Abstract
Background
Several meta-analyses and reports from the World Cancer Research Fund supported a risk association between alcohol consumption and colorectal cancer (CRC). However, the association for beer consumption, the common type of alcoholic beverage, remains unclear.
Methods
We identified studies by a literature search of PUBMED and EMBASE through 30 June 2014. Summary relative risks (SRRs) with their 95 % CIs were calculated with a fixed or random effects model.
Results
Twelve case–control and nine cohort studies were included. Compared with non-alcohol drinkers or non-beer drinkers, any beer drinkers were associated with an increased risk of CRC (SRR = 1.20, 95 % CI, 1.06–1.37; p heterogeneity <0.001, I 2 = 73.3 %), which was stronger in the rectum than in the colon. The categorical meta-analysis indicated that heavy (≥2 drinks/day) beer drinking was related to increased risk of CRC (SRR = 1.37, 95 % CI 1.26–1.49), while light or moderate beer drinking was not. The dose–response analysis demonstrated that an increase of one drink per day in beer consumption was related to an increased risk of CRC (SRR = 1.13, 95 % CI, 1.06–1.21). There was evidence of a potential nonlinear association between beer intake and CRC incidence (p = 0.002 for nonlinearity).
Conclusions
The results from this meta-analysis suggest that heavy (≥2 drinks/day) beer drinking may be associated with increased CRC risk. More researches with improved control of confounding and actual measurement of beer consumption are needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol drinking has been identified as an important risk factor for several cancers, including colorectal cancer (CRC) [1], which ranks the fourth most commonly diagnosed cancer and the second most common cause of cancer death in North America [2]. Great investment has been made to gain new insight into effects of environmental and genetic factors on the development of CRC [3, 4]. Several meta-analyses and reports from the Working Group of World Cancer Research Fund (WCRF) systematic literature review continuous update project (CUP) [5, 6] have supported a positive risk association between alcohol consumption and CRC.
Consumption of beer is one of the most common types of alcoholic beverage in the world, and mixed results have been reported for the association of CRC risk in many studies [7–27]. Some observational studies have reported an increase in CRC risk of those who drank more beer [7, 10, 13, 25, 27], while a non-significantly risk association was observed in most of cohort studies [8, 12, 15, 21, 22]. The report from the CUP showed a summary relative risk (RR) for an increase in beer consumption per one drink/day of 1.11 (95 % CI, 1.03–1.21) for CRC incidence, 1.05 (95 % CI, 0.94–1.17) for colon cancer and 1.21 (95 % CI, 1.04–1.42) for rectal cancer. However, this report was based on only four cohort studies [20, 21, 28, 29].
Therefore, to better characterize this issue, we conducted a comprehensive meta-analysis of observational studies by using our own methods and criteria. We also examined the shape of the dose–response relationship (i.e., whether there are any threshold effects) by conducting nonlinear dose–response analyses. A categorical quantification review of the association for light, moderate, and heavy beer consumption and incidence of CRC was also conducted.
Methods
Data sources and searches
Two independent investigators (Z. C. and Z. M.) identified publications using PubMed and EMBASE from the beginning of indexing for each database until 30 June 2014. We searched the relevant studies using the following text words and/or medical subject heading (MeSH) terms: “alcohol OR ethanol OR vodka OR alcoholic beverages OR beer,” “colorectal OR colon OR rectum OR large bowel,” “cancer OR carcinoma,” AND “case–control OR cohort.” To identify additional studies, we performed hand searches in the reference lists of the identified articles. Only articles written in English were included.
Study selection
We independently evaluated all of the studies retrieved according to the pre-specified selection criteria. To be included, the study had to meet the following criteria: (1) published as original articles using a case–control or cohort design; (2) reported RR estimates and corresponding 95 % CI for consumption of beer and CRC incidence at least adjusted or matched for age. If results based on the same study population were reported in more than one study, we included the one with the largest number of cases. Two cohort studies [28, 29] included in the CUP were updated by the larger studies [19, 21]. We also excluded studies using CRC mortality as outcome of interest.
Data extraction and quality assessment
We extracted the following information from each included study: publication year, the first author’s last name, country of origin, study design, number of cases, sex, number of controls and participants, method of epidemiologic data collection, source of controls, duration of follow-up in cohort studies, and matching or covariates adjusted for in the analysis. For studies that reported several multivariable-adjusted risk estimates, we extracted the ones that reflected the greatest degree of control for potential confounders. In case of studies that reported risk estimations separately for men and women, and for cancer subsites, we treated them as if they were from different studies. To assess the study quality, two of us (Z. C. and Z. M.) adopted the Newcastle–Ottawa quality assessment scale (NOS) [30]. The NOS uses three parameters of quality for case–control or cohort studies: selection (n = 4 stars), comparability (n = 2 stars), and exposure/outcome assessment (n = 3 stars). Thus, the total score was nine stars, and a study with seven or more stars was defined as a high-quality study.
Statistical methods
Given the fact that different studies used different ways to describe the consumption level, the following formularies were used for the conversion: A drink of beer was defined as a 12-ounce serving or 330 ml per bottle, or contained 13 g of ethanol. We categorized beer consumption into any, light (<1 drink/day), moderate (1–2 drinks/day), and heavy intake (≥2 drinks/day) based on accepted definitions from dietary guidelines for Americans (2005) [18, 31]. When more than one study category fell in the range considered for light, moderate, or heavy beer drinking, we combined the corresponding risk estimates using the method according to a fixed effect model. Nondrinkers or occasional alcohol drinkers were the reference category.
All statistical analyses were performed using STATA, version 11.0 (College Station, TX, USA) and R-package statistical software (version 2.11.0 beta). All the tests were 2-tailed; tests of significance were evaluated at the p < 0.05 levels. We used the method of a random effects model to calculate summary relative risks (SRRs) and 95 % CIs of CRA, which considered both within- and between-study variations [32].
In assessing heterogeneity among studies, we used the Cochran Q and I 2 statistics [33]. I 2 assess the percentage of variability in the effect estimates that is due to heterogeneity rather than chance, and a value >50 % is considered a measure of severe heterogeneity. Stratified analyses were performed according to study design (case–control vs. cohort), sex, geographic locations (Asia, the USA and Europe), cancer subsites, method of epidemiologic data collection, contrast (abstainer and non-beer drinkers), type of FFQ, and study quality score. Confounders were defined as total alcohol consumption, tobacco smoking, body mass index (BMI), physical activity, and dietary energy intake, all of which have been reported to be associated with the risk of CRC. We also conducted sensitivity analysis to estimate the influence of each individual study on the summary results by repeating the meta-analysis after omitting one study at a time.
Dose–response relationships were expressed per increment of intake of one drink per day for beer and risk of CRC using generalized least-squares trend estimation (GLST) analysis, which requires three or more levels of intake categories. [34, 35] Means or medians of the intake categories were used when reported in the articles; if not reported, midpoints were assigned to the relative risk of the corresponding category. Zero consumption was used as boundary when the lowest category was open-ended. If the highest category was open-ended, it was assumed that the open-ended interval length had the same length as the adjacent interval.
A potential nonlinear dose–response relationship was checked by fractional polynomial models [36]. The best-fitting second-order fractional polynomial regression model was defined as the one with the lowest deviance. A likelihood ratio test was used to assess the difference between the nonlinear and linear models to test for nonlinearity [36].
Several methods were used to evaluate the publication bias. Visual inspection of asymmetry in funnel plots was performed. We also conducted formal testing using the Begg’s adjusted rank correlation and Egger’s weighted regression test [37].
Results
Study characteristics
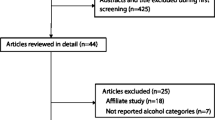
Figure 1 showed the selection process for the studies involved in this meta-analysis. The search strategy yielded 1464 citations. After excluding the duplicates, 1049 titles and abstracts were screened. Ninety-five of these were considered of potential value and the full text was retrieved for detailed evaluation. Seventy-eight of these 95 articles were excluded from the meta-analysis due to various reasons. By hand-search of reference lists, additional four articles were included. Thus, a total of 12 independent case–control studies and nine cohort studies concerning CRC incidence and intakes of beer were identified. As shown in Tables 1, 2, a total of 10,736 cases of CRC were used, and four studies were from Asia, eight studies from the USA, eight studies from Europe, and one study from Australia. As shown in supplementary Table 1, the quality scores ranged from five to nine. The majority of included studies (15/21) were of high quality (NOS score ≥7).
Any beer drinkers versus nondrinkers
Overall, summary RR of any beer drinkers with respect to non-alcohol drinkers or non-beer drinkers was 1.20 (95 % CI, 1.06–1.37), with evidence of significant heterogeneity (Q = 97.46, p heterogeneity <0.001, I 2 = 73.3 %; Fig. 2). We observed no evidence of publication bias according to the Egger’ test (p = 0.75) and Begg’s test (p = 0.72; Fig. 3). As shown in supplementary Fig. 1A–C, the categorical SRRs for comparison with non-/occasional drinkers were as follows: light drinkers, 1.03 (95 % CI, 0.95–1.11); moderate drinkers, 1.09 (95 % CI, 0.91–1.31); heavy drinkers, 1.37 (95 % CI, 1.26–1.49). There was no evidence of publication bias for light, moderate, and heavy drinkers (supplementary Fig. 2A–C).
When stratifying based on study design, we found an increased risk of CRC in both case–control (SRR = 1.29, 95 % CI, 1.00–1.66) and cohort studies (SRR = 1.08, 95 % CI, 1.02–1.15). In stratified analysis by sex, the SRR estimated for CRC incidence was 1.15 (95 % CI, 0.66–2.03) in males and 0.96 (95 % CI, 0.69–1.33) in females. When stratified analysis for site of cancer, summary RR estimates were significant for both colon cancer (SRR = 1.05, 95 % CI, 1.00–1.14) and rectal cancer (SRR = 1.30, 95 % CI 1.10–1.55), with significant heterogeneity (p = 0.03). We found an elevated risk associations between beer consumption and CRC risk for studies conducted in Europe (SRR = 1.34, 95 % CI, 1.09–1.66), but not in the US (SRR = 1.10, 95 % CI, 0.95–1.26) and Asia (SRR = 0.87, 95 % CI, 0.62–1.22). Studies with low quality (NOS < 7) showed a stronger risk relationship than studies with high quality did (p for difference = 0.04), although both risk estimates were significant. Furthermore, both the methods of data collection and type of FFQ did not significantly alter this risk relation.
We then conducted subgroup analyses by adjustment for confounders of total alcohol consumption, tobacco smoking, BMI, physical activity, and dietary energy intake. The SRR estimated for CRC incidence were positive in all strata, except when the summary estimates were not adjusted by smoking status (Table 3).
We conducted a meta-regression analysis to investigate the impact of the above study characteristics on the risk relations. We found that both study quality score (p = 0.04) and study locations (p = 0.03) were statistically significant factors for the association between beer intake and CRC incidence. We found that the study from Zhivotovskiy et al. [27] contributed to most of the heterogeneity among studies, and the SRR was decreased with moderate heterogeneity when this study was excluded (SRR = 1.12, 95 % CI 1.02–1.23, p = 0.005, I 2 = 46.7 %). For categorical analysis of moderate drinkers, we found the study from Kune et al. [25] contributed to most of the heterogeneity among studies.
Dose–response analysis
Two studies [17, 20] presented RR of CRC for continuous increase in beer consumption (per one drink/d), and the other eight studies [7, 9, 15, 16, 19, 21, 24, 25] presented data for more than three categorized exposure levels. Meta-analysis of these ten studies showed that an increased intake of one drink of beer per day was associated with 13 % excess risk of CRC (SRR = 1.13, 95 % CI, 1.06–1.21), with evidence of significant heterogeneity (p heterogeneity = 0.002, I 2 = 62.0 %). Stratified analysis by study design showed a similar risk association (case–control: SRR = 1.17, 95 % CI, 1.01–1.36; Cohort: SRR = 1.13, 95 % CI, 1.03–1.16; Fig. 4a). There was evidence of a potential nonlinear association between beer intake and CRC risk (p = 0.002 for nonlinearity; Fig. 4b). The relationship between beer intake and CRA risk was ln (RR) = 0.0931 * dose^2 + 0.0440 * dose.
Discussion
To our knowledge, this is the first comprehensive meta-analysis of specific type of alcoholic beverage (beer) intake and CRC risk. Results from this meta-analysis found that any beer drinkers were associated with 20 % increased risk of CRC, compared with nondrinkers or occasional alcohol drinkers, which is stronger for rectal cancer than that for colon cancer. The dose–response analysis found 13 % increased risk of CRC for per one drink/day increased intake of beer, and we found evidence of a nonlinear association between beer consumption and CRC incidence. Furthermore, the categorical meta-analysis indicated that light or moderate beer drinking was not related to increased risk; however, heavy (≥2 drinks/day) beer drinkers have an increased risk of CRC development.
The previous meta-analysis from Fedirko et al. [5] presented a stronger CRC risk association with any/light alcohol drinking in the rectum than that in the colon, although it was not made for moderate/heavy alcohol drinking. Within the Netherlands Cohort Study [21], which presented data on beer consumption and CRC subsites, authors found increasing risks advancing from the proximal colon to the rectum, suggesting a subsite-specific effect. In line with the meta-analysis and the cohort study, results from our analyses also indicated a stronger cancer risk of any beer drinker in the rectum than in the colon. The reasons for this disparity in site association remain not clear. It is assumed that differences in anatomic, embryologic, and physiologic evidence between colon and rectum have indicated that they may have partly different etiologic pathways and should probably be considered as two separate entities [38].
Furthermore, the categorical meta-analysis indicated that light or moderate beer drinking was not related to increased CRC risk; however, heavy beer drinking had ~50 % increased risk. These results may be accounted by the presence of a nonlinear dose–response relation, i.e., consumption of beer at <2 drinks per day is not associated with CRC incidence, whereas above this consumption level, the risk of CRC would become significant and evidently stronger. We should note that association does not prove cause and effect, but the presence of a dose–response relation is important. The risks of excess beer drinking should always be highlighted, and heavy beer drinkers should be pushed to cut down, or even quit, their beer consumption.
Meta-analyses of the observational studies have supported the positive relationship between alcohol consumption and CRC risk varied according to sex, and indicated that the CRC-moderate alcohol drinking association is stronger among men than among women [5]. The suggested mechanism for this sex difference in alcohol–CRC association may be related to the differences in alcohol metabolism by gender [39]. Epidemiological studies have reported that women appear to become more susceptible to carcinogenesis than men after drinking equivalent amounts of alcohol [40]. Our data, however, showed similar results between beer consumption and sex, consistent with the large meta-analyses, the Pooling Project [41] and the EPIC study [29]. Reasons for the disparity in the association of gender and cancer are not clear. However, it may be inferred that use of different statistical methods and the presence of a nonlinear association may partially account for this discrepancy. In addition, we should be cautious that these associations were only due to chance, given that only three or four studies were included, resulting in the probability of the presence of type Ι error.
Stratified analysis according to study design showed a somewhat stronger risk of CRC in case–control studies compared with cohort studies (SRR: 1.30 vs. 1.08). Among the 21 studies included in this meta-analysis, 12 studies used a case–control design, which was more susceptible to recall and selection biases, especially dietary recall bias, than a cohort design. In case–control studies, exposure information was available after the cancer diagnosis, thus, may be subject to recall bias and inaccurate measurements of beer intake. In cohort studies, alcohol consumption was assessed only once at baseline and based on “self-reported” in most studies. However, results of the EPIC cohort showed that associations between average lifetime alcohol intake and CRC risk were similar to those between baseline consumption and CRC risk [19]. Furthermore, our analyses observed an enhanced risk association between beer consumption and cancer incidence in both case–control and cohort studies, which may strengthen this positive association.
The suggested mechanisms for the potential carcinogenic effect of beer consumption included: (1) the generation of common metabolite acetaldehyde, which has been found to increase cellular proliferation rate and to cause cellular injury and gene mutations [42], biomarkers of cancer risk, in the rectal mucosa. (2) The interrupted metabolic of folate [43], and thus leading to folate deficiency in the colon and rectum, which may increase risk of CRC via alteration in DNA integrity and stability; (3) The enhanced induction of cytochrome p450 activity, which may activate other procarcinogens [44, 45]. In addition to ethanol, the presence of carcinogenic compounds in beer [46], such as nitrosamines, polycyclic aromatic hydrocarbons (PAH), and arsenic pesticide residues, may also contribute to the increased cancer risk.
The advantages of the current study include as follows: (1) The majority of the included studies evaluated multiple confounders including diet factors, physical activity, BMI, and smoking. (2) The observed significant dose–response relation between beer intake and risk of CRC further strengthened this association. Our findings also indicate there are threshold effects of beer consumption on CRC incidence.
Our meta-analysis has some limitations. First, our findings were likely to be influenced by imprecise assessments of beer intake, which could have led to a tendency for RR to be biased toward the null hypothesis. Thus, the actual risk associations between beer consumption and CRC incidence may be stronger than our results. In addition, non-validated questionnaire and self-administered data collection were used for dietary assessment in several studies, although subgroup analyses by methods of data collection and type of FFQ did not found a significant change in the association between beer intake and CRC risk.
Second, residual confounders are always of concern in observational studies. It is hard to elaborate the independent effect of beer on CRC risk given people always drink other alcoholic beverages together. However, combining the six studies [10, 13, 15, 21, 23, 25], which were adjusted by total alcohol consumption, showed a similar SRR with that from studies not controlling for this variable. These results indicated an effect of beer consumption on CRC, independent of alcohol use. However, it is important to note that the number of studies adjusted by alcohol use was small. More researches controlling for total alcohol consumption are needed.
Alcohol abuse may be associated with behaviors that predispose to colorectal neoplasm, such as tobacco smoking, low physical activity, obesity, dietary, and high-energy and high-fat intake [47–49]. However, restricting the meta-analysis to studies which were controlled for these potential confounders, the positive association was not significantly altered. Furthermore, beer drinking may result in folate deficiency in the colon and rectum, which may increase risk of colorectal neoplasms; however, we did not examine whether this association was changed by folate status, because only one study was adjusted by this variable [13]. Although most included studies were adjusted for a wide range of potential confounders for CRC, we still could not exclude the possibility that other unmeasured or inadequately measured factors have confounded the true association.
Third, high heterogeneity was observed for case–control analysis and overall analysis. Based on sensitivity analysis, we found that a study from Russia [27], which observed significantly stronger risk estimation for any beer drinkers (RR = 9.24, 95 % CI 5.14–16.61), contributed to most of the heterogeneity among studies and the higher risk association. When this study was excluded, the summary RR was decreased, not significant for case–control studies, with moderate heterogeneity (I 2 = 46.7 %). Likewise, this study also contributed to the stronger risk association among European populations with regard to Asian and American populations. Furthermore, they may be ascribed to different types of beer available, different consumption patterns of alcoholic beverages between Russia and the other regions and the different screening guidelines among the different countries. In Russia, the alcohol-attributable fraction of all-cause mortality was estimated to be over 50 % in the 15–54 year old, particularly for men, exceeding the attributable fractions of other countries in Europe and elsewhere [50, 51].
Forth, whether quitting beer drinking would reduce risk of CRC would be interesting and informative, which would lend stronger support to a causal role of beer consumption in colorectal carcinogenesis. However, to the best of our knowledge, few reports have examined the effect of stopping alcohol use, especially specific type of alcohol beverages, on CRC risk. One previous case–control study from China observed a progressive reduction in CRC risks with increasing duration of alcohol abstention in a dose-responsive manner [52]. Moreover, the risk reduction was independent of the frequency and the amount of alcohol consumed [52]. Although the other study from Italy found no association between CRC risk and drinking cessation, it failed to demonstrate any relationship between alcohol drinking and CRC risk [53].
Finally, the possibility of publication bias is inevitable, because studies with null results and with insufficient information to estimate an adjusted RR tend to be unpublished. However, the results obtained from funnel plot analysis and formal statistical tests did not provide evidence for such bias in any, light, moderate, and heavy beer drinking analysis.
Our results suggest that heavy beer drinking may have an adverse effect on cancer incidence in the colorectum, especially in the rectum. These findings have important implications for countries where beer is consumed heavily. More researches with improved control of confounding and actual measurement of beer consumption are needed to confirm these findings.
References
Boffetta P, Hashibe M, La Vecchia C et al (2006) The burden of cancer attributable to alcohol drinking. Int J Cancer 119:884–887
Jemal A, Siegel R, Ward E et al (2006) Cancer statistics, 2006. CA Cancer J Clin 56:106–130
Lochhead P, Chan AT, Giovannucci E et al (2014) Progress and opportunities in molecular pathological epidemiology of colorectal premalignant lesions. Am J Gastroenterol 109:1205–1214
Brenner H, Kloor M, Pox CP (2014) Colorectal cancer. Lancet 383:1490–1502
Fedirko V, Tramacere I, Bagnardi V et al (2011) Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol 22:1958–1972
WCRF/AICR Systematic Literature Review Continuous Update Project Report (2011) The Associations between Food, Nutrition and Physical Activity and the Risk of Colorectal Cancer. AICR, Washington
Kabat GC, Howson CP, Wynder EL (1986) Beer consumption and rectal cancer. Int J Epidemiol 15:494–501
Klatsky AL, Armstrong MA, Friedman GD et al (1988) The relations of alcoholic beverage use to colon and rectal cancer. Am J Epidemiol 128:1007–1015
Peters RK, Garabrant DH, Yu MC et al (1989) A case–control study of occupational and dietary factors in colorectal cancer in young men by subsite. Cancer Res 49:5459–5468
Riboli E, Cornee J, Macquart-Moulin G et al (1991) Cancer and polyps of the colorectum and lifetime consumption of beer and other alcoholic beverages. Am J Epidemiol 134:157–166
Hoshiyama Y, Sekine T, Sasaba T (1993) A case–control study of colorectal cancer and its relation to diet, cigarettes, and alcohol consumption in Saitama Prefecture, Japan. Tohoku J Exp Med 171:153–165
Gapstur SM, Potter JD, Folsom AR (1994) Alcohol consumption and colon and rectal cancer in postmenopausal women. Int J Epidemiol 23:50–57
Boutron MC, Faivre J, Dop MC et al (1995) Tobacco, alcohol, and colorectal tumors: a multistep process. Am J Epidemiol 141:1038–1046
Knekt P, Jarvinen R, Dich J et al (1999) Risk of colorectal and other gastro-intestinal cancers after exposure to nitrate, nitrite and N-nitroso compounds: a follow-up study. Int J Cancer 80:852–856
Pedersen A, Johansen C, Gronbaek M (2003) Relations between amount and type of alcohol and colon and rectal cancer in a Danish population based cohort study. Gut 52:861–867
Murtaugh MA, Ma KN, Caan BJ et al (2004) Association of fluids from beverages with risk of rectal cancer. Nutr Cancer 49:25–31
Su LJ, Arab L (2004) Alcohol consumption and risk of colon cancer: evidence from the national health and nutrition examination survey I epidemiologic follow-up study. Nutr Cancer 50:111–119
Anderson JC, Alpern Z, Sethi G et al (2005) Prevalence and risk of colorectal neoplasia in consumers of alcohol in a screening population. Am J Gastroenterol 100:2049–2055
Ferrari P, Jenab M, Norat T et al (2007) Lifetime and baseline alcohol intake and risk of colon and rectal cancers in the European prospective investigation into cancer and nutrition (EPIC). Int J Cancer 121:2065–2072
Tsong WH, Koh WP, Yuan JM et al (2007) Cigarettes and alcohol in relation to colorectal cancer: the Singapore Chinese Health Study. Br J Cancer 96:821–827
Bongaerts BW, van den Brandt PA, Goldbohm RA et al (2008) Alcohol consumption, type of alcoholic beverage and risk of colorectal cancer at specific subsites. Int J Cancer 123:2411–2417
Lim HJ, Park BJ (2008) Cohort study on the association between alcohol consumption and the risk of colorectal cancer in the Korean elderly. J Prev Med Public Health 41:23–29
Omata F, Brown WR, Tokuda Y et al (2009) Modifiable risk factors for colorectal neoplasms and hyperplastic polyps. Intern Med 48:123–128
Crockett SD, Long MD, Dellon ES et al (2011) Inverse relationship between moderate alcohol intake and rectal cancer: analysis of the North Carolina Colon Cancer Study. Dis Colon Rectum 54:887–894
Kune G, Watson L (2011) Lowering the risk of rectal cancer among habitual beer drinkers by dietary means. Adv Prev Med 2011:1–5
Kontou N, Psaltopoulou T, Soupos N et al (2012) Alcohol consumption and colorectal cancer in a Mediterranean population: a case–control study. Dis Colon Rectum 55:703–710
Zhivotovskiy AS, Kutikhin AG, Azanov AZ et al (2012) Colorectal cancer risk factors among the population of South-East Siberia: a case–control study. Asian Pac J Cancer Prev 13:5183–5188
Bongaerts BW, de Goeij AF, van den Brandt PA et al (2006) Alcohol and the risk of colon and rectal cancer with mutations in the K-ras gene. Alcohol 38:147–154
Park JY, Mitrou PN, Dahm CC et al (2009) Baseline alcohol consumption, type of alcoholic beverage and risk of colorectal cancer in the European Prospective Investigation into Cancer and Nutrition-Norfolk study. Cancer Epidemiol 33:347–354
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P.(The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/ oxford.asp. Accessed 15 June 2012
Sterne JAC, Egger M, Moher D (eds) (2008) Chapter 10: Addressing reporting biases. In Cochrane Handbook for Systematic Reviews of Interventions, Version 5.0.1 [updated September 2008]. Higgins JPT, Green S (eds) The Cochrane Collaboration. www.cochrane-handbook.org
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135:1301–1309
Orsini NBR, Greenland S (2006) Generalized least squares for trend estimation of summarized dose-response data. Stata J 6:40–57
Royston P (2000) A strategy for modelling the effect of a continuous covariate in medicine and epidemiology. Stat Med 19:1831–1847
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Li FY, Lai MD (2009) Colorectal cancer, one entity or three. J Zhejiang Univ Sci B 10:219–229
Angstadt AY, Berg A, Zhu J et al (2013) The effect of copy number variation in the phase II detoxification genes UGT2B17 and UGT2B28 on colorectal cancer risk. Cancer 119:2477–2485
Otani T, Iwasaki M, Yamamoto S et al (2003) Alcohol consumption, smoking, and subsequent risk of colorectal cancer in middle-aged and elderly Japanese men and women: Japan Public Health Center-based prospective study. Cancer Epidemiol Biomarkers Prev 12:1492–1500
Cho E, Smith-Warner SA, Ritz J et al (2004) Alcohol intake and colorectal cancer: a pooled analysis of 8 cohort studies. Ann Intern Med 140:603–613
Seitz HK, Poschl G, Simanowski UA (1998) Alcohol and cancer. Recent Dev Alcohol 14:67–95
Islam T, Ito H, Sueta A et al (2013) Alcohol and dietary folate intake and the risk of breast cancer: a case–control study in Japan. Eur J Cancer Prev 22:358–366
Boffetta P, Hashibe M (2006) Alcohol and cancer. Lancet Oncol 7:149–156
Seitz HK, Becker P (2007) Alcohol metabolism and cancer risk. Alcohol Res Health 30(38–41):37–44
Lijinsky W (1999) N-Nitroso compounds in the diet. Mutat Res 443:129–138
Breslow RA, Guenther PM, Juan W et al (2010) Alcoholic beverage consumption, nutrient intakes, and diet quality in the US adult population, 1999-2006. J Am Diet Assoc 110:551–562
Hansel B, Thomas F, Pannier B et al (2010) Relationship between alcohol intake, health and social status and cardiovascular risk factors in the Urban Paris-Ile-de-France Cohort: is the cardioprotective action of alcohol a myth? Eur J Clin Nutr 2164:561–568
Paavola M, Vartiainen E, Haukkala A (2004) Smoking, alcohol use, and physical activity: a 13-year longitudinal study ranging from adolescence into adulthood. J Adolesc Health 35:238–244
Rehm J, Baliunas D, Borges GL et al (2010) The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction 105:817–843
Leon DA, Shkolnikov VM, McKee M (2009) Alcohol and Russian mortality: a continuing crisis. Addiction 104:1630–1636
Ho JW, Lam TH, Tse CW et al (2004) Smoking, drinking and colorectal cancer in Hong Kong Chinese: a case–control study. Int J Cancer 109:587–597
Tavani A, Ferraroni M, Mezzetti M et al (1998) Alcohol intake and risk of cancers of the colon and rectum. Nutr Cancer 30:213–219
Conflict of interests
The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10552_2015_532_MOESM2_ESM.doc
Supplementary Fig. 1: Pooled risk estimates for colorectal cancer for light (less than 1 drink/day, A), moderate (1–2 drinks/day, B), heavy (2 or more than 2 drinks/day, C) beer drinkers versus nondrinkers or occasional drinkers from case–control and cohort studies. Supplementary material 2 (DOC 33 kb)
10552_2015_532_MOESM3_ESM.tif
Supplementary Fig. 2: Funnel plot of studies evaluating the association between light, moderate, and heavy beer drinkers vs. non-/occasional drinkers and colorectal cancer risk, according to the Begg’s adjusted rank correlation test. Supplementary material 3 (TIFF 4790 kb)
Rights and permissions
About this article
Cite this article
Zhang, C., Zhong, M. Consumption of beer and colorectal cancer incidence: a meta-analysis of observational studies. Cancer Causes Control 26, 549–560 (2015). https://doi.org/10.1007/s10552-015-0532-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-015-0532-5