Abstract
Background
Cardiopulmonary bypass (CPB) is commonly applied to support circulation during heart surgery but frequently causes adverse effects.
Aims
The purpose of this study was to examine the potential of probiotics to improve small intestinal mucosa barrier function after CPB.
Methods
Twenty-four adult male SD rats were randomly divided into sham-operated (S), CPB-operated (CPB), and probiotic-fed (Y) groups. Diamine oxidase (DAO) activity and concentrations of D-lactic acid, endotoxin, TNFα, and IL-6 were measured in portal vein blood. IgA concentrations were determined in plasma and the small intestine. Vena cava blood and tissue samples were used to monitor bacterial growth. Intestinal epithelial ultrastructure was analyzed by transmission electron microscopy (TEM). Occludin and ZO-1 expression levels in the intestinal epithelium were detected by western blotting and immunohistochemistry, respectively.
Results
D-lactic acid, endotoxin, TNFα and IL-6 levels, DAO activity, and bacterial translocation rate were increased (P < 0.05) in CPB and Y compared to the S group. The above indices were relatively lower (P < 0.05) in Y than in CPB. Plasma and small intestinal IgA levels were significantly lower (P < 0.05) in CPB, while in Y they were significantly increased (P < 0.05) but lower than in S (P < 0.05). These results were confirmed by TEM. Consistently, occludin and ZO-1 expression levels were significantly higher in Y than in CPB (P < 0.05) but still lower compared to S (P < 0.05).
Conclusion
Pre-administration of probiotics can improve, to some extent, intestinal barrier function after CPB in rats, and this effect is likely related to inhibition of the CPB-induced inflammatory response, improvement in local intestinal immune function, and increased expression of intestinal epithelial tight junction proteins.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiopulmonary bypass (CPB) is commonly used to support circulation during heart surgery. However, CPB leads to damage of the intestinal mucosa, resulting in bacterial translocation and endotoxemia [1]. These effects synergistically contribute to the development of systemic inflammatory response syndrome (SIRS) and multiple organ dysfunction syndrome, which are leading causes of severe complications after cardiac surgery [2]. Previous studies have attempted to mitigate this problem via inhibition of inflammation and elevation of intestinal perfusion, oxygen supply, and other measures to protect intestinal barrier function during CPB, but the outcome was not positive [3–5]. Therefore, it is of great significance to develop a treatment that reduces the number of potential pathogenic bacteria and endotoxin levels in the intestine. To offer clinical benefits, this treatment should also maintain the balance of intestinal flora and enhance the physical barrier and immune functions of the intestinal tract, thereby reducing bacterial translocation and inflammatory response after CPB.
In recent years, animal experiments and clinical studies have suggested that eco-therapy can increase intestinal mucosal barrier immunity [6]. Probiotics are eco-agents, which have been associated with protective effects on intestinal barrier function [7, 8]. One of the most notable strains is Bifidobacterium, which contributes to the maintenance of the microenvironmental stability of the tract and the protection of intestinal barrier [9, 10]. Bifidobacteria dominate in the physiological human intestinal flora and work together with other anaerobic bacteria to build a biological barrier via intestinal epithelial cell-specific binding [11]. They produce large amounts of lactic, acetic, and other organic acids by glucose fermentation and thereby lower the intestinal pH, which inhibits the growth of diverse pathogenic bacteria such as Bacillus dysenteriae, Bacillus typhi, Bacillus proteus, Pseudomonas aeruginosa, and fungi. The pH drop also prevents potential adhesion of the above pathogens and their toxins to intestinal epithelial cells [12]. Moreover, the Bifidobacteria antigen stimulates immunoactive cells, including natural killer cells and macrophages, to mount immune responses and improve intestinal barrier function. The latter prevents colonization and invasion of pathogens and opportunistic pathogens to enhance resistance to microbial infection, thereby reducing the production of intestinal endotoxemia and endotoxin levels in the blood [13]. Based on these results, we hypothesized that probiotics in the intestinal barrier may offer protective effects in the context of CPB.
We previously reported that the main mechanism of intestinal barrier dysfunction following CPB is related to a decrease of tight junction protein expression in the intestinal epithelium, which subsequently leads to changes in structure and function of the intestinal mucosa, increased intestinal permeability, bacterial translocation, and endotoxemia [14]. This study was designed to examine the multiple effects of probiotics on intestinal permeability, bacterial translocation, sIgA levels in plasma and intestinal tissue, and the expression profile of intestinal epithelial tight junction proteins after CPB in rats. Further aims were to investigate the potential protective mechanisms of probiotics on intestinal barrier damage caused by CPB, provide new ideas for protection of the intestinal mucosal barrier after CPB, and present experimental support for clinical applications.
Materials and Methods
Experimental Groupings
Twenty-four clean grade healthy male Sprague–Dawley rats, weighing 350–450 g, were provided by the clinical research center of Shenyang Military Region General Hospital. The rats were randomly divided into three groups (n = 8): the sham operation group without CPB or probiotic feeding (group S), the group without probiotic feeding before CPB operation (group CPB), and the group fed with probiotics before CPB operation (group Y). Group S rats were intubated but not subjected to CPB. In group Y, rats were fed with 2 ml (1.0 × 107 CFU) of probiotic cocktail (a triple viable preparation including Bifidobacterium, Lactobacillus, and Streptococcus thermophilus) each morning for 7 days before CPB. Rats in groups S and CPB were fed with 2 ml of normal saline instead.
Surgical Manipulations
Rats were subjected to water deprivation and fasting 6 h before CPB. Subsequently, the animals were anesthetized by intraperitoneal injection with 10 % chloral hydrate (350 mg/kg) and subjected to endotracheal intubation and mechanical ventilation with a TKR-200 C ventilator (Teli Anesthesia Breathing Equipment Company, China). The respiratory rate was 60/min, the pressure was 2.5–3.0 cm H2O, and the inhaled oxygen concentration was 100 %. Electrocardiogram was assessed by a multi-function monitor (Space Company, USA), and body temperature was measured by a rectal temperature probe. A 22G trocar was placed into the left femoral vein and linked to a micro-infusion pump to inject heparin sodium (300 IU/kg), while a 24G trocar was placed into the left femoral artery and linked to monitors through a pressure transducer device for continuous monitoring of arterial pressure. In addition, a 24G trocar was placed into the right common carotid artery and connected with an arterial pump tube for the input of CPB arterial blood. Furthermore, a specially-crafted 16G puncture catheter with reticular lateral eyes was placed into the right jugular vein at the right atrium level, for drainage of venous blood to the blood storage tank.
The CPB circuit was composed of a blood storage tank, a BT00-300M constant flow peristaltic pump (Baoding Lange Constant Flow Pump Co., Ltd.), a micro-membrane oxygenator (Guangdong Kuwait Medical Devices Co., Ltd.), and a connecting pipeline. The CPB circuit was primed with 16 ml of priming buffer composed of lactated Ringer solution (7 ml), succinylated gelatin (7 ml), 15 % mannitol (1 ml), and 5 % sodium bicarbonate (1 ml).
At the start of bypass surgery, the perfusion flow rate was approximately 35 ml kg−1 min−1, and it was gradually increased to 90–100 ml kg−1 min−1. After the start of CPB, the oxygen supply was transferred from mechanical ventilation to the oxygenator (FiO2 = 100 %), and the oxygen flow to perfusion flow ratio remained at 0.8–1.0. In addition, the arterial pressure was maintained at 60–80 mmHg (1 kPa = 7.5 mmHg) during the procedure. During CPB, the appropriate amount of crystal glue was added to the blood reservoir at a 1:1 ratio to the blood, while maintaining the storage amount at 2–3 ml. Incandescent lighting (100 W) was used for heating the top of the blood reservoir and the lung membrane in order to maintain a rectal temperature between 36.5 and 37.5 °C. Management of acid–base balance was in α-homeostasis mode. Femoral artery blood (0.3 ml) was extracted before CPB, 15 and 30 min after the start of CPB, and at the stop of CPB, and it was analyzed by a GEM Premier 2,300 blood-gas analyzer to maintain the arterial blood pH between 7.35 and 7.45 and the PaCO2 between 35 and 45 mmHg. Mechanical ventilation was restored 60 min after CPB; the perfusion flow was gradually reduced and then shut down, followed by removal of the pipe. The remaining blood in the blood storage tank was slowly infused back into the rat to maintain stable circulation. The ventilator was stopped when autonomic breathing became active. The appropriate amounts of dopamine, blood supplementation, and rehydration were executed according to the physical status. Rats were returned to the observation box when they fully recovered, keeping the proper temperature, water, and oxygen supply. Subsequently, rats were decapitated 2 h after CPB.
Biochemical Analysis of Blood
Portal vein blood (1 ml) and vena cava blood (2 ml) were extracted aseptically, and the plasma samples were isolated and stored at −40 °C. Diamine oxidase (DAO) activity and D-lactate concentration in the vena cava plasma (1 ml) were examined by a spectrophotometric assay [15]. DAO standard (batch number D7876-250), o-dianisidine (batch number D9143-5), and D-lactate standard (lot number L0625-25) were purchased from Sigma. Endotoxin concentration in the portal vein plasma was determined by a limulus lysate test kit (Yihua Clinical Technology, Inc., China). TNF-alpha and IL-6 concentrations in the vena cava plasma (1 ml) were measured by using a radioimmunoassay kit (Tianjin JIUDING Medical and Biological Engineering Co., Ltd., China), according to the manufacturer’s instructions.
Determination of IgA Concentration in Plasma and Intestinal Mucus
An approximately 10-cm section in the middle of the jejunoileum was clipped, and the contents were gently removed after the longitudinal incision. Intestinal mucus was collected into an Eppendorf tube by scraping, mixed with 0.01 M phosphate-buffered saline (PBS), and centrifuged at 3,000 rpm. At the same time, 1 ml of vena cava blood was extracted and centrifuged for 10 min to get the supernatant. IgA content was measured by a double-antibody sandwich radioimmunoassay kit (The Bonding Company, China) according to the manufacturer’s protocol, and total proteins were determined by the standard biuret method. Values were used to calculate the relative IgA content per mg of protein in the plasma and the intestinal mucus.
Bacterial Translocation Analysis
A sample of vena cava blood (100 μl) was extracted under sterile conditions and inoculated on blood agar medium. Liver, lung, or kidney tissue samples, or mesenteric lymph nodes (MLN), 0.1–0.2 g each, were ground in a sterile grinding tube with 1 ml of saline into a suspension. A 20-μl aliquot of the suspension was inoculated for blood agar culture, and bacterial growth and bacterial species were checked 24 h after incubation.
Assessment of Intestinal Morphology
A 1-cm section of ileum was taken and cut into 1 mm × 1 mm blocks, which were fixed in 2.5 % glutaraldehyde. After rinsing with PBS, the specimens were fixed with 1 % (V/V) osmium tetroxide in 0.1 M PBS for 2 h at 4 °C. The specimens were progressively dehydrated by ethanol and acetone, saturated with epoxy resin 618, and cut into ultrathin sections after embedding. Morphological changes of intestinal mucosa in the sections were detected by electron microscopy after double staining with lead citrate and uranyl acetate for 10 min.
Detection of Occludin and Zona Occluden-1 (ZO-1) by Western Blotting and Immunohistochemistry (IHC)
Western blotting
After rats were euthanized as described above, terminal ilea were isolated, excised, flushed with ice-cold PBS to remove the fecal debris, and then opened longitudinally. Intestinal mucosa samples were harvested with a razor blade. Tissues were homogenized by mechanical disruption in lysis buffer (50 mM Tris–HCl, pH 7.5, 150 mM NaCl, 0.1 % dodecyl sodium sulfate, 1 % Nonidet P-40, 0.5 % sodium deoxycholate, 100 mg/ml phenylmethylsulfonyl fluoride, and 1 mg/ml aprotinin) and incubated on ice for 30 min. Homogenate was then pelleted at 6,000×g for 10 min, and the supernatant was collected. The quantity of total protein was determined in the supernatant by using the Lowry method. The protein extracts were incubated with primary antisera (rabbit anti-occludin and anti-ZO-1, 1:500; Zymed Laboratories, San Francisco, CA) at 4 °C overnight, and then the mixture was incubated with secondary antibody (horseradish peroxidase-conjugated goat anti-rabbit IgG, 1:1000; Beijing Zhongshan Biotech, Co.) at 4 °C for 6–8 h. Immunoprecipitates were subjected to SDS-PAGE and electrotransferred onto a nitrocellulose membrane. After a final wash in TBST (50 mM Tris–HCl, pH 7.5, 150 mM NaCl, 0.1 %Tween 20), the membrane was processed with the enhanced chemiluminescence kit (Shanghai Pufei Biotech, Co.), according to the manufacturer’s recommendations. Immunoreactive bands were visualized by autoradiography and quantified by using the Gel Imaging Analysis System (ChemiImager 5500, Alpha Innotech, USA). Results were expressed as relative intensity of target protein to the internal standard (tubulin).
Immunohistochemistry
Rat ileum tissue sections from rats of different groups were subjected to hematoxylin and eosin staining, or immunohistochemical staining with occludin and ZO-1 antibodies by using the PV-6001/6002 Two-Step Histostaining kits (Immnovision, USA). The immunohistochemical data were quantified to assess occludin and ZO-1 expression. Five slides with clear staining were randomly selected from each group, ten vision fields were randomly selected from these slides, and the average optical densities of a fixed window area under a light microscope were measured and analyzed for their protein content. The analysis was conducted with Meta Moth software from Universal Imaging Corporation Image Analysis Systems (USA).
The BCA Protein Assay Kit was purchased from Pierce (USA), and rabbit anti-rat occludin and ZO-1 polyclonal antibodies were purchased from Zymed (USA). Poly-l-lysine and two-step immunohistochemical detection reagents (PV-6001/6002 US DAB substrate reagents) were purchased from Beijing Zhongshan Golden Bridge Biotechnology (China).
Statistical Methods
All numerical data were analyzed by using SPSS13.0 software and were represented as mean ± standard deviation (x ± s). ANOVA analysis and the χ 2 test were adopted for the data within a group. P < 0.05 was considered as statistically significant.
Results
Probiotics Can Alleviate Intestinal Epithelial Damage Caused by CBP
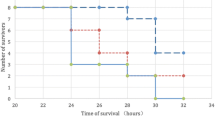
After CBP, DAO activity and levels of D-lactate, TNF-alpha, IL-6, and LPS were increased (P < 0.05) in plasma from rats in groups CPB and Y, as compared to the control group S. However, all values were significantly lower in group Y compared to group CPB (Fig. 1). Moreover, morphological analysis of the intestinal epithelium by transmission electron microscopy (TEM) showed that the intestinal epithelial ultrastructure was maintained better in group Y compared to group CBP rats (Fig. 2). Consistently, IgA concentrations in the plasma and small intestine were significantly increased in group Y, compared to group CPB (P < 0.05), but they remained lower than those of group S (P < 0.05, Fig. 3). The above results suggest that CBP promoted intestinal damage and inflammation, while probiotics alleviated these effects and partially restored intestinal immunity.
Ultrastructure changes of intestinal epithelial samples from each of the three groups (×7200). In group S, rat intestinal epithelial cell microvilli were arranged in neat rows, with normal cell connection structure, normal organelles, regular nuclear shape, and evenly distributed chromatin. However, in group CPB, there was degeneration, necrosis, and demyelination in intestinal epithelial microvilli, nuclear condensation, vacuolation in the mitochondria and endoplasmic reticulum, and unclear cellular tight junctions. In group Y, intestinal epithelial villi showed slight dropout; there was also vacuolation in the mitochondria and endoplasmic reticulum, but cell tight junctions were more obvious compared to those in group CPB
Intestinal bacterial translocation rate, another important index of intestinal epithelial damage, was also examined and compared among the three experimental groups. Four types and a total of 47 strains of bacteria, which are physiological constituents of the permanent intestinal flora, including Escherichia coli, Enterococcus, Corynebacterium, and Proteus, were detected in the blood, MLN, liver, kidney, and lung tissues from all groups. The bacterial translocation rates were calculated to be 7.5 % (group S), 75.0 % (group CBP), and 35.0 % (group Y), respectively (Table 1). Thus, compared with group S, the bacterial translocation rates of groups CPB and Y increased 10- and 4.7-fold, respectively (P < 0.05). Importantly, the bacterial translocation rate of group Y was 2.1-fold lower (P < 0.05) compared to group CPB.
Probiotics Prevented the Decline of Tight Junction Protein Expression Caused by CBP
Tight junction protein expression is very important for normal intestinal ultrastructure. As shown in Figs. 4 and 5, in the control group S, the rat intestinal epithelial tight junction proteins occludin and ZO-1 were uniformly distributed on the edges of intestinal epithelial cells with honeycomb or linear-shapes. After CBP, the expression of tight junction proteins was dramatically reduced. As a result, occludin and ZO-1 staining was unevenly distributed or faded. However, the decline of tight junction protein expression caused by CBP was significantly reduced in group Y rats that received probiotics (Figs. 4 and 5). The average IHC optical density values of occludin and ZO-1 decreased significantly (P < 0.05) in groups CPB and Y, as compared to group S. Nevertheless, the values in group Y were significantly higher compared to CBP (P < 0.05), as shown in Table 2.
These findings were validated by western blot analysis. As shown in Fig. 6, the levels of occludin and ZO-1 were significantly lower in groups CPB and Y compared to group S (Fig. 6, P < 0.05). However, the expression of occludin and ZO-1 in group Y was significantly higher than that in the CBP group (Fig. 6, P < 0.05).
Discussion
Over the past 20 years, probiotics have been widely used to treat various types of diarrhea, prevent and treat inflammatory bowel disease, alleviate constipation, relieve irritable bowel syndrome, reduce allergy symptoms, and lower plasma cholesterol and triglyceride concentrations [16, 17]. Most studies adopted probiotic supplements to protect the intestinal mucosa after traumatic stress [18–20]. However, under these conditions, the body stress response has already initiated intestinal mucosal barrier function damage, leading to intestinal villus atrophy and decreased mucosal regeneration ability. Moreover, body stress also reduces the secretion of gastric acid, bile, lysozyme, and the chemical sterilization capacity of intestinal fluid, resulting in growth of intestinal pathogenic bacteria [21]. For these reasons, we opted to add a sufficient amount of probiotics to preblock or reduce inflammation and intestinal dysfunction before the stress response. Based on this idea, probiotic intervention was initiated 7 days before CPB (open heart surgery with CPB is usually performed 7 days after patients are hospitalized). The probiotic preparation used in this study contained mostly Bifidobacterium as well as Lactobacillus and Streptococcus, and the selected dose was 1.0 × 107 CFU/d, which has been shown to be optimal for reducing inflammatory reactions and bacterial translocation [22]. Our previous study found that DAO activity and D-lactate levels in rat plasma reach a maximum 2 h after termination of CPB [14]. Therefore, all specimens in this study were prepared at this time point for each experimental group.
Previous studies have shown that DAO activity in peripheral blood reflects the maturity and the integrity of mucosal epithelial cells [23]. D-lactate levels in the blood not only can reflect the status of intestinal mucosal damage [24], but they also correspond to changes in intestinal mucosa permeability. The results of this study showed that necrosis and shedding of intestinal mucosa and villous edema were significantly reduced after CPB in rats pretreated with probiotics (group Y). Consistently, a substantial improvement in intestinal mucosal barrier function was found in group Y compared to group CPB, mirrored by significant decreases in plasma D-lactate concentration and DAO activity, plasma LPS concentration, and distant organ bacterial translocation rates. We speculate that probiotics exert protective effects by inhibiting the inflammatory response, enhancing local immune function, regulating the connection between intestinal epithelial cells, and improving the physical barrier function of the intestinal epithelium.
Adawi et al. [25]. used Lactobacillus to pretreat rats with acute liver injury by gavage for 8 days, and this treatment resulted in a significant reduction of the bacterial translocation rate and liver cell damage. Schrveder provided the first evidence that prophylactic probiotics can effectively inhibit the production of endotoxin by pig intestinal pathogens [26]. In addition, other studies showed that the application of an ecological immune nutrition agent for SIRS rats can apparently prevent intestinal mucosal barrier dysfunction in the state of endotoxin shock and can effectively reduce endotoxin levels in the portal vein and the intestinal bacterial translocation rate [27]. In this study, plasma TNF-alpha, IL-6, and LPS concentrations and the distant organ bacterial translocation rate were reduced after CPB in rats pretreated with probiotics; nevertheless, values did not reach the normal levels found in the control group. These results indicate that probiotics play a protective role in mitigating the inflammatory response and endotoxemia, which can effectively improve intestinal barrier function after CPB, and reduce intestinal permeability and bacterial translocation.
Local intestinal immune function plays an important protective role in the context of invasive bacterial translocation [28]. The intestinal mucosal surface layer has a critical physiological barrier function in which glycoprotein and sIgA cooperate with each other and sIgA-surrounded bacteria adhere firmly to the mucus layer. Thus, harmful bacteria will be removed from the body with flow of the mucus layer enveloping [29]. Impaired post-traumatic immune function will lead to reduced secretion of sIgA. Therefore, pathogenic bacteria will easily adhere for colonization and induce bacterial translocation, even causing systemic disseminated infection [30]. Our results show that sIgA levels in rat plasma and the small intestine of group CPB rats were significantly reduced, while no significant changes were found in group S rats. These findings indicate a diminished local humoral immune function of the intestinal mucus in the early stage after CPB. A significant increase of sIgA levels in plasma and the small intestine of group Y rats was found compared to group CPB, suggesting that probiotic pretreatment can improve the local intestinal immune function. This may be due to the immunomodulatory effects of probiotics or their metabolites, which directly stimulate the secretion of plasma cell sIgA. Accordingly, we suggest that maintaining sIgA at high levels could reduce the occurrence of intestinal-sourced infections after treatment with probiotics in the intestinal mucosa.
The structural basis of the mechanical barrier comes from the intestinal mucosal tight junctions between intestinal epithelial cells and the adjacent intestinal epithelial cells. Various proteins are involved in tight junction formation, including occludin, claudin, ZOs, and connection or adhesion molecules [31, 32]. Restaenert found that probiotics protect intestinal mucosal tight junction proteins from invasive E. coli and reduce intestinal permeability. Additionally, probiotics have also been shown to protect epidermal growth factor receptor and facilitate the repair of damaged intestinal mucosa [33]. Qing et al. found that supplementary probiotics can increase intestinal epithelial occludin protein expression in rats with acute pancreatitis, which maintains intestinal epithelial tight junctions, corrects the disorder of the intestinal flora, and reduces bacterial translocation, thereby protecting the intestinal mucosal barrier [34]. We report herein that in samples of group S rats, the tight junction proteins occludin and ZO-1 showed a uniform distribution on the edge of the top of intestinal epithelial cells with honeycomb or linear-shapes. The uneven distribution and fading of occludin and ZO-1 staining in samples of the CPB group were significantly corrected in the Y group. Moreover, the optical density values were higher in the Y group than in the CPB group.
Cardiopulmonary bypass is a nonphysiological stress stimulus, which causes increased secretion of adrenal corticosteroids, growth hormone, pancreatic glucagon, and catecholamine. These responses lead to insulin resistance and elevated blood sugar levels. CPB also causes a rise in lactate levels, which indirectly reflect the imbalance between tissue oxygen supply and utilization [35]. Whether these changes can aggravate the intestinal mucosal barrier dysfunction and interfere with the protective effects of probiotics remains to be clarified. Along these lines, a possible association between probiotic pretreatment with bacterial infection and the development of resistance should also be noted [36, 37]. Further work is required to elucidate the mechanism of action of probiotics, but also to assess their safety, in order to develop standard guidelines for their application.
In summary, pretreatment of rats with probiotic preparations cannot offer complete protection to the gut against CPB stress injury, but it can effectively reduce intestinal permeability and the bacterial translocation rate. The apparent improvement of intestinal barrier function caused by probiotic pretreatment may be related to inhibition of the inflammatory response triggered by CPB, improvement of the local intestinal immune function, and increased expression of intestinal epithelial tight junction proteins. Our data suggest that pretreatment with probiotic preparations, combined with the necessary anti-inflammatory postoperative treatment, has the potential to reduce the incidence of complications following CPB and improve organ function and prognosis of patients.
References
Riddington DW, Venkatesh B, Boivin CM, et al. Intestinal permeability, gastric intramucosal pH, and systemic endotoxemia in patients undergoing cardiopulmonary bypass. JAMA. 1996;275:1007–1012.
Hamilton-Davies C, Barclay GR, Cardigan RA, et al. Relationship between preoperative endotoxin immune status, gut perfusion, and outcome from cardiac valve replacement surgery. Chest. 1997;112:1189–1196.
Mojcik CF, Levy JH. Aprotinin and the systemic inflammatory response after cardiopulmonary bypass. Ann Thorac Surg. 2001;2:745–754.
Thoren A, Nygren A, Houltz E, et al. Cardiopulmonary bypass in humans jejunal perfusion increases in parallel with well-maintained microvascular hematocrit. Acta Anaesthesiol Scand. 2005;49:502–509.
Sack FU, Reidenbach B, Schledt A, et al. Dopexamine attenuates microvascular perfusion injury of the small bowel in pigs induced by extracoporeal circulation. Anaesthesia. 2002;88:841–847.
Salvatore S, Hauser B, Vandenplas Y. Chronic enteropathy and feeding. Nestle Nutr Workshop Ser Pediatr Program. 2007;59:115–126.
Wang B, Huang Q, Zhang W, et al. Lactobacillus plantarum prevents bacterial translocation in rats following ischemia and reperfusion injury. Dig Dis Sci. 2011;56:3187–3194.
Patel RM, Lin PW. Developmental biology of gut-probiotic interaction. Gut Microbes. 2010;1:186–195.
Lievin V, Peiferl, Hudault S, et al. Bifidobacterium strains from resident infant human gastrointestinal microflora exert antimicrobial activity. Gut. 2000;47:646–652.
Asahara T, Shimizu K, Nomoto K, et al. Probiotic bifidobacteria protect mice from lethal infection with Shiga toxin producing Escherichia coli l57:H7. Infect Immun. 2004;72:2240–2247.
Collado MC, Gueimonde M, Hernández M, et al. Adhesion of selected Bifidobacterium strains to human intestinal mucus and the role of adhesion in enteropathogen exclusion. J Food Prot. 2005;68:2672–2678.
Mochizuki H, Trocki O, Dominioni L, et al. Mechanism of prevention of postburn hypermetabolism and catabolism by early enteral feeding. Ann Surg. 1984;200:297–310.
Haller D, Antoine JM, Bengmark S, et al. Guidance for substantiating the evidence for beneficial effects of probiotics: probiotics in chronic inflammatory bowel disease and the functional disorder irritable bowel syndrome. J Nutr. 2010;140:690–697.
Sun YJ, Chen WM, Zhang TZ, et al. Effects of cardiopulmonary bypass on tight junction protein expressions in intestinal mucosa of rats. World J Gastroenterol. 2008;14:5869.
Fürst W, Schiesser A. Test for stereospecifity of an automated D-lactate assay based on selective removal of Ll-lactate. Anal Biochem. 1999;269:214–215.
Gareau MG, Sherman PM, Walker WA. Probiotics and the gut microbiota in intestinal health and disease. Nat Rev Gastroenterol Hepatol. 2010;7:503–514.
Sanz Y, Nadal I, Sánchez E. Probiotics as drugs against human gastrointestinal infections. Recent Pat Antiinfect Drug Discov. 2007;2:148–156.
Ait-Belgnaoui A, Durand H, Cartier C, et al. Prevention of gut leakiness by a probiotic treatment leads to attenuated HPA response to an acute psychological stress in rats. Psychoneuroendocrinology. 2012;37:1885–1895.
Deng W, Dong XF, Tong JM, et al. The probiotic Bacillus licheniformis ameliorates heat stress-induced impairment of egg production, gut morphology, and intestinal mucosal immunity in laying hens. Poult Sci. 2012;91:575–582.
Lutgendorff F, Akkermans LM, Söderholm JD. The role of microbiota and probiotics in stress-induced gastro-intestinal damage. Curr Mol Med. 2008;8:282–298.
Bhatia V, Tandon RK. Stress and the gastrointestinal tract. J Gastroenterol Hepatol. 2005;20:332–339.
Mogilner JG, Srugo I, Lurie M, et al. Effect of probiotics on intestinal regrowth and bacterial translocation after massive small bowel resection in a rat. J Pediatr Surg. 2007;42:1365–1371.
Tsunooka N, Maeyama K, Nakagawa H, et al. Localization and changes of diamine oxidase during cardiopulmonary bypass in rabbits. J Surg Res. 2006;131:58.
Johnson SD, Smye M, Watson RP. Intestinal permeability tests in celiac disease. Clin Lab. 2001;47:143.
Adawi D, Ahrne S, Molin G. Effects of different probiotic strains of Lactobacillus and bifido-bacterium on bacterial translocation and liver injury in an acute liver injury model. Int J Food Microbiol. 2001;70:213–220.
Schroeder B, Duncker S, Barth S. Preventive effects of the probiotic Escherihia on acute secretory diarrhea in a pig model of intestinal infection. Dig Dis Sci. 2006;51:724–731.
Cole CR, Frem JC, Schmotzer B, et al. The rate of bloodstream infection is high in infants with short bowel syndrome: relationship with small bowel bacterial overgrowth, enteral feeding and inflammatory and immune responses. J Pediatr. 2010;156:941–947.
Woodcock NP, Robertson J, Morgan DR, et al. Bacterial translocation and immunohistochemical measurement of gut immune function. J Clin Pathol. 2001;54:619–623.
Mantis NJ, Forbes SJ. Secretory IgA: arresting microbial pathogens at epithelial borders. Immunol Invest. 2010;39:383–406.
Ljungdahl M, Lundholm M, Katouli M, et al. Bacterial translocation in experimental shoch is dependent in the intestinal flora. Scand J Gastroenterol. 2000;35:3892–3971.
Braniste V, Jouault A, Gaultier E, et al. Impact of oral bisphenol A at reference doses on intestinal barrier function and sex differences after perinatal exposure in rats. Proc Natl Acad Sci USA. 2010;107:448–453.
Ebnet K, Aurrand-ions M, Kuhn A, et al. The junctional adhesion molecule (JAM) family members JAM-2 and JAM23 associate with the cell polarity protein PAR-3: a possible role for JAM sin endothelial cell polarity. J Cell Sci. 2003;116:3879–3891.
Resta-Lenert S, Barrett KE. Live probiotics protect intestinal epithelia cells from the effects of infection with enteroinvasive Escherichia col (EIEC). Gut. 2003;52:988–9971.
Dai C, Guandalini S, Zhao DH, Jiang M. Antinociceptive effect of VSL#3 on visceral hypersensitivity in a rat model of irritable bowel syndrome: a possible action through nitric oxide pathway and enhance barrier function. Mol Cell Biochem. 2012;362:43–53.
Daxin Cheng, Qixiang Shen, Limin Chen, et al. Effects prolonged extracorporeal circulation on metabolism. Chin J ECC. 2005;3:44–46.
Land MH, Rouster-Stevens K, Woods CR, et al. Lactobacillus sepsis associated with probiotic therapy. Pediatrics. 2005;1l5(1):178–181.
D’Aimmo MR, Modesto M, Biavati B. Antibiotic resistance of lactic acid bacteria and Bifidobacterium spp. isolated from dairy and pharmaceutical products. Int J Food Microbiol. 2007;115(1):35–42.
Acknowledgments
This work was supported by a grant from the Doctor Priming Foundation of Liaoning Province (20091099).
Conflict interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, YJ., Cao, HJ., Song, DD. et al. Probiotics Can Alleviate Cardiopulmonary Bypass-Induced Intestinal Mucosa Damage in Rats. Dig Dis Sci 58, 1528–1536 (2013). https://doi.org/10.1007/s10620-012-2546-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2546-0