Abstract
Introduction
Voluntary muscle activity, including swallowing, decreases during the night. The association between nocturnal awakenings and swallowing activity is under-researched with limited information on the frequency of swallows during awake and asleep periods.
Aim
The aim of this study was to assess nocturnal swallowing activity and identify a cut-off predicting awake and asleep periods.
Methods
Patients undergoing impedance-pH monitoring as part of GERD work-up were asked to wear a wrist activity detecting device (Actigraph®) at night. Swallowing activity was quantified by analysing impedance changes in the proximal esophagus. Awake and asleep periods were determined using a validated scoring system (Sadeh algorithm). Receiver operating characteristics (ROC) analyses were performed to determine sensitivity, specificity and accuracy of swallowing frequency to identify awake and asleep periods.
Results
Data from 76 patients (28 male, 48 female; mean age 56 ± 15 years) were included in the analysis. The ROC analysis found that 0.33 sw/min (i.e. one swallow every 3 min) had the optimal sensitivity (78 %) and specificity (76 %) to differentiate awake from asleep periods. A swallowing frequency of 0.25 sw/min (i.e. one swallow every 4 min) was 93 % sensitive and 57 % specific to identify awake periods. A swallowing frequency of 1 sw/min was 20 % sensitive but 96 % specific in identifying awake periods.
Summary and Conclusion
Impedance-pH monitoring detects differences in swallowing activity during awake and asleep periods. Swallowing frequency noticed during ambulatory impedance-pH monitoring can predict the state of consciousness during nocturnal periods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
We routinely monitor patients in the ambulatory setting with 24-h multichannel-impedance-pH measurements for assessment of GERD. A by-product of these assessments are swallows, which are well visible on impedance studies. We long ago noted the difference in swallowing activity during recumbent and upright position, but also periods of quiescence during the day, which we attributed to sleeping time, with intermittent bursts of activity, which we hypothesized to be arousal periods.
This notion is supported by the fact that physiologic swallowing activity differs between night and day [1]. Arousal periods, a marker of sleep fragmentation, are a matter of concern, especially in our GERD population. Sleep deprivation is also a highly prevalent problem and is associated with increased use of health care services and products, as well as functional impairment [2–4]. GERD may adversely affect sleep by awakening patients from sleep during the night, leading to sleep fragmentation and deprivation. Patients with GERD and night-time related symptoms have been shown to have a lower quality of life than patients without night-time related symptoms [3]. Based on a nationwide telephone survey of 1,000 adults experiencing heartburn at least once a week, Shaker et al. [4] reported that almost 80 % of heartburn sufferers experience heartburn at night and virtually all of them reported that the symptom affected their sleep. Finding a simple diagnostic tool without involvement of additional costly, invasive or technically challenging resources in patients that are being referred for GERD testing anyhow would be welcomed to better characterize and evaluate this complex patient population. We were therefore intrigued to possibly judge a patient’s state of consciousness based on swallowing activity.
Small studies using pharyngeal pressure sensors have indicated that swallows at night are associated with movement arousals. These arousals can be recorded using actigraphy, a validated tool used clinically and in research to monitor sleep efficiency. For the outpatient ambulatory setting wristband actigraphs are available, that allow monitoring of sleep efficiency and night-time arousals whilst patients rest in the comfort of their own home.
The aim of our study was therefore to compare overnight ambulatory combined multichannel intraluminal impedance-pH (MII-pH) detected swallow activity with nocturnal awakenings as detected by actigraphy technology in patients with GERD. We hypothesized that swallowing activity is higher during arousal periods at night and may be a reliable indicator for monitoring consciousness in patients with GERD. In addition, the determination of arousal periods based on MII-pH detected increased swallowing activity could be a useful indicator of sleep fragmentation in patients with GERD.
Methods
Patients
Patients referred for evaluation of suspected gastroesophageal reflux disease with ambulatory overnight combined multichannel intraluminal impedance-pH (MII-pH) monitoring to the Esophageal and Motility Clinic at the Medical University of South Carolina were included in this study. Patients presented with typical reflux symptoms such as heartburn, regurgitation and chest pain and atypical symptoms such as throat clearing and cough. Patients taking medications affecting gastrointestinal motility, sleep affecting drugs (narcotics, sedatives) and with documented major motility abnormalities were excluded. All patients gave written informed consent. The Institutional Review Board (IRB) for Human Research of the Medical University of South Carolina approved this study.
Study Protocol
Impedance and pH Monitoring
Patients eligible for the study underwent stationary combined impedance manometry (MII-EM, Sandhill Scientific Inc., Highlands Ranch, CO) for location of the upper border of the lower esophageal sphincter. For ambulatory MII-pH testing a 2.1-mm catheter (Sandhill Scientific Inc.; Highlands Ranch, CO, USA) with six 2-cm impedance recording segments and two antimony pH-electrodes was used. Impedance-measuring segments were located at 3, 5, 7, 9, 15 and 17 cm above the proximal border of the LES. The esophageal pH electrode was placed 5 cm above the proximal border of the LES with a gastric pH electrode 15 cm distally. All signals were stored in a digital data logger.
During monitoring, subjects were encouraged to maintain normal activities and sleep schedule and eat their usual meals at usual times. They kept a diary in which periods of ingestion and periods spent in the recumbent position were noted in addition to symptoms and medication.
During the period of the MII-pH testing, patients enrolled were also asked to wear a watch-like device on one wrist for actigraphy monitoring (ActiSleep Monitor, ActiGraph Inc., Pensacola, FL). The primary endpoint of this study was the determination of frequency of swallows detected by MII-pH during awake and asleep periods in recumbent position determined by actigraphy.
Actigraphy
The actigraph is a small, wrist-worn device that contains an accelerometer to monitor the number of wrist movements per epoch (60 s). Motion is converted to an electric signal and digitally integrated to derive an activity count. The widely used and validated Sadeh algorithm was used to identify sleep or wake states based on activity counts and to determine sleep parameters such as sleep onset latency, total sleep time, number and duration of awakenings [5, 6]. Time calibration between the actigraph device and MII-pH data logger was performed prior to every study to ensure accuracy of concordance between motion signals and swallowing activity in this simultaneous analysis of sleep and esophageal impedance for detection of arousal periods and swallows. The stored digital information was downloaded and analyzed to determine the nocturnal arousal and sleeping periods and their duration.
Data Analysis
The analysis of the impedance recordings and sleep reports was performed after upload of data to a personal computer with dedicated software. Swallow activity detected by MII-pH has been shown by Hila et al. [7] to have a strong association with manometric assessment of esophageal function. Swallows were evaluated in a 5-min window and marked by hand by an expert reader. Swallows were identified as rapid drops in impedance in at least two proximal impedance channels (17 and 15 cm above LES) and progressing over time in aboral direction. The reader was blinded to state of consciousness as the actigraph data were assessed separately. A software tool designed to extract impedance data from the impedance-pH files allowed simple and reliable assessment of time point of swallow and body position. Sleep and awake times of individual subjects were tabulated using a second macro (Microsoft Excel, Microsoft Inc, Irvine, CA) using the Sadeh algorithm with specifications of ActiGraph Inc., Pensacola. Impedance identified number of swallows (SW) per body position for all subjects were determined and correlated with number of awakenings (AW) per matching time frame.
Times are displayed as mean ± standard deviation (SD) unless specified otherwise. An ROC analysis (SPSS 12.0, IBM, Chicago, IL, USA) was used to calculate cut-off values for sensitivity and specificity in regards to identification of awake and asleep periods. Level of significance was set at p < 0.05 for all tests.
Results
Patient Demographics
Eighty-seven patients were enrolled in the study. Two has insufficient 24 h-MII-pH data, and nine were missing data from the actigraph (actigraph not activated, taken off during study, corrupt data file). Complete data sets (i.e. 24-h impedance-pH monitoring and actigraph recordings) from 76 patients (28 males, 48 females; mean age 56.3 ± 14.8 years) were available for analysis. Sixty-four (84 %) were investigated on acid suppressive therapy (PPI) while 12 (16 %) patients were studied off medication.
Swallow Frequency Characteristics
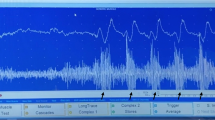
The average ± SD time spent in a recumbent position was 449 ± 95 min. While in the recumbent position patients were awake on average 109 ± 83 min corresponding to 24.2 ± 16.3 % of total recumbent time. In recumbent position patients swallowed on average 67.3 ± 60.5 times while awake and 91.2 ± 67.3 times while asleep. The swallowing frequency while awake (0.7 ± 0.1 swallows/min) was significantly higher (p < 0.001) compared to the swallowing frequency while asleep (0.3 ± 0.0 swallows/min (Fig. 1). Individual data are shown in Fig. 2.
ROC Analysis
The ROC analysis showed that swallowing frequency performed very well in identifying awake and asleep periods. The area under the ROC curve was 0.865 ± 0.030 (p < 0.001) (Fig. 3). According to the ROC analysis the cut-off value of 0.33 sw/min (i.e. one swallow every 3 min) had the optimal sensitivity (78 %) and specificity (76 %) to differentiate awake from asleep periods. A swallowing frequency of 0.25 sw/min was 93 % sensitive and 57 % specific to identify awake periods. In other words, if a patients swallows fewer than once every 4 min she/he was most likely asleep. A swallowing frequency of 1 sw/min was 20 % sensitive but 96 % specific in identifying awake periods. In other words, if a patient swallowed more than once a minute she/he was most likely awake.
Discussion
We evaluated swallow activity in association with sleeping and awake periods in patients having ambulatory overnight MII-pH testing for evaluation of possible GERD symptoms. We found that swallowing activity indeed can be used to monitor state of consciousness. During sleep we monitored an average swallowing activity of 0.3 per minute, or 18 per hour compared to 0.7 per minute, or 48 per hour during awake periods. When seeking high sensitivity to determine sleep, a cut-off of <0.25 swallows per minute showed greater than 90 % sensitivity to detect sleep. A cut-off of 1 swallow per minute identified sleep with 96 % specificity. The analysis therefore allows for individual cut-offs to differentiate sleep from awake periods.
Deglutition is a vital function that occurs both voluntarily and involuntarily. Its functions include transport of nutrients from the oral cavity into the stomach, clearance of intra-esophageal content, protection from aspiration and moistening of the pharyngeal and esophageal mucosa with saliva. The amount of saliva produced is greatest during the awake hours of the day and diminishes greatly during sleep [8]. Few studies have assessed sleep related deglutition; the ones available discuss findings from the otolaryngology (ENT) community. When Lichter and Muir first described sleep related deglutition in 1975, they noted that swallowing during sleep was associated with movement artefacts most of the time. Their data are in agreement with our findings although measured with different techniques; Lichter and Muir assessed swallowing by activity of the thyrohyoid muscle using electromyography (EMG). Sato et al. [9] recently evaluated ten healthy volunteers, recording their swallow activity during asleep states. Consciousness was assessed using surface EMG. In healthy volunteers primary swallowing activity was a mean of 2.4 swallows per hour, ranging between 0.2 and 11.2 per hour dependant on sleep stage. This is in contrast to our findings, which showed a much higher mean swallowing rate of almost 18 per hour. Our population was suspected of having GERD by their referring physician and complained of symptoms possibly related to esophageal dysfunction, whereas Sato’s volunteers did not report any such symptoms. As reflux episodes have been shown to trigger swallowing events, this may play a significant role. Furthermore, we used a catheter based technique, which may induce both primary and secondary peristalsis.
There a few studies available assessing swallowing activities during the night in patients with GERD. Freiden et al. [10] were not able to show differences in swallowing activity between 11 subjects with erosive esophagitis and 11 healthy volunteers recording intra-esophageal pressure using a catheter-based technique. However, a type-2 error cannot be excluded due to the small study population, as swallowing frequency as reported in the paper was higher both in the awake state and during sleep in the esophagitis population. Nominal values were not given in the paper however the graphs show a mean swallowing frequency of approximately 53/h during the awake state compared to 3–25 swallows depending on sleep state in the esophagitis population. This is similar to the values assessed by MII-pH in our GERD symptom group and may underline the much higher incidence of swallows per se when comparing a pharyngeal recording technique and a catheter-based intra-esophageal recording technique.
Limitations to our study are of technical nature, yet are difficult to overcome. The gold standard to monitor night-time arousals are EEG-based sleep laboratory evaluations that also allow sleep stage assessment. It would be highly interesting to assess swallowing activity assessed by multichannel-impedance within different sleep stages; however, studying this in a large patient sample size as we did is difficult to perform due to high costs and extensive resources needed for sleep laboratory testing. A further drawback to formal sleep laboratory testing is the fact that sleeping in an alien environment and different bed with electrodes attached to the scalp does not represent patient everyday physiology. A limitation of actigraphy is the non-continuous sampling rate of 1 measurement per minute, which may miss movement activity and therefore arousals. Yet the Sadeh algorithm accounts for this data frequency monitoring and was validated against formal sleep studies with such [11].
The effects of acid suppressive therapy on sleep patterns and gastro-esohageal reflux have been previously studied [12]. The majority of patients (84 %) in our population were on PPI therapy such that the small minority of patients off PPI does not allow for comparisons within these groups. As we sought to determine the feasibility of using swallowing activity as a surrogate parameter for state of consciousness, we de not believe swallowing activity itself would be different in its association to arousals yet we cannot fully exclude it. Most patients in our lab are tested on PPI therapy as multichannel-impedance allows assessment of both acid and non-acid gastroesophageal reflux episodes [13].
Based on our findings we conclude that swallowing activity differs between the awake and sleeping state. Different cut-off values for swallowing frequency can be used to optimize the sensitivity and specificity to identify awake and asleep periods. For patients undergoing overnight combined impedance-pH monitoring, additional information on the patient’s sleep activity can be derived by analyzing the swallowing frequency. In future studies we wish to extend the use of this technique to assess effects of GERD on sleep pattern and sleep stages.
References
Lichter I, Muir RC. The pattern of swallowing during sleep. Electroencephalogr Clin Neurophysiol. 1975;38:427–432.
Hiestand DM, Britz P, Goldman M, Phillips B. Prevalence of symptoms and risk of sleep apnea in the US population: results from the national sleep foundation sleep in America 2005 poll. Chest. 2006;130:780–786.
Dubois RW, Aguilar D, Fass R, et al. Consequences of frequent nocturnal gastro-oesophageal reflux disease among employed adults: symptom severity, quality of life and work productivity. Aliment Pharmacol Ther. 2007;25:487–500.
Shaker R, Castell DO, Schoenfeld PS, Spechler SJ. Nighttime heartburn is an under-appreciated clinical problem that impacts sleep and daytime function: the results of a Gallup survey conducted on behalf of the American Gastroenterological Association. Am J Gastroenterol. 2003;98:1487–1493.
Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–392.
Sadeh A, Acebo C. The role of actigraphy in sleep medicine. Sleep Med Rev. 2002;6:113–124.
Hila A, Chowdhury N, Hajar N, Castell DO. Swallow evaluation during multichannel intraluminal impedance and pH: an alternate method to assess esophageal transit. J Clin Gastroenterol. 2011;45(10):862–866.
Thie NM, Kato T, Bader G, Montplaisir JY, Lavigne GJ. The significance of saliva during sleep and the relevance of oromotor movements. Sleep Med Rev. 2002;6:213–227.
Sato K, Umeno H, Chitose S, Nakashima T. Deglutition and respiratory patterns during sleep in younger adults. Acta Otolaryngol. 2011;131:190–196.
Freidin N, Fisher MJ, Taylor W, et al. Sleep and nocturnal acid reflux in normal subjects and patients with reflux oesophagitis. Gut. 1991;32:1275–1279.
Paquet J, Kawinska A, Carrier J. Wake detection capacity of actigraphy during sleep. Sleep. 2007;30:1362–1369.
Orr WC, Goodrich S, Robert J. The effect of acid suppression on sleep patterns and sleep-related gastro-oesophageal reflux. Aliment Pharmacol Ther. 2005;21:103–108.
Tutuian R, Castell DO. Review article: complete gastro-oesophageal reflux monitoring—combined pH and impedance. Aliment Pharmacol Ther. 2006;24:27–37.
Acknowledgments
This study was not financially supported by external sources. Costs were covered by a personal research fund of the Medical University of South Carolina for investigator Prof. Donald Castell, Digestive Disease Center, MUSC, USA.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pohl, D., Arevalo, F., Singh, E. et al. Swallowing Activity Assessed by Ambulatory Impedance-pH Monitoring Predicts Awake and Asleep Periods at Night. Dig Dis Sci 58, 1049–1053 (2013). https://doi.org/10.1007/s10620-012-2474-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2474-z