Abstract
Aims
Combined ERCP/EUS is becoming common. Combined procedures are frequently performed in elderly patients. We hypothesized that combined ERCP/EUS is equally safe in elderly patients when compared to non-elderly patients.
Methods
This was a retrospective single-center study comparing outcomes in elderly and non-elderly patients undergoing combined ERCP/EUS.
Results
A total of 206 patients were included. Mean age was 65 years (M:F 113:93); 99 were <65 years and 107 were >65. Indications included: jaundice (51 %), abnormal imaging (17 %), pancreatic tumor (11 %), abdominal pain (5 %), stent placement/change (5 %), acute or chronic pancreatitis (5 %), other (6 %). Fine needle aspiration was performed in 134 (65 %) procedures. Malignancy was identified in 142/206 (69 %) patients. Mean Charlson Comorbidity Index (CCI) was 7.5 (range 0–22). Among patients <65 years old there were no immediate adverse events. Long-term adverse events in patients <65 (within 30 days) included cholangitis (1), increasing abdominal pain (4), post-ERCP pancreatitis (3), nausea/vomiting (1), increasing fatigue (1), and increasing jaundice (1). A subgroup analysis among geriatric patients (>65) was performed. Mean CCI was 8.2 (range 0–22). There was one immediate adverse event of non-sustained ventricular tachycardia in a 76-year old. Long-term adverse events included increasing fatigue (1), nausea/vomiting (2), increasing abdominal pain (2), urosepsis (1), fever (2) and dehydration (1). There were no statistically significant differences in outcomes in elderly compared to non-elderly patients. Elderly patients had higher CCI scores (p = 0.04).
Conclusion
Combined ERCP/EUS in one session is safe in the general population and elderly patients, with no more adverse events than in non-elderly patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic ultrasound (EUS) has developed into a widely used and powerful tool for the evaluation of a variety of gastrointestinal disorders, most notably the staging of a variety of gastrointestinal cancers such as esophageal, gastric, pancreatic, and rectal cancer. EUS has also been widely used to investigate benign gastrointestinal conditions, such as choledocholithiasis and chronic pancreatitis. There has been little data on the safety and potential adverse events of EUS in the elderly [1–5].
Endoscopic retrograde cholangiopancreatography (ERCP) is another endoscopic procedure that is considered the gold standard in the diagnosis and treatment of pancreaticobiliary disease [6, 7]. Although the safety of ERCP in the elderly has been explored in the past, the majority of studies have been performed with smaller cohorts [8–15].
There has been one large study by Benson et al. [5] demonstrating no significant increase in the rate of overall procedure-related adverse events seen with either ERCP or EUS in elderly patients studying 1,000 geriatric patients (according to The World Health Organization’s definition of geriatric patients for developed countries defined as ≥65 years old) who underwent ERCP or EUS. There are limited data on the outcomes of combined EUS and ERCP in a single session (in either a general pool of patients or elderly patients) [16]. Combining these procedures takes advantage of the strengths of both modalities, allows for both diagnostic and therapeutic maneuvers, provides both prompt tissue diagnosis and relief of obstructive jaundice, completes locoregional staging, and reduces the delay for the initiation of neoadjuvant therapy in appropriate patients. However, to date, there have been no studies completed investigating adverse events seen with concomitant ERCP and EUS in elderly patients and no data exists comparing combined ERCP and EUS in elderly patients when compared to non-elderly patients.
As the median age of the population continues to rise, the volume of endosonographers in clinical practice increases, and the diagnostic and therapeutic roles of ERCP and EUS continue to expand, as increasing numbers of geriatric patients are referred for these advanced endoscopic procedures. A better understanding of potential adverse events related to these procedures within the elderly is necessary. The aim of this study was to investigate the findings, outcomes, and adverse events of patients receiving combined ERCP and EUS, with an emphasis on comparing outcomes in non-elderly to elderly individuals.
Materials and Methods
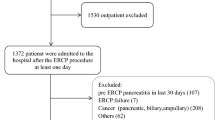
A retrospective chart review was performed of all patients 18 years and older who underwent combined EUS and ERCP at our institution. Data collected included but were not limited to age, gender, indication for procedure, primary and co-morbid medical conditions, procedure times, endoscopic and clinical outcomes, and pathology reports.
All procedures were performed under general anesthesia with patients in the prone position for the duration of the combined ERCP/EUS procedures. Olympus echoendoscopes and duodenoscopes were used for all procedures. All cases were performed by a single endoscopist (DGA) with the assistance of a third year gastroenterology fellow.
Comorbidity scores were calculated for each patient using the Charlson Comorbidity Index (CCI) (Charlson, ME). A subgroup analysis of all elderly patients (≥65 years old) was performed and compared to non-elderly patients. This study was approved by the University of Utah Institutional Review Board.
Statistical Analysis
Data were analyzed using STATA v10 statistical software for Windows (College Station, TX, StataCorp LP). Continuous variables were analyzed with a t test for independent samples. All statistical tests were analyzed as two-sized unless otherwise stated. A p value of <0.05 was considered significant.
Results
Demographic Data
Combined ERCP and EUS was performed on 206 patients between July 2006 through December 2010. Mean patient age was 65 years (range 24–92 years). There were 93/206 (45 %) females compared to 113/206 (55 %) males. A subgroup analysis among geriatric patients (age 65 and older) was performed (n = 107). Indications for ERCP/EUS in all age groups were as follows: jaundice (51 %), abnormal imaging (17 %), previously diagnosed pancreatic tumor (11 %), abdominal pain (5 %), stent placement/change with need for additional tissue (5 %), acute or chronic pancreatitis (5 %), evaluation and treatment of suspected choledocholithiasis (6 %) (see Table 1).
Among patients less than 65 years old, 14 were treated as inpatients and 85 were treated as outpatients. Among patients greater than 65 years old, 13 were treated as inpatients and 94 were treated as outpatients. All outpatients were discharged to home on the same day as the procedure. In both groups inpatient mean length of stay was 3 days, including the day of the procedure.
Indications for ERCP/EUS in patients under 65 were as follows: jaundice 45 %, abnormal imaging 22 %, pancreatic mass 10 %, abdominal pain 9 %, stent placement/change 2 %, acute or chronic pancreatitis 9 %, evaluation and treatment of suspected choledocholithiasis 2 %.
Indications for patients over 65 were as follows: patients received ERCP for jaundice in 56 %, abnormal imaging 12 %, pancreatic mass 13 %, abdominal pain of suspected pancreaticobiliary origin 0.9 %, stent placement/change with need for tissue acquisition 7 %, acute or chronic pancreatitis 0.9 %, evaluation and treatment of suspected choledocholithiasis 9 % (see Table 1).
EUS Guided Fine Needle Aspiration
Fine needle aspiration (FNA) was performed in 134 (65 %) of EUS procedures overall. FNA was performed in 43 of 103 (42 %) of patients under 65 years and in 67 of 107 (63 %) of patients 65 and older. The mean number of needle passes in both groups was three. There were no FNA-related adverse events in patients under or older than 65 years.
Final Clinical Diagnosis
Specific data regarding diagnoses in patients over or under 65 years of age are presented in Table 2. Among patients under 65 who were found to have malignant disease, metastatic pancreatic cancer was found in 23/58 (40 %) cases, localized pancreatic cancer was identified in 19/58 (33 %) cases, cholangiocarcinoma in 7/58 (12 %) cases, metastases to the pancreas in 4/58 (7 %) cases, and ampullary cancer in 3/58 (5 %) cases (see Table 3).
Thirty-eight out of 99 (38 %) cases yielded benign diagnoses. Three patients were indeterminate for malignancy on long-term follow up. Benign findings were as follows: benign biliary stricture in 16/38 (42 %), abdominal pain in 5/38 of pancreaticobiliary origin (13 %), dilated bile ducts without other underlying pathology in 6/38 (16 %), bile duct stones in 3/38 (8 %), acute pancreatitis in 3/38 (8 %), inflammatory pancreatic cysts in 3/38 (8 %) and 2/38 (5 %) were diagnosed as chronic pancreatitis. The diagnosis of abdominal pain of pancreaticobiliary origin was reached if the patient was felt to have findings that did not fit into other benign categories such as ampullary/sphincter-related issues such as evaluation of ampullary adenomas, patients undergoing ampullectomy, patients with HIV cholangiopathy, etc.
Among patients older than 65 with malignant diagnoses, localized pancreatic cancer was identified in 47/85 (55 %) cases, metastatic pancreatic cancer in 22/85 (25 %), cholangiocarcinoma in 4/85 (5 %) cases, ampullary cancer in 4/85 (5 %) cases, and metastases to the pancreas in 4/85 (5 %) cases (see Table 3). Sixteen out of 107 (15 %) of these patients were ultimately found to have benign diagnoses. There were seven cases that were indeterminate. Of the benign findings, abdominal pain of pancreaticobiliary origin was found in 3/16 (19 %), dilated bile ducts in 4/16 (25 %), acute pancreatitis in 1/16 (6 %), benign biliary stricture in 7/16 (44 %), and ascending cholangitis in 1/16 (6 %).
Charlson Comorbidity Index Scores
The mean CCI among all ages was 7.5 (0–22). The mean CCI for elderly patients was 8.2 (range 0–22). Among patients under 65, the mean CCI was 6.8 (0–22). Elderly patients had higher mean CCI scores by chi-square testing, and this was statistically significant, (p = 0.04). There was also a statistically significant correlation between age and mean CCI scores via Spearman’s rank test (p = 0.02).
Adverse Events
Among patients under 65-years old there were no immediate adverse events. Long-term adverse events (within 30 days) in patients under 65 years of age that may have been attributed to the ERCP/EUS procedure included ascending cholangitis (1), increasing abdominal pain (4), mild post-ERCP pancreatitis (3), nausea/vomiting requiring treatment (1), severe fatigue (1), and worsening jaundice (1).
In patients over 65 years of age, there was one intra-procedure adverse event of non-sustained ventricular tachycardia in a 76-year-old female which resolved spontaneously. Long-term adverse events included fatigue (1), nausea/vomiting requiring treatment (2), increasing abdominal pain (2), urosepsis (1), fever due to bacteremia from a pleural effusion (2), and dehydration (1). There were no statistically significant differences in adverse events or outcomes in elderly versus non-elderly patients when age was analyzed both as a dichotomous and a continuous variable.
Duration of Combined Procedures
Procedure times were similar among patients under 65 and patients 65 and older. Mean combined ERCP/EUS time in patients under 65 was 58 ± 1.8 min. Mean procedure times for combined ERCP/EUS in patients over 65 was 56 ± 2.1 min. There was no statistically significant difference between procedure times for the two groups (p = 0.5). Of note, no procedures were rendezvous procedures.
Discussion
While ERCP is considered the gold standard for the endoscopic diagnosis and treatment of biliary diseases, the procedure is not without risk. ERCP carries a higher potential for adverse events ranging from minor issues such as abdominal discomfort to major adverse events including post-ERCP pancreatitis (which can be severe), cholangitis, infection, bleeding, and perforation. Though the safety of ERCP performed in isolation in the elderly has been explored in the past, the majority of studies have been performed with smaller cohorts [8–15]. Furthermore, there has been very little data on the safety and potential adverse events of ERCP and EUS in the elderly, and there is no data on the outcomes of combined EUS and ERCP in a single session in elderly patients at all, let alone when compared to non-elderly patients.
Our study is the largest study to date to focus on the outcomes for combined ERCP/EUS in the elderly as compared to non-elderly patients. The use of Charlson Comorbidity Index scores (a prospective applicable method for classifying comorbid conditions that may alter the risk of mortality) in this context is also novel.
The reported rate of significant adverse events with pancreatic FNA is 2.5–5 %, and the risk of pancreatitis is 0.5–2.0 % [17–20]. ERCP adverse event rates have been reported between 5 and 15.9 % based on previous studies; however, our adverse event rates were lower, on average, than expected when compared to previous studies [5, 21]. Among patients under and over 65 years of age in our study, we did not encounter any immediate adverse events. Long-term adverse events tended to be typically mild. Using the Charlson Comorbidity Index score, we did not find any difference in adverse event rates between patients within both age groups based on our study. Our study is also the first to investigate potential adverse events in patients undergoing combined procedures while under general anesthesia rather than moderate sedation only; as described above, combined procedures under general anesthesia for both the elderly and non-elderly appear to be well tolerated.
There were no severe adverse events such as perforation, significant bleeding, pancreatitis, death, intra-procedure mild bleeding, intra-procedure respiratory or hemodynamic compromise, or significant post-procedure pain. Infectious complications were uncommon. Adverse events that did occur were mild, rare and self limited in both age groups. There was no 30-day mortality in either age group.
Despite higher CCI scores, there was no statistically significant increase in the adverse event rate for elderly patients undergoing ERCP and EUS compared to non-elderly patients undergoing combined procedures (p = 0.61). Our procedure times were similar among patients under 65 and patients 65 and older; specifically there was no statistically significant difference between procedure times for the two groups. Our results suggest that combined EUS and ERCP can be performed safely in elderly and non-elderly patients without a greater adverse event rate than those published for EUS and ERCP in either of these patient groups alone. Advanced age itself should not be an absolute contraindication to these combined endoscopic interventions.
In this study, general anesthesia was administered for all patients undergoing simultaneous ERCP and EUS. The elderly group appeared to tolerate general anesthesia just as well as the non-elderly. Previous studies have suggested that elderly patients may be more sensitive to sedating agents [22]; there was only one patient in our study (age 76) who experienced non-sustained ventricular tachycardia while under anesthesia that spontaneously resolved, arguing that general anesthesia for combined ERCP/EUS in these patients is safe.
Our study is the first and largest to investigate the safety of combined ERCP with EUS in the elderly. A study by Benson et al. [5] evaluated adverse events from ERCP and EUS in the elderly compared to the non-elderly; however, the study did not evaluate the risks of combined procedures which are more time consuming and involve more sedation. Additionally, whereas FNA was performed in 21 % of EUS procedures overall for Benson’s study, FNA was performed in 65 % of procedures in our study, evidencing good patient tolerance of a high rate of endoscopic interventions.
A study by Ross et al. investigated outcomes for patients undergoing combined EUS and ERCP; however, there were only a total of 114 patients during the study period with overall mean age at 62.6. This study contained insufficient data specifically relating to the elderly to make conclusions regarding the safety of combined procedures for the elderly [16].
Limitations of the study include its retrospective, single-center design and the fact that this study reflects the experience of a single operator who is very experienced in both ERCP and EUS, which could limit generalizability to some extent. The fact that a third year gastroenterology fellow was involved in 100 % of cases may help to expand generalizability. Factors in support of this study include a large number of patients and a high rate of long-term follow up. Additionally, despite a heterogenous group of patients covering a period of four and one-half years, the procedures were performed by one endoscopist, providing fewer potential confounding factors.
Combined ERCP/EUS procedures enable rapid initiation of appropriate care including establishment of tissue diagnosis, complete local staging and relieving biliary obstruction in a single session. Based on our study, these combined procedures appear feasible with an adverse event rate no greater than that for each individual procedure in both the elderly and non-elderly patients.
Conclusion
Overall, our data demonstrates that combined ERCP/EUS procedures under general anesthesia appear to be safe, efficient and can be performed during a single session without compromising patient safety. Age greater than 65 does not appear to be associated with adverse events or poor outcomes. Combining both procedures expedites patient evaluation and reduces the demand on repeat endoscopic sessions.
References
Conway JD, Hawes RH. The expanding role of endoscopic ultrasound in pancreatic disease. Rev Gastroenterol Disord. 2006;6:201–208.
Caddy GR, Chen RY. Current clinical applications of endoscopic ultrasound. ANZ J Surg. 2007;77:101–111.
Irisawa A, Katakura K, Ohira H, et al. Usefulness of endoscopic ultrasound to diagnose the severity of chronic pancreatitis. J Gastroenterol. 2007;42:90–94.
Verma D, Kapadia A, Adler DG. EUS versus MRCP for detection of choledocholithiasis. Gastrointest Endosc. 2006;64:248–254.
Benson M, Byrne S, Brust D, et al. EUS and ERCP complication rates are not increased in elderly patients. Digestive Diseases and Sciences. 2010;55:3278–3283.
Gluck M, Cantone NR, Brandabur JJ, Patterson DJ, Bredfeldt JE, Kozarek RA. A twenty-year experience with endoscopic therapy for symptomatic primary sclerosing cholangitis. J Clin Gastroenterol. 2008;42:1032–1039.
Etzel JP, Eng SC, Ko CW, et al. Complications after ERCP in patients with primary sclerosing cholangitis. Gastrointestinal Endosc. 2008;67:643–648.
Katsinelos P, Paroutoglou G, Kountouras J, Zavos C, Beltsis A, Tzovaras G. Efficacy and safety of therapeutic ERCP in patients 90 years of age and older. Gastrointest Endosc. 2006;63:417–423.
Mitchell RM, O’Connor F, Dickey W. Endoscopic retrograde cholangiopancreatography is safe and effective in patients 90 years of age and older. J Clin Gastroenterol. 2003;36:72–74.
Rodriguez-Gonzalez FJ, Naranjo-Rodriguez A, Mata-Tapia I, et al. ERCP in patients 90 years of age and older. Gastrointest Endosc. 2003;58:220–225.
Chong VH, Yim HB, Lim CC. ERCP in the elderly: more than just the age factor. Age Ageing. 2006;35:322–323.
Deans GT, Sedman P, Martin DF, et al. Are complications of endoscopic sphincterotomy age related? Gut. 1997;41:545–548.
Gandolfi L, Rossi A, Vaira D, Tonti R, Ramini R. Endoscopic retrograde cholangiopancreatography (ERCP) in the elderly. Acta Gastroenterol Belg. 1986;49:602–607.
MacMahon M, Walsh TN, Brennan P, Osborne H, Courtney MG. Endoscopic retrograde cholangiopancreatography in the elderly: a single unit audit. Gerontology. 1993;39:28–32.
Rastogi A, Campbell DR. ERCP in the elderly: How safe is it? (Marathons, marathon ERCPs, and marathon ERCPs in the elderly). Gastrointest Endosc. 2006;63:956–958.
Ross WA, Wasan SM, Evans DB, et al. Combined EUS with FNA and ERCP for the evaluation of patients with obstructive jaundice from presumed pancreatic malignancy. Gastrointest Endosc. 2008;68:461–466.
Eloubeidi MA, Gress FG, Savides TJ, et al. Acute pancreatitis after EUS guided FNA of solid pancreatic masses: a pooled analysis from EUS centers in the United States. Gastrointest Endosc. 2004;60:385–389.
Gress FG, Gottlieb K, Sherman S, et al. Endoscopic ultrasonographyguided fine-needle aspiration biopsy of suspected pancreatic cancer. Ann Intern Med. 2001;134:459–464.
American Society for Gastrointestinal Endoscopy, Adler DG, Jacobson BC, et al. ASGE guidelines: complications of EUS. Gastrointest Endosc. 2005;61:8–12.
Eloubeidi MA, Tamhane A, Varadarajulu S, et al. Frequency of major complications after EUS-guided FNA of solid pancreatic masses: a prospective evaluation. Gastrointest Endosc. 2006;63:622–629.
Freeman ML. Post-ERCP pancreatitis: patient and technique-related risk factors. JOP. 2002;3:169–176.
Rivera R, Antognini JF. Perioperative drug therapy in elderly patients. Anesthesiology. 2009;110:1176–1181.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iles-Shih, L., Hilden, K. & Adler, D.G. Combined ERCP and EUS in One Session Is Safe in Elderly Patients When Compared to Non-elderly Patients: Outcomes in 206 Combined Procedures. Dig Dis Sci 57, 1949–1953 (2012). https://doi.org/10.1007/s10620-012-2135-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2135-2