Abstract
Background
Previous studies have shown that non-erosive reflux disease (NERD) patients are less sensitive to proton pump inhibitor (PPI) treatment than patients with erosive reflux disease. The aim of this study was to investigate whether treatment with prokinetics in addition to omeprazole therapy would improve clinical symptoms, gastric emptying and esophageal peristalsis in PPI-resistant NERD patients with or without delayed gastric emptying.
Methods
Subjects were 64 consecutive patients presenting with typical symptoms of PPl-resistant NERD (n = 44) and 20 healthy volunteers. PPI-resistant NERD patients underwent mosapride citrate (15 mg/day) and omeprazole (20 mg/day) co-therapy for 12 weeks. We evaluated the clinical symptoms as well as gastric emptying and esophageal manometry before and after combined therapy. We measured both acylated- and des-acylated plasma ghrelin levels by the ELISA method. The primary endopoint was to investigate whether co-administration of mosapride citrate and omeprazole would improve clinical symptoms and gastric emptying in PPI-resistant NERD patients with delayed gastric emptying.
Results
Tmax value in PPI-resistant NERD patients was significantly higher than in healthy volunteers. Combination therapy with the prokinetic agent mosapride citrate and omeprazole significantly improved reflux symptoms and Tmax value in Tmax > 65 min NERD patients. Co-therapy also significantly reduced des-acylated-ghrelin levels in NERD patients with delayed gastric emptying.
Conclusions
Administration of mosapride citrate in addition to omeprazole improved gastro-esophageal reflux and gastric emptying in PPI-resistant NERD patients with delayed gastric emptying.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
About one-fifth of the adult population in Western countries experiences typical weekly symptoms of gastroesophageal reflux disease (GERD), such as heartburn and regurgitation [1]. Recently, we have come to realize that the majority of GERD patients do not have any endoscopically visible lesions in the distal part of the esophagus. Several mechanisms have been proposed for the pathogenesis of non-erosive reflux disease (NERD), including visceral hypersensitivity, prolonged contraction of the esophagus and psychological factors [2–4]. Therefore, it is clear that NERD is an umbrella concept covering heterogenous subgroups of patients with different mechanisms responsible for their symptoms. It has been shown that between 33 and 50% of NERD patients presenting with heartburn do not have any evidence of pathological acid reflux during 24-h esophageal pH testing [5, 6]. Indeed, several studies have demonstrated that NERD patients are less sensitive to proton pump inhibitor (PPI) treatment than patients with erosive reflux disease [7–9].
In fact, some recent studies have suggested that the pathogenesis of NERD may differ from that of erosive GERD or Barrett’s esophagus [10, 11]. The physiology of the lower esophageal sphincter, so fundamental to the pathophysiology of all manifestations of GERD, is intimately related to that of the gastric fundus and cardia. In other studies, gastric distention significantly increased the transient lower esophageal sphincter relaxation (tLESR) [11–13]. To date, there are no available data regarding the relationship between gastric motility and NERD patients.
Mosapride citrate is a prokinetic agent known to stimulate the serotonin 5-hydroxytryptan-4 (5-HT4) receptor, increase acetylcholine release from the parasympathetic nerve endings, and promote bowel motility and gastric emptying [14]. Some previous studies have revealed that mosapride citrate decreases acid reflux to the esophagus in GERD patients and improves gastric emptying in healthy volunteers and diabetic patients for both solids and liquids [15, 16]. Therefore, in this study, we investigated whether mosapride citrate and omeprazole co-therapy could alleviate clinical symptoms in PPI-resistant NERD patients by improving gastric emptying and esophageal peristalsis.
Materials and methods
Patients
Forty-four consecutive patients presenting with typical symptoms of PPI-resistant NERD and 20 healthy volunteers were enrolled after upper gastrointestinal endoscopy and abdominal ultrasonography. Participants were recruited from September 2006 to April 2008. The diagnosis of NERD was based on typical reflux-associated symptoms (QUEST score >4 points) that occurred at least twice a week for at least 6 months before diagnosis in the absence of visible esophageal mucosal breaks at endoscopy. The exclusion criteria included severe heart disease, renal or pulmonary failure, liver cirrhosis, severe systemic illness and history of malignant disease. Patients with previous gastroduodenal surgery and those on recently used NSAlD or anticoagulant medication were also excluded. H. pylori infection was determined by both the 13C-urea breath test and histological identification. Healthy volunteers were recruited from a general pool of medical students and doctors. Written informed consent was obtained from all subjects prior to undergoing upper gastrointestinal endoscopy and abdominal ultrasonography for evaluation of dyspeptic symptoms. The study protocol was approved by the Ethical Review Committee of the Nippon Medical School Hospital.
Study protocol
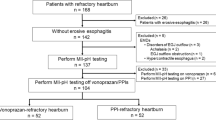
Proton pump inhibitor-resistant NERD was diagnosed when 4-week omeprazole treatment (20 mg/day) failed to improve clinical symptoms (QUEST score >4 points) in NERD patients. PPI-resistant NERD patients were treated with the prokinetic agent mosapride citrate for 12 weeks in addition to omeprazole (20 mg/day). We evaluated clinical symptoms as well as gastric emptying and esophageal manometry twice in this study; the first evaluation was done after 4-week omeprazole treatment prior to mosapride citrate co-therapy, and the second evaluation after 12-week mosapride citrate (15 mg/day) administration in addition to omeprazole (20 mg/day) (Fig. 1). All study personnel and participants were blinded to treatment assignment for the duration of the study. In addition, we evaluated gastric emptying and esophageal manometry blindly.
Study protocol. PPI-resistant NERD was diagnosed when 4-week omeprazole treatment (20 mg/day) failed to improve clinical symptoms in NERD patients. PPI-resistant NERD patients were treated for 12 weeks with combined mosapride citrate (15 mg/day) and omeprazole (20 mg/day) therapy. Clinical symptoms, gastric emptying and esophageal manometry were evaluated before and after combined therapy
Endoscopic assessment of NERD
The patients were evaluated by endoscopy for reflux-associated disease if they complained of typical heartburn symptoms, i.e., a burning feeling rising from the stomach or lower chest up toward the neck at least twice a week [17] for a period of at least 6 months prior to examination.
Clinical symptoms
Gl symptoms were assessed based on the GSRS questionnaire, which proved reliable and valid for the evaluation of GI symptoms [18, 19]. The GSRS consists of 15 items, each rated on the 7-point Likert scale (1–7), ranging from “no discomfort at all” to “very severe discomfort.” The scores for abdominal pain, reflux, diarrhea, indigestion and constipation subscales were calculated by averaging the scores of the items completed within an individual subscale, with higher scores indicating more severe symptoms. After combined therapy, patients experiencing no discomfort at all for a particular symptom were considered cured for that clinical symptom; that is, when the GI score for each symptom such as abdominal pain, reflux, diarrhea, indigestion, and constipation improved to a score 1.
Measurement of gastric motility
Sodium acetate (water soluble) for emptying of liquids was used as a tracer (Cambridge Isotope Laboratories; Cambridge, MA). Probes were analyzed by non-dispersive infrared spectroscopy (IRIS, Wagner Analyzentechnik; Bremen, Germany). The subject’s own production of 300 mmol CO2 per m2 body surface and per hour was set as default value. Integrated software solutions calculated the half gastric emptying time (T 1/2) and the lag phase (T max) as the point of maximum gastric emptying according to Hellmig et al. [20]. Hellmig et al. [20] have also reported that the gastric emptying of liquid meals was similar to that of solid meals. T max value >65 min indicated disturbance of gastric emptying [21].
Study protocol for gastric emptying of liquids
The liquid test meal consisted of 100 mg of 13C-acetate dissolved in 200 ml of a liquid meal (Racol, l ml/1 kcal; Otsuka Pharmacia Company; Tokyo, Japan). Breath samples were taken at 0, 10 s, 5, 10, 15, 20, 30, 40, 50, 60, 75 and 90 min after ingestion. The patients were instructed not to drink, eat or smoke during the test.
Recording methods
Esophageal manometry was performed with a 21-channel manometric assembly (Dentsleeve; Wayville, Australia). We used ten-side holes, which were spaced at 1-cm intervals starting at 3 cm above the distal end of the assembly to monitor the pressure from the proximal stomach, LES and distal esophagus. We used another seven side holes, spaced at 2-cm intervals, to monitor the pressure from the distal to the proximal esophagus and four side holes at 3, 6, 10, and 13 cm above the most proximal of the 2-cm interval side holes to monitor the pressure from the proximal esophagus to the pharynx. Each lumen was perfused with degassed distilled water at 0.15 ml/min by a low compliance manometric infusion pump (Dentsleeve). The data were digitized with a computer, and the digitized signals were displayed, stored and analyzed using Trace Software (Dr GS Hebbard, Royal Melbourne Hospital; Melbourne, Australia).
Study protocol for esophageal manometry
The subjects were examined in the sitting position after fasting overnight. The manometric assembly was passed via an anesthetized nostril and positioned so that the most proximal of the 1-cm interval side holes was 2 cm above the LES. The subjects were then allowed to adapt to the assembly for 10 min. Baseline recordings of LES pressure were made for 5 min, and then primary and secondary peristalsis was assessed. The primary peristalsis was assessed in response to ten swallows of a 5-ml water bolus. Each swallow was separated by a 30-s interval. Secondary peristalsis was triggered by esophageal distention using a 20-ml air bolus, which was injected rapidly by hand into the mid-esophagus through an infusion port located 11 cm above the LES. After 20 s, each stimulus was followed by a dry swallow to clear any residual air. Each stimulus was repeated five times [22].
Intraluminal esophageal pH recording
Twenty-four-hour esophageal pH values were monitored in nine PPI-resistant NERD patients with delayed gastric emptying who consented to the monitoring for assessment of the severity of acid reflux in the esophagus. The study was carried out on an outpatient basis, after at least 6 h of fasting. A Digitrapper Mark III recorder (Synectics Medical, Stockholm, Sweden) was used. An antimony pH catheter (Zenetics Medical; Salt Lake City, UT) was inserted intranasally and positioned 5 cm above the lower esophageal sphincter. Patients then underwent 24-h pH monitoring, and diaries were provided for them to record their symptoms during the study period. At the end of the 24-h recording period, data were transferred to a commercially available software program (Esophagogram, Gastrosoft; Stockholm, Sweden). Patients were encouraged to maintain normal activity and sleep schedules. Meals (total 1,500 kcal, fat 25%) were given at 9:00 a.m. (breakfast), 12:30 p.m. (lunch) and 7:30 p.m. (supper).
Data analysis
The primary and secondary peristalsis was classified as successful if a pressure wave of more than 12 mmHg at the three proximal esophageal recording sites (16, 19 and 22 cm above the LES) and of more than 25 mmHg at the middle and distal esophageal recording sites progressively traversed all of the esophageal recording sites. Peristaltic progression was defined as a peristaltic velocity of <6 cm/s. The criteria of failed peristalsis were failure of a pressure wave of more than 12 mmHg at the three proximal esophageal recording sites, failure to traverse each of the esophageal recording sites, or a peristaltic velocity of more than 6 cm/s between the recording sites at 2 and 22 cm above the LES [15]. Normal secondary peristalsis was defined as the occurrence of four or more complete peristaltic responses to the five air boluses [17].
Tracings were reviewed, meals periods were timed, changes in body position were noted and the time that symptoms were recorded was compared with the information written in the diaries. The pathological acid reflux (abnormal acid exposure time) is considered present when intra-esophageal pH falls below 4 for >4.2% of the time [23]. Analysis of pH tracing was done as follows: (1) the time period percentage with an esophageal pH of <4.0 was calculated as a proportion of the recording periods and (2) acid reflux was defined as those periods when the pH in the esophagus dropped to below 4.0.
Measurement of plasma ghrelin levels
We then measured the plasma ghrelin levels to evaluate their association with gastric motility. Blood was drawn into chilled tubes containing EDTA-2Na (1 mg/ml) and aprotinin (500 U/ml), and the plasma was taken after immediate centrifugation and stored at −30°C until assay. Plasma immunoreactive ghrelin concentrations (acylated- and des-acylated) were measured in duplicate using a commercial radioimmunoassay (Phoenix Pharmaceuticals; Belmont, CA). The intra-assay coefficient of variation (CV) was 8.1%, and the inter-assay CV, 9%. The range of detection was 10–1,280 pg/ml.
Measurement of serum pepsinogen I and II
Serum PGI and II levels were measured using E Plate Pepsinogen I and II (Eiken Chemical Co., Ltd.) using cutoff levels of PGI < 70 μg/L + PGI/II ratio <3 as low PG levels (L-PG) and PGI < 30 μg/l + PGI/II ratio <2 as very low PG levels (VL-PG) according to the instructions of the manufacturer.
Statistical analysis
For statistical evaluation of group data, Student’s t test for paired data and analysis of variance (ANOVA) for multiple comparisons were followed by Scheffe’s F test. Mann–Whitney U test was used for analysis of categorical data. A P value of <0.05 was considered statistically significant.
Results
Characteristics of PPI-resistant NERD patients
BMI scores did not vary significantly between the two groups of patients and healthy volunteers (Table 1). There was also no significant variation in H. pylori positivity rates between PPI-resistant NERD patients with delayed gastric emptying and those without (Table 1). The pepsinogen I/II ratio in PPI-resistant NERD patients with or without delayed gastric emptying and healthy volunteers was 5.68 ± 2.4, 5.72 ± 1.9 and 6.71 ± 1.8, respectively. There was no significant difference in the pepsinogen I/II ratio among the three groups (Table 1).
Tmax value in PPI-resistant NERD patients
We then used the 13C-acetate breath test to calculate the T max value as a marker of gastric emptying of liquids and compared gastric motility among PPI-resistant NERD patients and healthy volunteers. The T max value in PPI-resistant NERD patients was significantly higher than that in healthy volunteers (Fig. 2).
Mosapride citrate combined with omeprazole improves reflux symptoms and T max value in PPI-resistant NERD patients with delayed gastric emptying
To elucidate the possibility that the prokinetic effect of mosapride citrate improved gastro-esophageal reflux symptoms via its effect on gastric emptying, we measured the T max value and clarified whether administration of mosapride citrate in addition to omeprazole affected gastric emptying in PPI-resistant NERD patients with or without delayed gastric emptying. Mosapride citrate in combination with omeprazole therapy significantly improved the T max value in PPI-resistant NERD patients with delayed gastric emptying (Fig. 3). Combined therapy significantly improved T max value in 83% (20/24) of PPI-resistant NERD patients with delayed gastric emptying. We also investigated whether mosapride citrate combined with omeprazole improved the upper GI symptoms and lower GI symptoms. Mosapride citrate combined with omeprazole significantly improved reflux symptoms in the T max > 65 min group of NERD patients compared to that in the T max < 65 min group (Fig. 4).
Mosapride citrate combined with omeprazole improves T max value in PPI-resistant NERD patients with delayed gastric emptying. Mosapride citrate significantly improved (P < 0.05) the T max value in T max > 65 min NERD patients. *Versus T max value in T max > 65 min NERD patients before combined therapy, P < 0.05
The ratios of NERD patients with T max > 65 min and T max < 65 min cured with mosapride citrate and omeprazole co-therapy. Mosapride citrate significantly improved reflux symptoms in PPI-resistant NERD patients with T max value > 65 min. In contrast, mosapride citrate did not improve any clinical symptoms in PPI-resistant NERD patients with T max value < 65 min. *Versus the ratio of cured patients after 12 weeks of treatment with mosapride citrate combined with omeprazole in PPI-resistant NERD patients with T max < 65 min, P < 0.05
In some T max > 65 min NERD patients (n = 9), we investigated whether combined mosapride citrate and omeprazole treatment affects the acid exposure time and the frequency of acid reflux using 24-h pH monitoring. There was no abnormal acid exposure time (0.1 ± 0.08%) in nine PPI-resistant NERD patients with delayed gastric emptying under 4-week omeprazole treatment. In addition, there was no difference in the acid exposure time (0.1 ± 0.08 and 0.07 ± 0.06%) and the frequency of acid reflux (5.2 ± 3.2, 3.6 ± 3.4) in nine PPI-resistant NERD patients with delayed gastric emptying between before and after combined therapy.
Esophageal secondary peristalsis in PPI-resistant NERD patients after combined mosapride citrate and omeprazole therapy
To elucidate the possibility that the prokinetic effect of mosapride citrate improved gastro-esophageal reflux symptoms via its effect on esophageal peristalsis, we measured secondary esophageal peristalsis in NERD patients with or without delayed gastric emptying. Although mosapride citrate and omeprazole co-therapy increased the amplitude of primary esophageal peristalsis in some cases (Fig. 5a, b), combined mosapride citrate and omeprazole therapy did not affect primary esophageal peristalsis in most of cases. In addition, mosapride citrate and omeprazole co-therapy did not significantly increase esophageal secondary peristalsis in PPI-resistant NERD patients with or without delayed gastric emptying (Fig. 5c).
Esophageal secondary peristalsis in PPI-resistant NERD patients with or without delayed gastric emptying after combined mosapride citrate and omeprazole therapy. Mosapride citrate and omeprazole co-therapy had no statistically significant effect on esophageal secondary peristalsis in PPI-resistant NERD patients with or without delayed gastric emptying
Plasma ghrelin levels in PPI-resistant NERD patients after combined mosapride citrate and omeprazole therapy
Mosapride citrate combined with omeprazole did not significantly increase acylated ghrelin levels in PPI-resistant NERD patients with or without delayed gastric emptying (Fig. 6). In contrast, mosapride citrate combined with omeprazole significantly reduced des-acylated ghrelin levels in PPI-resistant NERD patients with delayed gastric emptying (Fig. 6).
Mosapride citrate and omeprazole co-therapy reduces des-acylated ghrelin levels in PPI-resistant NERD patients with delayed gastric emptying. Mosapride citrate combined with omeprazole significantly reduced the des-acylated ghrelin levels in PPI-resistant NERD patients with delayed gastric emptying. *Versus desacylated-ghrelin levels in T max > 65 min NERD patients before combined therapy, P < 0.05
Discussion
The major findings in this study are as follows: (1) T max values, one of the markers of gastric emptying, were significantly higher in PPI-resistant NERD patients than in healthy volunteers. (2) Administration of mosapride citrate in addition to omeprazole significantly improved reflux symptoms and T max value in PPI-resistant NERD patients with delayed gastric emptying. (3) Mosapride citrate combined with omeprazole significantly reduced des-acylated ghrelin levels in NERD patients with T max > 65 min.
Non-erosive reflux disease is a chronic disease with high impact on the quality of life [5, 7, 24]. Between 37 and 60% of NERD patients have no increased distal esophageal acid exposure. In addition, they do not respond very well to anti-secretory therapy with PPIs. Several mechanisms have been proposed for the pathogenesis of NERD patients, including visceral hypersensitivity, prolonged contraction of the esophagus and psychological factors [2–4]. We could not find any clinical reports in the available literature regarding the association between gastric emptying and NERD patients. The present study is the first to show that the T max value, which serves as a marker of gastric emptying, was significantly higher in PPI-resistant NERD patients than in healthy volunteers, as confirmed by the 13C breath test. The current standard method for measuring gastric emptying is the radioactive isotope method [25]. The 13C-acetate breath test has also been reported to be a reliable and non-invasive tool for analysis of gastric emptying rates without radiation exposure and to be comparable to scintigraphy [26].
Previous studies have shown that mosapride citrate significantly improved gastric emptying in healthy volunteers, and in patients with Parkinson’s disease and diabetic mellitus [16, 27, 28]. Recently, using capsule endoscopy or percutaneous electrogastrogram (EGG), mosapride citrate has been found to improve gastric emptying [29, 30]. We are the first to report that, when combined with omeprazole, the prokinetic effect of mosapride citrate alleviates reflux symptoms and gastric emptying in PPI-resistant NERD patients with delayed gastric emptying, determined by the 13C-acetate breath test. Some studies have failed to find a relationship between delayed gastric emptying and the pattern of symptoms in FD patients [31, 32]. Quigley et al. [33] have reported that the precise prevalence of delayed gastric emptying remains to be defined in GERD. Ruth et al. [34] have also reported that mosapride citrate decreases acid reflux to the esophagus in GERD patients by its improvement of gastric emptying, as seen in healthy volunteers and diabetic patients for both solids and liquids [16]. Further studies are needed to clarify whether the synergistic effect of mosapride citrate and omeprazole also improves clinical symptoms through their combined effect on gastric motility in PPI-resistant NERD patients.
The current concepts in the pathophysiology of NERD include peripheral factors in the esophageal lumen, such as non-acid reflux, gas reflux and proximal distention of the esophagus [35, 36]. Other studies have shown that roughly 40% of patients with heartburn had normal test results during 24-h intraesophageal pH monitoring [37, 38]. In addition, esophageal hypersensitivity to normal levels of intraesophgeal acid may play an important role in the pathogenesis of heartburn, and this hypersensitivity appears to be enhanced in NERD patients [39]. In our study, there was no abnormal acid exposure time in omeprazole-treated NERD patients. Then, after mosapride and omeprazole combined therapy, we could find no significant difference in the acid exposure time and the frequency of acid reflux in PPI-resistant NERD patients in spite of improvements in delayed gastric emptying. A previous study has reported that mosapride citrate inhibited the visceromotor response by gastric distention in conscious rats [40]. Therefore, mosapride and omeprazole cotherapy may act through its modification of visceral sensation. Previous studies have reported that non-acid reflux was also related to symptoms in NERD patients using impedance test [41, 42]. Thus, in addition to more in-depth analysis of esophageal hypersensitivity, further studies are needed to clarify the precise relationship between the acceleration of gastric emptying induced by mosapride citrate and reduction in the positive symptom index for non-acid reflux in PPI-resistant NERD patients with delayed gastric emptying, as measured by impedance test. Esophageal secondary peristalsis is a component of the acid clearance mechanism [43]. Our group has reported that the triggering of secondary peristalsis was disturbed in NERD patients [44]. Ruth et al. [45] have reported that mosapride citrate improved esophageal motor function in GERD patients. Therefore, in this study, we investigated the effect of mosapride citrate on esophageal secondary peristalsis in omeprazole-treated NERD patients with or without delayed gastric emptying. However, we confirmed that mosapride citrate and omeprazole co-therapy did not significantly improve esophageal secondary peristalsis in this group of patients.
In human studies, ghrelin infusion also increased food intake and sensation of hunger as compared with saline infusion alone [46]. Although we investigated whether the prokinetic effect of mosapride citrate improved gastric emptying via the up-regulation of plasma acylated ghrelin levels, mosapride did not significantly affect plasma acylated ghrelin levels in PPI-resistant NERD patients. A previous study has demonstrated that mosapride citrate increases acetylcholine release from parasympathetic nerve endings [14]. Furthermore, Broglio et al. [47] have reported that acetylcholine regulates ghrelin secretion. Therefore, mosapride citrate may increase the T max value via the up-regulation of acetylcholine-stimulated ghrelin levels. However, in our study, although mosapride treatment improved T max values in PPI-resistant NERD patients, there was no corresponding elevation in acylated ghrelin levels. In contrast, when combined with omeprazole, mosapride citrate significantly reduced des-acylated ghrelin levels in PPI-resistant NERD patients with delayed gastric emptying. Further studies are needed to clarify the effects of mosapride citrate on des-acylated ghrelin levels. In addition, another study showed that plasma ghrelin levels correlated with gastric atrophy [48]. Suzuki et al. [49] have reported that plasma ghrelin levels correlated well with levels of serum pepsinogen I/II (PGI/II) ratio and decreased with extent of gastric mucosal atrophy. However, in our study, there was no significant difference in the serum pepsinogen I/II ratio between the mosapride-treated group and the non-treated groups.
Taken together, in this study, the prokinetic effect of mosapride citrate combined with omeprazole improved gastro-esophageal reflux symptoms and gastric emptying in PPI-resistant NERD patients with delayed gastric emptying. Further studies are needed to clarify the mechanisms by which mosapride citrate affects gastric emptying in PPI-resistant NERD patients.
References
Locke GR 3rd, Talley NJ, Fett SL, Zinsmeiser AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted Country, Minnesota. Gastroenterology. 1997;112:1448–56.
Shi G, Bruley des Varannes S, Scarpignato C, Le Rhun M, Galmiche JP. Reflux related symptoms in patients with normal oesophageal exposure to acid. Gut. 1995;37:457–64.
Fass R, Naliboff B, Higa L, Johnson C, Kodner A, Munakata J, et al. Differential effect of long-term esophageal acid exposure on mechanosensitivity and chemosensitivity in humans. Gastroenterology. 1998;115:1363–73.
Kamolz T, Velanovich V. Psychological and emotional aspects of gastroesophageal reflux disease. Dis Esophagus. 2002;15:199–203.
Fass R, Fennerty MB, Vakil N. Nonerosive reflux disease-current concepts and dilemmas. Am J Gastroenterol. 2001;96:303–14.
Watson RG, Tham TC, Johnston BT, McDougall NI. Double blind cross-over placebo controlled study of omeprazole in the treatment of patients with reflux symptoms and physiological levels of acid reflux, the sensitive esophagus. Gut. 1997;40:587–90.
Tew S, Jamieson GG, Pilowsky I, Myers J. The illness behavior of patients with gastroesophageal reflux disease with and without endoscopic esophagitis. Dis Esophagus. 1997;10:9–15.
Lind T, Havelund T, Carlsson R, Anker-Hansen O, Glise H, Hernqvist H, et al. Heartburn without oesophagitis: efficacy of omeprazole therapy and features determining therapeutic response. Scand J Gastroenterol. 1997;32:974–9.
Richter JE, Kovacs TO, Greski-Rose PA, Huang section sign B, Fisher R. Lansoprazole in the treatment of heartburn in patients without erosive oesophagitis. Aliment Pharmacol Ther. 1999;13:795–804.
Martinez SD, Malagon IB, Garewal HS, Cui H, Fass R. Non-erosive reflux disease (NERD)—acid reflux and symptom patterns. Aliment Pharmacol Ther. 2003;17:537–45.
Scheffer RC, Tatum RP, Shi G, Akkermans LM, Joehl RJ, Kahrilas PJ. Reduced tLESR elicitation in response to gastric distension in fundoplication patients. Am J Physiol Gastrointest Liver Physiol. 2003;284:G815–20.
Penagini R, Carmagnola S, Cantu P, Allocca M, Bianchi PA. Mechanoreceptors of the proximal stomach: role in triggering transient lower esophageal sphincter relaxation. Gastroenterology. 2004;126:49–56.
Zerbib F, Bicheler V, Leray V, Joubert M, Bruley des Varannes S, Galmiche JP. H. pylori and transient lower esophageal sphincter relaxations induced by gastric distension in healthy humans. Am J Physiol Gastrointest Liver Physiol. 2001;281:G350–6.
Chen CY, Chao Y, Chang FY, Chien EJ, Lee SD, Doong ML. Intracisternal des-acyl ghrelin inhibits food intake and non-nutrient gastric emptying in conscious rats. Int J Mol Med. 2005;16:695–9.
Yamada M, Hongo M, Okuno Y, Nishimura N, Ueno M, Kawakami H, et al. Effect of AS-4370 on gastric motility in patients with diabetic autonomic neuropathy. J Smooth Muscle Res. 1992;28:153–8.
Kanaizumi T, Nakano H, Matsui Y, Ishikawa H, Shimizu R, Park S, et al. Prokinetic effect of AS-4370 on gastric emptying in healthy adults. Eur J Clin Pharmacol. 1991;41:335–7.
Dickman R, Bautista JM, Wong WM, Bhatt R, Beeler JN, Malagon I, et al. Comparison of esophageal acid exposure distribution along the esophagus among the different gastroesophageal reflux disease (GERD) groups. Am J Gastroenterol. 2006;101:2463–9.
Svedlund J, Sjodin I, Dotevall G. GSRS—a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci. 1988;33:129–34.
Revicki DA, Wood M, Wiklund I, Crawley J. Reliability and validity of the Gastrointestinal Symptom Rating Sale in patients with gastroesophageal reflux disease. Qual Life Res. 1998;7:75–83.
Hellmig S, Von Schoning F, Gadow C, Katsoulis S, Hedderich J, Folsch UR, et al. Gastric emptying time of fluids and solids in healthy subjects determined by 13C breath tests: influence of age, sex and body mass index. J Gastroenterol Hepatol. 2006;21:1832–8.
Shindo T, Futagami S, Hiratsuka T, Horie A, Hamamoto T, Ueki N, et al. Comparison of gastric emptying and plasma ghrelin levels in patients with functional dyspepsia and non-erosive reflux disease. Digestion. 2009;79:65–72.
Schoeman MN, Holloway RH. Stimulation and characteristics of secondary oesophageal peristalsis in normal subjects. Gut. 1994;35:152–8.
Johnson LF, DeMeester TR. Twenty-four hour pH monitoring of the in the distal esophagus. Am J Gastroenterol. 1974;62:323–32.
Trimble KC, Douglas S, Pryde A, Heading RC. Clinical characteristics and natural history of symptomatic but not excess gastroesophageal reflux. Dig Dis Sci. 1995;40:1098–104.
Prather CM, Camilleri M, Zinsmeister AR, McKinzie S, Thomforde G. Tegaserod accelerates orocecal transit in patients with constipation-predominant irritable bowel syndrome. Gastroenterology. 2000;118:463–8.
Sanaka M, Urita Y, Sugimoto M, Yamamoto T, Kuyama Y. Comparison between gastric scintigraphy and the 13C-acetate breath test with Wagner–Nelson analysis in humans. Clin Exp Pharmacol Physiol. 2006;33:1239–43.
Asai H, Udaka F, Hirano M, Minami T, Oda M, Kubori T, et al. Increased gastric motility during 5-HT4 agonist therapy reduces response fluctuations in Parkinson’s disease. Parkinsonism Relat Disord. 2005;11:499–502.
Asakawa H, Hayashi I, Fukui T, Tokunaga K. Effect of mosapride on glycemic control and gastric emptying in type 2 diabetes mellitus patients with gastropathy. Diabetes Res Clin Pract. 2003;61:175–82.
Endo J, Nomura M, Morishita S, Uemura N, Inoue S, Kishi S, et al. Influence of mosapride citrate on gastric motility and autonomic nervous function: evaluation by spectral analyses of heart rate and blood pressure variabilities, and by electrogastrography. J Gastroenterol. 2002;37:888–95.
Wei W, Ge ZZ, Lu H, Gao YJ, Hu YB, Xiao SD. Effect of mosapride on gastrointestinal transit time and diagnostic yield of capsule endoscopy. J Gastroenterol Hepatol. 2007;22:1605–8.
Talley NJ, Verlinden M, Jones M. Can symptoms discriminate among those with delayed or normal gastric emptying in dysmotility-like dyspepsia? Am J Gastroenterol. 2001;96:1422–8.
Scott AM, Kellow JE, Shuter B, Cowan H, Corbett AM, Riley JW, et al. Intragastric distribution and gastric emptying of solids and liquids in functional dyspepsia. Lack of influence of symptom subgroups and H. pylori-associated gastritis. Dig Dis Sci. 1993;38:2247–54.
Quigley EM, DiBaise JK. Non-erosive reflux disease: the real problem in gastrooesophageal reflux disease. Dig Liver Dis. 2001;33:523–7.
Ruth M, Hamelin B, Rohss K, Lundell L. The effect of mosapride, a novel prokinetic, on acid reflux variables in patients with gastro-esophageal reflux disease. Aliment Pharmacol Ther. 1998;12:35–40.
Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Characteristics of gastroesophageal reflux in symptomatic patients with and without excessive esophageal acid exposure. Am J Gastroenterol. 2006;101:2470–5.
Weusten BL, Akkermans LM, vanBerge-Henegouwen GP, Smout AJ. Symptom perception in gastroesophageal reflux disease is dependent on spatiotemporal reflux characteristics. Gastroenterology. 1995;108:1739–44.
Fass R, Ofman JJ, Sampliner RE, Camargo L, Wendel C, Fennerty MB. The omeprazole test is as sensitive as 24-h oesophageal pH monitoring in diagnosing gastro-oesophageal reflux disease in symptomatic patients with erosive oesophagitis. Aliment Pharmacol Ther. 2000;14:389–96.
Cicala M, Emerenziani S, Caviglia R, Guarino MPL, Vavassori P, Ribolsi M, et al. Intra-oseophageal distribution and perception of acid reflux in patients with non-erosive gastro-oseophageal reflux disease. Aliment Pharmacol Ther. 2003;18:605–13.
Miwa H, Minoo T, Hojo M, Yaginuma R, Nagahara A, Kawabe M, et al. Oesophageal hypersensitivity in Japanese patients with non-erosive gastro-oesophageal reflux diseases. Aliment Pharmacol Ther. 2004;20(suppl 1):112–7.
Kaneko H, Konagaya T, Kakumu S. Visceral specific analgesic action of mosapride citrate, a gastroprokinetic drug, and its metabolite against gastric distention through a 5-HT4 and 5-HT3 receptor in conscious rats (abstr). Gastroenterology. 2006;130:A-246.
Iwakiri K, Kawami N, Sano H, Tanaka Y, Umezawa M, Kotoyori M, et al. Acid and non-acid reflux in Japanese patients with non-erosive reflux disease with persistent reflux symptoms, despite taking a double-dose of proton pump inhibitor: a study using combined pH-impedance monitoring. J Gastroenterol. 2009;44:708–12.
Mainie I, Tutuian R, Shay S, Vela M, Zhang X, Sifrim D, et al. Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut. 2006;55:1398–402.
Holloway RH. Esophageal body motor response to reflux events: secondary peristalsis. Am J Med. 2000;108:20–6.
Iwakiri K, Hayashi Y, Kotoyori M, Tanaka Y, Kawami N, Sano H, et al. Defective triggering of secondary peristalsis in patients with non-erosive reflux disease. J Gastroenterol Hepatol. 2007;22:2208–11.
Ruth M, Finizia C, Cange L, Lundell L. The effect of mosapride on esophageal motor function and acid reflux in patients with gastro-oesophageal reflux disease. Eur J Gastroenterol Hepatol. 2003;15:1115–21.
Quigley EM. Gastric motor and sensory function, and motor disorders of the stomach. In: Feldman M, Friedman LS, Sleisenger MH, editors. Gastrointestinal and liver disease, pathophysiology/diagnosis/management. Philadelphia: WB Saunders; 2002. p. 691–714.
Broglio F, Gottero C, Van Koetsveld P, Prodam F, Destefanis S, Benso A, et al. Acetylcholine regulates ghrelin secretion in humans. J Clin Endocrinol Metab. 2004;89:2429–33.
Osawa H, Nakazato M, Date Y, Kita H, Ohnishi H, Ueno H, et al. Impaired production of gastric ghrelin in chronic gastritis associated with Helicobacter pylori. J Clin Endocrinol Metab. 2005;90:10–6.
Suzuki H, Masaoka T, Hosoda H, Nomura S, Ohara T, Kangawa K, et al. Plasma ghrelin concentration correlates with the levels of serum pepsinogen I and pepsinogen I/II ratio-a possible novel and non-invasive marker for gastric atrophy. Hepatogastroenterology. 2004;51:1249–54.
Acknowledgments
This work was supported in part by grants from the Ministry of Education, Culture, and Science and from the Ministry of Health, Japan.
Conflict of interest statement
There is no conflict of interest statement in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Futagami, S., Iwakiri, K., Shindo, T. et al. The prokinetic effect of mosapride citrate combined with omeprazole therapy improves clinical symptoms and gastric emptying in PPI-resistant NERD patients with delayed gastric emptying. J Gastroenterol 45, 413–421 (2010). https://doi.org/10.1007/s00535-009-0173-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-009-0173-0