Abstract
Background
Whether addition of prokinetics to proton pump inhibitors improves esophageal peristalsis and symptoms in patients with gastroesophageal reflux disease (GERD) remains unknown.
Aim
We evaluated the effect of mosapride, a 5-HT4 agonist, and PPI cotherapy in patients with GERD on esophageal motility using high-resolution manometry (HRM).
Method
This study was designed as a double-blind, randomized, placebo-controlled trial. Patients with GERD were allocated to a group either taking 40 mg esomeprazole plus 30 mg mosapride or taking esomeprazole plus placebo. Symptom assessment and the HRM study were conducted before drug treatment and after 4 weeks.
Results
Of 50 patients enrolled, 24 in the mosapride group (49 years old, 15 males) and 19 in the placebo group (43 years old, nine males) completed the study. Approximately 79 % of the patients had normal peristaltic function. Treatment response was not different between the two groups (79 vs. 68 %). Mosapride cotherapy tended to yield better response in patients with dyspepsia than those without dyspepsia (92 vs. 67 %). Lower esophageal sphincter pressure didn’t change in both groups. Intrabolus pressure decreased in the mosapride group (3.4 ± 3.5 mmHg to 1.4 ± 4.1 mmHg, P < 0.05). Distal esophageal amplitude increased in the mosapride group and not in the placebo group (81 ± 34 to 89 ± 29 mmHg vs. 82 ± 32 to 83 ± 31 mmHg).
Conclusion
Adding mosapride on esomeprazole improved esophageal contractability and lowered intrabolus pressure in patients with GERD. Mosapride and esomeprazole cotherapy tended to yield better response in patients with concomitant dyspepsia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroesophageal reflux disease (GERD) is primarily a motor disorder with a multifactorial pathogenesis. The main motility abnormalities are represented by an impaired function of the lower esophageal sphincter (LES), abnormal esophageal clearing, delayed gastric emptying, and increased transient LES relaxation.
It has been proposed that prokinetic drugs improve GERD by increasing LES basal pressure, improving esophageal peristalsis, accelerating esophageal acid clearance and facilitating gastric emptying. In Asian consensus on the management of GERD, the use of prokinetic agents either as monotherapy or adjunctive therapy to PPIs may have a role in the treatment of GERD in Asia [1]. Some prokinetics that are currently available demonstrate some efficacy as sole therapy or in combination with a PPI in subsets of patients with GERD [2, 3]. However, the quality of evidence is poor. Thus, further studies are needed to clarify the benefit of the prokinetic agent.
Mosapride, a selective 5-HT4 agonist, elevates resting LES pressure and stimulates esophageal body contractions [4]. In a healthy volunteer study, mosapride enhanced esophageal motility and accelerated esophageal bolus transit [5]. However, another healthy volunteer study showed controversial results [6]. In a few studies, prokinetics combined with PPI showed therapeutic gains compared with use of a PPI alone. Administration of mosapride in addition to omeprazole improved gastroesophageal reflux and gastric emptying in PPI-resistant patients with non-erosive reflux disease (NERD) and delayed gastric emptying [7]. However, a Japanese study showed mosapride did not provide additional benefit to a PPI therapy [8].
High-resolution manometry (HRM) displays and quantifies esophageal function using pressure topography plots. HRM shows a spatial continuum of esophageal pressure. Compared to conventional manometry, HRM provides more detailed information about esophageal segmental contraction and components of the esophageal junction. The aim of this study was to evaluate the efficacy of mosapride on esophageal motility and reflux symptoms using high-resolution esophageal manometry (HRM) in patients with GERD when used with a PPI.
Materials and Methods
Study Design
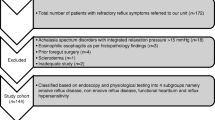
The study was designed as a double-blind, randomized, placebo-controlled trial. Patients diagnosed with GERD who were referred to our hospital from 2010 to 2011 were enrolled. All patients were confirmed not to have alarm symptoms through an interview. The GERD diagnosis was based on one of endoscopy, 48-h Bravo pH monitoring, and typical reflux-associated symptoms. Typical reflux-associated symptoms were heartburn or acid regurgitation that occurred at least twice per week for at least 3 months, and severity was moderate to severe. All patients underwent an endoscopy before enrollment. Erosive esophagitis was stratified using the Los Angeles classification. Some patients underwent 48-h esophageal Bravo pH monitoring. Abnormal esophageal acid exposure was defined as the percentage of time pH<4 was >4 during 48-h Bravo pH monitoring for at least 1 day. Among them, patients who were diagnosed with abnormal acid exposure were classified as the GERD group. Exclusion criteria included severe heart disease, renal or pulmonary failure, liver cirrhosis, severe systemic illness, and a history of malignant disease. Patients who had undergone gastroduodenal surgery and those who recently used NSAlDs or anticoagulant medications were also excluded.
A baseline symptom assessment was performed using a reflux-symptoms questionnaire before the HRM study. This questionnaire included typical symptoms (heartburn and acid regurgitation), epigastric pain, epigastric soreness, and atypical symptoms (e.g., globus, hoarseness, chronic cough, and chest pain). Symptom severity was evaluated using a 5-point Likert scale consisting of “none,” “mild” (an occasional symptom that can be ignored, does not influence daily routine or sleep), “moderate” (symptom cannot be ignored and/or occasionally influences daily routine or sleep), “severe” (symptom presents more frequently during the day or night and/or regularly influences daily routine or sleep) and “very severe” (a constant symptom and/or markedly influences daily routine or sleep). Symptom frequency (2–3 times per month, 1–2 times per week, 3–4 times per week, 5–6 times per week, and daily) and the most-bothersome symptom were also confirmed. Patients whose symptom severity was moderate to severe and occurred at least twice per week were included. Dyspepsia symptoms such as early satiety, postprandial fullness, bloating, nausea, and belching were surveyed with a dyspepsia symptoms questionnaire. These symptom scores were defined by symptom severity as per the 5-point scale.
Enrolled patients were randomly allocated into the mosapride or placebo groups. Patients in the mosapride group were given esomeprazole 40 mg qd + mosapride 10 mg three times per day for 4 weeks after baseline symptom assessment and HRM. Patients in the placebo group were given esomeprazole 40 mg qd + placebo three times per day for 4 weeks. After 4 weeks, symptom assessment and HRM study were repeated. The PPI response was considered positive if global symptoms improved >50 % from the 6-point Likert scale of the reflux symptom questionnaire after PPI treatment, and when predominant symptoms greater than moderate severity decreased to become mild or absent.
Written informed consent was obtained from all subjects prior to undergoing upper gastrointestinal endoscopy and abdominal ultrasonography for evaluation of dyspeptic symptoms. This study protocol was approved by the Ethical Review Committee of Seoul St. Mary’s Hospital.
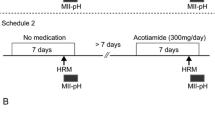
HRM Protocol
Antisecretory agents including PPIs and medications affecting esophageal motility were discontinued within 1 week before the HRM study. We performed HRM using a ManoScan 360 instrument (Sierra Scientific Instruments, Inc., Los Angeles, CA, USA). The subjects were examined in the sitting position after fasting overnight. The manometric assembly was passed through an anesthetized nostril and positioned so that the most proximal of the 1-cm interval side holes was 2-cm above the lower esophageal sphincter (LES). The subjects were then allowed to adapt to the assembly for 10 min. Baseline recordings of LES pressure were made for 5 min, and then esophageal peristalsis was assessed in response to 15 swallows of a 5-ml water bolus. Each swallow was separated by a 30-s interval.
HRM Data Analysis
The primary outcome parameters were esophageal motility or peristalsis measured by HRM and secondary outcome parameter was symptomatic improvement. High-resolution topographical plots from the 15 swallows were analyzed to determine the best pressure trough locations, which were used to separate the peristaltic sequence into individual segments. Topographical measurements were then performed while focusing on esophageal segmental contraction. The ManoView analysis software (Sierra Scientific Instruments) was used to calculate the segmental contraction variables by creating a space–time box. Manometry interpretation was performed by one physician who was blinded to the patient groups.
Baseline LES pressure and post deglutative relaxation were measured. Peristaltic contractions in the esophageal body were divided into proximal, mid, and distal segments separated by two troughs, as shown in Fig. 1. Using ManoView analysis, the mid and distal-esophageal segmental contractions were assessed in detail, at 3-, 7-, and 11-cm above the LES by (1) contractile pressure, (2) onset velocity and (3) duration as the peristaltic contraction passes from the pharynx to the stomach. HRM measurements of esophageal peristalsis also included the distal contractile integral [HRM plot “contraction volume” with x, y, and z axes represented by the length (cm), width (s), and pressure (mmHg)]. The proximal “transition zone” was defined by the presence of a pressure trough between the proximal and midesophageal peristaltic contractions. Coordination (temporal and spatial separation) between these contractions was quantified at a 30-mmHg isobaric contour per swallow. A position two-thirds down the length of the esophagus was used for measurement in the absence of a clear pressure trough at this level.
Esophageal pressure activity shown in high resolution manometry. The proximal transition zone (pressure trough) between the proximal and midoesophagus was measured at 30 mmHg isobaric contour. The changes in velocity, contractile pressure and width in the mid- and distal-segmental contractions measured at 11, 7, and 3 cm above the lower esophageal sphincter
Sample Size and Statistical Analysis
Initially, sample sizes were calculated by referring to two esophageal impedance manometry studies [5, 9]. Assuming a 15 % dropout rate and about ten swallows per subject, a sample size of 40 patients (20 patients per group) was planned. After initial enrollment of 40 patients, we extended the study population to 50 patients to determine whether HRM parameters of statistically borderline significance were really different. However, the results did not change after including additional ten patients.
HRM data are presented as means ± standard deviations. Descriptive statistics (median and 25th–75th percentile) are used to describe the HRM findings, because they were not normally distributed. The Mann–Whitney U test was used to determine the differences in the symptom scores between the two groups. The Wilcoxon rank-sum test was used to assess differences in HRM data between the two groups. All tests were performed using the SPSS software (SPSS Inc., Chicago, IL, USA). A value of P < 0.05 was considered to indicate statistical significance.
Results
This study was conducted between November 2009 and May 2011. The 50 recruited patients were randomized into the esomeprazole + mosapride (n = 27) and esomeprazole (n = 23) groups. Five patients did not complete the study, and two showed <80 % drug compliance. The overall compliance rate was >90 % for the remaining patients in both treatment groups. Twenty-four patients in the esomeprazole + mosapride group (mean 49 ± 16 years; M:F = 15:9) and 19 in the esomeprazole group (mean 43 ± 15 years; M:F = 9:10) completed the study. Therefore, 43 patients were analyzed by the protocol. Baseline demographic variables of the two groups are shown in Table 1. No significant difference was observed between the treatment groups for any baseline demographic characteristic (Table 1).
Symptom Assessment
Overall responsiveness in all patients was 74 % (32/43). Treatment responsiveness in the esomeprazole + mosapride group was not different from the esomeprazole group (79 vs. 68 %). Twenty of 46 patients complained of dyspepsia symptoms. Adding mosapride on PPI tended to have better PPI responsiveness only in patients having concomitant dyspepsia whereas this effect was negligent in patients without dyspepsia (92 vs. 67 %, P = 0.07, Table 2).
Effect of Mosapride on LES Pressure and Intrabolus Pressure (IBP)
LES length and basal LES pressure did not change after treatment in either group. However, mean IBP decreased significantly in the esomeprazole + mosapride group (3.4 ± 3.5 mmHg to 1.4 ± 4.1 mmHg, P = 0.04), whereas it did not change in the esomeprazole group (Table 3, Fig. 2).
Effect of Mosapride on Esophageal Peristalsis and Esophageal Segmental Contraction
The baseline HRM diagnosis was normal in 19 (79 %) patients, intermittent hypotensive peristalsis in two, and diffuse hypotensive peristalsis in three patients in the esomeprazole + mosapride group. In the esomeprazole group, HRM diagnosis was normal in 15 (79 %), intermittent hypotensive peristalsis was present in two, and diffuse hypotensive peristalsis was present in two patients. In the esomeprazole + mosapride group, one patient with diffuse hypotensive peristalsis improved as intermittent hypotensive peristalsis. Except for that one patient, the HRM diagnoses didn’t change in either group (Fig. 3).
Most swallows showed normal peristalsis. Approximately 91 % of the swallows showed normal peristalsis in the esomeprazole + mosapride group, whereas 95 % were normal in the esomeprazole group. The proportion of peristaltic contractions, simultaneous contractions, and failed contractions did not change after treatment in either group (Table 4). Distal esophageal amplitude increased slightly after esomeprazole + mosapride treatment (80.8 ± 33.7 to 89.1 ± 29.1 mmHg), whereas it did not change after esomeprazole treatment. The spatial separation of the proximal transition zone (separation between the proximal and mid-esophageal contractions) in both groups was unaffected by treatment.
Discussion
We investigated the effect of mosapride on esophageal peristaltic function in patients with GERD. Our study showed that mosapride combined with esomeprazole improved esophageal segmental contractibility and decreased IBP in patients with GERD. The promoting effect of mosapride even reached patients with normal peristaltic function. In addition, a combination of mosapride and esomepazole tended to yield better PPI responsiveness in patients with concomitant dyspepsia than in those without dyspepsia.
Mosapride citrate may improve symptoms of patients with GERD by modulating esophageal motor function, which may result in reducing reflux and accelerating gastric emptying. PPI responsiveness in the two groups was not significantly different (79 vs. 68 %). In the mosapride group, patients with dyspepsia tended to improve better (92 vs. 67 %). However, the number of patients was small to make a firm conclusion about symptom improvement. Further study with a large number of patients is needed.
Mosapride had no effect on LES pressure or deglutative LES relaxation. Instead, IBP decreased significantly in the esomeprazole + mosapride group. A physiological significance of these findings is not known. IBP is common cavity pressure “beneath” the peristaltic wave and measured between the leading edge of the distal segment contraction and the esophagogastric junction (EGJ). Thus, IBP indicates outflow resistance against bolus transit. So, elevated IBP occurs with a functional EGJ obstruction or outflow obstruction, such as incomplete EGJ relaxation. Therefore, reduced IBP after mosapride treatment can be translated such that mosapride makes bolus transit easier by reducing outflow resistance.
The distal contractile integral did not change after mosapride treatment. However, distal esophageal amplitude tended to increase in the esomeprazole + mosapride group. Mid esophageal contractibility was not affected. We used HRM to assess the effects of mosapride on the motor activity of different segments of the esophageal body. Conventional manometry is not sufficiently sensitive to measure peristaltic contractions in the three esophageal body segments [10]. HRM displays and quantifies esophageal function using pressure topography plots. Peristaltic contraction in the distal segment of the esophageal body is the strongest in amplitude and the most important factor for volume clearance of acidic refluxant from the stomach [11]. The proximal peristaltic segment represents the skeletal muscle component of the esophageal body, whereas the lowest distal segment represents the smooth muscle component. A transition zone (TZ) exists between the proximal and distal contractile segments and represents the region of spatiotemporal merging between these two contractile waves [12]. Mosapride did not affect shortening of the proximal TZ despite its enhancement of distal contractile amplitude.
Although these were statistically significant changes of the IBP and contraction amplitude, these magnitude changes may be negligible in terms of clinical improvement. In the mosapride group, five patients were initially diagnosed as hypotensive peristalsis in HRM study. One of them with diffuse hypotensive peristalsis improved as intermittent hypotensive peristalsis. Also, the proportion of failed contraction didn’t improve in either group. In addition, the prominent symptom improvement in the patients with dyspepsia in the mosapride group may be associated with overlap with functional dyspepsia and GERD.
Several outcome studies using HRM have been conducted. HRM provides precise information regarding esophageal segmental motility, peristalsis, and the constituents of the EGJ [13]. In this study, HRM identified the functionally important aspects of esophageal motor activity that could not be assessed by conventional manometry. Our results suggest that HRM can be used to identify outcomes in patients with suspected or mild esophageal motility disorders.
In conclusion, a combination of mosapride with esomeprazole affected esophageal peristalsis by improving esophageal contractibility and lowering IBP in patients with GERD that could lead to facilitating esophageal bolus transit. These findings suggest that addition of prokinetics to PPI therapy would be useful for patients with GERD.
References
Fock KM, Talley NJ, Fass R, et al. Asia-Pacific consensus on the management of gastroesophageal reflux disease: update. J Gastroenterol Hepatol. 2008;23:8–22.
Cucchiara S, Staiano A, Boccieri A, et al. Effects of cisapride on parameters of oesophageal motility and on the prolonged intraoesophageal pH test in infants with gastro-oesophageal reflux disease. Gut. 1990;31:21–25.
Goldin GF, Marcinkiewicz M, Zbroch T, Bityutskiy LP, McCallum RW, Sarosiek J. Esophagoprotective potential of cisapride. An additional benefit for gastroesophageal reflux disease. Dig Dis Sci. 1997;42:1362–1369.
Ruth M, Finizia C, Cange L, Lundell L. The effect of mosapride on oesophageal motor function and acid reflux in patients with gastro-oesophageal reflux disease. Eur J Gastroenterol Hepatol. 2003;15:1115–1121.
Cho YK, Choi MG, Han HW, et al. The effect of mosapride on esophageal motility and bolus transit in asymptomatic volunteers. J Clin Gastroenterol. 2006;40:286–292.
Koshino K, Adachi K, Furuta K, et al. Effects of mosapride on esophageal functions and gastroesophageal reflux. J Gastroenterol Hepatol. 2010;25:1066–1071.
Futagami S, Iwakiri K, Shindo T, et al. The prokinetic effect of mosapride citrate combined with omeprazole therapy improves clinical symptoms and gastric emptying in PPI-resistant NERD patients with delayed gastric emptying. J Gastroenterol. 2010;45:413–421.
Miwa H, Inoue K, Ashida K, et al. Randomised clinical trial: efficacy of the addition of a prokinetic, mosapride citrate, to omeprazole in the treatment of patients with non-erosive reflux disease—a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2011;33:323–332.
Chen CL, Yi CH. Utility of esophageal impedance in identifying dysmotility in patients with erosive esophagitis. Dis Esophagus. 2008;21:539–543.
Clouse RE, Staiano A, Alrakawi A, Haroian L. Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol. 2000;95:2720–2730.
Murray JA, Clouse RE, Conklin JL. Components of the standard oesophageal manometry. Neurogastroenterol Motil. 2003;15:591–606.
Ghosh SK, Janiak P, Schwizer W, Hebbard GS, Brasseur JG. Physiology of the esophageal pressure transition zone: separate contraction waves above and below. Am J Physiol Gastrointest Liver Physiol. 2006;290:G568–G576.
Fox M, Menne D, Stutz B, Fried M, Schwizer W. The effects of tegaserod on oesophageal function and bolus transport in healthy volunteers: studies using concurrent high-resolution manometry and videofluoroscopy. Aliment Pharmacol Ther. 2006;24:1017–1027.
Acknowledgments
This work was supported by a research grant from Daewoong Pharmaceuticals Co, Ltd.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cho, Y.K., Choi, MG., Park, E.Y. et al. Effect of Mosapride Combined with Esomeprazole Improves Esophageal Peristaltic Function in Patients with Gastroesophageal Reflux Disease: A Study Using High Resolution Manometry. Dig Dis Sci 58, 1035–1041 (2013). https://doi.org/10.1007/s10620-012-2430-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2430-y