies were extracted for subgroup meta-analysis. Figure 4 demonstrated that only the heavy alcohol consumption drinkers had an increased risk of colorectal SP, with the RR of 1.24 (95 % CI 1.01–1.52). Furthermore, the limited analysis showed that alcohol intake appeared to have a slight association with SSA and HP, with the RR of 1.14 (95 % CI 0.84–1.56) and 0.99 (95 % CI 0.86–1.14), respectively, when compared to all drinkers with non-/occasional drinkers (Table 2).
Pooled risk estimates for colorectal SP incidence for all drinkers versus non-/occasional drinkers, light drinkers versus non-/occasional drinkers, moderate drinkers versus non-/occasional drinkers and heavy drinkers vs. non-/occasional drinkers with respect to subgroup of SPs [hyperplastic ployps (HPs) and sessile serrated adenomas (SSAs)]
Sub-analysis of Smokers with SP
The risk factor of cigarette smoking can also be evaluated in the included studies, from which eight were associated with former/past smokers and nine were about the current/present smokers with colorectal SP. The studies on both past and current smokers demonstrated statistically increased risks of colorectal SP in contrast with the non-smokers, with RR of 1.58 (95 % CI 1.31–1.89) and 2.25 (95 % CI 1.78–2.86) in past smokers and current smokers, respectively (Fig. 5).
Meta-regression Analysis
We conducted a meta-regression analysis to investigate the impact of these study characteristics on the study estimates of RR. No variables such as study design, published year and geographical region, showed statistically significant associations with the sources of heterogeneity in univariate or multivariate meta-regression analyses.
Sensitivity Analysis
The sensitivity analysis was conducted by omitting one study at a time and calculating the pooled RRs for the remainder of the studies. There were no changes in the tendency of the risk effect when any one study was excluded. For instance, when the study by Burnett et al. [30] (the study that carried the most weight) was excluded from the analysis, the summarized RR of all drinkers remained significant (SRR 1.33; 95 % CI 1.21–1.45), compared with non-/occasional drinkers. Meanwhile, the RR for light drinkers (1.08, 95 % CI 0.94–1.24), moderate drinkers (1.26, 95 % CI 1.13–1.40) and heavy drinkers (1.72, 95 % CI 1.52–1.94) also share the same effect. Therefore, this analysis confirmed the stability of the risk tendency between alcohol consumption and colorectal SP (Fig. 6a–d).
Sensitivity analysis by omitting the study of Burnett-Hartman et al. [30] (the study that carried the most weight) and calculating the pooled RRs of the remaining studies when comparing all drinkers and non-/occasional drinkers (a), light drinkers and non-/occasional drinkers (b), moderate drinkers and non-/occasional drinkers (c), heavy drinkers and non-/occasional drinkers (d)
Publication Bias
The shape of the funnel plots for studies on the association between alcohol consumption and colorectal SP seemed to be symmetrical. What’s more, the P value of Begg’s adjusted rank correlation test was >0.05, indicating no statistical evidence of publication bias (Fig. 7a–d).
a Funnel plot of studies evaluating the association between all drinkers versus non-/occasional drinkers (Begg’s test, P = 0.030) and colorectal SP risk. b Funnel plot of studies evaluating the association between light drinkers versus non-/occasional drinkers (Begg’s test, P = 0.154) and colorectal SP risk. c Funnel plot of studies evaluating the association between moderate drinkers versus non-/occasional drinkers (Begg’s test, P = 0.144) and colorectal SP risk. d Funnel plot of studies evaluating the association between heavy drinkers versus non-/occasional drinkers (Begg’s test, P = 0.144) and colorectal SP risk
Dose–Response Meta-Analysis
Among the second-order fractional polynomial random effects models, the best explanatory variable is dose. The relationship between alcohol intake and CRA risk was ln (RR) = −0.09679 + 0.00569178 × dose. Compared with non-/occasional alcohol consumption, the fractional polynomial model estimates of RR were 0.96 (95 % CI 0.88–1.05), 1.05 (95 % CI 0.96–1.14), 1.21 (95 % CI 1.11–1.32) and 1.60 (95 % CI 1.47–1.75) for 10, 25, 50 and 100 g/day of alcohol intake, respectively (Fig. 8).
Discussion
The comprehensive meta-analysis attempted to reveal the association between alcohol consumption and colorectal SP by pooling the data from ten observational studies. The systematic review with meta-analysis and dose–response analysis of the alcohol and colorectal SP had never been reported before.
In general, the categorical meta-analysis demonstrated that all drinkers were associated with a 24 % increased risk of colorectal SP (RR 1.24; 95 % CI 1.07–1.44), and the RR of moderate drinkers (8–36 g/day) and heavy drinkers (≥36 g/day) were 1.19 (95 % CI 1.02–1.40) and 1.60 (95 % CI 1.35–1.91), respectively, when compared with the non-/occasional drinkers. Nevertheless, the light drinkers (≤8 g/day) might not have statistically significant influence on the colorectal SP, with an RR of 1.05 (95 % CI 0.93–1.18). Notably, the further dose–response analysis produced consistent results. For drinkers of 10, 25, 35, 50, 75, and 100 g/day alcohol intake, the estimated RRs of colorectal SP were 0.96 (95 % CI 0.88–1.05), 1.05 (95 % CI 0.96–1.14), 1.11 (95 % CI 1.02–1.21), 1.21 (95 % CI 1.11–1.32), 1.39 (95 % CI 1.28–1.52) and 1.60 (95 % CI 1.47–1.75) in the fractional polynomial model. Moreover, the correlation of alcohol consumption with increased risk of colorectal SP in the United States and Europe was stronger than in Asia, especially in comparison with the heavy dose in the subgroup analysis of geographical region, as well as in the subgroup analysis of race. In terms of sub-classification of colorectal SP, alcohol consumption had a greater influence on SSA than HP, with an RR of 1.14 (95 % CI 0.84–1.56) versus 0.99 (95 % CI 0.86–1.14) for all drinkers. Cigarette smoking both in the past and at present is associated closely with serrated polyps compared to non-smokers. The estimated RR of past smokers was 1.58 (95 % CI 1.31–1.89) and current smokers was 2.25 (95 % CI 1.78–2.86).
Although the mechanisms underlying the association between alcohol intake and the increased risk of colorectal SP were not clear, several possibilities have been hypothesized. Serrated neoplasia is a relatively new concept in the field of CRC pathogenesis. Recent studies have further indicated that some SPs may develop into serrated carcinomas via serrated pathways which account for approximately 35 % of the CRCs [33–36]. Unlike the traditional microsatellite-stabled adenoma-carcinoma pathways, these pathways are characterized by microsatellite instability through the nucleotide mismatch repair defect, methylation or loss of hMLH1 or methylguanine DNA methyltransferase (MGMT), exaggerated crypt serration, excess mucin expression, and evidence of architectural dysplasia [37–41]. Epidemiologic studies on CRC have suggested that risk factor profiles may have different effects between the microsatellite instability tumors and microsatellite stable tumors [42–44]. Alcohol may activate the BRAF gene mutation, which inhibits normal apoptosis of colonic epithelial cells. Furthermore, alcohol induces CpG island methylation (CIMP) that can lead the normal mucin to become serrated lesions which are mainly mirocvesicular hyperplastic polyps (MVHPs) and SSAs [37]. Additionally, intestinal bacteria can utilize the alcohol dehydrogenase to transfer excessive ethanol to acetaldehyde, which can change the status of the intestinal flora microecology [45]. Knowledge of risk factors and their effects in the early stage of tumorigenesis is the pivotal issue in the prevention of CRC [46]. Based on the results of the present study, the screening guideline of precancerous polyps could be adjusted to consider individuals who are accustomed to high dose of alcohol (≥36 g/day) as the susceptible population.
This meta-analysis has the following strengths: (1) studies were identified after a comprehensive exclusion criteria which includes at least three categories of alcohol consumption by a multidisciplinary work team having specialists in gastroenterology, gastrointestinal endoscopy and statistics, (2) study participants in the included studies were nearly homogeneous, for they all went through the endoscopy examination and had histological evidence if polyps were found in the colon or rectum, (3) in addition, the value of relative risk was extracted from the primary data source which could avoid confounders including cigarette smoking, nonsteroidal anti-inflammatory drug use, BMI level and other factors in the selected studies, (4) finally, subgroup analyses, sensitivity and meta-regression analyses were made to reduce or remove the sources of heterogeneity and to make some better understanding of the SP-CRC sequence.
However, the systematic review with the meta-analysis and dose–response analysis also has some limitations that might affect the results. First, nine of the selected studies used a case–control or cross-sectional design which may have the selection and recall bias more or less. Second, the results were influenced by the alcohol consumption misclassification resulting from the different classifications of the alcoholic levels in each included studies although we used the accurate statistics methods to integrate them. Furthermore, the significant heterogeneity was observed across the studies when pooling the estimate RRs of all drinkers, which to some extent might cast doubt on the reliability. This significant heterogeneity might come from the study design, characteristics of the population, duration of the follow-ups and unawareness of the accurate subgroup of serrated polyps or neoplasia. We were unable to clarify these confounders, despite the random-effect models. In addition, the distributions of some other lifestyle factors may have a co-effect of alcohol consumption in the progression of the disease that we could not clearly differentiate from our analysis.
In summary, this meta-analysis suggested that moderate or heavy alcohol intake was related to a significant increased risk of colorectal SP. To be specific, the risk was stronger in SSA than in HP, and significantly higher in white people than Asian. This systematic review shed light on the fact that alcohol consumption may to some extent be involved in the etiology and pathogenesis of colorectal SP to CRC and provided additional evidence that limiting heavy dose drinking is important for early prevention of colorectal SP and CRC.
Abbreviations
- SP:
-
Serrated polyp
- CRC:
-
Colorectal cancer
- HP:
-
Hyperplastic polyp
- SSA:
-
Sessile serrated adenoma
- TSA:
-
Traditional serrated adenoma
- RR:
-
Relative risk
- OR:
-
Odds ratio
- CI:
-
Confidence intervals
References
Boyle P, Langman JS. ABC of colorectal cancer: epidemiology. BMJ. 2000;321:805–808.
Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917.
Martinez ME, Baron JA, Lieberman DA, et al. A pooled analysis of advanced colorectal neoplasia diagnoses after colonoscopic polypectomy. Gastroenterology. 2009;136:832–841.
Cottet V, Jooste V, Fournel I, et al. Long-term risk of colorectal cancer after adenoma removal: a population-based cohort study. Gut. 2012;61:1180–1186.
Rosty C, Hewett DG, Brown IS, et al. Serrated polyps of the large intestine: current understanding of diagnosis, pathogenesis, and clinical management. J Gastroenterol. 2013;48:287–302.
Carr NJ, Mahajan H, Tan KL, et al. Serrated and non-serrated polyps of the colorectum: their prevalence in an unselected case series and correlation of BRAF mutation analysis with the diagnosis of sessile serrated adenoma. J Clin Pathol. 2009;62:516–518.
Spring KJ, Zhao ZZ, Karamatic R, et al. High prevalence of sessile serrated adenomas with BRAF mutations: a prospective study of patients undergoing colonoscopy. Gastroenterology. 2006;131:1400–1407.
Goldstein NS, Bhanot P, Odish E, et al. Hyperplastic-like colon polyps that preceded microsatellite-unstable adenocarcinomas. Am J Clin Pathol. 2003;119:778–796.
Higuchi T, Sugihara K, Jass JR. Demographic and pathological characteristics of serrated polyps of colorectum. Histopathology. 2005;47:32–40.
Rex DK, Ahnen DJ, Baron JA, et al. Serrated lesions of the colorectum: review and recommendations from an expert panel. Am J Gastroenterol. 2012;107:1315–1329; quiz 1314, 1330.
Lash RH, Genta RM, Schuler CM. Sessile serrated adenomas: prevalence of dysplasia and carcinoma in 2139 patients. J Clin Pathol. 2010;63:681–686.
Erhardt JG, Kreichgauer HP, Meisner C, Bode JC, Bode C. Alcohol, cigarette smoking, dietary factors and the risk of colorectal adenomas and hyperplastic polyps—a case control study. Eur J Nutr. 2002;2002:35–43.
Kearney J, Giovannucci E, Rimm EB, et al. Diet, alcohol, and smoking and the occurrence of hyperplastic polyps of the colon and rectum (United States). Cancer Causes Control. 1995;6:45–56.
Ben Q, An W, Jiang Y, et al. Body mass index increases risk for colorectal adenomas based on meta-analysis. Gastroenterology. 2012;142:762–772.
Stern MC, Siegmund KD, Conti DV, et al. XRCC1, XRCC3, and XPD polymorphisms as modifiers of the effect of smoking and alcohol on colorectal adenoma risk. Cancer Epidemiol Biomark Prev. 2006;15:2384–2390.
Peipins LA, Sandler RS. Epidemiology of colorectal adenomas. Epidemiol Rev. 1994;16:273–297.
Lieberman DA, Prindiville S, Weiss DG, et al. Risk factors for advanced colonic neoplasia and hyperplastic polyps in asymptomatic individuals. JAMA. 2003;290:2959–2967.
Morimoto LM, Newcomb PA, Ulrich CM, et al. Risk factors for hyperplastic and adenomatous polyps: evidence for malignant potential? Cancer Epidemiol Biomark Prev. 2002;11:1012–1018.
Shrubsole MJ, Wu H, Ness RM, et al. Alcohol drinking, cigarette smoking, and risk of colorectal adenomatous and hyperplastic polyps. Am J Epidemiol. 2008;167:1050–1058.
Martinez ME, McPherson RS, Levin B, et al. A case–control study of dietary intake and other lifestyle risk factors for hyperplastic polyps. Gastroenterology. 1997;113:423–429.
Bingham SA. Diet and large bowel cancer. J R Soc Med. 1990;83:420–422.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34.
Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634.
van Houwelingen HC, Arends LR, Stijnen T. Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat Med. 2002;21:589–624.
Bagnardi V, Zambon A, Quatto P, et al. Flexible meta-regression functions for modeling aggregate dose-response data, with an application to alcohol and mortality. Am J Epidemiol. 2004;159:1077–1086.
Ulrich CM, Kampman E, Bigler J, et al. Lack of association between the C677T MTHFR polymorphism and colorectal hyperplastic polyps. Cancer Epidemiol Biomark Prev. 2000;9:427–433.
Jung AY, Poole EM, Bigler J, et al. DNA methyltransferase and alcohol dehydrogenase: gene-nutrient interactions in relation to risk of colorectal polyps. Cancer Epidemiol Biomark Prev. 2008;17:330–338.
Burnett-Hartman AN, Passarelli MN, Adams SV, et al. Differences in epidemiologic risk factors for colorectal adenomas and serrated polyps by lesion severity and anatomical site. Am J Epidemiol. 2013;177:625–637.
Hassan C, Pickhardt PJ, Marmo R, et al. Impact of lifestyle factors on colorectal polyp detection in the screening setting. Dis Colon Rectum. 2010;53:1328–1333.
Wang FW, Hsu PI, Chuang HY, et al. Prevalence and risk factors of asymptomatic colorectal polyps in Taiwan. Gastroenterol Res Pract. 2014;2014:985205.
Hawkins NJ, Ward RL. Sporadic colorectal cancers with microsatellite instability and their possible origin in hyperplastic polyps and serrated adenomas. J Natl Cancer Inst. 2001;93:1307–1313.
Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010;138:2088–2100.
Huang CS, O’Brien MJ, Yang S, et al. Hyperplastic polyps, serrated adenomas, and the serrated polyp neoplasia pathway. Am J Gastroenterol. 2004;99:2242–2255.
Snover DC. Update on the serrated pathway to colorectal carcinoma. Hum Pathol. 2011;42:1–10.
Torlakovic E, Skovlund E, Snover DC, et al. Morphologic reappraisal of serrated colorectal polyps. Am J Surg Pathol. 2003;27:65–81.
O’Brien MJ, Yang S, Mack C, et al. Comparison of microsatellite instability, CpG island methylation phenotype, BRAF and KRAS status in serrated polyps and traditional adenomas indicates separate pathways to distinct colorectal carcinoma end points. Am J Surg Pathol. 2006;30:1491–1501.
Baker K, Zhang Y, Jin C, et al. Proximal versus distal hyperplastic polyps of the colorectum: different lesions or a biological spectrum? J Clin Pathol. 2004;57:1089–1093.
Issa JP. The epigenetics of colorectal cancer. Ann N Y Acad Sci. 2000;910:140–153; discussion 153–155.
Torlakovic E, Snover DC. Sessile serrated adenoma: a brief history and current status. Crit Rev Oncog. 2006;12:27–39.
Slattery ML, Curtin K, Anderson K, et al. Associations between cigarette smoking, lifestyle factors, and microsatellite instability in colon tumors. J Natl Cancer Inst. 2000;92:1831–1836.
Limsui D, Vierkant RA, Tillmans LS, et al. Cigarette smoking and colorectal cancer risk by molecularly defined subtypes. J Natl Cancer Inst. 2010;102:1012–1022.
Campbell PT, Jacobs ET, Ulrich CM, et al. Case-control study of overweight, obesity, and colorectal cancer risk, overall and by tumor microsatellite instability status. J Natl Cancer Inst. 2010;102:391–400.
Giovannucci E. Epidemiologic studies of folate and colorectal neoplasia: a review. J Nutr. 2002;132:2350s–2355s.
Acott AA, Theus SA, Marchant-Miros KE, et al. Association of tobacco and alcohol use with earlier development of colorectal cancer: Should we modify screening guidelines? Am J Surg. 2008;196:915–918; discussion 918–919.
Conflict of interest
The authors have declared that no conflicts of interest exist.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yu-Ming Wang and Qin-Yi Zhou have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, YM., Zhou, QY., Zhu, JZ. et al. Systematic Review with Meta-Analysis: Alcohol Consumption and Risk of Colorectal Serrated Polyp. Dig Dis Sci 60, 1889–1902 (2015). https://doi.org/10.1007/s10620-014-3518-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3518-3